Ehrlichia and Anaplasma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ehrlichia and Anaplasma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ehrlichia and Anaplasma US Medical PG Question 1: A 24-year-old woman complains of intermittent fever and joint pain. She says that these symptoms have been present for the past month. Before that, she had no signs or symptoms and was completely healthy. She has also lost her appetite and some weight. A complete blood count (CBC) showed severe pancytopenia. What is the next best step in evaluating this patient?
- A. Repeated CBCs for several weeks and reassess
- B. Treatment with corticosteroids
- C. Treatment with antibiotics
- D. Treatment for acute leukemia
- E. Bone marrow examination (Correct Answer)
Ehrlichia and Anaplasma Explanation: ***Bone marrow examination***
- The combination of **fever**, **joint pain**, **weight loss**, and **pancytopenia** in a previously healthy young woman raises suspicion for serious hematologic conditions like **aplastic anemia** or **acute leukemia**.
- A **bone marrow examination** is crucial for definitive diagnosis by evaluating the cellularity, morphology, and presence of abnormal cells.
*Repeated CBCs for several weeks and reassess*
- This approach is inappropriate given the **severe pancytopenia** and progressive symptoms, which indicate an urgent underlying pathology.
- Delaying diagnosis could worsen the patient's condition and compromise treatment outcomes due to the potential for severe infections or bleeding.
*Treatment with corticosteroids*
- While corticosteroids might be used in some autoimmune conditions causing pancytopenia, initiating treatment without a definitive diagnosis is premature and could mask the underlying cause, especially in cases of malignancy.
- There is no specific indication for corticosteroid use in this scenario without further diagnostic information.
*Treatment with antibiotics*
- Although **fever** is present, there's no clear evidence of an infection (like localized symptoms or positive cultures), and **pancytopenia** is not primarily managed with antibiotics.
- Administering antibiotics empirically without a confirmed infection addresses a symptom rather than the underlying progressive hematological disorder.
*Treatment for acute leukemia*
- While **acute leukemia** is a strong possibility, definitive treatment should only commence after a confirmed diagnosis through **bone marrow examination**, as misdiagnosis can lead to inappropriate and harmful therapy.
- Other conditions like severe aplastic anemia also present with similar features but require different management strategies.
Ehrlichia and Anaplasma US Medical PG Question 2: A 33-year-old man presents to the emergency department with a fever and fatigue. He states that he has not felt well since he returned from a hiking trip in Alabama. He is generally healthy and has no other medical conditions. His temperature is 101°F (38.3°C), blood pressure is 127/85 mmHg, pulse is 108/min, respirations are 14/min, and oxygen saturation is 99% on room air. Physical exam including a full dermatologic inspection is unremarkable. Laboratory studies are ordered as seen below.
Hemoglobin: 13 g/dL
Hematocrit: 39%
Leukocyte count: 2,200/mm^3 with normal differential
Platelet count: 77,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
HCO3-: 24 mEq/L
BUN: 19 mg/dL
Glucose: 98 mg/dL
Creatinine: 1.3 mg/dL
Ca2+: 10.2 mg/dL
AST: 92 U/L
ALT: 100 U/L
Which of the following is the most likely diagnosis?
- A. Lyme disease
- B. Babesiosis
- C. Influenza
- D. Ehrlichiosis (Correct Answer)
- E. Rocky Mountain spotted fever
Ehrlichia and Anaplasma Explanation: ***Ehrlichiosis***
- This patient's symptoms (fever, fatigue), recent travel to an **endemic area** (Alabama), **leukopenia** (WBC 2,200/mm^3), **thrombocytopenia** (platelet 77,000/mm^3), and **elevated liver enzymes** (AST 92, ALT 100) are highly characteristic of ehrlichiosis, a **tick-borne disease**.
- The absence of a rash helps differentiate it from some other tick-borne illnesses.
*Lyme disease*
- While Lyme disease is also tick-borne, it typically presents with an **erythema migrans rash**, which is absent in this case.
- Lyme disease is less commonly associated with the **pronounced leukopenia** and **thrombocytopenia** seen here.
*Rocky Mountain spotted fever*
- Rocky Mountain Spotted Fever (RMSF) is characterized by a **maculopapular rash** that often starts on the ankles and wrists and spreads centrally, involving the palms and soles. This rash is absent in the patient.
- While RMSF can cause thrombocytopenia and elevated liver enzymes, the **lack of rash is a key differentiator**.
*Babesiosis*
- Babesiosis is a tick-borne parasitic infection that causes **hemolytic anemia**, which is not clearly indicated by the patient's hemoglobin and hematocrit, and typically results in severe fatigue and sometimes splenomegaly.
- This condition is often seen in immunocompromised individuals or those without a spleen, and the labs here are more consistent with ehrlichiosis than babesiosis.
*Influenza*
- Influenza presents with fever, fatigue, myalgia, and respiratory symptoms, but it does not cause **thrombocytopenia**, **leukopenia**, or **elevated liver enzymes** to the extent seen in this patient.
- The symptoms are more indicative of a **tick-borne illness** given the travel history and specific lab abnormalities.
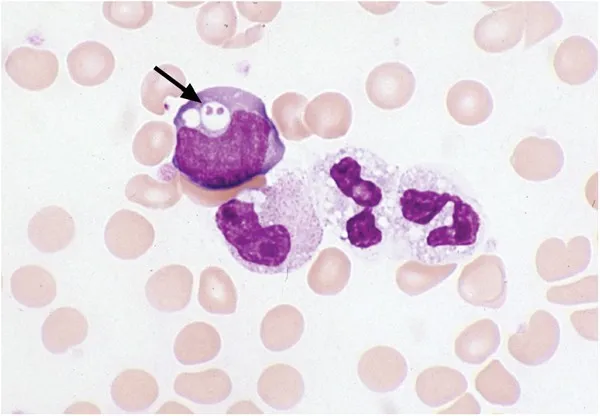
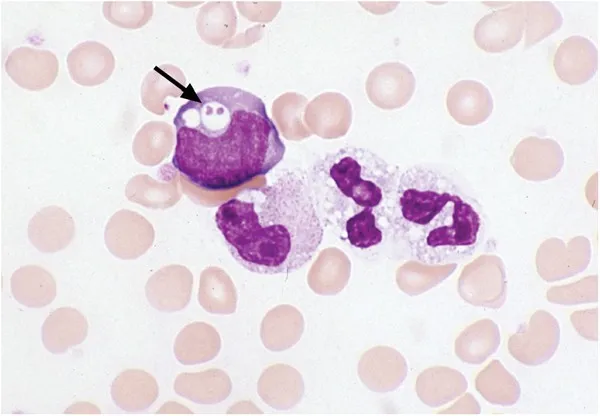
Ehrlichia and Anaplasma US Medical PG Question 3: A 32-year-old man is brought to the physician by his wife for a 3-day history of fever, headaches, and myalgias. He returned from a camping trip in Oklahoma 10 days ago. He works as a computer salesman. His temperature is 38.1°C (100.6°F). Neurologic examination shows a sustained clonus of the right ankle following sudden passive dorsiflexion. He is disoriented to place and time but recognizes his wife. Laboratory studies show a leukocyte count of 1,700/mm3 and a platelet count of 46,000/mm3. A peripheral blood smear shows monocytes with intracytoplasmic morulae. Which of the following is the most likely causal organism?
- A. Coxiella burnetii
- B. Rickettsia rickettsii
- C. Anaplasma phagocytophilum
- D. Borrelia burgdorferi
- E. Ehrlichia chaffeensis (Correct Answer)
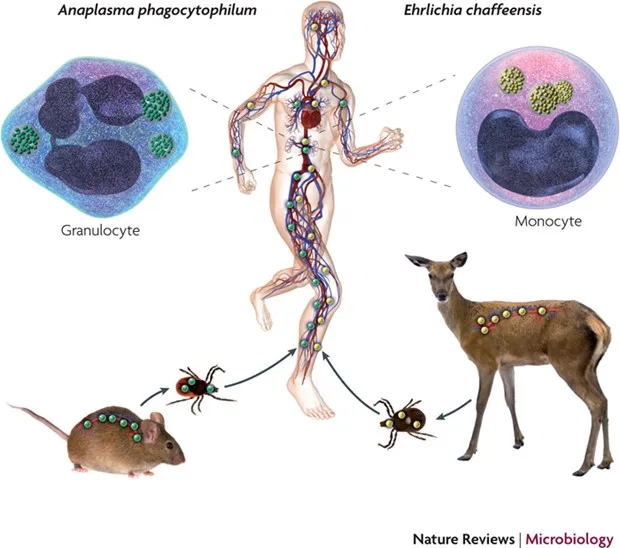
Ehrlichia and Anaplasma Explanation: ***Correct: Ehrlichia chaffeensis***
- The presence of **intracytoplasmic morulae** in **monocytes** is a pathognomonic sign for *Ehrlichia chaffeensis* infection, which causes **human monocytic ehrlichiosis**.
- The patient's symptoms of **fever, headache, myalgias, thrombocytopenia, leukopenia**, and the history of a **camping trip** in an endemic area (Oklahoma) are highly consistent with ehrlichiosis.
*Incorrect: Coxiella burnetii*
- This bacterium causes **Q fever**, characterized by fever, headache, and atypical pneumonia, but it does **not cause intracytoplasmic morulae** in monocytes or frequently lead to the degree of leukopenia and thrombocytopenia seen here.
- While it can be acquired from environments, the **microscopic findings** rule it out in this specific case.
*Incorrect: Rickettsia rickettsii*
- This organism causes **Rocky Mountain spotted fever**, which presents with fever, headache, myalgias, and a characteristic **rash** that is usually present on the palms and soles, none of which are mentioned here.
- It does not form **intracytoplasmic morulae** in monocytes.
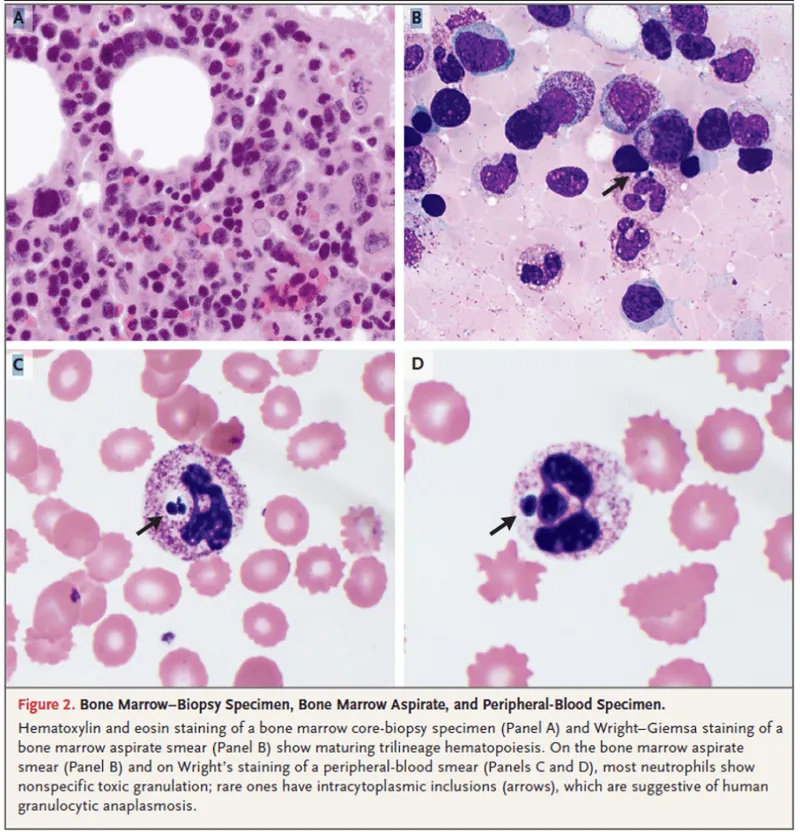
*Incorrect: Anaplasma phagocytophilum*
- This bacterium causes **human granulocytic anaplasmosis**, which is clinically similar to ehrlichiosis but forms **morulae in granulocytes** (neutrophils), not monocytes.
- The peripheral blood smear specifically identifies morulae in **monocytes**, directing towards *Ehrlichia*.
*Incorrect: Borrelia burgdorferi*
- This spirochete causes **Lyme disease**, characterized by an **expanding erythematous rash (erythema migrans)**, fever, and musculoskeletal symptoms, but it does not cause leukopenia or thrombocytopenia.
- It does not produce **morulae** in any blood cells.
Ehrlichia and Anaplasma US Medical PG Question 4: A 24-year-old female comes to the physician because of flu-like symptoms and a new rash for 2 days. She denies contacts with sick individuals or recent travel abroad, but recently went camping in Vermont. Vital signs are within normal limits. Examination of the lateral right thigh shows a circular red ring with central clearing. Which of the following is the natural reservoir of the pathogen responsible for this patient's symptoms?
- A. Rat
- B. Rabbit
- C. Tick
- D. Mouse (Correct Answer)
- E. Flea
Ehrlichia and Anaplasma Explanation: ***Mouse***
- The patient's symptoms, including **flu-like illness** and a **circular red rash with central clearing** (erythema migrans) after camping in Vermont, are classic for **Lyme disease**.
- The causative agent, *Borrelia burgdorferi*, is primarily maintained in **white-footed mice** (genus *Peromyscus*) in its natural reservoir during its larval and nymphal stages.
*Rat*
- While **rats** can carry and transmit various diseases, they are not the primary natural reservoir for *Borrelia burgdorferi*, the pathogen responsible for Lyme disease.
- Diseases associated with rats often include **leptospirosis** and **plague**, which present with different clinical pictures.
*Rabbit*
- **Rabbits** are known reservoirs for diseases like **tularemia** (*Francisella tularensis*), which can cause fever, skin lesions, and lymphadenopathy, but typically not the characteristic **erythema migrans** rash.
- They are not a significant natural reservoir for *Borrelia burgdorferi*.
*Tick*
- The **tick** (specifically *Ixodes scapularis* or **deer tick**) is the **vector** that transmits *Borrelia burgdorferi* to humans, not the natural reservoir.
- The tick acquires the bacteria from infected animal hosts such as mice and deer.
*Flea*
- **Fleas** are vectors for diseases such as **bubonic plague** (*Yersinia pestis*) and **endemic typhus** (*Rickettsia typhi*), which do not manifest with erythema migrans.
- They are not involved in the transmission or natural history of **Lyme disease**.
Ehrlichia and Anaplasma US Medical PG Question 5: A 29-year-old man comes to the physician because of a 3-day history of a swollen right knee. Over the past several weeks, he has had similar episodes affecting the right knee and sometimes also the left elbow, in which the swelling lasted an average of 5 days. He has a history of a rash that subsided 2 months ago. He lives in Connecticut with his wife and works as a landscaper. His temperature is 37.8°C (100°F), pulse is 90/min, respirations are 12/min, and blood pressure is 110/75 mm Hg. Physical examination shows a tender and warm right knee; range of motion is limited by pain. The remainder of the examination shows no abnormalities. His hematocrit is 44%, leukocyte count is 10,300/mm3, and platelet count is 145,000/mm3. Serum electrolyte concentrations are within normal limits. Arthrocentesis is performed and the synovial fluid is cloudy. Gram stain is negative. Analysis of the synovial fluid shows a leukocyte count of 70,000/mm3 and 80% neutrophils. Serologic testing confirms the diagnosis. Which of the following is the most likely cause?
- A. Rheumatoid arthritis
- B. Neisseria gonorrhoeae
- C. Borrelia burgdorferi (Correct Answer)
- D. Campylobacter jejuni
- E. Osteoarthritis
Ehrlichia and Anaplasma Explanation: ***Borrelia burgdorferi***
- The patient's **migratory polyarthritis** (affecting knee and elbow intermittently), history of a **rash** (consistent with erythema migrans), and residence in an **endemic area** (Connecticut) strongly suggest **Lyme disease**.
- **Synovial fluid analysis** showing high leukocyte count with neutrophilic predominance is typical of inflammatory arthritis, including Lyme arthritis, and **serologic testing** will confirm the presence of *Borrelia burgdorferi* antibodies.
*Rheumatoid arthritis*
- While rheumatoid arthritis causes inflammatory polyarthritis, it typically presents with **symmetrical joint involvement**, morning stiffness, and often involves smaller joints first, which is not described.
- The presence of a preceding **rash** and resolution within weeks is not characteristic of rheumatoid arthritis.
*Neisseria gonorrhoeae*
- **Disseminated gonococcal infection** can cause migratory polyarthralgia or septic arthritis, but it is typically associated with a history of recent unprotected sexual activity and often with tenosynovitis or dermatitis (pustular or vesicular lesions).
- While gram stain is negative in this case, gonococcal arthritis usually has a more rapid onset and systemic symptoms.
*Campylobacter jejuni*
- *Campylobacter jejuni* is a common cause of **reactive arthritis**, which can cause inflammatory joint pain after a gastrointestinal infection.
- However, reactive arthritis typically involves the **lower extremities** and has a specific pattern of oligoarthritis, often with enthesitis or dactylitis, and the preceding rash and geographical factors do not fit.
*Osteoarthritis*
- Osteoarthritis is a **degenerative joint disease** characterized by pain that worsens with activity and improves with rest, and typically affects older individuals.
- It does not present with a preceding **rash**, migratory inflammatory episodes, or a highly inflammatory synovial fluid (high leukocyte count with neutrophilic predominance).
Ehrlichia and Anaplasma US Medical PG Question 6: A 54-year-old woman comes to the physician because of lower back pain, night sweats, and a 5-kg (11-lb) weight loss during the past 4 weeks. She has rheumatoid arthritis treated with adalimumab. Her temperature is 38°C (100.4°F). Physical examination shows tenderness over the T10 and L1 spinous processes. Passive extension of the right hip causes pain in the right lower quadrant. The patient's symptoms are most likely caused by an organism with which of the following virulence factors?
- A. Proteins that bind to the Fc region of immunoglobulin G
- B. Protease that cleaves immunoglobulin A
- C. Polysaccharide capsule that prevents phagocytosis
- D. Surface glycolipids that prevent phagolysosome fusion (Correct Answer)
- E. Polypeptides that inactivate elongation factor 2
Ehrlichia and Anaplasma Explanation: ***Surface glycolipids that prevent phagolysosome fusion***
- The patient's symptoms (low back pain, night sweats, weight loss, fever, spinal tenderness, and hip pain) in a patient on **adalimumab** (a TNF-alpha inhibitor) suggest **disseminated tuberculosis** (Pott disease).
- *Mycobacterium tuberculosis* uses **mycolic acids** and other surface glycolipids to prevent phagolysosome fusion, allowing it to survive and replicate within macrophages.
*Proteins that bind to the Fc region of immunoglobulin G*
- This virulence factor is characteristic of bacteria like *Staphylococcus aureus* (Protein A) and *Streptococcus pyogenes* (Protein G), which is not consistent with the clinical picture.
- These proteins interfere with opsonization and antibody-mediated immunity, but are not the primary mechanism of *Mycobacterium tuberculosis* survival within macrophages.
*Protease that cleaves immunoglobulin A*
- **IgA protease** is a virulence factor for bacteria such as *Neisseria gonorrhoeae*, *Neisseria meningitidis*, and *Streptococcus pneumoniae*, which colonize mucosal surfaces.
- This mechanism helps these bacteria evade mucosal immunity, but it is not relevant to the pathogenesis of tuberculosis.
*Polysaccharide capsule that prevents phagocytosis*
- A polysaccharide capsule is a major virulence factor for many encapsulated bacteria (e.g., *Streptococcus pneumoniae*, *Haemophilus influenzae*, *Neisseria meningitidis*) that helps them evade phagocytosis.
- However, *Mycobacterium tuberculosis* is not primarily characterized by a polysaccharide capsule for immune evasion; its internal survival within macrophages is more critical.
*Polypeptides that inactivate elongation factor 2*
- Toxins that inactivate **elongation factor 2** are associated with *Corynebacterium diphtheriae* (**diphtheria toxin**) and *Pseudomonas aeruginosa* (**exotoxin A**), leading to inhibition of protein synthesis.
- This mechanism is not involved in the pathogenesis of *Mycobacterium tuberculosis* infection or its ability to cause disseminated disease.
Ehrlichia and Anaplasma US Medical PG Question 7: A 27-year-old man comes to the physician with throbbing right scrotal pain for 1 day. He has also had a burning sensation on urination during the last 4 days. He is sexually active with multiple female partners and does not use condoms. Physical examination shows a tender, palpable swelling on the upper pole of the right testicle; lifting the testicle relieves the pain. A Gram stain of urethral secretions shows numerous polymorphonuclear leukocytes but no organisms. Which of the following is the most likely causal pathogen of this patient's symptoms?
- A. Mycobacterium tuberculosis
- B. Pseudomonas aeruginosa
- C. Mumps virus
- D. Chlamydia trachomatis (Correct Answer)
- E. Staphylococcus aureus
Ehrlichia and Anaplasma Explanation: ***Chlamydia trachomatis***
- The patient's presentation with **epididymitis** (scrotal pain, tender palpable swelling on the upper pole of the testicle), **dysuria**, and a history of **multiple sexual partners without condoms** is classic for a sexually transmitted infection.
- **Positive Prehn's sign** (pain relief with testicular elevation) supports epididymitis over testicular torsion.
- The Gram stain showing **numerous polymorphonuclear leukocytes but no organisms** is highly suggestive of *C. trachomatis* infection, as it is an **obligate intracellular bacterium** that does not readily stain with Gram stain.
- This finding distinguishes it from *Neisseria gonorrhoeae* (the other common cause of STI-related epididymitis in young men), which would appear as **Gram-negative intracellular diplococci**.
*Mycobacterium tuberculosis*
- **Tuberculosis epididymitis** is rare in developed countries and typically presents with a more **insidious onset** over weeks to months, not acute onset over 1 day.
- It may involve caseating granulomas and is more common in immunocompromised patients.
- It would not explain the acute dysuria or the Gram stain findings of PMNs without organisms in a patient with risk factors for common STIs.
*Pseudomonas aeruginosa*
- **Pseudomonas epididymitis** is typically seen in older men (>35 years), those with urinary tract abnormalities, or after instrumentation/catheterization.
- It is uncommon in young, sexually active individuals without these risk factors.
- Gram stain would show **Gram-negative rods**, which is inconsistent with the "no organisms" finding.
*Mumps virus*
- **Mumps orchitis** typically presents with **testicular pain and swelling** (affecting the testis itself, not the epididymis).
- Mumps orchitis is usually preceded by **parotitis** (salivary gland swelling) 4-8 days earlier.
- It does not typically cause dysuria or lead to urethral secretions with PMNs.
- Mumps is now rare due to widespread MMR vaccination.
*Staphylococcus aureus*
- **Staphylococcus aureus** can cause epididymitis, especially in cases of direct trauma, hematogenous spread, or in patients with indwelling catheters.
- However, it's not a common cause of sexually transmitted epididymitis in young, healthy men.
- A Gram stain would reveal **Gram-positive cocci in clusters**, which was not seen in this case.
Ehrlichia and Anaplasma US Medical PG Question 8: A 19-year-old college student presents to student health with 1 day of fever and chills. He says that he has also been coughing for 2 days. His roommate was sick 3 days ago with similar symptoms and was diagnosed with Mycoplasma infection. He has otherwise been healthy and has had all the required vaccines as scheduled. He is currently taking introductory biology as part of his premedical studies and recently learned about antibodies. He therefore asks his physician about what his body is doing to fight off the infection. At this stage of his infection, which of the following forms are the antibodies circulating in his serum?
- A. Pentamers (Correct Answer)
- B. Dimers
- C. Tetramers
- D. Trimers
- E. Monomers
Ehrlichia and Anaplasma Explanation: ***Pentamers***
- In the **early stages** of a primary immune response, the B cells initially produce **IgM antibodies**.
- IgM antibodies circulate in the serum primarily as **pentamers**, making them highly effective at binding multiple antigens and activating complement.
*Dimers*
- **IgA antibodies** can exist as dimers, particularly secretory IgA found in mucosal secretions, but they are not the predominant form during the initial systemic immune response to an infection.
- While IgA plays a role in immunity, IgM is the primary antibody class produced in the **first few days of a new infection**.
*Tetramers*
- Antibodies typically do not form **stable tetrameric structures** as a functional unit in serum.
- The primary forms of antibodies are monomers, dimers, and pentamers, each with specific roles and locations.
*Trimers*
- **Trimeric antibody forms** are not a standard or significant configuration for immunoglobulins circulating in the serum.
- Antibody structures are well-defined as monomers (IgG, IgE, IgD), dimers (secretory IgA), or pentamers (IgM).
*Monomers*
- While **IgM can exist as a monomer** when expressed on the surface of B cells, serum IgM is predominantly in its **pentameric form**.
- **IgG** is the most abundant monomeric antibody in serum, but it is produced later in the immune response and at higher concentrations during secondary immune responses.
Ehrlichia and Anaplasma US Medical PG Question 9: A 21-year-old man presents to the emergency room complaining of pain upon urination and a watery discharge from his penis. It started a few days ago and has been getting progressively worse. His temperature is 98.0°F (36.7°C), blood pressure is 122/74 mmHg, pulse is 83/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for a tender urethra with a discharge. Gram stain of the discharge is negative for bacteria but shows many neutrophils. Which of the following is the most likely infectious etiology of this patient's symptoms?
- A. Chlamydia trachomatis (Correct Answer)
- B. Trichomonas vaginalis
- C. Neisseria gonorrhoeae
- D. Staphylococcus saprophyticus
- E. Escherichia coli
Ehrlichia and Anaplasma Explanation: ***Chlamydia trachomatis***
- The presentation of **dysuria**, **watery discharge**, and a **Gram stain negative for bacteria but positive for neutrophils** is highly characteristic of **non-gonococcal urethritis**, with *Chlamydia trachomatis* being the most common cause.
- *Chlamydia* is an **intracellular bacterium** and does not readily stain with Gram stain, explaining the negative result despite the presence of inflammation (neutrophils).
*Trichomonas vaginalis*
- While *Trichomonas vaginalis* can cause urethritis and discharge in men, it typically presents with **frothy yellow-green discharge** and is less common than *Chlamydia* in male urethritis.
- It would also likely be identifiable on a **wet mount microscopy** rather than just a Gram stain negative for bacteria.
*Neisseria gonorrhoeae*
- **Gonococcal urethritis** typically presents with a **purulent, thick discharge** and would show **Gram-negative diplococci** on Gram stain, which are absent in this case.
- The Gram stain finding of "negative for bacteria" specifically rules out *Neisseria gonorrhoeae*.
*Staphylococcus saprophyticus*
- *Staphylococcus saprophyticus* is a common cause of **urinary tract infections (UTIs)**, especially in young women, but less commonly causes urethritis with discharge in men.
- If present, it would likely be detected on a standard **Gram stain** and culture as **Gram-positive cocci**.
*Escherichia coli*
- *Escherichia coli* is the most common cause of **UTIs** but typically causes **cystitis** or **pyelonephritis** rather than isolated urethritis with discharge in men, unless associated with specific risk factors.
- It would appear as **Gram-negative rods** on Gram stain if it were the causative agent and would typically result in a positive bacterial finding.
Ehrlichia and Anaplasma US Medical PG Question 10: A 23-year-old male comes to the physician because of a 2-week history of fatigue, muscle aches, and a dry cough. He has also had episodes of painful, bluish discoloration of the tips of his fingers, nose, and earlobes during this period. Three months ago, he joined the military and attended basic training in southern California. He does not smoke or use illicit drugs. His temperature is 37.8°C (100°F). Physical examination shows mildly pale conjunctivae and annular erythematous lesions with a dusky central area on the extensor surfaces of the lower extremities. Which of the following is the most likely causal organism?
- A. Chlamydophila pneumoniae
- B. Streptococcus pneumoniae
- C. Mycoplasma pneumoniae (Correct Answer)
- D. Adenovirus
- E. Influenza virus
Ehrlichia and Anaplasma Explanation: ***Mycoplasma pneumoniae***
- This patient's symptoms (fatigue, muscle aches, dry cough, slightly elevated temperature, and **erythema multiforme**-like lesions) are characteristic of **atypical pneumonia**. The **Raynaud-like phenomenon** (bluish discoloration of fingertips, nose, earlobes) and recent military basic training environment are highly suggestive of *Mycoplasma pneumoniae* infection.
- *Mycoplasma pneumoniae* is a common cause of **atypical pneumonia**, especially in crowded settings like military barracks, and is associated with extrapulmonary manifestations such as **Raynaud's phenomenon**, **hemolytic anemia** (suggested by pale conjunctivae), and **erythema multiforme**.
*Chlamydophila pneumoniae*
- This organism also causes **atypical pneumonia** with a dry cough and constitutional symptoms but is less commonly associated with the prominent extrapulmonary findings like **Raynaud's phenomenon** and **erythema multiforme** seen in this patient.
- While it can cause pharyngitis and hoarseness, the constellation of symptoms, particularly the cutaneous and vascular manifestations, points away from *Chlamydophila pneumoniae*.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* typically causes **typical bacterial pneumonia**, characterized by a **productive cough**, high fever, chills, and often **lobar consolidation** on chest X-ray.
- It is not associated with **Raynaud's phenomenon**, **erythema multiforme**, or the specific demographic and exposure history (military basic training for atypical presentation) described.
*Adenovirus*
- **Adenovirus** can cause **respiratory tract infections**, including pharyngitis, conjunctivitis, and pneumonia, often seen in outbreaks in crowded settings.
- However, it is less commonly associated with the dramatic extrapulmonary manifestations like **Raynaud's phenomenon** and **erythema multiforme** that are prominent in this case.
*Influenza virus*
- **Influenza virus** causes a **respiratory illness** with fever, myalgia, fatigue, and cough, but **dry cough** is more common.
- While it can lead to pneumonia, the presence of **Raynaud's phenomenon** and **erythema multiforme** is not a typical presentation of influenza.
More Ehrlichia and Anaplasma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.