Mycobacteria overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mycobacteria overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
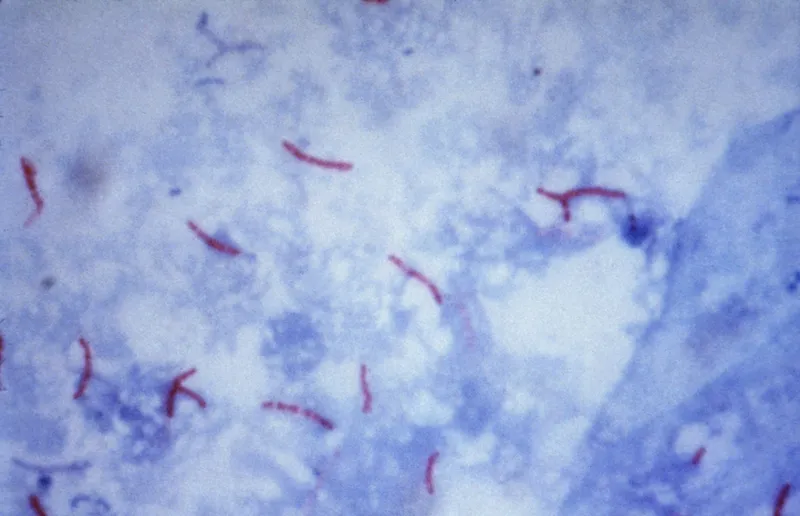
Mycobacteria overview US Medical PG Question 1: A medical technician is trying to isolate a pathogen from the sputum sample of a patient. The sample is heat fixed to a slide then covered with carbol fuchsin stain and heated again. After washing off the stain with clean water, the slide is covered with 1% sulfuric acid for decolorization. The sample is rinsed again and stained with methylene blue. Microscopic examination shows numerous red, branching filamentous organisms. Which of the following is the most likely isolated pathogen?
- A. Cryptococcus neoformans
- B. Tropheryma whipplei
- C. Nocardia asteroides (Correct Answer)
- D. Rickettsia rickettsii
- E. Staphylococcus aureus
Mycobacteria overview Explanation: ***Nocardia asteroides***
- The described staining procedure is a **modified acid-fast stain**, indicated by the use of **carbol fuchsin**, heating, and decolorization with **weak acid (1% sulfuric acid)**, followed by a counterstain with methylene blue.
- **Nocardia species** are **weakly acid-fast bacteria** that resist decolorization with weak acids (1-3% sulfuric acid), appearing as **red, branching filamentous organisms** under this staining method.
- The **modified acid-fast stain** uses weaker decolorizing agents compared to the standard Ziehl-Neelsen stain, making it suitable for detecting weakly acid-fast organisms like Nocardia.
- Nocardia are aerobic actinomycetes commonly found in soil and can cause pulmonary infections, especially in immunocompromised patients.
*Cryptococcus neoformans*
- This is a **yeast** that is typically identified using an **India ink stain** to visualize its polysaccharide capsule, or through fungal stains like Gomori methenamine silver (GMS).
- It would not appear as acid-fast red branching filaments with the described technique.
*Tropheryma whipplei*
- This bacterium is typically identified by **periodic acid-Schiff (PAS) stain** in tissue biopsies, which highlights its cell wall glycoproteins (appears magenta).
- It is not acid-fast and would not retain the carbol fuchsin after acid decolorization.
*Rickettsia rickettsii*
- This is an **obligate intracellular bacterium** that is difficult to culture and is often diagnosed by **serological tests** or **immunohistochemistry** on skin biopsy specimens.
- It is not acid-fast and would not be detected by this staining technique.
*Staphylococcus aureus*
- This is a **Gram-positive coccus** that would be stained **purple** by a Gram stain as it retains crystal violet.
- It is not acid-fast and would be completely decolorized by sulfuric acid in the described procedure, appearing blue (counterstain color) rather than red.
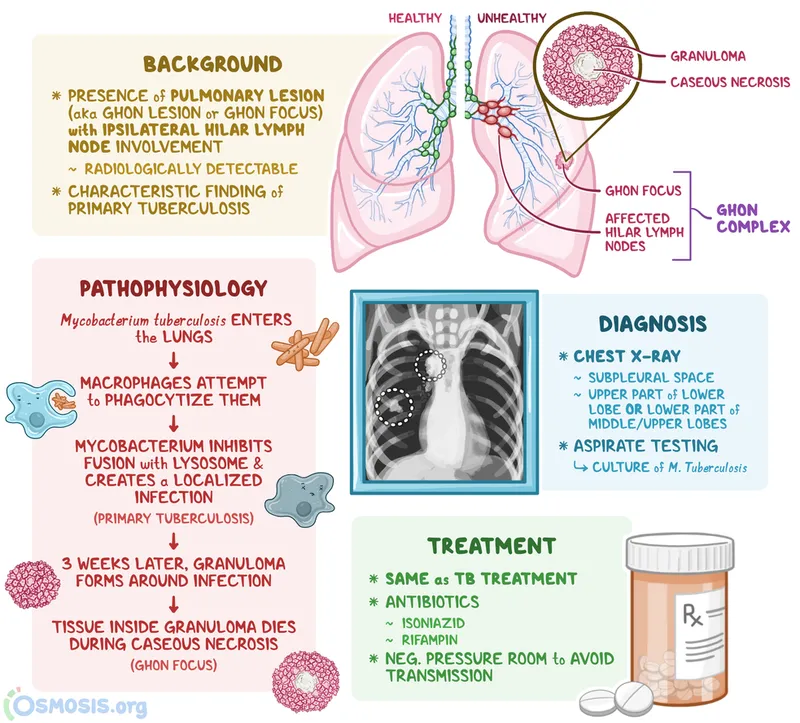
Mycobacteria overview US Medical PG Question 2: A 28-year-old woman comes to the physician because of a two-month history of fatigue and low-grade fevers. Over the past 4 weeks, she has had increasing shortness of breath, a productive cough, and a 5.4-kg (11.9-lb) weight loss. Three months ago, the patient returned from a two-month trip to China. The patient appears thin. Her temperature is 37.9°C (100.2°F), pulse is 75/min, and blood pressure is 125/70 mm Hg. Examination shows lymphadenopathy of the anterior and posterior cervical chain. Rales are heard at the left lower lobe of the lung on auscultation. Laboratory studies show a leukocyte count of 11,300/mm3 and an erythrocyte sedimentation rate of 90 mm/h. An x-ray of the chest shows a patchy infiltrate in the left lower lobe and ipsilateral hilar enlargement. Microscopic examination of the sputum reveals acid-fast bacilli; polymerase chain reaction is positive. Sputum cultures are pending. After placing the patient in an airborne infection isolation room, which of the following is the most appropriate next step in management?
- A. Administer only isoniazid for 9 months
- B. Administer isoniazid, rifampin, pyrazinamide, and ethambutol for 2 months, followed by isoniazid and rifampin for 4 months (Correct Answer)
- C. Await culture results before initiating treatment
- D. Obtain CT scan of the chest
- E. Perform interferon-γ release assay
Mycobacteria overview Explanation: ***Administer isoniazid, rifampin, pyrazinamide, and ethambutol for 2 months, followed by isoniazid and rifampin for 4 months***
- This patient presents with symptoms such as **fatigue, fever, weight loss, productive cough, and shortness of breath**, along with **lymphadenopathy, rales, patchy infiltrate, ipsilateral hilar enlargement, and acid-fast bacilli in sputum**, all highly suggestive of active **pulmonary tuberculosis (TB)**.
- Given the strong clinical and microbiological evidence (acid-fast bacilli, positive PCR), immediate initiation of a **four-drug regimen (isoniazid, rifampin, pyrazinamide, ethambutol)** is crucial to prevent disease progression, reduce transmission, and ensure effective treatment.
*Administer only isoniazid for 9 months*
- **Isoniazid monotherapy** is typically used for **latent tuberculosis infection (LTBI)**, not active TB, as it is insufficient to treat active disease and carries a high risk of developing drug resistance.
- The patient's symptoms, imaging findings, and positive acid-fast bacilli smear indicate **active disease**, not just latent infection.
*Await culture results before initiating treatment*
- Delaying treatment for active TB until **culture results** are available (which can take several weeks) is inappropriate and can lead to disease progression, increased morbidity, and higher risk of transmission to others.
- The **acid-fast bacilli smear and PCR positivity** provide sufficient evidence to initiate empiric treatment immediately.
*Obtain CT scan of the chest*
- While a **CT scan** might provide more detailed imaging information, it is not the most immediate next step for management when active TB is strongly suspected and requires urgent treatment initiation.
- The **chest x-ray findings** are already consistent with TB and sufficient to guide initial management.
*Perform interferon-γ release assay*
- An **interferon-γ release assay (IGRA)** is used to diagnose **latent tuberculosis infection (LTBI)**, not active TB, and does not differentiate between the two.
- The patient's presentation with active symptoms, positive sputum smear, and positive PCR strongly indicates **active TB**, rendering an IGRA redundant and not helpful for determining the immediate treatment course.
Mycobacteria overview US Medical PG Question 3: A 32-year-old man comes to the physician because of a 3-week history of cough, weight loss, and night sweats. He migrated from Sri Lanka 6 months ago. He appears emaciated. His temperature is 38.1°C (100.5°F). Physical examination shows enlargement of the right supraclavicular lymph node. Chest and abdominal examination show no abnormalities. An interferon-gamma assay is positive. A biopsy specimen of the cervical lymph node is most likely to show the causal organism in which of the following locations?
- A. Mantle zone
- B. Medullary sinus
- C. Germinal center
- D. Subcapsular sinus
- E. Paracortex (Correct Answer)
Mycobacteria overview Explanation: ***Paracortex***
- The patient's symptoms (cough, weight loss, night sweats, fever), recent migration from an endemic area (Sri Lanka), **supraclavicular lymphadenopathy**, and positive **interferon-gamma release assay (IGRA)** strongly suggest **tuberculosis**.
- In tuberculous lymphadenitis, **caseating granulomas** containing *Mycobacterium tuberculosis* organisms characteristically form in the **paracortex** (T-cell zone).
- The **paracortex** is where **cell-mediated immunity** occurs, with T cells interacting with infected macrophages and dendritic cells to form the **epithelioid granulomas** with **Langhans giant cells** that are pathognomonic for TB.
- The organisms are found within these **granulomas**, which predominantly occur in the paracortical (interfollicular) region.
*Mantle zone*
- The **mantle zone** primarily contains **naïve B cells** surrounding germinal centers.
- This is a B-cell area not typically involved in granuloma formation or mycobacterial infection.
*Germinal center*
- **Germinal centers** are sites of B cell proliferation, somatic hypermutation, and antibody class switching.
- TB is a disease of **cell-mediated immunity** (T cells and macrophages), not humoral immunity, so granulomas do not form in germinal centers.
*Medullary sinus*
- The **medullary sinuses** are channels in the medulla of the lymph node through which lymph flows toward the efferent lymphatic vessels.
- While macrophages line these sinuses and may contain some organisms in acute infections, the characteristic **caseating granulomas** of chronic tuberculous lymphadenitis form in the **paracortex**, not in the sinuses.
*Subcapsular sinus*
- The **subcapsular sinus** is the initial entry point for afferent lymph into the lymph node.
- While this is where pathogens first enter, chronic granulomatous infections like TB develop their characteristic pathology deeper in the node, specifically in the **paracortex** where T-cell-mediated granuloma formation occurs.
Mycobacteria overview US Medical PG Question 4: A 55-year-old woman comes to the physician because of fevers for 2 weeks. She works as a nurse and recently returned from a charity work trip to India, where she worked in a medically-underserved rural community. A tuberculin skin test 3 months ago prior to her trip showed an induration of 3 mm. Physical examination is unremarkable. An x-ray of the chest shows right-sided hilar lymphadenopathy. A sputum culture shows acid-fast bacilli. Which of the following immunologic processes most likely occurred first?
- A. Production of interferon-gamma by T-helper cells
- B. Migration of T-helper cells to the lungs
- C. Replication of bacteria within alveolar macrophages (Correct Answer)
- D. Formation of a nodular tubercle in the lung
- E. Transportation of bacterial peptides to regional lymph nodes
Mycobacteria overview Explanation: ***Replication of bacteria within alveolar macrophages***
- After initial infection, **Mycobacterium tuberculosis** is phagocytosed by **alveolar macrophages** in the lungs, where it **replicates unimpeded** for about 2–4 weeks before the adaptive immune response is fully mounted.
- This phase of unchecked bacterial growth precedes the immune system's attempt to contain the infection, making it the first significant immunologic event.
*Transportation of bacterial peptides to regional lymph nodes*
- This process involves **antigen-presenting cells** (APCs) — typically macrophages or dendritic cells — migrating from the lungs to regional lymph nodes to present bacterial antigens to T cells.
- This step occurs *after* the initial bacterial replication and phagocytosis but *before* a robust T-cell mediated immune response develops, as T-cells need to be activated in the lymph nodes.
*Formation of a nodular tubercle in the lung*
- The **tubercle** (granuloma) is a hallmark of tuberculosis, representing the body's attempt to contain the infection.
- Its formation is a complex process involving activated macrophages, T cells, and fibroblasts, and it occurs *after* the initial bacterial replication and the subsequent immune cell activation and recruitment.
*Migration of T-helper cells to the lungs*
- **T-helper cells** migrate to the lungs only after they have been **activated** in the regional lymph nodes by antigen-presenting cells.
- This migration is crucial for orchestrating the immune response and containing the infection but happens *after* initial bacterial proliferation and antigen presentation.
*Production of interferon-gamma by T-helper cells*
- **Interferon-gamma** (IFN-$\gamma$) is a key cytokine produced by activated T-helper cells (Th1 cells) that activates macrophages to become more effective at killing intracellular bacteria.
- This production signifies a mature adaptive immune response and occurs *after* T-helper cell activation in the lymph nodes and subsequent migration to the infected site.
Mycobacteria overview US Medical PG Question 5: A 55-year-old homeless man is presented to the emergency department by a group of volunteers after they found him coughing up blood during 1 of the beneficiary dinners they offer every week. His medical history is unknown as he recently immigrated from Bangladesh. He says that he has been coughing constantly for the past 3 months with occasional blood in his sputum. He also sweats a lot at nights and for the past 2 days, he has been thirsty with increased frequency of urination and feeling hungrier than usual. The respiratory rate is 30/min and the temperature is 38.6°C (101.5°F). He looks emaciated and has a fruity smell to his breath. The breath sounds are reduced over the apex of the right lung. The remainder of the physical exam is unremarkable. Biochemical tests are ordered, including a hemoglobin A1c (HbA1c) (8.5%) and chest radiography reveals cavitations in the apical region of the right lung. Which of the following immune cells is most critical in orchestrating the formation and maintenance of the granulomatous structure that led to these cavitations?
- A. B lymphocytes
- B. Treg lymphocytes
- C. Epithelioid cells
- D. Th1 lymphocytes (Correct Answer)
- E. Th2 lymphocytes
Mycobacteria overview Explanation: ***Th1 lymphocytes***
- The clinical picture strongly suggests **reactivation of tuberculosis** due to the cavitary lung lesions, constitutional symptoms, and likely immunocompromise from undiagnosed diabetes (HbA1c 8.5%).
- **Th1 lymphocytes** are crucial for the cell-mediated immune response against **intracellular pathogens** like *Mycobacterium tuberculosis*, producing **interferon-gamma** which activates macrophages to form granulomas and contain the infection, thus preventing dissemination and contributing to cavitation.
*B lymphocytes*
- **B lymphocytes** primarily mediate **humoral immunity** by producing antibodies, which are less critical for controlling intracellular bacterial infections like tuberculosis.
- While antibodies can play a role in modulating inflammation, they are not the primary cells involved in the **granuloma formation** and containment of *M. tuberculosis* within the lungs.
*Treg lymphocytes*
- **Treg lymphocytes** (regulatory T cells) primarily function to **suppress immune responses** to prevent autoimmunity and limit tissue damage.
- While they can modulate the immune response in tuberculosis, their main role is not in the initial formation of **cavities** or primary defense against the pathogen, but rather in regulating the overall inflammatory process.
*Epithelioid cells*
- **Epithelioid cells** are **activated macrophages** that form the core of granulomas, but they are not lymphocytes; they are derived from monocytes.
- They are a crucial component of the **granulomatous structure** itself, but their differentiation and activation are largely driven by cytokines produced by **Th1 lymphocytes**.
*Th2 lymphocytes*
- **Th2 lymphocytes** are primarily involved in immunity against **extracellular parasites** and in allergic reactions, mediating humoral responses through cytokines like **IL-4, IL-5, and IL-13**.
- An effective immune response against *Mycobacterium tuberculosis* is dominated by a **Th1 cellular response**, and a prominent Th2 response is generally considered detrimental or insufficient in controlling the infection.
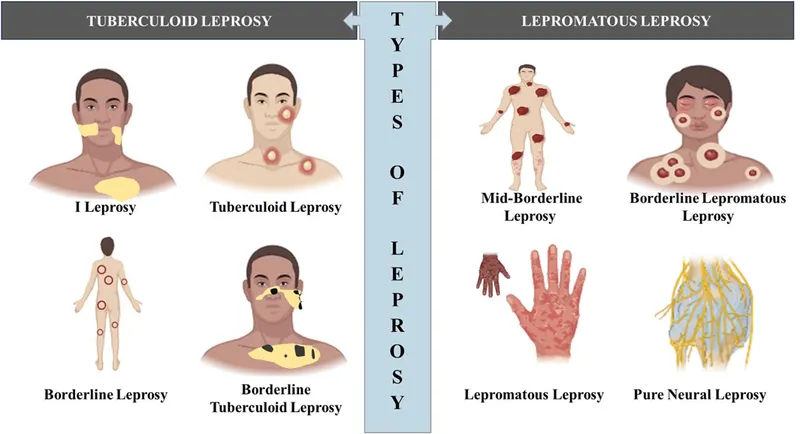
Mycobacteria overview US Medical PG Question 6: A 45-year-old man presents with well-circumscribed, hypopigmented patches on his face and arms. The lesions are asymmetric and show decreased sensation to light touch. Microscopic examination of a skin biopsy stained with Fite stain shows acid-fast bacilli within macrophages in dermal nerve bundles. Which of the following is the most appropriate treatment?
- A. Multidrug therapy with dapsone, rifampin, and clofazimine (Correct Answer)
- B. Topical steroids
- C. Oral terbinafine
- D. Oral acyclovir
- E. Phototherapy
Mycobacteria overview Explanation: ***Multidrug therapy with dapsone, rifampin, and clofazimine***
- The clinical presentation of **hypopigmented patches with decreased sensation**, along with the presence of **acid-fast bacilli (AFB) in dermal nerve bundles** on Fite stain, is characteristic of **leprosy** (Hansen's disease) [1].
- This specific regimen of **dapsone, rifampin, and clofazimine** is the standard and most effective **multidrug therapy (MDT)** for treating **multibacillary leprosy**, ensuring eradication of the pathogen and preventing drug resistance [1].
*Topical steroids*
- **Topical steroids** are primarily used for inflammatory skin conditions like eczema or psoriasis and would not be effective against **bacterial infections** like leprosy [1].
- While steroids might be used as an adjunct to manage **leprosy reactions**, they do not treat the underlying bacterial infection [1].
*Oral terbinafine*
- **Oral terbinafine** is an **antifungal medication** used to treat fungal infections, such as onychomycosis or ringworm.
- It has no activity against the **acid-fast bacillus** responsible for leprosy.
*Oral acyclovir*
- **Oral acyclovir** is an **antiviral medication** used to treat viral infections, particularly those caused by herpesviruses.
- It is completely ineffective against **bacterial infections** like leprosy.
*Phototherapy*
- **Phototherapy**, using ultraviolet light, is a treatment modality for certain skin conditions like psoriasis, vitiligo, or severe eczema.
- It is not an effective treatment for **bacterial infections** and would not address the underlying pathology of leprosy.
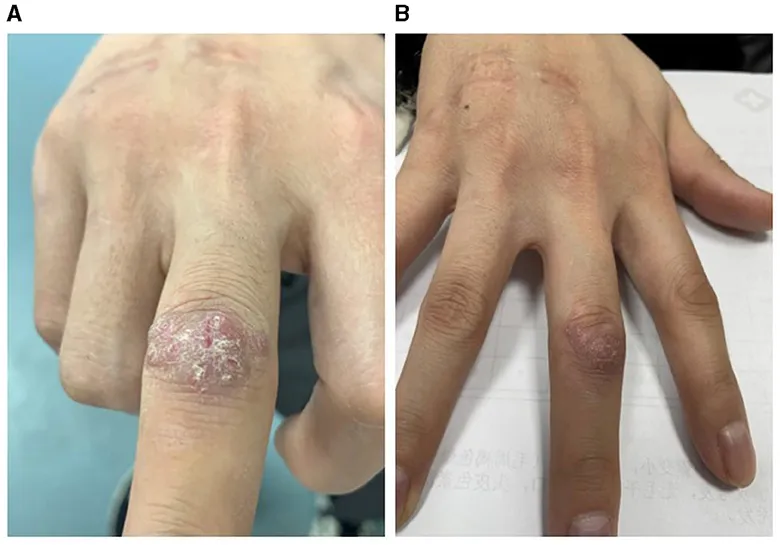
Mycobacteria overview US Medical PG Question 7: A 48-year-old man comes to the physician because of a hypopigmented skin lesion on his finger. He first noticed it 4 weeks ago after cutting his finger with a knife while preparing food. He did not feel the cut. For the past week, he has also had fever, fatigue, and malaise. He has not traveled outside the country since he immigrated from India to join his family in the United States 2 years ago. His temperature is 38.7°C (101.7°F). Physical examination shows a small, healing laceration on the dorsal aspect of the left index finger and an overlying well-defined, hypopigmented macule with raised borders. Sensation to pinprick and light touch is decreased over this area. Which of the following is the most likely causal pathogen of this patient's condition?
- A. Epidermophyton floccosum
- B. Mycobacterium leprae (Correct Answer)
- C. Malassezia furfur
- D. Pseudomonas aeruginosa
- E. Leishmania donovani
Mycobacteria overview Explanation: ***Mycobacterium leprae***
- The patient's history of immigration from **India**, a country endemic for leprosy, coupled with the **hypopigmented, anesthetic skin lesion** with raised borders, is classic for **leprosy** (Hansen's disease).
- The diminished sensation to pinprick and light touch in the affected area points to **nerve involvement**, a hallmark of *Mycobacterium leprae* infection.
*Epidermophyton floccosum*
- This fungus primarily causes **tinea infections** (ringworm), such as athlete's foot and jock itch.
- While it can cause skin lesions, they are typically **erythematous** and scaly, not hypopigmented with sensory loss.
*Malassezia furfur*
- This yeast is responsible for **tinea versicolor**, characterized by **hypopigmented or hyperpigmented patches** that typically scale.
- However, it does not cause **nerve damage** or accompanying sensory loss, and systemic symptoms like fever and malaise are not typical.
*Pseudomonas aeruginosa*
- This bacterium can cause various opportunistic infections, including skin infections like **ecthyma gangrenosum** or **folliculitis** in immunocompromised patients.
- *Pseudomonas* infections are usually painful, often associated with a characteristic **grape-like odor**, and do not typically present with chronic, anesthetic, hypopigmented lesions.
*Leishmania donovani*
- This parasite causes **visceral leishmaniasis** (kala-azar), which presents with fever, weight loss, hepatosplenomegaly, and **hyperpigmentation of the skin** (darkening), not hypopigmentation.
- It does not cause localized anesthetic skin lesions like those described in the patient.
Mycobacteria overview US Medical PG Question 8: A 35-year-old man from Thailand presents with low-grade fever, chronic cough, and night sweats for 3 months. He describes the cough as productive and producing white sputum that is sometimes streaked with blood. He also says he has lost 10 lb in the last 3 months. Past medical history is unremarkable. The patient denies any smoking history, alcohol, or recreational drug use. The vital signs include blood pressure 115/75 mm Hg, heart rate 120/min, respiratory rate 20/min, and temperature 36.6℃ (97.8℉). On physical examination, the patient is ill-looking and thin with no pallor or jaundice. Cardiopulmonary auscultation reveals some fine crackles in the right upper lobe. A chest radiograph reveals a right upper lobe homogeneous density. Which of the following tests would be most helpful in making a definitive diagnosis of active infection in this patient?
- A. PPD test
- B. Silver stain
- C. Ziehl-Neelsen stain (Correct Answer)
- D. Gram stain
- E. Interferon-gamma assay
Mycobacteria overview Explanation: ***Ziehl-Neelsen stain***
- The patient's symptoms (low-grade fever, chronic cough with white/bloody sputum, night sweats, weight loss) and chest X-ray findings (right upper lobe homogeneous density) are highly suggestive of **active tuberculosis (TB)**, especially given his origin from Thailand (a country with a high TB burden).
- The **Ziehl-Neelsen stain** (acid-fast stain) directly visualizes **acid-fast bacilli** (AFB) like *Mycobacterium tuberculosis* in sputum, providing a rapid and definitive diagnosis of active infection.
*PPD test*
- A **PPD test** (tuberculin skin test) indicates exposure to *Mycobacterium tuberculosis* but cannot differentiate between **latent TB infection** and **active disease**.
- A positive PPD can occur in individuals previously exposed or vaccinated with BCG, offering no direct evidence of current active infection.
*Silver stain*
- **Silver stain** (e.g., Gomori methenamine silver) is used to identify fungal organisms like *Pneumocystis jirovecii* or certain bacteria, such as *Legionella pneumophila*.
- It is not the primary stain for diagnosing tuberculosis, which requires detection of acid-fast bacilli.
*Gram stain*
- **Gram stain** is used to classify bacteria based on their cell wall properties (Gram-positive or Gram-negative).
- *Mycobacterium tuberculosis* has a unique **mycolic acid-rich cell wall** that makes it resistant to Gram staining and requires acid-fast staining for visualization.
*Interferon-gamma assay*
- An **interferon-gamma release assay (IGRA)**, like the Quantiferon-TB Gold test, detects exposure to *Mycobacterium tuberculosis* and is used to diagnose **latent TB infection**.
- Similar to the PPD test, it cannot distinguish between latent infection and **active disease**, and a positive result requires further investigation for active TB.
Mycobacteria overview US Medical PG Question 9: A 68-year-old man comes to the physician because of a 1-month history of fatigue, low-grade fevers, and cough productive of blood-tinged sputum. He has type 2 diabetes mellitus and chronic kidney disease and underwent kidney transplantation 8 months ago. His temperature is 38.9°C (102.1°F) and pulse is 98/min. Examination shows rhonchi in the right lower lung field. An x-ray of the chest shows a right-sided lobar consolidation. A photomicrograph of specialized acid-fast stained tissue from a blood culture is shown. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Sharing of unsterile IV needles
- B. Poor oral hygiene
- C. Exposure to contaminated air-conditioning unit
- D. Exposure to contaminated soil (Correct Answer)
- E. Crowded living situation
Mycobacteria overview Explanation: ***Exposure to contaminated soil***
- The photomicrograph shows **acid-fast stain** demonstrating **filamentous, branching gram-positive rods**, consistent with **Nocardia species**.
- **Nocardiosis** is acquired through **inhalation of Nocardia spores from contaminated soil or dust**, which is the primary environmental source and route of transmission.
- While this patient's **immunocompromised status** (post-kidney transplant on immunosuppressive therapy) is the critical host factor that predisposes him to infection, **soil exposure** is the specific environmental predisposing factor among the options listed.
- Nocardia is an opportunistic pathogen that primarily affects immunocompromised individuals, causing pulmonary infection that can disseminate.
*Sharing of unsterile IV needles*
- Sharing unsterile IV needles is a common route for transmitting **bloodborne pathogens** (e.g., HIV, hepatitis B/C) or causing bacterial endocarditis and soft tissue infections.
- This is not the typical route of acquisition for **pulmonary nocardiosis**, which is acquired via inhalation.
*Poor oral hygiene*
- Poor oral hygiene predisposes to dental caries, periodontal disease, and aspiration of oral flora causing pneumonia or lung abscess.
- **Actinomyces** (not acid-fast) is associated with poor oral hygiene and can be confused with Nocardia morphologically, but Actinomyces is not acid-fast positive.
- This is not a risk factor for acquiring **Nocardia** infection.
*Exposure to contaminated air-conditioning unit*
- Contaminated air-conditioning units and water systems are associated with **Legionella pneumophila**, causing Legionnaires' disease.
- Legionella is not acid-fast and does not show the branching filamentous morphology seen with Nocardia.
*Crowded living situation*
- Crowded living situations increase risk of person-to-person transmission of respiratory pathogens such as **Mycobacterium tuberculosis**, influenza, and other droplet-spread infections.
- **Nocardia** is acquired from environmental sources (soil, dust), not through person-to-person transmission.
Mycobacteria overview US Medical PG Question 10: A 16-year-old female presents to her pediatrician complaining of 2 weeks of fever and 1 week of swollen lumps in her left armpit. Upon examination of the left upper extremity, her physician notes the presence of a single papule which the patient claimed appeared one week ago. The patient started her first job at a pet store 2.5 weeks ago. Which of the following is the vector of transmission of the causative agent?
- A. Cats (Correct Answer)
- B. Rabbits
- C. Animal urine
- D. Parrots
- E. Armadillos
Mycobacteria overview Explanation: ***Cats***
- The combination of **fever**, **swollen lymph nodes** (lumps in the armpit), a **single papule**, and a recent history of working at a **pet store** strongly suggests **cat scratch disease**.
- **Cat scratch disease** is caused by *Bartonella henselae*, which is primarily transmitted to humans through the **scratch or bite of a cat**, especially kittens.
*Rabbits*
- Rabbits are known vectors for diseases like **tularemia**, which can cause fever and swollen lymph nodes.
- However, the typical presentation of tularemia often includes a more prominent **ulcerative lesion** at the site of inoculation, and the papule described is less characteristic.
*Animal urine*
- While animal urine can transmit diseases like **leptospirosis**, which can cause fever and various systemic symptoms, it typically does not present with a localized papule followed by regional lymphadenopathy in this manner.
- Exposure to animal urine usually occurs through contact with contaminated water or soil, and the pet store context points more towards direct animal contact.
*Parrots*
- Parrots are associated with **psittacosis** (parrot fever), caused by *Chlamydia psittaci*.
- Psittacosis primarily manifests as a **respiratory illness** (pneumonia) and does not typically present with a localized papule and regional lymphadenopathy.
*Armadillos*
- Armadillos are significant reservoirs for **Mycobacterium leprae**, the causative agent of **leprosy**.
- Leprosy has a very long incubation period and presents with skin lesions, nerve damage, and sometimes lymphadenopathy, but a 2-week onset and the described acute symptoms are inconsistent with leprosy.
More Mycobacteria overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.