Leptospira species US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Leptospira species. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Leptospira species US Medical PG Question 1: A 23-year-old woman presents with progressively worsening headache, photophobia, and intermittent fever that have lasted for 6 days. She says her headache is mostly frontal and radiates down her neck. She denies any recent history of blood transfusions, recent travel, or contact with animals. Her past medical history is unremarkable. She is sexually active with a single partner for the past 3 years. Her temperature is 38.5°C (101.3°F). On physical examination, she appears pale and diaphoretic. A fine erythematous rash is noted on the neck and forearms. A lumbar puncture is performed and CSF analysis reveals:
Opening pressure: 300 mm H2O
Erythrocytes: None
Leukocytes: 72/mm3
Neutrophils: 10%
Lymphocytes: 75%
Mononuclear: 15%
Protein: 100 mg/dL
Glucose: 70 mg/dL
Which of the following is the most likely diagnosis in this patient?
- A. Lymphocytic choriomeningitis virus
- B. Ehrlichiosis
- C. Enterovirus meningitis (Correct Answer)
- D. Brucellosis
- E. Mumps meningitis
Leptospira species Explanation: ***Enterovirus meningitis***
- The patient's symptoms of **headache**, **photophobia**, **fever**, and a **fine erythematous rash**, combined with CSF findings of **lymphocytic pleocytosis (75%)**, **elevated protein**, and **normal glucose**, are classic for **viral (aseptic) meningitis**.
- Enteroviruses (including coxsackievirus and echovirus) are the **most common cause** of viral meningitis in immunocompetent adults, particularly in summer and fall.
- The **normal glucose level** (70 mg/dL) effectively rules out bacterial meningitis, while the **lymphocytic predominance** with mildly elevated protein is pathognomonic for viral etiology.
- The fine erythematous rash is consistent with enteroviral exanthem.
*Lymphocytic choriomeningitis virus*
- While LCMV can cause aseptic meningitis with similar CSF findings (lymphocytic pleocytosis, normal glucose), it is typically acquired through contact with **rodent urine or feces**, particularly from pet hamsters or mice.
- The patient **denies animal contact**, making this diagnosis less likely than the more prevalent enterovirus infection.
*Ehrlichiosis*
- Ehrlichiosis is a **tick-borne illness** (from *Ehrlichia* species) that can cause fever, headache, and rash, but typically presents with **leukopenia**, **thrombocytopenia**, and elevated liver enzymes.
- The rash in ehrlichiosis is often petechial or absent entirely. CNS involvement is uncommon and would more likely present as meningoencephalitis rather than isolated meningitis.
- The CSF profile with prominent lymphocytic pleocytosis and normal glucose fits viral meningitis better than ehrlichiosis.
*Brucellosis*
- Brucellosis is a **zoonotic infection** acquired through contact with **unpasteurized dairy products** or infected livestock (cattle, goats, pigs), which the patient denies.
- While *Brucella* can cause chronic meningitis with lymphocytic pleocytosis, it classically presents with **undulating fever**, hepatosplenomegaly, and a more protracted course (weeks to months).
- The acute 6-day presentation without exposure history makes this unlikely.
*Mumps meningitis*
- Mumps virus can cause aseptic meningitis with a similar CSF profile (lymphocytic pleocytosis, normal glucose).
- However, mumps meningitis typically occurs in association with or following **parotitis (parotid gland swelling)**, which is not mentioned in this case.
- With widespread MMR vaccination, mumps is now rare in immunized populations, making enterovirus a more likely diagnosis.
Leptospira species US Medical PG Question 2: A 26-year-old immigrant from Mexico presents to your clinic for a physical. He tells you that several weeks ago, he noticed a lesion on his penis which went away after several weeks. It was nontender and did not bother him. He currently does not have any complaints. His temperature is 97.9°F (36.6°C), blood pressure is 139/91 mmHg, pulse is 87/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is unremarkable and shows no evidence of any rash. A VDRL and FTA-ABS test are both positive. What is the most appropriate management of this patient?
- A. Penicillin (Correct Answer)
- B. Doxycycline
- C. No treatment indicated
- D. Acyclovir
- E. Azithromycin and ceftriaxone
Leptospira species Explanation: ***Penicillin***
- The patient's history of a **painless genital ulcer** that resolved spontaneously, followed by positive VDRL and FTA-ABS tests, is classic for **syphilis**. Given the VDRL and FTA-ABS are both positive, this indicates a current or treated syphilis infection.
- **Penicillin G** is the drug of choice for all stages of syphilis; the specific formulation (e.g., benzathine penicillin G) and duration depend on the stage of infection.
*Doxycycline*
- **Doxycycline** can be used as an alternative treatment for syphilis in patients with a **penicillin allergy**.
- However, it is not the first-line treatment and there is no indication of a penicillin allergy in this patient.
*No treatment indicated*
- The positive VDRL and FTA-ABS tests definitively confirm an active or recently treated syphilis infection, requiring **treatment**.
- Leaving syphilis untreated can lead to severe complications, including **neurosyphilis** and **cardiovascular syphilis**.
*Acyclovir*
- **Acyclovir** is an antiviral medication used to treat **herpes simplex virus (HSV)** infections, which cause painful genital ulcers, not the painless chancre seen in syphilis.
- It has no efficacy against the bacterial pathogen *Treponema pallidum* that causes syphilis.
*Azithromycin and ceftriaxone*
- The combination of **azithromycin and ceftriaxone** is typically used to treat uncomplicated **gonorrhea** and **chlamydia** simultaneously.
- While these are common sexually transmitted infections, they do not cause the painless chancre or result in the serological findings (positive VDRL and FTA-ABS) characteristic of syphilis.
Leptospira species US Medical PG Question 3: A 30-year-old woman comes to the emergency department because of fever, watery diarrhea, and abdominal cramping for the past 24 hours. She recently went to an international food fair. Her temperature is 39°C (102.2°F). Physical examination shows increased bowel sounds. Stool cultures grow gram-positive, spore-forming, anaerobic rods that produce alpha toxin. The responsible organism also causes which of the following physical examination findings?
- A. Diffuse, flaccid bullae
- B. Subcutaneous crepitus (Correct Answer)
- C. Facial paralysis
- D. Rose spots
- E. Petechial rash
Leptospira species Explanation: ***Subcutaneous crepitus***
- The description of gram-positive, spore-forming, anaerobic rods producing alpha toxin is characteristic of *Clostridium perfringens*.
- This organism causes **two main clinical syndromes**: (1) **food poisoning** with diarrhea (as in this patient), and (2) **gas gangrene** (clostridial myonecrosis).
- **Gas gangrene** is characterized by muscle necrosis, gas production in tissues (leading to **crepitus** on palpation), and rapid tissue destruction.
*Diffuse, flaccid bullae*
- This finding is more commonly associated with **staphylococcal scalded skin syndrome (SSSS)** caused by *Staphylococcus aureus* exfoliative toxins.
- *Clostridium perfringens* infections typically lead to **gas formation** and tissue necrosis rather than superficial bullae.
*Facial paralysis*
- **Facial paralysis** is characteristic of *Clostridium botulinum* (botulism), which produces neurotoxins that block acetylcholine release.
- *Clostridium perfringens* does not produce neurotoxins that cause paralysis; its pathogenicity is due to **alpha toxin** (phospholipase C) causing tissue destruction.
*Rose spots*
- **Rose spots** are characteristic of **typhoid fever**, caused by *Salmonella Typhi*.
- They are faint, salmon-colored maculopapular lesions on the trunk that blanch with pressure.
*Petechial rash*
- A **petechial rash** is often seen in conditions like **meningococcemia** (*Neisseria meningitidis*), **Rocky Mountain spotted fever**, or bacterial **endocarditis** due to vascular damage.
- While *Clostridium perfringens* can cause severe sepsis, a petechial rash is not its classic presentation.
Leptospira species US Medical PG Question 4: Six days after undergoing an elective hip replacement surgery, a 79-year-old man develops dysuria, flank pain, and fever. His temperature is 38.5°C (101.3°F). Examination shows marked tenderness in the right costovertebral area. Treatment with an antibiotic is begun, but his symptoms do not improve. Further evaluation shows that the causal organism produces an enzyme that inactivates the antibiotic via phosphorylation. An agent from which of the following classes of antibiotics was most likely administered?
- A. Macrolides
- B. Tetracyclines
- C. Aminoglycosides (Correct Answer)
- D. Glycopeptides
- E. Fluoroquinolones
Leptospira species Explanation: ***Aminoglycosides***
- **Aminoglycosides** are commonly inactivated by bacterial enzymes through **phosphorylation**, acetylation, or adenylation, leading to resistance.
- The patient's lack of improvement despite antibiotic treatment and the mechanism of inactivation point towards this class of antibiotics.
*Macrolides*
- **Macrolide resistance** typically involves mechanisms such as modification of the ribosomal binding site (e.g., methylation), drug efflux pumps, or enzymatic inactivation by esterases, not phosphorylation.
- While macrolides can treat various infections, their inactivation mechanism is different from what is described.
*Tetracyclines*
- **Tetracycline resistance** is primarily mediated by bacterial efflux pumps that actively transport the antibiotic out of the cell, or by ribosomal protection proteins that interfere with drug binding.
- **Enzymatic inactivation via phosphorylation** is not a characteristic resistance mechanism for tetracyclines.
*Glycopeptides*
- **Glycopeptide resistance**, particularly to vancomycin, is mainly associated with alterations in the cell wall precursor target (e.g., D-Ala-D-Lac modification), which prevents the antibiotic from binding.
- This mechanism is distinct from enzymatic phosphorylation of the antibiotic molecule itself.
*Fluoroquinolones*
- **Fluoroquinolone resistance** primarily arises from mutations in the genes encoding bacterial DNA gyrase and topoisomerase IV, or via efflux pumps.
- There is no significant mechanism of resistance involving direct enzymatic phosphorylation of fluoroquinolone drugs.
Leptospira species US Medical PG Question 5: A 13-year-old boy is brought to a physician with severe fevers and headaches for 3 days. The pain is constant and mainly behind the eyes. He has myalgias, nausea, vomiting, and a rash for one day. Last week, during an academic winter break, he traveled on a tour with his family to several countries, including Brazil, Panama, and Peru. They spent many evenings outdoors without any protection against insect bites. There is no history of contact with pets, serious illness, or use of medications. The temperature is 40.0℃ (104.0℉); the pulse is 110/min; the respiratory rate is 18/min, and the blood pressure is 110/60 mm Hg. A maculopapular rash is seen over the trunk and extremities. Several tender lymph nodes are palpated in the neck on both sides. A peripheral blood smear shows no organisms. Which of the following is most likely responsible for this patient’s presentation?
- A. Chagas disease
- B. Zika virus
- C. Babesiosis
- D. Malaria
- E. Dengue fever (Correct Answer)
Leptospira species Explanation: ***Dengue fever***
- This patient's symptoms (fever, **retro-orbital headache**, myalgias, nausea, vomiting, rash, and travel history to endemic areas like **Brazil, Panama, and Peru**) are classic for dengue fever. The **high fever (40°C)** and rash are also highly suggestive.
- Exposure to mosquito bites in tropical regions, typical of travel during an academic break, is a common mode of transmission for this **flavivirus**.
*Chagas disease*
- Chagas disease, caused by **Trypanosoma cruzi**, is typically transmitted by the **reduviid bug** (kissing bug).
- Acute symptoms can include **fever**, **Romana's sign** (unilateral periorbital swelling), and sometimes a chagoma, but the widespread **maculopapular rash** and severe retro-orbital headache are less characteristic.
*Zika virus*
- Zika virus infection can present with **fever**, **rash**, **arthralgia**, and **conjunctivitis**.
- While the travel history fits, the **severe retro-orbital headache**, high fever, and myalgias are more prominent in dengue fever; Zika symptoms are generally milder in adults.
*Babesiosis*
- Babesiosis is a **tick-borne** illness caused by **Babesia parasites**, often presenting with **fever**, **fatigue**, chills, and **hemolytic anemia**.
- There is no mention of tick exposure, and the characteristic rash and retro-orbital headache are not typical features of babesiosis.
*Malaria*
- Malaria, caused by **Plasmodium parasites** transmitted by **Anopheles mosquitoes**, presents with cyclical fevers, chills, sweats, and fatigue.
- While the travel history to endemic areas is relevant, the **retro-orbital headache** and **maculopapular rash** as described are not typical for uncomplicated malaria; malaria is also detected on a peripheral blood smear, which was negative here.
Leptospira species US Medical PG Question 6: A 26-year-old woman seeks evaluation at an urgent care clinic with complaints of fever and generalized muscle and joint pain for the past 3 days. She also complains of nausea, but denies vomiting. She does not mention any past similar episodes. Her past medical history is unremarkable, but she returned to the United States 1 week ago after spending 2 weeks in southeast Asia doing charity work. She received all the recommended vaccines prior to traveling. The temperature is 40.0°C (104.0°F), the respirations are 15/min, the pulse is 107/min, and the blood pressure is 98/78 mm Hg. Physical examination shows mild gingival bleeding and a petechial rash over the trunk. Laboratory studies show the following:
Laboratory test
Leukocyte count 4,000/mm³
Platelet count 100,000/mm³
Partial thromboplastin time (activated) 45 seconds
Which of the following is the most likely cause of this patient’s condition?
- A. Dengue fever (Correct Answer)
- B. Leptospirosis
- C. Typhoid fever
- D. Yellow fever
- E. Ebola virus
Leptospira species Explanation: ***Dengue fever***
- This patient presents with a classic constellation of symptoms including **high fever**, **myalgia**, **arthralgia** (break-bone fever), **nausea**, and **petechial rash**, along with **thrombocytopenia** and evidence of **hemorrhagic manifestations** (mild gingival bleeding, petechiae, and prolonged PTT due to thrombocytopenia). Recent travel to Southeast Asia, an endemic region, further supports this diagnosis.
- The combination of **fever**, **leukopenia**, **thrombocytopenia**, and **hemorrhagic signs** in a patient returning from an endemic area is highly suggestive of dengue fever.
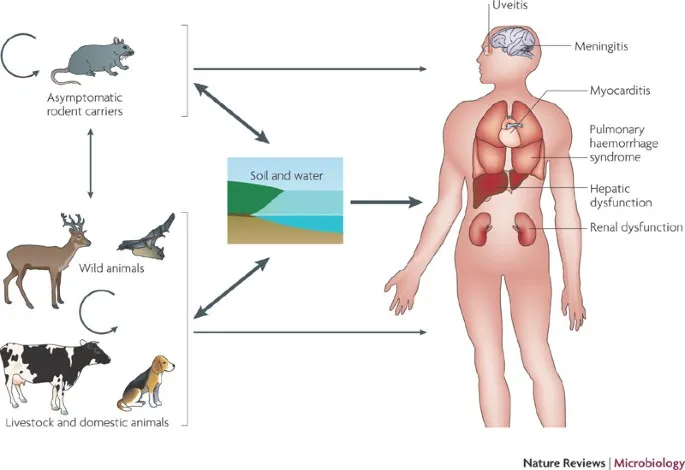
*Leptospirosis*
- While leptospirosis can cause **fever**, **myalgia**, and **nausea**, it is typically associated with contact with **contaminated water** or animal urine and often presents with **conjunctival suffusion** and sometimes **renal or hepatic involvement**, which are not prominent here.
- **Thrombocytopenia** and **hemorrhagic manifestations** are less common or severe in typical leptospirosis compared to dengue.
*Typhoid fever*
- Typhoid fever is characterized by a **gradually escalating fever**, **relative bradycardia**, and often a **"rose spot" rash**, along with **gastrointestinal symptoms** like constipation or diarrhea.
- While leukopenia can occur, **thrombocytopenia** and **hemorrhagic signs** like petechiae and gingival bleeding are not typical features.
*Yellow fever*
- Yellow fever, though mosquito-borne and endemic in some tropical regions, typically presents with **jaundice** (hence "yellow" fever), **renal failure**, and more severe **hemorrhage** (black vomitus) in its toxic phase.
- The patient's symptoms are more consistent with dengue's milder hemorrhagic picture and lack the prominent liver and kidney involvement seen in yellow fever.
*Ebola virus*
- Ebola virus disease causes a severe **hemorrhagic fever** with rapid onset and high mortality, characterized by profound **multi-organ failure**, widespread **hemorrhage** (internal and external), and severe **gastrointestinal symptoms** (vomiting, diarrhea).
- The clinical presentation, while including fever and some hemorrhagic signs, is not as severe or rapidly progressing as typical Ebola, nor does it fit the travel epidemiology for this patient (Ebola is endemic to Central and West Africa, not Southeast Asia).
Leptospira species US Medical PG Question 7: A 29-year-old man presents to the clinic complaining of fatigue and loss of sensation in his lower legs. The patient notes no history of trauma or chronic disease but states that he spends a lot of time outside and often encounters wild animals. On examination, the patient has multiple dark lesions over the skin of his face and back, as well as a decreased sensation of fine touch and vibration bilaterally in the lower extremities. What is the morphology of the etiologic agent causing this patient’s symptoms?
- A. An acid-fast, intracellular bacillus (Correct Answer)
- B. Reactivation of latent viral infection
- C. Maltose-fermenting gram-negative diplococci
- D. A spirochete transmitted via tick
- E. Gram-positive, branching anaerobe
Leptospira species Explanation: ***An acid-fast, intracellular bacillus***
- The patient's symptoms (fatigue, loss of sensation in lower legs, dark skin lesions, exposure to wild animals, and decreased fine touch/vibration) are highly suggestive of **leprosy** (Hansen's disease).
- Leprosy is caused by **_Mycobacterium leprae_**, which is an **acid-fast, obligate intracellular bacillus** that preferentially infects macrophages and Schwann cells, leading to nerve damage and skin lesions.
*Reactivation of latent viral infection*
- While viral infections can cause neurological symptoms, the presentation with specific **dark skin lesions** and the history of exposure to **wild animals** (potentially armadillos, a reservoir for _M. leprae_) point away from a common latent viral reactivation.
- **Herpes zoster** (shingles) is a common reactivation of a latent viral infection (varicella-zoster virus), but it typically presents with a dermatomal rash and neuropathic pain rather than widespread dark lesions and bilateral sensory loss in the lower extremities.
*Maltose-fermenting gram-negative diplococci*
- **Maltose-fermenting gram-negative diplococci** describe **_Neisseria meningitidis_**, which causes meningitis.
- This organism primarily causes symptoms related to meningitis (fever, headache, neck stiffness), and does not typically present with the chronic sensory loss or characteristic skin lesions seen in this patient.
*A spirochete transmitted via tick*
- A **spirochete transmitted via a tick** refers to **_Borrelia burgdorferi_**, the causative agent of **Lyme disease**.
- Lyme disease presents with an **erythema migrans rash** (bull's-eye rash), joint pain, and neurological symptoms, but the skin lesions described here (multiple dark lesions) and the progressive sensory loss are not typical for Lyme disease.
*Gram-positive, branching anaerobe*
- A **gram-positive, branching anaerobe** describes **_Actinomyces_ species**, which cause **actinomycosis**.
- Actinomycosis typically presents with chronic abscesses and sinus tracts, often affecting the head and neck, thorax, or abdomen, and does not cause the diffuse sensory loss or skin lesions described in this case.
Leptospira species US Medical PG Question 8: A 42-year-old man comes to his physician with a history of fever, non-bloody diarrhea, and headache for 10 days. He also complains of anorexia and abdominal pain. He returned from a trip to India 3 weeks ago. His temperature is 40.0°C (104.0°F), pulse is 65/min, respirations are 15/min, and blood pressure is 135/80 mm Hg. He has developed a blanchable rash on his chest and trunk. A photograph of the rash is shown. Examination of the heart, lungs, and abdomen show no abnormalities. Laboratory studies show:
Hemoglobin 15 g/dL
Mean corpuscular volume 95 μm3
White blood cell count 3400/mm3
Percent segmented neutrophils 40%
Which of the following is the most likely diagnosis?
- A. Leptospirosis
- B. Enteric fever (Correct Answer)
- C. Dengue fever
- D. Malaria
- E. Nontyphoidal salmonellosis
Leptospira species Explanation: ***Enteric fever***
- The constellation of **fever**, **non-bloody diarrhea**, **bradycardia** (pulse 65/min with 40°C fever), **leukopenia** (WBC 3400/mm³), **rose spots** (blanchable rash on chest/trunk), and recent travel to **India** (endemic area) is highly characteristic of enteric fever caused by *Salmonella Typhi* or *Paratyphi*.
- Abdominal pain, anorexia, and headache are also common symptoms, and the relatively low **neutrophil percentage** (40%) further supports the diagnosis of a bacterial infection with atypical white blood cell response.
*Leptospirosis*
- While leptospirosis can cause **fever** and **headache** and is found in tropical regions, it typically presents with **conjunctival suffusion**, **muscle pain**, and sometimes **jaundice** or **renal involvement**, none of which are detailed here.
- Exposure usually involves contact with contaminated water or soil, and **diarrhea** is less common than in enteric fever.
*Dengue fever*
- Dengue fever is characterized by **high fever**, severe **myalgia** and **arthralgia** ("breakbone fever"), and often a **maculopapular rash**, but **bradycardia** and **leukopenia** with low neutrophils are not typical features.
- **Hemorrhagic manifestations** are also a concern in severe dengue, which are not described.
*Malaria*
- Malaria presents with cyclical **fever** (often paroxysmal), **chills**, **sweats**, and frequently causes **anemia** and **thrombocytopenia**.
- While **leukopenia** can occur, the presence of **rose spots** and sustained fever with relative **bradycardia** point away from malaria as the primary diagnosis.
*Nontyphoidal salmonellosis*
- This typically causes **gastroenteritis** with **diarrhea**, **vomiting**, and **fever**, which is usually self-limiting.
- It would not typically present with **rose spots**, pronounced **bradycardia**, or a prolonged course with systemic symptoms suggestive of enteric fever.
Leptospira species US Medical PG Question 9: A 44-year-old woman presents to her primary care physician for worsening dysuria, hematuria, and lower abdominal pain. Her symptoms began approximately 2 days ago and have progressively worsened. She denies headache, nausea, vomiting, or diarrhea. She endorses feeling "feverish" and notes to having foul smelling urine. She has a past medical history of Romano-Ward syndrome and is not on any treatment. She experiences profuse diarrhea and nausea when taking carbapenems and develops a severe rash with cephalosporins. Her temperature is 100.4°F (38C), blood pressure is 138/93 mmHg, pulse is 100/min, and respirations are 18/min. On physical exam, the patient appears uncomfortable and there is tenderness to palpation around the bilateral flanks and costovertebral angle. A urinalysis and urine culture is obtained and appropriate antibiotics are administered. On her next clinical visit urine studies and a basic metabolic panel is obtained, which is shown below:
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.2 mEq/L
HCO3-: 22 mEq/L
BUN: 20 mg/dL
Glucose: 94 mg/dL
Creatinine: 2.4 mg/dL
Urinalysis
Color: Yellow
Appearance: Clear
Blood: Negative
pH: 7 (Normal 5-8)
Protein: Negative
Nitrite: Negative
Leukocyte esterase: Negative
Cast: Epithelial casts
FeNa: 3%
Urine culture
Preliminary report: 10,000 CFU/mL E. coli
Which of the following antibiotics was most likely given to this patient?
- A. Aztreonam (Correct Answer)
- B. Vancomycin
- C. Clindamycin
- D. Levofloxacin
- E. Tobramycin
Leptospira species Explanation: ***Aztreonam***
- This patient presents with **pyelonephritis** (fever, flank pain, dysuria, hematuria, CVA tenderness) with confirmed *E. coli* urinary tract infection
- She has **severe allergies to both carbapenems and cephalosporins**, eliminating most beta-lactam options
- **Aztreonam** is a monobactam antibiotic with excellent activity against **gram-negative bacteria** including *E. coli*
- Critically, aztreonam **does not cross-react** with other beta-lactams due to its unique monocyclic structure, making it safe in patients with penicillin/cephalosporin allergies
- **No QT prolongation** - safe in Romano-Ward syndrome
*Vancomycin*
- Primarily effective against **gram-positive bacteria** (MRSA, enterococci)
- **No activity against gram-negative organisms** like *E. coli*
- Would not be appropriate for this urinary tract infection
*Clindamycin*
- Used primarily for **anaerobic infections** and some gram-positive bacteria
- **Limited to no activity against *E. coli*** and other gram-negative organisms
- Not an effective choice for gram-negative pyelonephritis
*Levofloxacin*
- Fluoroquinolone with excellent gram-negative coverage and urinary penetration
- Generally a good choice for *E. coli* pyelonephritis
- **CONTRAINDICATED in this patient**: Fluoroquinolones cause **QT interval prolongation**, which is dangerous in patients with **Romano-Ward syndrome (congenital long QT syndrome)**
- This critical drug-disease interaction eliminates fluoroquinolones as an option
*Tobramycin*
- Aminoglycoside with good gram-negative coverage including *E. coli*
- **Highly nephrotoxic** - contraindicated in this patient with **acute kidney injury** (elevated creatinine 2.4 mg/dL, epithelial casts, FENa 3%)
- Risk of worsening renal function and ototoxicity makes it a poor choice
Leptospira species US Medical PG Question 10: A 24-year-old man presents with a painless genital ulcer for the past 2 weeks. He reports that he recently has been having unprotected sex with multiple partners. Past medical history is unremarkable. On physical examination, a single ulcer is present on the dorsal shaft of the penis which is circumscribed, indurated, and partially healed. There is moderate inguinal lymphadenopathy but no buboes. Which of the following tests would confirm the most likely diagnosis in this patient?
- A. Perform a darkfield microscopic examination of a swab from the chancre (Correct Answer)
- B. Swab the chancre and perform a saline wet mount
- C. Fluorescent treponemal antibody absorption (FTA-ABS) test
- D. Frei test
- E. Venereal Disease Research Laboratory (VDRL) test
Leptospira species Explanation: ***Perform a darkfield microscopic examination of a swab from the chancre***
- This patient's presentation with a **painless, indurated genital ulcer** (chancre) and regional lymphadenopathy is highly suggestive of **primary syphilis**.
- **Darkfield microscopy** directly visualizes the spirochetes (**_Treponema pallidum_**) from the chancre, providing a definitive and rapid diagnosis.
*Swab the chancre and perform a saline wet mount*
- A **saline wet mount** is used to identify mobile organisms like **_Trichomonas vaginalis_** or clue cells suggestive of **bacterial vaginosis**, neither of which are associated with this type of ulcer.
- This test would not reveal the spirochetes responsible for syphilis and is not appropriate for diagnosing a genital ulcer.
*Fluorescent treponemal antibody absorption (FTA-ABS) test*
- The **FTA-ABS test** is a **treponemal-specific serological test** used to confirm a syphilis diagnosis, particularly in later stages or when non-treponemal tests are reactive.
- While sensitive for syphilis, it's typically reactive later in the disease course and cannot directly visualize the bacteria from the ulcer, making darkfield microscopy a more immediate and direct diagnostic tool for primary syphilis.
*Frei test*
- The **Frei test** is an obsolete intradermal skin test used to diagnose **lymphogranuloma venereum (LGV)**, which typically presents with a transient, unnoticed lesion followed by severe lymphadenopathy and buboes.
- It is not used for the diagnosis of syphilis and would not be helpful for this patient's presentation.
*Viral and rickettsial disease research laboratory (VDRL) test*
- The **VDRL test** is a **non-treponemal serological test** for syphilis that detects antibodies against cardiolipin, a lipid released from damaged host cells.
- While used for screening and monitoring treatment response, it can be **negative in early primary syphilis** (before seroconversion) and may not be positive at the time of presentation with a fresh chancre.
More Leptospira species US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.