Chlamydia psittaci US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Chlamydia psittaci. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Chlamydia psittaci US Medical PG Question 1: A 16-year-old male with no significant past medical, surgical, or family history presents to his pediatrician with new symptoms following a recent camping trip. He notes that he went with a group of friends and 1 other group member is experiencing similar symptoms. Over the past 5 days, he endorses significant flatulence, nausea, and greasy, foul-smelling diarrhea. He denies tenesmus, urgency, and bloody diarrhea. The blood pressure is 118/74 mm Hg, heart rate is 88/min, respiratory rate is 14/min, and temperature is 37.0°C (98.6°F). Physical examination is notable for mild, diffuse abdominal tenderness. He has no blood in the rectal vault. What is the patient most likely to report about his camping activities?
- A. The patient camped as a side excursion from a cruise ship.
- B. The patient camped in Mexico.
- C. This has been going on for months.
- D. Recent antibiotic prescription
- E. Collecting water from a stream, without boiling or chemical treatment (Correct Answer)
Chlamydia psittaci Explanation: ***Collecting water from a stream, without boiling or chemical treatment***
- The patient's symptoms of **greasy, foul-smelling diarrhea**, flatulence, and nausea following a camping trip are highly suggestive of **giardiasis**.
- **Giardiasis** is commonly acquired through the consumption of untreated **contaminated water**, often from streams or lakes in wilderness areas.
*The patient camped as a side excursion from a cruise ship.*
- While cruise ships can be sources of infectious outbreaks, the specific symptoms of **greasy, foul-smelling diarrhea** are less typical for common cruise-associated infections.
- Furthermore, cruise-related illnesses are usually associated with cruise ship facilities rather than **wilderness camping** directly.
*The patient camped in Mexico.*
- Traveling to Mexico is a risk factor for **traveler's diarrhea**, often caused by bacterial pathogens like ***E. coli***.
- However, typical traveler's diarrhea tends to be watery, occasionally bloody, and often presents with fever, which is not consistent with the patient's symptoms of **greasy, foul-smelling diarrhea** and absence of fever.
*This has been going on for months.*
- The symptoms are described as **new** and have developed over the past 5 days following a recent camping trip, indicating an **acute onset**, not a chronic condition.
- Chronic diarrhea lasting for months would point towards other persistent or long-term gastrointestinal issues, not an acute infection from a recent exposure.
*Recent antibiotic prescription*
- Recent antibiotic use can lead to **antibiotic-associated diarrhea**, most notably ***Clostridioides difficile*** infection.
- However, this patient has no history of recent antibiotic prescription, and the specific symptom of **greasy, foul-smelling diarrhea** is not characteristic of *C. difficile* infection.
Chlamydia psittaci US Medical PG Question 2: An 18-year-old male in his first year of college presents to the emergency room with a fever and a severe headache. He reports having unprotected sex with several partners over the past few weeks. Upon examination, the male demonstrates nuchal rigidity and photophobia. His past medical history is notable for a lack of vaccinations beginning from infancy due to his parents' belief that vaccinations may cause autism. The bacteria causing these symptoms would most likely demonstrate which of the following?
- A. Negative catalase test
- B. Gram-negative bacteria (Correct Answer)
- C. Urease positive
- D. Positive quellung reaction
- E. Lactose fermentation
Chlamydia psittaci Explanation: ***Gram-negative bacteria***
- The clinical picture of fever, severe headache, **nuchal rigidity**, and photophobia in an unvaccinated 18-year-old college student strongly suggests **bacterial meningitis** caused by *Neisseria meningitidis*.
- *Neisseria meningitidis* is a **Gram-negative diplococcus**, which is the most definitive laboratory characteristic for identifying this organism.
- College dormitory settings and unvaccinated status are major risk factors for **meningococcal meningitis**, and Gram stain is typically the first diagnostic step showing Gram-negative diplococci in CSF.
*Positive quellung reaction*
- The Quellung reaction (capsular swelling) is classically associated with **Streptococcus pneumoniae**, not *Neisseria meningitidis*.
- While *N. meningitidis* does have a polysaccharide capsule, the Quellung test is not the standard identification method for this organism.
- *S. pneumoniae* would be more common in older adults or those with specific risk factors like asplenia.
*Negative catalase test*
- *Neisseria meningitidis* is **catalase-positive**, so a negative catalase test would rule out this organism.
- Catalase-negative organisms include Streptococcus and Enterococcus species, which have different clinical presentations.
*Lactose fermentation*
- *Neisseria meningitidis* is a **non-lactose fermenter** and does not utilize lactose fermentation for energy.
- Lactose fermentation is characteristic of enteric Gram-negative bacteria like *E. coli* and *Klebsiella*, not Neisseria species.
- *N. meningitidis* ferments **maltose and glucose**, which distinguishes it from *N. gonorrhoeae* (glucose only).
*Urease positive*
- *Neisseria meningitidis* is **urease-negative**, so urease positivity would rule out this organism.
- Urease-positive bacteria include *Helicobacter pylori*, *Proteus* species, and *Klebsiella*, none of which typically cause meningitis in this clinical setting.
Chlamydia psittaci US Medical PG Question 3: A 58-year-old woman visits a physician because of fever, chills, dry cough, and a few enlarging masses on her cheeks and neck. Wart-like lesions are present on the nose as shown in the photograph. She reports that she visited the Mississippi area a few months before on a business trip. Her temperature is 38.1°C (100.6°F), the pulse is 80/min, and the blood pressure is 121/78 mm Hg. A fine needle aspirate of the lymph node is sent for pathological investigation. Culture growth shows white colonies on Sabouraud glucose agar (SGA). Which of the following is the most likely causal organism?
- A. Histoplasma capsulatum
- B. Malassezia furfur
- C. Blastomyces dermatitidis (Correct Answer)
- D. Coccidioides immitis
- E. Aspergillus fumigatus
Chlamydia psittaci Explanation: ***Blastomyces dermatitidis***
- The patient's symptoms, including **fever, chills, dry cough, enlarging masses on cheeks and neck, and wart-like lesions on the nose**, along with a history of travel to the **Mississippi area**, are highly characteristic of **blastomycosis**.
- **_Blastomyces dermatitidis_** is a dimorphic fungus endemic to the **Ohio and Mississippi River valleys** and the Great Lakes region, often causing pulmonary disease that can disseminate to the skin, bones, and other organs, producing lesions such as those described.
*Histoplasma capsulatum*
- This fungus is also endemic to the **Ohio and Mississippi River valleys** but typically causes **histoplasmosis**, which often presents with asymptomatic lung infection, or in severe cases, disseminated disease with **hepatosplenomegaly** and **oral ulcers**, rather than aggressive cutaneous **wart-like lesions**.
- While it can cause pulmonary symptoms, the prominent **skin lesions** and masses described are less typical for disseminated histoplasmosis compared to **blastomycosis**.
*Malassezia furfur*
- **_Malassezia furfur_** is associated with superficial fungal infections like **tinea versicolor** (pityriasis versicolor), which presents as hypopigmented or hyperpigmented patches on the skin, mainly on the trunk and upper extremities.
- It does not typically cause **deep-seated infections** with systemic symptoms (fever, chills, cough) or **wart-like lesions** on the nose and neck masses.
*Coccidioides immitis*
- **_Coccidioides immitis_** is endemic to the **southwestern United States** (e.g., California, Arizona) and is the causative agent of **Coccidioidomycosis** (Valley Fever).
- While it can cause pulmonary symptoms and disseminate, the classic dermatological manifestations are often **erythema nodosum** or **erythema multiforme**, not the wart-like, verrucous lesions described in this case, and its endemic region does not fit the patient's travel history to Mississippi.
*Aspergillus fumigatus*
- **_Aspergillus fumigatus_** is an opportunistic mold that primarily causes allergic bronchopulmonary aspergillosis (ABPA), aspergilloma (fungus ball in pre-existing lung cavities), or invasive aspergillosis in **immunocompromised individuals**.
- It is not typically associated with cutaneous **wart-like lesions** or the specific endemic pattern and systemic symptoms described in an otherwise seemingly immunocompetent individual in the Mississippi region.
Chlamydia psittaci US Medical PG Question 4: A 23-year-old woman presents to the emergency department with abnormal vaginal discharge and itchiness. She states it started a few days ago and has been worsening. The patient has a past medical history of a medical abortion completed 1 year ago. Her temperature is 98.6°F (37.0°C), blood pressure is 129/68 mmHg, pulse is 80/min, respirations are 14/min, and oxygen saturation is 99% on room air. Physical exam demonstrates an anxious woman. Pelvic exam reveals yellow cervical discharge. Nucleic acid amplification test is negative for Neisseria species. Which of the following is the best next step in management?
- A. Ceftriaxone
- B. Azithromycin and ceftriaxone
- C. Fluconazole
- D. Azithromycin (Correct Answer)
- E. Cervical cultures
Chlamydia psittaci Explanation: ***Azithromycin***
- A **yellow cervical discharge** and **negative *Neisseria* species NAAT** strongly suggest a *Chlamydia trachomatis* infection, for which azithromycin is a first-line treatment.
- Given the patient's symptoms of **vaginal discharge and itchiness**, along with the high prevalence of chlamydia, empirical treatment is appropriate while awaiting further test results.
*Ceftriaxone*
- This antibiotic is primarily used to treat **gonorrhea**, which has been ruled out by the negative *Neisseria* NAAT.
- While sometimes given in combination therapy, it is not the best single agent in this scenario.
*Azithromycin and ceftriaxone*
- This combination is typically used for **empirical treatment of cervicitis** when both gonorrhea and chlamydia are suspected.
- However, since **gonorrhea has been excluded** by NAAT, adding ceftriaxone is unnecessary at this point.
*Fluconazole*
- Fluconazole is an **antifungal medication** used to treat **yeast infections** (*Candida* species).
- While the patient reports itchiness, a **yellow discharge** is more characteristic of a bacterial infection like chlamydia, rather than the typically white, cottage-cheese-like discharge of a yeast infection.
*Cervical cultures*
- While collecting cervical cultures for other pathogens (e.g., **Trichomonas**) might be considered, the immediate priority in a symptomatic patient with suspected chlamydia is to **initiate treatment to prevent complications** and reduce transmission.
- **NAATs are highly sensitive and specific** for chlamydia and gonorrhea, making them preferred over traditional cultures for these infections.
Chlamydia psittaci US Medical PG Question 5: An investigator is studying the growth of an organism in different media. The organism is inoculated on a petri dish that contains heated sheep blood, vancomycin, nystatin, trimethoprim, and colistin. The resulting growth medium is incubated at 37°C. Numerous small, white colonies are seen after incubation for 48 hours. This organism is most likely to cause which of the following conditions?
- A. Pontiac fever
- B. Pseudomembranous colitis
- C. Hemolytic uremic syndrome
- D. Oral thrush
- E. Gonorrhea (Correct Answer)
Chlamydia psittaci Explanation: ***Gonorrhea***
- The growth medium described is **Thayer-Martin agar**, a selective medium containing **heated sheep blood** (supplies NAD+), **vancomycin** (inhibits Gram-positives), **colistin** (inhibits Gram-negatives), **nystatin** (inhibits fungi), and **trimethoprim** (inhibits Proteus). This medium is specifically designed for the isolation of *Neisseria gonorrhoeae* from polymicrobial samples.
- *Neisseria gonorrhoeae* typically grows as **small, translucent-to-white colonies** on selective media like Thayer-Martin agar, and incubation at 37°C in CO2 (not explicitly mentioned but often required) for 24-48 hours yields visible growth, causing **gonorrhea**.
*Pontiac fever*
- Pontiac fever is a mild, self-limiting form of **legionellosis**, caused by *Legionella pneumophila*.
- *Legionella* requires a specialized medium such as **buffered charcoal yeast extract (BCYE) agar** for growth, not Thayer-Martin agar.
*Pseudomembranous colitis*
- This condition is caused by **toxin-producing *Clostridioides difficile***, often after antibiotic use.
- *C. difficile* is an obligate anaerobe and requires **anaerobic conditions** and specific selective media (e.g., CCFA agar) for isolation, not Thayer-Martin agar under aerobic conditions.
*Hemolytic uremic syndrome*
- Hemolytic uremic syndrome (HUS) is often caused by **Shiga toxin-producing *Escherichia coli* (STEC)**, particularly O157:H7.
- STEC can be isolated on media like **sorbitol MacConkey agar (SMAC)**, where O157:H7 appears as non-sorbitol fermenting colonies, distinct from the growth seen on Thayer-Martin.
*Oral thrush*
- Oral thrush is caused by *Candida albicans*, a yeast.
- *Candida* would be inhibited by **nystatin** in the Thayer-Martin medium, which is an antifungal agent.
Chlamydia psittaci US Medical PG Question 6: A 27-year-old woman visits your office with a 3-day complaint of fever, malaise, myalgias, and headaches associated with vulvar itching, vulvar soreness, dysuria, and urethral discharge. The pain when urinating is so severe that she has attempted to avoid the use of the toilet. She just returned from a spring break in the tropics and explains that she had multiple unprotected sexual encounters with men and women. Upon physical examination, the temperature was 38.7°C (101.6°F) and the heart rate was 90/min. The pelvic examination revealed vulvar ulcers, vulvar excoriations, erythema, vaginal mucosa edema, and ulcerative cervicitis. Which of the following will best aid you in the identification of the specific organism causing the above symptoms?
- A. Location of the lesions
- B. Culture in Thayer-Martin agar
- C. Direct fluorescence antigen (Correct Answer)
- D. Serology
- E. Tzanck smear
Chlamydia psittaci Explanation: ***Direct fluorescence antigen***
- A **direct fluorescence antigen (DFA)** test can rapidly identify viral antigens from the lesions, specifically for **Herpes Simplex Virus (HSV)**, which is highly suspected given the patient's symptoms (fever, malaise, myalgias, vulvar ulcers, dysuria, and recent unprotected sexual encounters).
- **HSV** is a common cause of genital ulcers, and DFA offers a quick, sensitive, and specific method for detection directly from clinical samples.
*Location of the lesions*
- While the **location of the lesions** (vulvar ulcers) is characteristic of several sexually transmitted infections (STIs), it is not specific enough to identify the *specific organism* without further laboratory testing.
- Conditions like syphilis, chancroid, and HSV all cause genital ulcers, making location alone insufficient for definitive diagnosis.
*Culture in Thayer-Martin agar*
- **Thayer-Martin agar** is selectively used for culturing **Neisseria gonorrhoeae**, which causes gonorrhea.
- Although the patient has urethral discharge and dysuria, the presence of **vulvar ulcers** and systemic symptoms like fever and myalgias point away from uncomplicated gonorrhea.
*Serology*
- **Serology** detects antibodies to pathogens, indicating past or present infection, but is often less useful for identifying the *acute* causative organism in the initial stages of a symptomatic outbreak like this one.
- For instance, HSV serology can distinguish between HSV-1 and HSV-2 exposure but does not confirm active infection in the way direct antigen methods or PCR do.
*Tzanck smear*
- A **Tzanck smear** can reveal characteristic **multinucleated giant cells** and **intranuclear inclusions**, which are indicative of herpesvirus infections (HSV or VZV).
- However, it is less sensitive and specific than a direct fluorescence antigen test or PCR, and results can be variable depending on the quality of the smear and interpretation.
Chlamydia psittaci US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Chlamydia psittaci Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Chlamydia psittaci US Medical PG Question 8: A previously healthy 24-year-old woman comes to the physician because of fever, headache, myalgia, photophobia, and a nonproductive cough for 2 days. Three weeks ago, she received a parrot as a birthday present. Her temperature is 38.5°C (101.3°F). Pulmonary examination shows crackles at both lung bases. Her leukocyte count is 8,000/mm3. An x-ray of the chest shows diffuse patchy infiltrates that are most prominent in the lower lobes. Which of the following is the most likely causal organism?
- A. Cryptococcus neoformans
- B. Francisella tularensis
- C. Babesia microti
- D. Chlamydia psittaci (Correct Answer)
- E. Leptospira interrogans
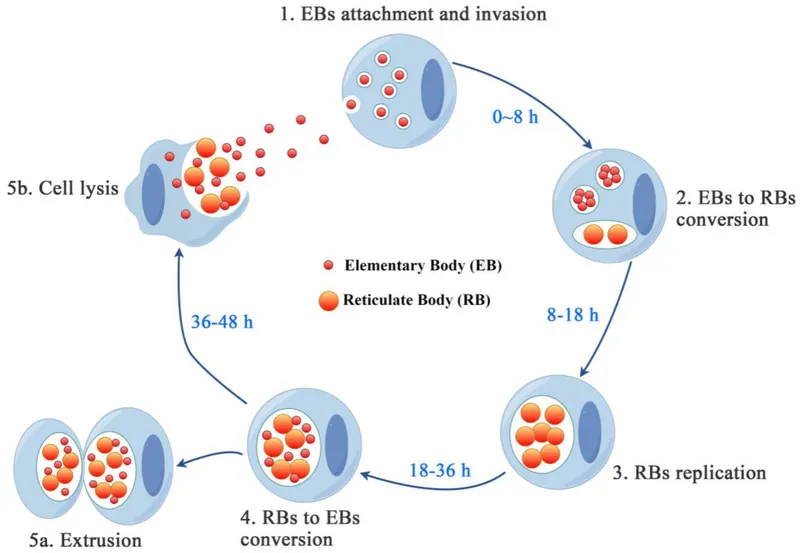
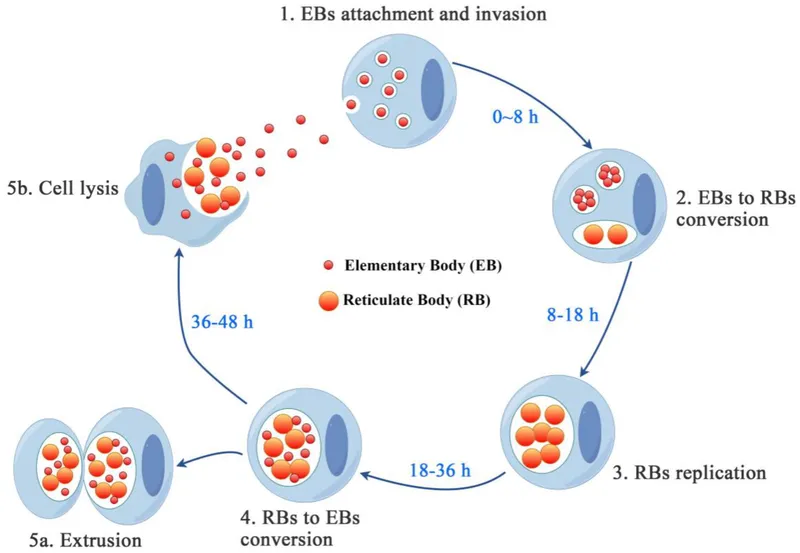
Chlamydia psittaci Explanation: ***Chlamydia psittaci***
- The patient's recent acquisition of a **parrot** and subsequent development of **fever, headache, myalgia, photophobia, nonproductive cough**, and **diffuse patchy infiltrates** on CXR are highly characteristic of **psittacosis** (ornithosis), caused by *Chlamydia psittaci*.
- This **atypical pneumonia** often presents with systemic symptoms out of proportion to respiratory findings and can mimic other viral illnesses.
*Cryptococcus neoformans*
- This is a **fungal infection** typically affecting immunocompromised individuals, causing **meningitis** or **pulmonary infections**.
- While it can cause pneumonia, the direct link to a parrot and the specific constellation of symptoms point away from *Cryptococcus* in an otherwise healthy individual.
*Francisella tularensis*
- This bacterium causes **tularemia**, often associated with **rabbit or rodent exposure** or **tick bites**.
- It presents with fever, ulceroglandular or pneumonic forms, but a history of parrot exposure makes it unlikely.
*Babesia microti*
- This is an **intraerythrocytic parasite** transmitted by **ticks**, causing **babesiosis**.
- Symptoms include fever, hemolytic anemia, and fatigue, but it does not typically cause the described respiratory symptoms or diffuse patchy infiltrates.
*Leptospira interrogans*
- This spirochete causes **leptospirosis**, an infection associated with **exposure to animal urine** or contaminated water.
- While it can present with fever, headache, and myalgia, the prominent respiratory symptoms and the specific parrot exposure do not fit well with leptospirosis, which more commonly involves liver and kidney dysfunction.
Chlamydia psittaci US Medical PG Question 9: A 32-year-old man comes to the physician because of severe burning with urination for the past 3 days. During this period, he has had clear urethral discharge early in the morning. He has no history of serious illness, except for a rash following treatment with erythromycin 20 years ago. The patient takes no medications. He is sexually active with one male and one female partner; they use condoms inconsistently. His younger brother was diagnosed with Crohn disease at the age of 24 years. The patient does not smoke. He drinks one to two beers on weekends. He appears well. Temperature is 36.8°C (98°F), pulse is 75/min, and blood pressure is 135/78 mm Hg. Physical examination shows no abnormalities. Gram stain of a urethral swab shows neutrophils but no organisms. Which of the following is the most likely causal pathogen?
- A. Adenovirus
- B. Herpes simplex virus
- C. Neisseria gonorrhoeae
- D. Chlamydia trachomatis (Correct Answer)
- E. Trichomonas vaginalis
Chlamydia psittaci Explanation: ***Chlamydia trachomatis***
- The presentation of **dysuria** (burning with urination), **clear urethral discharge**, and a **Gram stain showing neutrophils but no organisms** is highly characteristic of **non-gonococcal urethritis**, with *Chlamydia trachomatis* being the most common cause.
- The patient's **inconsistent condom use** and **multiple sexual partners** increase the risk of sexually transmitted infections like chlamydia.
*Adenovirus*
- Adenovirus can cause **urethritis**, but it is more commonly associated with symptoms like **pharyngitis**, **conjunctivitis**, and **acute respiratory disease**.
- While it can cause clear discharge, the clinical picture is more suggestive of a common STI.
*Herpes simplex virus*
- Herpes simplex virus (HSV) typically causes **painful genital ulcers or vesicles**, not primarily clear urethral discharge, although it can cause dysuria if the urethra is involved.
- The absence of external lesions and the presence of persistent discharge make HSV less likely.
*Neisseria gonorrhoeae*
- **Gonococcal urethritis** typically presents with a **purulent** (creamy, yellow, or greenish) urethral discharge and frequently shows **Gram-negative intracellular diplococci** on microscopy.
- The **clear discharge** and **absence of organisms** on Gram stain rule out *Neisseria gonorrhoeae* as the cause of this presentation.
*Trichomonas vaginalis*
- *Trichomonas vaginalis* can cause **urethritis** with discharge, but the discharge is typically described as **frothy**, **yellowish-green**, and associated with **itching**.
- While Gram stain might show neutrophils without other organisms, the classic discharge description and common co-occurrence with vaginitis in female partners are not present.
Chlamydia psittaci US Medical PG Question 10: A 27-year-old man comes to the physician with throbbing right scrotal pain for 1 day. He has also had a burning sensation on urination during the last 4 days. He is sexually active with multiple female partners and does not use condoms. Physical examination shows a tender, palpable swelling on the upper pole of the right testicle; lifting the testicle relieves the pain. A Gram stain of urethral secretions shows numerous polymorphonuclear leukocytes but no organisms. Which of the following is the most likely causal pathogen of this patient's symptoms?
- A. Mycobacterium tuberculosis
- B. Pseudomonas aeruginosa
- C. Mumps virus
- D. Chlamydia trachomatis (Correct Answer)
- E. Staphylococcus aureus
Chlamydia psittaci Explanation: ***Chlamydia trachomatis***
- The patient's presentation with **epididymitis** (scrotal pain, tender palpable swelling on the upper pole of the testicle), **dysuria**, and a history of **multiple sexual partners without condoms** is classic for a sexually transmitted infection.
- **Positive Prehn's sign** (pain relief with testicular elevation) supports epididymitis over testicular torsion.
- The Gram stain showing **numerous polymorphonuclear leukocytes but no organisms** is highly suggestive of *C. trachomatis* infection, as it is an **obligate intracellular bacterium** that does not readily stain with Gram stain.
- This finding distinguishes it from *Neisseria gonorrhoeae* (the other common cause of STI-related epididymitis in young men), which would appear as **Gram-negative intracellular diplococci**.
*Mycobacterium tuberculosis*
- **Tuberculosis epididymitis** is rare in developed countries and typically presents with a more **insidious onset** over weeks to months, not acute onset over 1 day.
- It may involve caseating granulomas and is more common in immunocompromised patients.
- It would not explain the acute dysuria or the Gram stain findings of PMNs without organisms in a patient with risk factors for common STIs.
*Pseudomonas aeruginosa*
- **Pseudomonas epididymitis** is typically seen in older men (>35 years), those with urinary tract abnormalities, or after instrumentation/catheterization.
- It is uncommon in young, sexually active individuals without these risk factors.
- Gram stain would show **Gram-negative rods**, which is inconsistent with the "no organisms" finding.
*Mumps virus*
- **Mumps orchitis** typically presents with **testicular pain and swelling** (affecting the testis itself, not the epididymis).
- Mumps orchitis is usually preceded by **parotitis** (salivary gland swelling) 4-8 days earlier.
- It does not typically cause dysuria or lead to urethral secretions with PMNs.
- Mumps is now rare due to widespread MMR vaccination.
*Staphylococcus aureus*
- **Staphylococcus aureus** can cause epididymitis, especially in cases of direct trauma, hematogenous spread, or in patients with indwelling catheters.
- However, it's not a common cause of sexually transmitted epididymitis in young, healthy men.
- A Gram stain would reveal **Gram-positive cocci in clusters**, which was not seen in this case.
More Chlamydia psittaci US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.