Mycoplasma pneumoniae US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mycoplasma pneumoniae. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
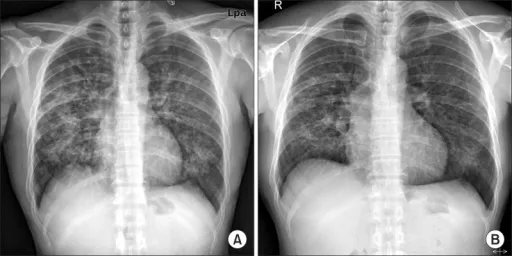
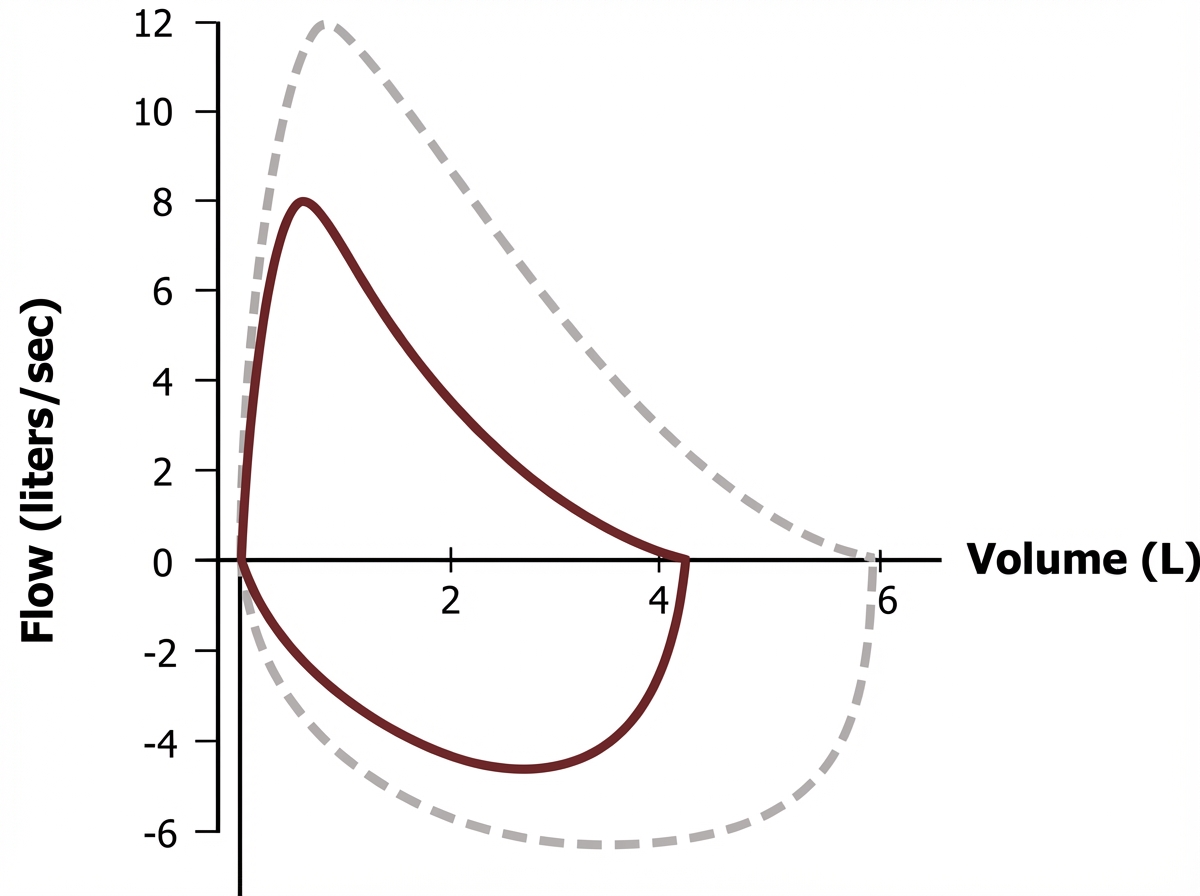
Mycoplasma pneumoniae US Medical PG Question 1: A 47-year-old woman comes to the physician because of a 3-week history of a dry cough. She does not smoke or use illicit drugs. Physical examination shows mild conjunctival hyperemia. Chest auscultation shows fine crackles in both lung fields. Laboratory studies show a total calcium concentration of 10.8 mg/dL. The results of spirometry are shown (dashed loop shows normal for comparison). Further evaluation of this patient is most likely to show an increase in which of the following?
- A. Mast cell tryptase activity
- B. Monoclonal IgG titers
- C. Angiotensin-converting enzyme activity (Correct Answer)
- D. Cold agglutinin titers
- E. Neutrophil elastase activity
Mycoplasma pneumoniae Explanation: ***Angiotensin-converting enzyme activity***
- The patient's symptoms (dry cough, crackles, hypercalcemia, conjunctival hyperemia, and restrictive spirometry pattern based on the image description) are classic for **sarcoidosis**.
- **Elevated ACE levels** are a common finding (seen in 60-80% of cases) in sarcoidosis, as the granulomas produce ACE.
*Mast cell tryptase activity*
- This is primarily elevated in **mastocytosis** and severe allergic reactions like **anaphylaxis**.
- The patient's presentation is not consistent with these conditions.
*Monoclonal IgG titers*
- Elevated monoclonal IgG titers are characteristic of **multiple myeloma** or other monoclonal gammopathies.
- While hypercalcemia can occur in multiple myeloma, the pulmonary findings and conjunctival hyperemia point away from this diagnosis.
*Cold agglutinin titers*
- Elevated cold agglutinin titers are associated with infections like **Mycoplasma pneumoniae** or **Epstein-Barr virus**, lymphomas, and some autoimmune diseases.
- The clinical picture (chronic cough, hypercalcemia, conjunctivitis, restrictive lung disease) is not typical for conditions causing cold agglutinins.
*Neutrophil elastase activity*
- Increased neutrophil elastase activity is primarily associated with conditions involving significant **neutrophilic inflammation**, such as **cystic fibrosis** or severe **COPD exacerbations**.
- The patient's presentation does not suggest such a condition; sarcoidosis is characterized by granulomatous inflammation.
Mycoplasma pneumoniae US Medical PG Question 2: A 10-year-old child presents to your office with a chronic cough. His mother states that he has had a cough for the past two weeks that is non-productive along with low fevers of 100.5 F as measured by an oral thermometer. The mother denies any other medical history and states that he has been around one other friend who also has had this cough for many weeks. The patient's vitals are within normal limits with the exception of his temperature of 100.7 F. His chest radiograph demonstrated diffuse interstitial infiltrates. Which organism is most likely causing his pneumonia?
- A. Mycoplasma pneumoniae (Correct Answer)
- B. Streptococcus agalactiae
- C. Staphylococcus aureus
- D. Pneumocystis jiroveci
- E. Streptococcus pneumoniae
Mycoplasma pneumoniae Explanation: ***Mycoplasma pneumoniae***
- This presentation of a **subacute onset** of a **non-productive cough** with **low-grade fevers** and **diffuse interstitial infiltrates** on chest X-ray in a school-aged child is highly characteristic of **atypical pneumonia** caused by *Mycoplasma pneumoniae*.
- The history of exposure to an infected friend further supports community spread of this organism, which commonly causes outbreaks of "walking pneumonia."
*Streptococcus agalactiae*
- This organism primarily causes infections in **neonates** (Group B Strep) and pregnant women, such as **sepsis** and **meningitis**, and is not a common cause of pneumonia in a 10-year-old.
- Pulmonary infections in older children due to *S. agalactiae* are rare and typically occur in those with significant comorbidities.
*Staphylococcus aureus*
- Pneumonia due to *Staphylococcus aureus* often presents with a more **acute and severe course**, including high fevers, productive cough, and sometimes **abscess formation** or **empyema** on imaging.
- It's commonly associated with preceding influenza infection, intravenous drug use, or hospitalization, none of which are described.
*Pneumocystis jiroveci*
- *Pneumocystis jiroveci* pneumonia (PJP) is almost exclusively seen in **immunocompromised individuals**, such as those with HIV/AIDS, organ transplant recipients, or those on immunosuppressive medications.
- The patient described is a healthy 10-year-old child with no history of immunosuppression.
*Streptococcus pneumoniae*
- **Pneumococcal pneumonia** typically presents with a **sudden onset** of high fever, **productive cough** with rusty sputum, and a more localized lobar infiltrate on chest X-ray.
- While common in children, the subacute, non-productive nature of the cough and the diffuse interstitial infiltrates are not typical for *S. pneumoniae*.
Mycoplasma pneumoniae US Medical PG Question 3: A 51-year-old man comes to the physician because of a 4-day history of fever and cough productive of foul-smelling, dark red, gelatinous sputum. He has smoked 1 pack of cigarettes daily for 30 years and drinks two 12-oz bottles of beer daily. An x-ray of the chest shows a cavity with air-fluid levels in the right lower lobe. Sputum culture grows gram-negative rods. Which of the following virulence factors is most likely involved in the pathogenesis of this patient's condition?
- A. IgA protease
- B. Exotoxin A
- C. Capsular polysaccharide (Correct Answer)
- D. P-fimbriae
- E. Heat-stable toxin
Mycoplasma pneumoniae Explanation: ***Capsular polysaccharide***
- The patient's symptoms (fever, foul-smelling sputum, cavitation with air-fluid levels) and risk factors (smoking) suggest a **lung abscess** likely caused by **_Klebsiella pneumoniae_**.
- **Capsular polysaccharide** is a major virulence factor for _Klebsiella pneumoniae_, providing resistance to phagocytosis and contributing to its invasive potential.
*IgA protease*
- **IgA protease** is a virulence factor produced by bacteria such as _Neisseria gonorrhoeae_, _Neisseria meningitidis_, and _Haemophilus influenzae_ to cleave IgA antibodies.
- While important for mucosal infections, it is not characteristic of the severe lung pathology described, nor a primary virulence factor for a gram-negative rod causing lung abscesses like _Klebsiella_.
*Exotoxin A*
- **Exotoxin A** is a potent exotoxin produced by _Pseudomonas aeruginosa_, which inhibits protein synthesis by ADP-ribosylation of elongation factor 2.
- While _Pseudomonas_ can cause lung infections in compromised patients, the classic description of dark red, gelatinous sputum and the strong association with gram-negative rods causing lung abscesses points more directly to _Klebsiella_.
*P-fimbriae*
- **P-fimbriae** (pyelonephritis-associated fimbriae) are adhesion factors found on uropathogenic _E. coli_, enabling them to bind to uroepithelial cells and cause urinary tract infections.
- These fimbriae are not relevant to the pathogenesis of a lung abscess caused by gram-negative rods in this clinical context.
*Heat-stable toxin*
- **Heat-stable toxin** is typically associated with enterotoxigenic _E. coli_ (ETEC), causing watery diarrhea by activating guanylate cyclase.
- This toxin is involved in gastrointestinal infections and has no role in the pathogenesis of a lung abscess.
Mycoplasma pneumoniae US Medical PG Question 4: An investigator is studying the genetic profile of an isolated pathogen that proliferates within macrophages. The pathogen contains sulfatide on the surface of its cell wall to prevent fusion of the phagosome and lysosome. She finds that some of the organisms under investigation have mutations in a gene that encodes the enzyme required for synthesis of RNA from a DNA template. The mutations are most likely to reduce the therapeutic effect of which of the following drugs?
- A. Pyrazinamide
- B. Ethambutol
- C. Rifampin (Correct Answer)
- D. Streptomycin
- E. Levofloxacin
Mycoplasma pneumoniae Explanation: ***Rifampin***
- **Rifampin** specifically targets bacterial **DNA-dependent RNA polymerase**, inhibiting **RNA synthesis**. Mutations in the gene encoding this enzyme would directly reduce rifampin's binding and effectiveness.
- The description of the pathogen thriving within macrophages and using **sulfatide to evade lysosomal fusion** strongly suggests **Mycobacterium tuberculosis**, a bacterium for which rifampin is a cornerstone treatment.
*Pyrazinamide*
- **Pyrazinamide** is a prodrug that, once converted to **pyrazinoid acid**, disrupts **mycobacterial membrane potential** and metabolism. Its primary target is not RNA synthesis.
- Its efficacy is pH-dependent and it acts optimally in acidic environments, such as within macrophages, but mutations affecting RNA synthesis would not directly compromise its action.
*Ethambutol*
- **Ethambutol** inhibits **arabinosyl transferase**, an enzyme essential for the synthesis of the **mycobacterial cell wall component arabinogalactan**.
- Its mechanism of action is distinct from RNA synthesis, thus mutations affecting RNA polymerase would not impact its efficacy.
*Streptomycin*
- **Streptomycin** is an **aminoglycoside antibiotic** that binds to the **30S ribosomal subunit**, inhibiting bacterial **protein synthesis**.
- This mechanism is unrelated to DNA-dependent RNA polymerase, so mutations in RNA synthesis enzymes would not affect streptomycin's action.
*Levofloxacin*
- **Levofloxacin** is a **fluoroquinolone antibiotic** that inhibits **bacterial DNA gyrase (topoisomerase II)** and **topoisomerase IV**, thereby blocking DNA replication and transcription.
- While it affects processes related to DNA, its direct target is not the DNA-dependent RNA polymerase enzyme itself, distinguishing it from rifampin's specific mechanism.
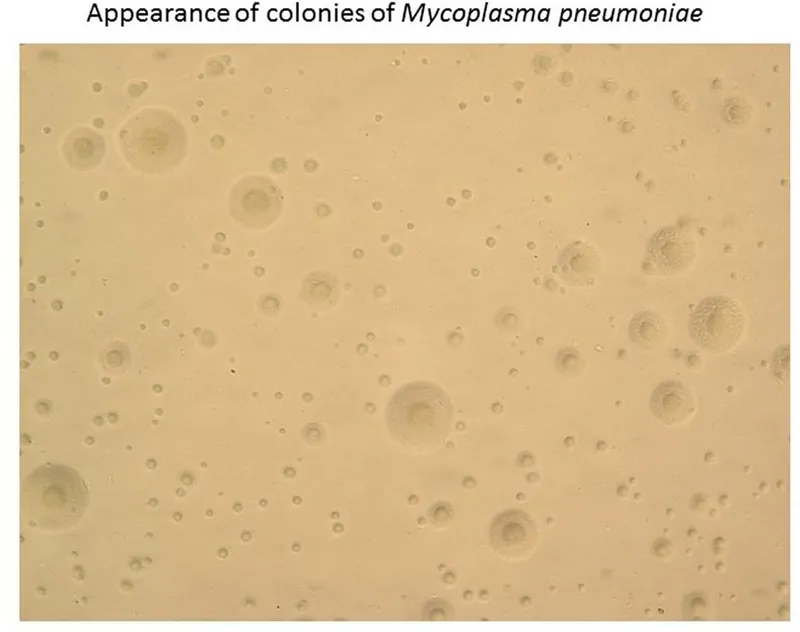
Mycoplasma pneumoniae US Medical PG Question 5: A typically healthy 27-year-old woman presents to the physician because of a 3-week history of fatigue, headache, and dry cough. She does not smoke or use illicit drugs. Her temperature is 37.8°C (100.0°F). Chest examination shows mild inspiratory crackles in both lung fields. An X-ray of the chest shows diffuse interstitial infiltrates bilaterally. A Gram stain of saline-induced sputum shows no organisms. Inoculation of the induced sputum on a cell-free medium that is enriched with yeast extract, horse serum, cholesterol, and penicillin G grows colonies that resemble fried eggs. Which of the following is the most appropriate next step in management?
- A. Oral amoxicillin
- B. Intravenous clindamycin
- C. Oral azithromycin (Correct Answer)
- D. Intravenous ceftriaxone and oral azithromycin
- E. Intravenous ceftriaxone
Mycoplasma pneumoniae Explanation: **Oral azithromycin**
- The patient's symptoms (fatigue, headache, dry cough, bilateral interstitial infiltrates) are consistent with **atypical pneumonia**, likely caused by *Mycoplasma pneumoniae*.
- The **fried egg colonies** on specialized media are characteristic of *Mycoplasma pneumoniae*, and macrolides such as **azithromycin** are the first-line treatment for this infection.
*Oral amoxicillin*
- **Amoxicillin** is a beta-lactam antibiotic that targets bacterial cell walls, which are **lacking in *Mycoplasma***.
- Therefore, amoxicillin would be **ineffective** against *Mycoplasma pneumoniae* infections.
*Intravenous clindamycin*
- **Clindamycin** is primarily used for anaerobic infections and some gram-positive bacteria; it is **not active against *Mycoplasma pneumoniae***.
- This antibiotic would not be an appropriate choice for atypical pneumonia.
*Intravenous ceftriaxone and oral azithromycin*
- While **azithromycin** is appropriate, **intravenous ceftriaxone** (a cephalosporin) is primarily used for typical bacterial pneumonia.
- Adding ceftriaxone is **unnecessary** and broad-spectrum for this clear case of *Mycoplasma pneumoniae* pneumonia, and the patient does not appear severely ill to warrant IV therapy.
*Intravenous ceftriaxone*
- **Ceftriaxone** targets bacterial cell walls and would be **ineffective against *Mycoplasma pneumoniae*** due to its lack of a cell wall.
- It is typically used for more severe or typical bacterial pneumonias, particularly when there is concern for *Streptococcus pneumoniae* or *Haemophilus influenzae*.
Mycoplasma pneumoniae US Medical PG Question 6: A 19-year-old college student presents to student health with 1 day of fever and chills. He says that he has also been coughing for 2 days. His roommate was sick 3 days ago with similar symptoms and was diagnosed with Mycoplasma infection. He has otherwise been healthy and has had all the required vaccines as scheduled. He is currently taking introductory biology as part of his premedical studies and recently learned about antibodies. He therefore asks his physician about what his body is doing to fight off the infection. At this stage of his infection, which of the following forms are the antibodies circulating in his serum?
- A. Pentamers (Correct Answer)
- B. Dimers
- C. Tetramers
- D. Trimers
- E. Monomers
Mycoplasma pneumoniae Explanation: ***Pentamers***
- In the **early stages** of a primary immune response, the B cells initially produce **IgM antibodies**.
- IgM antibodies circulate in the serum primarily as **pentamers**, making them highly effective at binding multiple antigens and activating complement.
*Dimers*
- **IgA antibodies** can exist as dimers, particularly secretory IgA found in mucosal secretions, but they are not the predominant form during the initial systemic immune response to an infection.
- While IgA plays a role in immunity, IgM is the primary antibody class produced in the **first few days of a new infection**.
*Tetramers*
- Antibodies typically do not form **stable tetrameric structures** as a functional unit in serum.
- The primary forms of antibodies are monomers, dimers, and pentamers, each with specific roles and locations.
*Trimers*
- **Trimeric antibody forms** are not a standard or significant configuration for immunoglobulins circulating in the serum.
- Antibody structures are well-defined as monomers (IgG, IgE, IgD), dimers (secretory IgA), or pentamers (IgM).
*Monomers*
- While **IgM can exist as a monomer** when expressed on the surface of B cells, serum IgM is predominantly in its **pentameric form**.
- **IgG** is the most abundant monomeric antibody in serum, but it is produced later in the immune response and at higher concentrations during secondary immune responses.
Mycoplasma pneumoniae US Medical PG Question 7: An investigator is studying a strain of bacteria that retains a blue color after crystal violet dye and acetone are applied. The bacteria are inoculated in a petri dish containing hypotonic saline. After the addition of an antibiotic, the bacteria swell and rupture. This antibiotic most likely belongs to which of the following classes?
- A. Macrolide
- B. Cephalosporin (Correct Answer)
- C. Sulfonamide
- D. Fluoroquinolone
- E. Tetracycline
Mycoplasma pneumoniae Explanation: ***Cephalosporin***
- This scenario describes a **Gram-positive bacterium** (retains blue color) which, after antibiotic treatment, swells and lyses in a hypotonic solution. This indicates a defect in the **peptidoglycan cell wall**.
- **Cephalosporins** are **β-lactam antibiotics** that inhibit bacterial cell wall synthesis by interfering with **peptidoglycan cross-linking**, leading to osmotic lysis in hypotonic environments.
*Macrolide*
- Macrolides like **azithromycin** and **erythromycin** inhibit bacterial **protein synthesis** by binding to the 50S ribosomal subunit.
- They do not directly target the cell wall, so they would not cause immediate osmotic lysis in this manner.
*Sulfonamide*
- Sulfonamides inhibit bacterial **folic acid synthesis** by acting as a competitive inhibitor of dihydropteroate synthase, disrupting DNA and RNA production.
- Their mechanism of action does not involve direct cell wall disruption or osmotic lysis.
*Fluoroquinolone*
- Fluoroquinolones interfere with bacterial **DNA replication and transcription** by inhibiting **DNA gyrase** and **topoisomerase IV**.
- This class of antibiotics does not primarily target the cell wall, and therefore would not lead to prompt osmotic swelling and rupture.
*Tetracycline*
- Tetracyclines inhibit bacterial **protein synthesis** by binding to the 30S ribosomal subunit, preventing the attachment of aminoacyl-tRNA.
- They do not affect the cell wall, so they would not cause the observed osmotic lysis.
Mycoplasma pneumoniae US Medical PG Question 8: A 43-year-old woman comes to the physician because of a fever, nausea, and a nonproductive cough for 7 days. During this period, she has had headaches, generalized fatigue, and muscle and joint pain. She has also had increasing shortness of breath for 2 days. She has type 2 diabetes mellitus and osteoarthritis of her left knee. Current medications include insulin and ibuprofen. She had smoked two packs of cigarettes daily for 20 years but stopped 10 years ago. Her temperature is 38.1°C (100.6°F), pulse is 94/min, respirations are 18/min, and blood pressure is 132/86 mm Hg. The lungs are clear to auscultation. There are multiple skin lesions with a blue livid center, pale intermediate zone, and a dark red peripheral rim on the upper and lower extremities. Laboratory studies show:
Hemoglobin 14.6 g/dL
Leukocyte count 11,100/mm3
Serum
Na+ 137 mEq/L
K+ 4.1 mEq/L
Cl- 99 mEq/L
Urea nitrogen 17 mg/dL
Glucose 123 mg/dL
Creatinine 0.9 mg/dL
Which of the following is the most likely causal organism?
- A. Legionella pneumophila
- B. Mycoplasma pneumoniae (Correct Answer)
- C. Haemophilus influenzae
- D. Klebsiella pneumoniae
- E. Staphylococcus aureus
Mycoplasma pneumoniae Explanation: ***Mycoplasma pneumoniae***
- The patient presents with a **nonproductive cough**, **headache**, **fatigue**, **myalgia**, and **arthralgia**, which are classic symptoms of **atypical pneumonia**. The presence of **erythema multiforme** (skin lesions with a blue livid center, pale intermediate zone, and dark red peripheral rim) is also strongly associated with *Mycoplasma pneumoniae* infection.
- While the chest X-ray specifically mentioned is not provided, atypical pneumonias often show **patchy infiltrates** that are out of proportion to the patient's symptoms (walking pneumonia), and the constellation of symptoms strongly points towards *Mycoplasma pneumoniae*.
*Legionella pneumophila*
- While *Legionella* can cause **atypical pneumonia** with gastrointestinal symptoms (**nausea** in this case) and hyponatremia, the prominent skin rash (erythema multiforme) is not a typical feature.
- **Hyponatremia** and **confusion** are more commonly associated with *Legionella*, neither of which are prominent findings here.
*Haemophilus influenzae*
- This typically causes **bacterial pneumonia** with more pronounced purulent sputum and lung consolidation, which is not suggested by the nonproductive cough and clear auscultation.
- While *Haemophilus influenzae* can cause respiratory infections, it is less likely to present with the systemic symptoms and characteristic rash seen in this patient.
*Klebsiella pneumoniae*
- Characteristically causes severe, **lobar pneumonia**, often seen in alcoholics and individuals with chronic lung disease, and is associated with **"currant jelly" sputum**.
- The patient's symptoms (nonproductive cough, systemic symptoms, rash) and the description of the lung auscultation (clear) do not align with a typical *Klebsiella pneumoniae* infection.
*Staphylococcus aureus*
- Can cause severe **necrotizing pneumonia**, often following a viral illness (e.g., influenza), and is associated with multiple cavitations and abscesses on chest imaging.
- While there is a history of smoking, the presentation with diffuse systemic symptoms and erythema multiforme is not typical for **staphylococcal pneumonia**.
Mycoplasma pneumoniae US Medical PG Question 9: A previously healthy 27-year-old woman comes to the physician because of a 3-week history of fatigue, headache, and dry cough. She does not smoke or use illicit drugs. Her temperature is 37.8°C (100°F). Chest examination shows mild inspiratory crackles in both lung fields. An x-ray of the chest shows diffuse interstitial infiltrates bilaterally. A Gram stain of saline-induced sputum shows no organisms. Inoculation of the induced sputum on a cell-free medium that is enriched with yeast extract, horse serum, cholesterol, and penicillin G grows colonies that resemble fried eggs. Which of the following organisms was most likely isolated on the culture medium?
- A. Bordetella pertussis
- B. Haemophilus influenzae
- C. Cryptococcus neoformans
- D. Mycoplasma pneumoniae (Correct Answer)
- E. Coxiella burnetii
Mycoplasma pneumoniae Explanation: ***Mycoplasma pneumoniae***
- The patient's presentation with **atypical pneumonia** symptoms (fatigue, headache, dry cough, diffuse interstitial infiltrates) along with the characteristic **"fried egg" colonies** cultured on a specialized medium (enriched with yeast extract, horse serum, cholesterol, and penicillin G) are highly indicative of *Mycoplasma pneumoniae*.
- Unlike most bacteria, *Mycoplasma pneumoniae* lacks a **cell wall**, explaining why it does not stain on Gram stain and requires specific culture conditions.
*Bordetella pertussis*
- This organism causes **whooping cough** and is characterized by distinct paroxysmal cough followed by an inspiratory 'whoop,' not typically the diffuse interstitial infiltrates and mild crackles described.
- *Bordetella pertussis* is usually cultured on **Bordet-Gengou agar** or Regan-Lowe medium, not the specialized medium described, and does not form "fried egg" colonies.
*Haemophilus influenzae*
- This bacterium is a common cause of **bacterial pneumonia** but typically presents with more acute symptoms and localized infiltrates, often seen in individuals with underlying lung disease or in children.
- *Haemophilus influenzae* would grow on standard chocolate agar and would not produce "fried egg" colonies; it also stains Gram-negative coccobacilli.
*Cryptococcus neoformans*
- This is a **fungus**, not a bacterium, and is a significant cause of pneumonia and meningoencephalitis, especially in immunocompromised individuals.
- Its presence would typically be identified by **India ink stain** (showing encapsulated yeast) or specific fungal cultures, not the described "fried egg" appearance on bacterial media.
*Coxiella burnetii*
- This intracellular bacterium causes **Q fever**, which can present with atypical pneumonia symptoms, but it is an **obligate intracellular parasite** and therefore cannot be grown on cell-free artificial media like the one described.
- Diagnosis typically relies on **serological tests** or PCR, as it cannot be easily cultured in a standard lab setup.
Mycoplasma pneumoniae US Medical PG Question 10: A 23-year-old male comes to the physician because of a 2-week history of fatigue, muscle aches, and a dry cough. He has also had episodes of painful, bluish discoloration of the tips of his fingers, nose, and earlobes during this period. Three months ago, he joined the military and attended basic training in southern California. He does not smoke or use illicit drugs. His temperature is 37.8°C (100°F). Physical examination shows mildly pale conjunctivae and annular erythematous lesions with a dusky central area on the extensor surfaces of the lower extremities. Which of the following is the most likely causal organism?
- A. Chlamydophila pneumoniae
- B. Streptococcus pneumoniae
- C. Mycoplasma pneumoniae (Correct Answer)
- D. Adenovirus
- E. Influenza virus
Mycoplasma pneumoniae Explanation: ***Mycoplasma pneumoniae***
- This patient's symptoms (fatigue, muscle aches, dry cough, slightly elevated temperature, and **erythema multiforme**-like lesions) are characteristic of **atypical pneumonia**. The **Raynaud-like phenomenon** (bluish discoloration of fingertips, nose, earlobes) and recent military basic training environment are highly suggestive of *Mycoplasma pneumoniae* infection.
- *Mycoplasma pneumoniae* is a common cause of **atypical pneumonia**, especially in crowded settings like military barracks, and is associated with extrapulmonary manifestations such as **Raynaud's phenomenon**, **hemolytic anemia** (suggested by pale conjunctivae), and **erythema multiforme**.
*Chlamydophila pneumoniae*
- This organism also causes **atypical pneumonia** with a dry cough and constitutional symptoms but is less commonly associated with the prominent extrapulmonary findings like **Raynaud's phenomenon** and **erythema multiforme** seen in this patient.
- While it can cause pharyngitis and hoarseness, the constellation of symptoms, particularly the cutaneous and vascular manifestations, points away from *Chlamydophila pneumoniae*.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* typically causes **typical bacterial pneumonia**, characterized by a **productive cough**, high fever, chills, and often **lobar consolidation** on chest X-ray.
- It is not associated with **Raynaud's phenomenon**, **erythema multiforme**, or the specific demographic and exposure history (military basic training for atypical presentation) described.
*Adenovirus*
- **Adenovirus** can cause **respiratory tract infections**, including pharyngitis, conjunctivitis, and pneumonia, often seen in outbreaks in crowded settings.
- However, it is less commonly associated with the dramatic extrapulmonary manifestations like **Raynaud's phenomenon** and **erythema multiforme** that are prominent in this case.
*Influenza virus*
- **Influenza virus** causes a **respiratory illness** with fever, myalgia, fatigue, and cough, but **dry cough** is more common.
- While it can lead to pneumonia, the presence of **Raynaud's phenomenon** and **erythema multiforme** is not a typical presentation of influenza.
More Mycoplasma pneumoniae US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.