Spirochetes overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Spirochetes overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Spirochetes overview US Medical PG Question 1: A 24-year-old man presents with a painless genital ulcer for the past 2 weeks. He reports that he recently has been having unprotected sex with multiple partners. Past medical history is unremarkable. On physical examination, a single ulcer is present on the dorsal shaft of the penis which is circumscribed, indurated, and partially healed. There is moderate inguinal lymphadenopathy but no buboes. Which of the following tests would confirm the most likely diagnosis in this patient?
- A. Perform a darkfield microscopic examination of a swab from the chancre (Correct Answer)
- B. Swab the chancre and perform a saline wet mount
- C. Fluorescent treponemal antibody absorption (FTA-ABS) test
- D. Frei test
- E. Venereal Disease Research Laboratory (VDRL) test
Spirochetes overview Explanation: ***Perform a darkfield microscopic examination of a swab from the chancre***
- This patient's presentation with a **painless, indurated genital ulcer** (chancre) and regional lymphadenopathy is highly suggestive of **primary syphilis**.
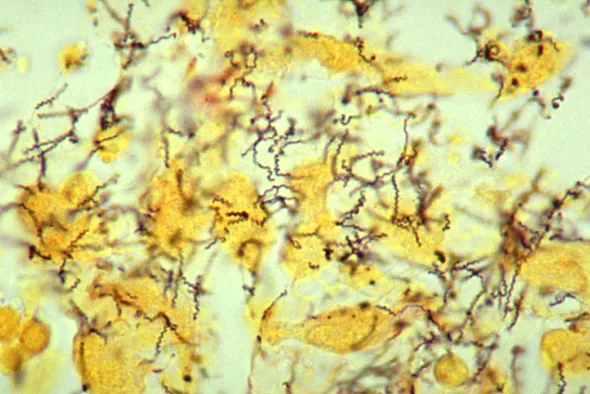
- **Darkfield microscopy** directly visualizes the spirochetes (**_Treponema pallidum_**) from the chancre, providing a definitive and rapid diagnosis.
*Swab the chancre and perform a saline wet mount*
- A **saline wet mount** is used to identify mobile organisms like **_Trichomonas vaginalis_** or clue cells suggestive of **bacterial vaginosis**, neither of which are associated with this type of ulcer.
- This test would not reveal the spirochetes responsible for syphilis and is not appropriate for diagnosing a genital ulcer.
*Fluorescent treponemal antibody absorption (FTA-ABS) test*
- The **FTA-ABS test** is a **treponemal-specific serological test** used to confirm a syphilis diagnosis, particularly in later stages or when non-treponemal tests are reactive.
- While sensitive for syphilis, it's typically reactive later in the disease course and cannot directly visualize the bacteria from the ulcer, making darkfield microscopy a more immediate and direct diagnostic tool for primary syphilis.
*Frei test*
- The **Frei test** is an obsolete intradermal skin test used to diagnose **lymphogranuloma venereum (LGV)**, which typically presents with a transient, unnoticed lesion followed by severe lymphadenopathy and buboes.
- It is not used for the diagnosis of syphilis and would not be helpful for this patient's presentation.
*Viral and rickettsial disease research laboratory (VDRL) test*
- The **VDRL test** is a **non-treponemal serological test** for syphilis that detects antibodies against cardiolipin, a lipid released from damaged host cells.
- While used for screening and monitoring treatment response, it can be **negative in early primary syphilis** (before seroconversion) and may not be positive at the time of presentation with a fresh chancre.
Spirochetes overview US Medical PG Question 2: A 23-year-old G1P0 female presents to her OB/GYN for her routine 36-week visit. Her current complaints include increased fatigue at the end of the day, and edema in her ankles. The patient’s physical examination is unremarkable except for inguinal adenopathy. Upon pelvic examination for cervical changes, the OB/GYN notices a vaginal chancre. The patient states that it is not painful when touched. Which of the following is the most likely diagnosis?
- A. Secondary syphilis
- B. Cardiovascular syphilis
- C. Primary syphilis (Correct Answer)
- D. Gummatous syphilis
- E. Neurosyphilis
Spirochetes overview Explanation: ***Primary syphilis***
- A **painless chancre** is the hallmark lesion of primary syphilis, which develops at the site of initial inoculation.
- While fatigue and edema are common in pregnancy, the presence of a **painless vaginal chancre** and **inguinal adenopathy** is highly indicative of primary syphilis.
*Secondary syphilis*
- This stage is characterized by a **disseminated skin rash** (often involving palms and soles), **condyloma lata**, and generalized lymphadenopathy, not a solitary chancre.
- Symptoms usually appear several weeks or months after the chancre of primary syphilis has healed.
*Cardiovascular syphilis*
- This is a form of **tertiary syphilis** that affects the heart and great vessels, typically resulting in **aortitis**, aneurysms, or aortic regurgitation.
- It develops years to decades after the initial infection and would not present with a chancre.
*Gummatous syphilis*
- This is another manifestation of **tertiary syphilis**, characterized by the formation of **gummas**—soft, non-cancerous granulomas that can affect any organ.
- Like cardiovascular syphilis, it occurs many years after initial infection and does not involve a primary chancre.
*Neurosyphilis*
- This involves the **central nervous system** and can occur at any stage of syphilis, but is usually a late complication.
- Symptoms vary widely but include **meningitis**, strokes, or psychiatric manifestations, none of which are consistent with a chancre or the acute presentation described.
Spirochetes overview US Medical PG Question 3: A 21-year-old man comes to the physician's office due to a 3-week history of fatigue and a rash, along with the recent development of joint pain that has moved from his knee to his elbows. The patient reports going camping last month but denies having been bitten by a tick. His past medical history is significant for asthma treated with an albuterol inhaler. His pulse is 54/min and blood pressure is 110/72. Physical examination reveals multiple circular red rings with central clearings on the right arm and chest. There is a normal range of motion in all joints and 5/5 strength bilaterally in the upper and lower extremities. Without proper treatment, the patient is at highest risk for which of the following complications?
- A. Liver capsule inflammation
- B. Bone marrow failure
- C. Heart valve stenosis
- D. Glomerular damage
- E. Cranial nerve palsy (Correct Answer)
Spirochetes overview Explanation: ***Cranial nerve palsy***
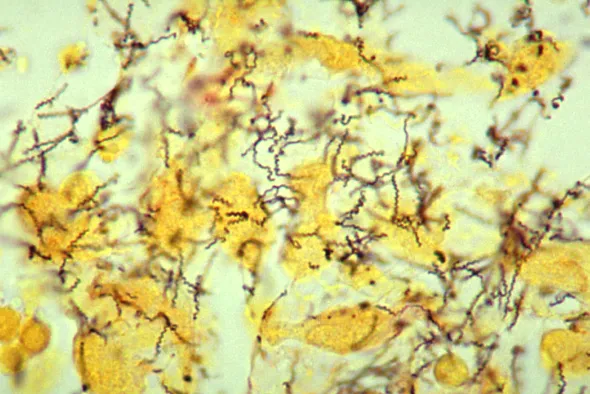
- This patient presents with classic **Lyme disease** (caused by *Borrelia burgdorferi*), including camping exposure, fatigue, migratory arthralgia, and **erythema migrans** (multiple circular red rings with central clearings on the arm and chest).
- The **bradycardia (pulse 54/min)** suggests early **Lyme carditis** with possible first-degree AV block, which typically resolves with treatment and rarely progresses to complete heart block in treated cases.
- Without proper antibiotic treatment, **cranial neuropathy** is one of the most common neurological complications in early disseminated Lyme disease, with **facial nerve palsy (Bell's palsy)** being the most frequent, occurring in up to 10% of untreated patients.
- Other neurological complications include meningitis, radiculoneuropathy, and peripheral neuropathy, making neurologic involvement a significant risk in untreated disease.
*Liver capsule inflammation*
- **Perihepatitis (Fitz-Hugh-Curtis syndrome)** is associated with **pelvic inflammatory disease (PID)** caused by *Chlamydia trachomatis* or *Neisseria gonorrhoeae*, not Lyme disease.
- This presents with right upper quadrant pain and "violin string" adhesions between the liver capsule and peritoneum.
*Bone marrow failure*
- **Bone marrow failure** (aplastic anemia) can be caused by parvovirus B19, certain medications, radiation, or idiopathic causes, but is **not a recognized complication of Lyme disease**.
- Lyme disease primarily affects the skin, joints, heart (conduction system), and nervous system, not hematopoietic function.
*Heart valve stenosis*
- **Lyme carditis** affects the **cardiac conduction system**, causing **AV blocks** (first, second, or third degree) and myocarditis, as suggested by this patient's bradycardia.
- Lyme does **not cause valvular stenosis or regurgitation**. Valvular disease is associated with rheumatic fever (post-streptococcal), endocarditis, or degenerative changes.
- The cardiac manifestations of Lyme typically resolve with appropriate antibiotic therapy and rarely cause permanent structural damage.
*Glomerular damage*
- **Glomerulonephritis** is not a typical complication of Lyme disease in humans (though "Lyme nephritis" occurs in dogs).
- Renal involvement in human Lyme disease is extremely rare and not a significant clinical concern compared to neurological, cardiac, or rheumatological manifestations.
Spirochetes overview US Medical PG Question 4: A 25-year-old professional surfer presents to the emergency room with leg pain and a headache. He recently returned from a surf competition in Hawaii and has been feeling unwell for several days. He regularly smokes marijuana and drinks 6-7 beers during the weekend. He is otherwise healthy and does not take any medications. His temperature is 102.2°F (39°C), blood pressure is 121/78 mmHg, pulse is 120/min, and respirations are 18/min saturating 99% on room air. He is sitting in a dim room as the lights bother his eyes and you notice scleral icterus on physical exam. Cardiopulmonary exam is unremarkable. Which of the following findings would most likely be seen in this patient?
- A. Epithelial cells covered with gram-variable rods
- B. Treponemes on dark-field microscopy
- C. Granulocytes with morulae in the cytoplasm
- D. Question mark-shaped bacteria on dark-field microscopy (Correct Answer)
- E. Monocytes with morulae in the cytoplasm
Spirochetes overview Explanation: ***Question mark-shaped bacteria on dark-field microscopy***
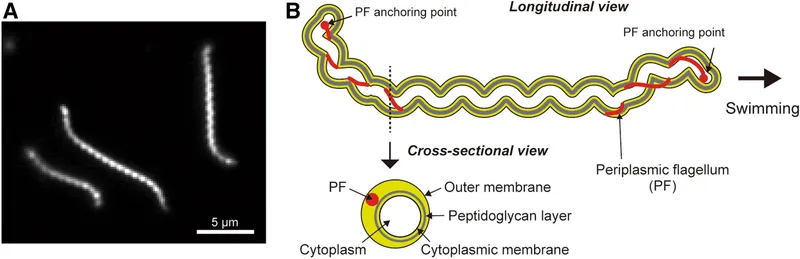
The patient's symptoms (fever, headache, leg pain, photophobia, and especially **scleral icterus** after returning from Hawaii) are highly suggestive of **leptospirosis**. **Leptospira interrogans** is a spirochete characterized by its **question mark-shape** and can be visualized using **dark-field microscopy** in early stages of infection from blood or CSF, and later in urine.
*Epithelial cells covered with gram-variable rods*
This description is characteristic of **bacterial vaginosis**, where epithelial cells are covered by **Gardnerella vaginalis** and other bacteria, forming "clue cells." This condition is a genital infection and does not align with the systemic symptoms and exposures described in the patient.
*Treponemes on dark-field microscopy*
**Treponema pallidum** is the causative agent of **syphilis**, which is also a spirochete and can be identified by dark-field microscopy from chancres. While this is a spirochetal infection, the clinical presentation of fever, leg pain, severe headache, photophobia, and jaundice (scleral icterus) following exposure to tropical waters is characteristic of leptospirosis, not early syphilis.
*Granulocytes with morulae in the cytoplasm*
**Morulae** (intracellular mulberry-shaped aggregates of bacteria) in the cytoplasm of **granulocytes** are characteristic of **anaplasmosis**, caused by Anaplasma phagocytophilum. While anaplasmosis can cause fever and headache, it is typically a tick-borne illness and does not explain the prominent **icterus** or the Hawaii exposure in this context.
*Monocytes with morulae in the cytoplasm*
**Morulae** within the cytoplasm of **monocytes** are characteristic of **ehrlichiosis**, caused by Ehrlichia chaffeensis. Like anaplasmosis, ehrlichiosis is a tick-borne disease and does not fit the epidemiological context (surfing in Hawaii) or the specific clinical picture (notably **icterus**) as well as leptospirosis.
Spirochetes overview US Medical PG Question 5: A previously healthy 25-year-old male comes to his primary care physician with a painless solitary lesion on his penis that developed 4 days ago. He has not experienced anything like this before. He is currently sexually active with multiple partners and uses condoms inconsistently. His temperature is 37.0°C (98.7°F), pulse is 67/min, respirations are 17/min, and blood pressure is 110/70 mm Hg. Genitourinary examination shows a shallow, nontender, firm ulcer with a smooth base along the shaft of the penis. There is nontender inguinal adenopathy bilaterally. Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Rapid plasma reagin
- B. Urine polymerase chain reaction
- C. Fluorescent treponemal antibody absorption test
- D. Swab culture
- E. Dark-field microscopy (Correct Answer)
Spirochetes overview Explanation: ***Dark-field microscopy***
- The patient's presentation with a **painless, firm, shallow ulcer** (chancre) on the penis and **bilateral nontender inguinal adenopathy**, in the context of high-risk sexual behavior, is highly suggestive of **primary syphilis**.
- **Dark-field microscopy** of exudate from the chancre allows for direct visualization of motile *Treponema pallidum* spirochetes and is the definitive method for confirming primary syphilis, especially before serological tests become positive.
*Rapid plasma reagin*
- **RPR is a nontreponemal serological test** used for screening syphilis. It typically becomes reactive 1-3 weeks after the appearance of a chancre.
- Given that the lesion developed only 4 days ago, the RPR might still be **negative due to the lag phase** before antibody production.
*Urine polymerase chain reaction*
- A **urine PCR** is primarily used to detect nucleic acids of infectious agents, commonly for conditions like chlamydia or gonorrhea.
- It is **not the standard or most accurate method** for diagnosing syphilis, which is caused by a spirochete and typically diagnosed by direct visualization or serology.
*Fluorescent treponemal antibody absorption test*
- The **FTA-ABS is a treponemal-specific serological test** that usually becomes reactive earlier than non-treponemal tests (like RPR), but still typically weeks after infection.
- While sensitive, it is generally used as a **confirmatory test** for positive nontreponemal results or when clinical suspicion is high and nontreponemal tests are initially negative. It is not a direct detection method.
*Swab culture*
- **Swab culture** is used to grow bacteria for identification and susceptibility testing.
- *Treponema pallidum*, the causative agent of syphilis, **cannot be cultured on artificial media**, making swab culture an inappropriate diagnostic method for syphilis.
Spirochetes overview US Medical PG Question 6: A 14-year-old girl presents with fever, headache, and muscle aches that have lasted for 2 days. She also complains of malaise and pain in her joints. She says she just returned from a camping trip in Delaware. Her past medical history is not significant. The patient denies any recent sick contacts. Her temperature is 38.3°C (101.0°F), pulse is 87/min, respirations are 17/min, and blood pressure is 120/78 mm Hg. On physical examination, there is a 3-inch-diameter, red, erythematous, round rash with central clearing on the right leg (see image). Antibodies against Proteus vulgaris OX-19 are absent. Which of the following is the most likely cause of this patient’s symptoms?
- A. Chlamydia trachomatis
- B. Dermatophytosis
- C. Rickettsia rickettsii
- D. Measles virus
- E. Borrelia burgdorferi (Correct Answer)
Spirochetes overview Explanation: ***Borrelia burgdorferi***
- The patient's symptoms (fever, headache, muscle aches, joint pain, malaise) coinciding with a recent camping trip in an endemic area for Lyme disease (Delaware), along with the characteristic **erythema migrans rash** (red, erythematous, round rash with central clearing), are highly suggestive of Lyme disease, caused by *Borrelia burgdorferi*.
- This **bull's-eye rash** is pathognomonic for Lyme disease and often appears within days to weeks of a tick bite.
*Chlamydia trachomatis*
- This bacterium primarily causes sexually transmitted infections (STIs) and can cause **conjunctivitis, urethritis, cervicitis**, or **pelvic inflammatory disease**.
- It does not typically cause a systemic febrile illness with a migratory rash or joint pain in this manner.
*Dermatophytosis*
- Dermatophytosis, or **ringworm**, is a fungal infection of the skin that can present with a red, annular rash.
- However, it is usually **itchy** and **scaly**, lacks the central clearing seen in erythema migrans, and typically does not cause systemic symptoms like fever, headache, and widespread muscle/joint aches.
*Rickettsia rickettsii*
- This is the causative agent of **Rocky Mountain spotted fever (RMSF)**, which also presents with fever, headache, and muscle aches following a tick bite.
- However, the rash of RMSF is typically a **maculopapular rash** that appears on the **wrists and ankles** and then spreads centrally, becoming petechial, and
- **Antibodies against Proteus vulgaris OX-19** (Weil-Felix test), which are used for diagnosis of Rickettsial infections, are absent in this case, ruling out RMSF.
*Measles virus*
- Measles (rubeola) is a highly contagious viral infection characterized by a prodrome of **fever, cough, coryza, and conjunctivitis**, followed by **Koplik spots** in the mouth.
- The rash of measles typically appears as a **maculopapular rash** that starts on the face and spreads downwards, which is distinct from the erythema migrans observed.
Spirochetes overview US Medical PG Question 7: A 42-year-old man comes to his physician with a history of fever, non-bloody diarrhea, and headache for 10 days. He also complains of anorexia and abdominal pain. He returned from a trip to India 3 weeks ago. His temperature is 40.0°C (104.0°F), pulse is 65/min, respirations are 15/min, and blood pressure is 135/80 mm Hg. He has developed a blanchable rash on his chest and trunk. A photograph of the rash is shown. Examination of the heart, lungs, and abdomen show no abnormalities. Laboratory studies show:
Hemoglobin 15 g/dL
Mean corpuscular volume 95 μm3
White blood cell count 3400/mm3
Percent segmented neutrophils 40%
Which of the following is the most likely diagnosis?
- A. Leptospirosis
- B. Enteric fever (Correct Answer)
- C. Dengue fever
- D. Malaria
- E. Nontyphoidal salmonellosis
Spirochetes overview Explanation: ***Enteric fever***
- The constellation of **fever**, **non-bloody diarrhea**, **bradycardia** (pulse 65/min with 40°C fever), **leukopenia** (WBC 3400/mm³), **rose spots** (blanchable rash on chest/trunk), and recent travel to **India** (endemic area) is highly characteristic of enteric fever caused by *Salmonella Typhi* or *Paratyphi*.
- Abdominal pain, anorexia, and headache are also common symptoms, and the relatively low **neutrophil percentage** (40%) further supports the diagnosis of a bacterial infection with atypical white blood cell response.
*Leptospirosis*
- While leptospirosis can cause **fever** and **headache** and is found in tropical regions, it typically presents with **conjunctival suffusion**, **muscle pain**, and sometimes **jaundice** or **renal involvement**, none of which are detailed here.
- Exposure usually involves contact with contaminated water or soil, and **diarrhea** is less common than in enteric fever.
*Dengue fever*
- Dengue fever is characterized by **high fever**, severe **myalgia** and **arthralgia** ("breakbone fever"), and often a **maculopapular rash**, but **bradycardia** and **leukopenia** with low neutrophils are not typical features.
- **Hemorrhagic manifestations** are also a concern in severe dengue, which are not described.
*Malaria*
- Malaria presents with cyclical **fever** (often paroxysmal), **chills**, **sweats**, and frequently causes **anemia** and **thrombocytopenia**.
- While **leukopenia** can occur, the presence of **rose spots** and sustained fever with relative **bradycardia** point away from malaria as the primary diagnosis.
*Nontyphoidal salmonellosis*
- This typically causes **gastroenteritis** with **diarrhea**, **vomiting**, and **fever**, which is usually self-limiting.
- It would not typically present with **rose spots**, pronounced **bradycardia**, or a prolonged course with systemic symptoms suggestive of enteric fever.
Spirochetes overview US Medical PG Question 8: A 24-year-old female comes to the physician because of flu-like symptoms and a new rash for 2 days. She denies contacts with sick individuals or recent travel abroad, but recently went camping in Vermont. Vital signs are within normal limits. Examination of the lateral right thigh shows a circular red ring with central clearing. Which of the following is the natural reservoir of the pathogen responsible for this patient's symptoms?
- A. Rat
- B. Rabbit
- C. Tick
- D. Mouse (Correct Answer)
- E. Flea
Spirochetes overview Explanation: ***Mouse***
- The patient's symptoms, including **flu-like illness** and a **circular red rash with central clearing** (erythema migrans) after camping in Vermont, are classic for **Lyme disease**.
- The causative agent, *Borrelia burgdorferi*, is primarily maintained in **white-footed mice** (genus *Peromyscus*) in its natural reservoir during its larval and nymphal stages.
*Rat*
- While **rats** can carry and transmit various diseases, they are not the primary natural reservoir for *Borrelia burgdorferi*, the pathogen responsible for Lyme disease.
- Diseases associated with rats often include **leptospirosis** and **plague**, which present with different clinical pictures.
*Rabbit*
- **Rabbits** are known reservoirs for diseases like **tularemia** (*Francisella tularensis*), which can cause fever, skin lesions, and lymphadenopathy, but typically not the characteristic **erythema migrans** rash.
- They are not a significant natural reservoir for *Borrelia burgdorferi*.
*Tick*
- The **tick** (specifically *Ixodes scapularis* or **deer tick**) is the **vector** that transmits *Borrelia burgdorferi* to humans, not the natural reservoir.
- The tick acquires the bacteria from infected animal hosts such as mice and deer.
*Flea*
- **Fleas** are vectors for diseases such as **bubonic plague** (*Yersinia pestis*) and **endemic typhus** (*Rickettsia typhi*), which do not manifest with erythema migrans.
- They are not involved in the transmission or natural history of **Lyme disease**.
Spirochetes overview US Medical PG Question 9: A 29-year-old man comes to the physician because of a 3-day history of a swollen right knee. Over the past several weeks, he has had similar episodes affecting the right knee and sometimes also the left elbow, in which the swelling lasted an average of 5 days. He has a history of a rash that subsided 2 months ago. He lives in Connecticut with his wife and works as a landscaper. His temperature is 37.8°C (100°F), pulse is 90/min, respirations are 12/min, and blood pressure is 110/75 mm Hg. Physical examination shows a tender and warm right knee; range of motion is limited by pain. The remainder of the examination shows no abnormalities. His hematocrit is 44%, leukocyte count is 10,300/mm3, and platelet count is 145,000/mm3. Serum electrolyte concentrations are within normal limits. Arthrocentesis is performed and the synovial fluid is cloudy. Gram stain is negative. Analysis of the synovial fluid shows a leukocyte count of 70,000/mm3 and 80% neutrophils. Serologic testing confirms the diagnosis. Which of the following is the most likely cause?
- A. Rheumatoid arthritis
- B. Neisseria gonorrhoeae
- C. Borrelia burgdorferi (Correct Answer)
- D. Campylobacter jejuni
- E. Osteoarthritis
Spirochetes overview Explanation: ***Borrelia burgdorferi***
- The patient's **migratory polyarthritis** (affecting knee and elbow intermittently), history of a **rash** (consistent with erythema migrans), and residence in an **endemic area** (Connecticut) strongly suggest **Lyme disease**.
- **Synovial fluid analysis** showing high leukocyte count with neutrophilic predominance is typical of inflammatory arthritis, including Lyme arthritis, and **serologic testing** will confirm the presence of *Borrelia burgdorferi* antibodies.
*Rheumatoid arthritis*
- While rheumatoid arthritis causes inflammatory polyarthritis, it typically presents with **symmetrical joint involvement**, morning stiffness, and often involves smaller joints first, which is not described.
- The presence of a preceding **rash** and resolution within weeks is not characteristic of rheumatoid arthritis.
*Neisseria gonorrhoeae*
- **Disseminated gonococcal infection** can cause migratory polyarthralgia or septic arthritis, but it is typically associated with a history of recent unprotected sexual activity and often with tenosynovitis or dermatitis (pustular or vesicular lesions).
- While gram stain is negative in this case, gonococcal arthritis usually has a more rapid onset and systemic symptoms.
*Campylobacter jejuni*
- *Campylobacter jejuni* is a common cause of **reactive arthritis**, which can cause inflammatory joint pain after a gastrointestinal infection.
- However, reactive arthritis typically involves the **lower extremities** and has a specific pattern of oligoarthritis, often with enthesitis or dactylitis, and the preceding rash and geographical factors do not fit.
*Osteoarthritis*
- Osteoarthritis is a **degenerative joint disease** characterized by pain that worsens with activity and improves with rest, and typically affects older individuals.
- It does not present with a preceding **rash**, migratory inflammatory episodes, or a highly inflammatory synovial fluid (high leukocyte count with neutrophilic predominance).
Spirochetes overview US Medical PG Question 10: A 26-year-old man with HIV and a recent CD4+ count of 800 presents to his PCP with fever, cough, and dyspnea. He notes that he recently lost his job as a construction worker and has not been able to afford his HAART medication. His temperature is 102.6°F (39.2°C), pulse is 75/min, respirations are 24/min, and blood pressure is 135/92 mmHg. Physical exam reveals a tachypneic patient with scattered crackles in both lungs, and labs show a CD4+ count of 145 and an elevated LDH. The chest radiography is notable for bilateral diffuse interstitial infiltrates. For definitive diagnosis, the physician obtains a sputum sample. Which stain should he use to visualize the most likely responsible organism?
- A. Periodic acid schiff stain
- B. Silver stain (Correct Answer)
- C. Ziehl-Neelsen stain
- D. India ink stain
- E. Carbol fuchsin stain
Spirochetes overview Explanation: ***Silver stain***
- The patient's presentation with **fever, cough, dyspnea, bilateral diffuse interstitial infiltrates**, and a **CD4+ count of 145** (indicating severe immunosuppression) is highly suggestive of ***Pneumocystis jirovecii*** **pneumonia (PCP)**, formerly known as ***Pneumocystis carinii***.
- ***Pneumocystis jirovecii*** **cysts** and **trophozoites** are best visualized using **silver-based stains** (e.g., Gomori methenamine silver stain) which stain the fungal cell walls dark brown or black.
*Periodic acid schiff stain*
- **PAS stain** is used to identify **glycogen, mucus, and fungal elements** like those of *Candida* or *Aspergillus*, by staining polysaccharides a magenta color.
- While it can stain some fungal organisms, it is **not the primary or most effective stain** for *Pneumocystis jirovecii*.
*Ziehl-Neelsen stain*
- The **Ziehl-Neelsen stain** (also known as acid-fast stain) is used to identify **acid-fast bacilli**, such as *Mycobacterium tuberculosis* or *Nocardia*.
- Although **tuberculosis** is common in HIV patients, the clinical presentation and CXR findings (diffuse interstitial infiltrates rather than cavitary lesions or granulomas) **do not strongly suggest tuberculosis** as the primary diagnosis here.
*India ink stain*
- The **India ink stain** is primarily used to visualize the **capsule of *Cryptococcus neoformans*** in cerebrospinal fluid or other body fluids, appearing as a halo around the yeast cells.
- This patient's symptoms are respiratory, and the likely pathogen is *Pneumocystis*, making India ink stain **inappropriate** for this suspected diagnosis.
*Carbol fuchsin stain*
- **Carbol fuchsin stain** is a component of the **acid-fast staining** procedure (like Ziehl-Neelsen), used as the primary stain to identify acid-fast organisms.
- As with Ziehl-Neelsen, this stain is for **mycobacteria** and would **not effectively visualize** ***Pneumocystis jirovecii***.
More Spirochetes overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.