Borrelia species US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Borrelia species. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
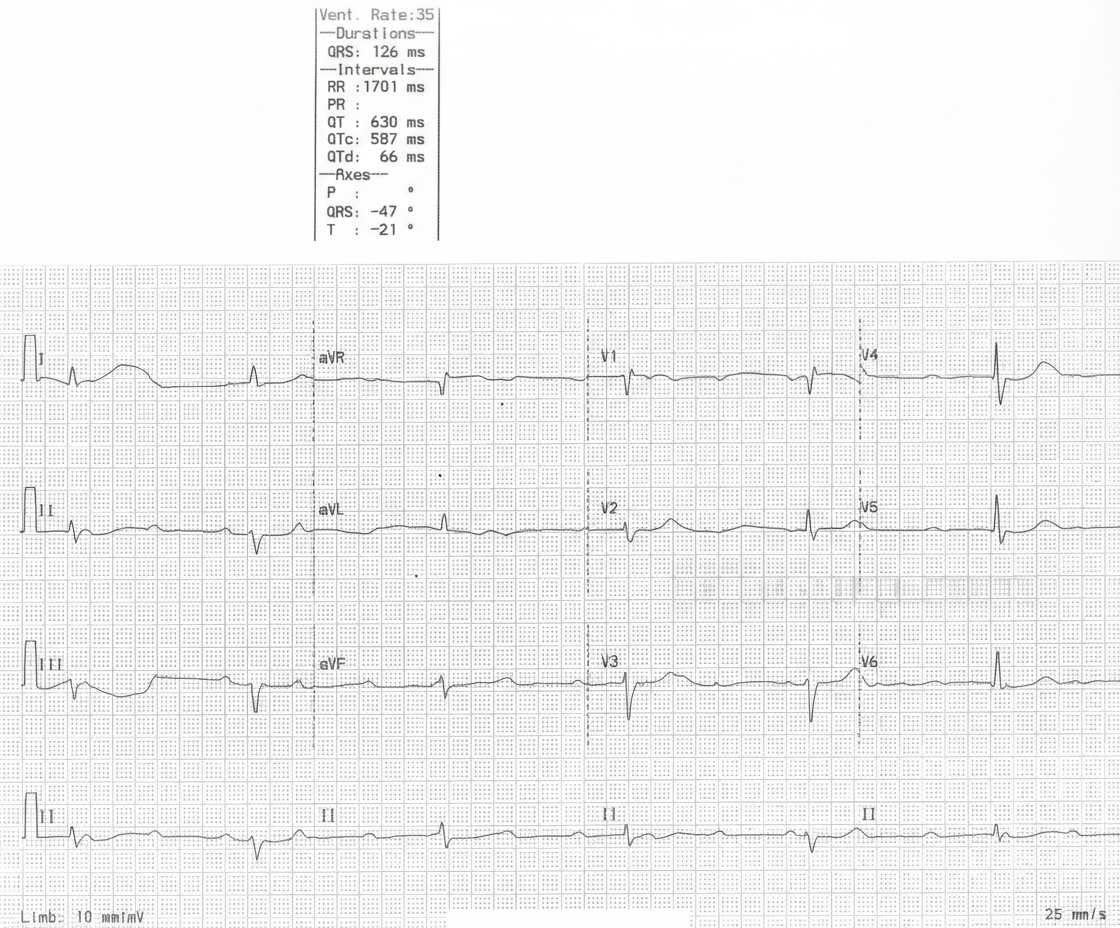
Borrelia species US Medical PG Question 1: A 29-year-old woman is brought to the emergency department after an episode of syncope. For the past 10 days, she has had dyspnea and palpitations occurring with mild exertion. The patient returned from a hiking trip in Upstate New York 5 weeks ago. Except for an episode of flu with fever and chills a month ago, she has no history of serious illness. Her temperature is 37.3°C (99.1°F), pulse is 45/min, respirations are 21/min, and blood pressure is 148/72 mm Hg. A resting ECG is shown. Two-step serological testing confirms the diagnosis. Which of the following is the most appropriate treatment?
- A. Intravenous ceftriaxone (Correct Answer)
- B. Atropine
- C. Oral doxycycline
- D. Beta blocker
- E. Permanent pacemaker implantation
Borrelia species Explanation: ***Intravenous ceftriaxone***
- The patient's symptoms (syncope, dyspnea, palpitations, travel history to Upstate New York, prior flu-like illness) and **bradycardia (pulse 45/min)** with the ECG findings strongly suggest **Stage II Lyme carditis** (AV block).
- **Intravenous ceftriaxone** is the recommended treatment for **severe Lyme disease manifestations**, including **Lyme carditis with high-grade AV block**, due to its excellent penetration and efficacy against *Borrelia burgdorferi*.
*Atropine*
- Atropine is used for **acute symptomatic bradycardia** to temporarily increase heart rate but does not treat the underlying cause of Lyme carditis.
- Its effect is **transient**, and it's not a definitive therapy for persistent bradycardia due to infection.
*Oral doxycycline*
- **Oral doxycycline** is appropriate for **early-stage Lyme disease** (e.g., erythema migrans, mild facial palsy) or **mild Lyme carditis** without high-grade AV block.
- Given the **high-grade AV block** (implied by bradycardia and syncope) and the need for prompt management of severe manifestations, intravenous therapy is preferred.
*Beta blocker*
- Beta blockers **slow the heart rate** and are contraindicated in patients with **symptomatic bradycardia** or **high-grade AV block**.
- Administering a beta blocker would worsen the patient's condition by exacerbating the existing bradycardia.
*Permanent pacemaker implantation*
- While a **temporary pacemaker** might be considered for **life-threatening bradycardia** not responding to medical therapy in Lyme carditis, **permanent pacemaker implantation** is typically reserved for **irreversible, persistent AV block**.
- In Lyme carditis, the AV block **often resolves with appropriate antibiotic treatment**, making a permanent pacemaker unnecessary in most cases.
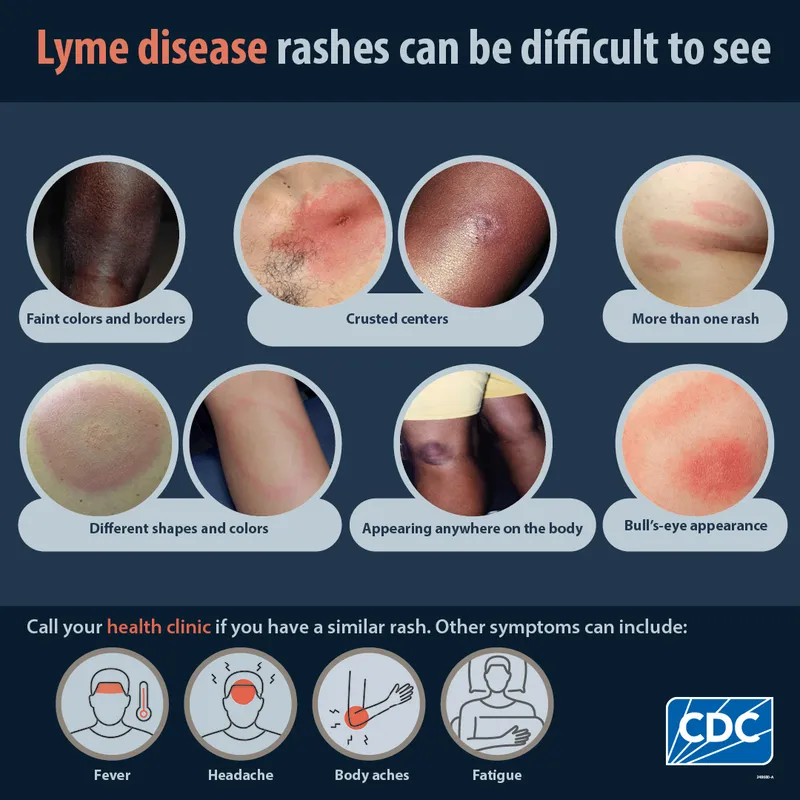
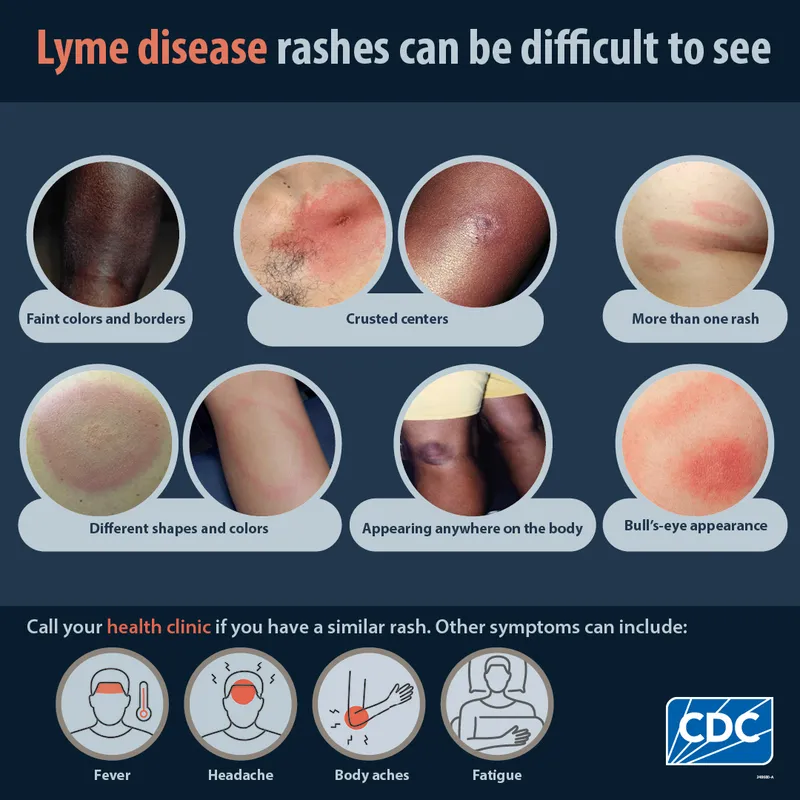
Borrelia species US Medical PG Question 2: A 45-year-old woman presents to the emergency department with a headache, fevers with chills, rigors, and generalized joint pain for the past week. She also complains of a progressive rash on her left arm. She says that a few days ago she noticed a small, slightly raised lesion resembling an insect bite mark, which had a burning sensation. The medical and surgical histories are unremarkable. She recalls walking in the woods 2 weeks prior to the onset of symptoms, but does not recall finding a tick on her body. On examination, the temperature is 40.2°C (104.4°F). A circular red rash measuring 10 cm x 5 cm in diameter is noted on the left arm, as shown in the accompanying image. The remainder of her physical examination is unremarkable. The tick causing her disease is also responsible for the transmission of which of the following pathogens?
- A. Rickettsia rickettsii
- B. Babesia microti (Correct Answer)
- C. Rickettsia typhi
- D. Ehrlichia
- E. Plasmodium vivax
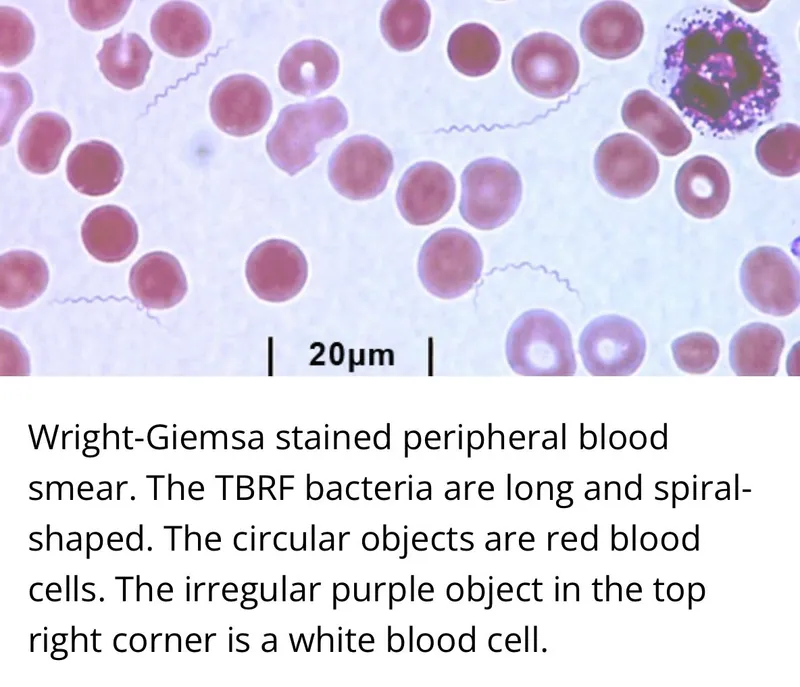
Borrelia species Explanation: ***Babesia microti***
- The clinical picture of **headache**, **fever with chills**, **rigors**, **generalized joint pain**, and an **expanding erythematous rash (erythema migrans)** after a woodland exposure points to **Lyme disease**, caused by *Borrelia burgdorferi*.
- **Both *Borrelia burgdorferi*** and ***Babesia microti*** are transmitted by the **deer tick** (*Ixodes scapularis*), making co-infection common in endemic areas.
*Rickettsia rickettsii*
- This pathogen causes **Rocky Mountain spotted fever**, which typically presents with a **maculopapular rash** that often becomes petechial and involves the palms and soles.
- The rash in this vignette is an **expanding erythematous lesion (erythema migrans)**, characteristic of Lyme disease, not RMSF.
*Rickettsia typhi*
- This bacterium causes **endemic (murine) typhus**, typically transmitted by the **infected flea** (*Xenopsylla cheopis*).
- Symptoms include fever, headache, and a **truncal maculopapular rash**, but it is not associated with a tick bite or erythema migrans.
*Ehrlichia*
- *Ehrlichia chaffeensis* causes **human monocytic ehrlichiosis**, transmitted by the **lone star tick** (*Amblyomma americanum*).
- While it can cause fever, headache, and myalgia, it does not typically present with the classic **erythema migrans rash** seen in Lyme disease.
*Plasmodium vivax*
- This protozoan causes **malaria**, transmitted by the **Anopheles mosquito**.
- Symptoms include cyclical fevers, chills, and headache but do not involve a tick bite or the characteristic **erythema migrans rash**.
Borrelia species US Medical PG Question 3: A 21-year-old man comes to the physician's office due to a 3-week history of fatigue and a rash, along with the recent development of joint pain that has moved from his knee to his elbows. The patient reports going camping last month but denies having been bitten by a tick. His past medical history is significant for asthma treated with an albuterol inhaler. His pulse is 54/min and blood pressure is 110/72. Physical examination reveals multiple circular red rings with central clearings on the right arm and chest. There is a normal range of motion in all joints and 5/5 strength bilaterally in the upper and lower extremities. Without proper treatment, the patient is at highest risk for which of the following complications?
- A. Liver capsule inflammation
- B. Bone marrow failure
- C. Heart valve stenosis
- D. Glomerular damage
- E. Cranial nerve palsy (Correct Answer)
Borrelia species Explanation: ***Cranial nerve palsy***
- This patient presents with classic **Lyme disease** (caused by *Borrelia burgdorferi*), including camping exposure, fatigue, migratory arthralgia, and **erythema migrans** (multiple circular red rings with central clearings on the arm and chest).
- The **bradycardia (pulse 54/min)** suggests early **Lyme carditis** with possible first-degree AV block, which typically resolves with treatment and rarely progresses to complete heart block in treated cases.
- Without proper antibiotic treatment, **cranial neuropathy** is one of the most common neurological complications in early disseminated Lyme disease, with **facial nerve palsy (Bell's palsy)** being the most frequent, occurring in up to 10% of untreated patients.
- Other neurological complications include meningitis, radiculoneuropathy, and peripheral neuropathy, making neurologic involvement a significant risk in untreated disease.
*Liver capsule inflammation*
- **Perihepatitis (Fitz-Hugh-Curtis syndrome)** is associated with **pelvic inflammatory disease (PID)** caused by *Chlamydia trachomatis* or *Neisseria gonorrhoeae*, not Lyme disease.
- This presents with right upper quadrant pain and "violin string" adhesions between the liver capsule and peritoneum.
*Bone marrow failure*
- **Bone marrow failure** (aplastic anemia) can be caused by parvovirus B19, certain medications, radiation, or idiopathic causes, but is **not a recognized complication of Lyme disease**.
- Lyme disease primarily affects the skin, joints, heart (conduction system), and nervous system, not hematopoietic function.
*Heart valve stenosis*
- **Lyme carditis** affects the **cardiac conduction system**, causing **AV blocks** (first, second, or third degree) and myocarditis, as suggested by this patient's bradycardia.
- Lyme does **not cause valvular stenosis or regurgitation**. Valvular disease is associated with rheumatic fever (post-streptococcal), endocarditis, or degenerative changes.
- The cardiac manifestations of Lyme typically resolve with appropriate antibiotic therapy and rarely cause permanent structural damage.
*Glomerular damage*
- **Glomerulonephritis** is not a typical complication of Lyme disease in humans (though "Lyme nephritis" occurs in dogs).
- Renal involvement in human Lyme disease is extremely rare and not a significant clinical concern compared to neurological, cardiac, or rheumatological manifestations.
Borrelia species US Medical PG Question 4: A 14-year-old girl presents with fever, headache, and muscle aches that have lasted for 2 days. She also complains of malaise and pain in her joints. She says she just returned from a camping trip in Delaware. Her past medical history is not significant. The patient denies any recent sick contacts. Her temperature is 38.3°C (101.0°F), pulse is 87/min, respirations are 17/min, and blood pressure is 120/78 mm Hg. On physical examination, there is a 3-inch-diameter, red, erythematous, round rash with central clearing on the right leg (see image). Antibodies against Proteus vulgaris OX-19 are absent. Which of the following is the most likely cause of this patient’s symptoms?
- A. Chlamydia trachomatis
- B. Dermatophytosis
- C. Rickettsia rickettsii
- D. Measles virus
- E. Borrelia burgdorferi (Correct Answer)
Borrelia species Explanation: ***Borrelia burgdorferi***
- The patient's symptoms (fever, headache, muscle aches, joint pain, malaise) coinciding with a recent camping trip in an endemic area for Lyme disease (Delaware), along with the characteristic **erythema migrans rash** (red, erythematous, round rash with central clearing), are highly suggestive of Lyme disease, caused by *Borrelia burgdorferi*.
- This **bull's-eye rash** is pathognomonic for Lyme disease and often appears within days to weeks of a tick bite.
*Chlamydia trachomatis*
- This bacterium primarily causes sexually transmitted infections (STIs) and can cause **conjunctivitis, urethritis, cervicitis**, or **pelvic inflammatory disease**.
- It does not typically cause a systemic febrile illness with a migratory rash or joint pain in this manner.
*Dermatophytosis*
- Dermatophytosis, or **ringworm**, is a fungal infection of the skin that can present with a red, annular rash.
- However, it is usually **itchy** and **scaly**, lacks the central clearing seen in erythema migrans, and typically does not cause systemic symptoms like fever, headache, and widespread muscle/joint aches.
*Rickettsia rickettsii*
- This is the causative agent of **Rocky Mountain spotted fever (RMSF)**, which also presents with fever, headache, and muscle aches following a tick bite.
- However, the rash of RMSF is typically a **maculopapular rash** that appears on the **wrists and ankles** and then spreads centrally, becoming petechial, and
- **Antibodies against Proteus vulgaris OX-19** (Weil-Felix test), which are used for diagnosis of Rickettsial infections, are absent in this case, ruling out RMSF.
*Measles virus*
- Measles (rubeola) is a highly contagious viral infection characterized by a prodrome of **fever, cough, coryza, and conjunctivitis**, followed by **Koplik spots** in the mouth.
- The rash of measles typically appears as a **maculopapular rash** that starts on the face and spreads downwards, which is distinct from the erythema migrans observed.
Borrelia species US Medical PG Question 5: A 28-year-old man presents with fever, chills, and malaise which began 5 days ago. He also mentions that the back of his right upper arm feels itchy. He says he works as a forest guide and recently came back from a forest expedition. Upon asking, he reports that the forest where he works is infested with ticks. His temperature is 38.3°C (100.9°F), the pulse is 87/min, the respiratory rate is 15/min, and the blood pressure is 122/90 mm Hg. On physical examination, there is a rash present on the posterior aspect of his upper right arm which is shown in the image. Which of the following medications is the best course of treatment for this patient?
- A. Clindamycin
- B. Doxycycline (Correct Answer)
- C. Trimethoprim-sulfamethoxazole
- D. Fluconazole
- E. Azithromycin
Borrelia species Explanation: ***Doxycycline***
- The patient's symptoms (fever, chills, malaise) combined with a history of **tick exposure** and the characteristic rash (likely **erythema migrans**) strongly suggest **Lyme disease**.
- **Doxycycline** is the first-line treatment for Lyme disease in adults due to its effectiveness against *Borrelia burgdorferi*, the spirochete causing the infection.
*Clindamycin*
- **Clindamycin** is an antibiotic primarily used for anaerobic infections and specific parasitic infections, and it is not the recommended treatment for Lyme disease.
- It does not effectively target *Borrelia burgdorferi* and would not be an appropriate choice for this patient.
*Trimethoprim-sulfamethoxazole*
- **Trimethoprim-sulfamethoxazole** is effective against various bacterial infections but is not recommended for the treatment of Lyme disease.
- Studies have shown it to be ineffective against *Borrelia burgdorferi* and should not be used.
*Fluconazole*
- **Fluconazole** is an antifungal medication, used to treat fungal infections such as candidiasis.
- It has no antibacterial activity and therefore would be ineffective against Lyme disease, which is a bacterial infection.
*Azithromycin*
- **Azithromycin** is a macrolide antibiotic that can be used for certain bacterial infections, and while it occasionally has some activity against *Borrelia burgdorferi*, it is generally considered less effective than doxycycline for Lyme disease.
- It may be considered in cases where doxycycline is contraindicated (e.g., pregnancy), but it is not the best first-line option.
Borrelia species US Medical PG Question 6: A 28-year-old man presents to the clinic complaining of chronic joint pain and fatigue for the past 2 months. The patient states that he usually has pain in one of his joints that resolve but then seems to move to another joint. The patient notes no history of trauma but states that he has experienced some subjective fevers over that time. He works as a logger and notes that he's heard that people have also had these symptoms in the past, but that he does not know anyone who is currently experiencing them. What is the most likely etiologic agent of this patient's disease?
- A. A gram-positive, spore-forming rod
- B. ssDNA virus of the Parvoviridae family
- C. A gram-positive cocci in chains
- D. A spirochete (Correct Answer)
- E. A gram-negative diplococci
Borrelia species Explanation: ***A spirochete***
- The migrating joint pain (**migratory polyarthritis**), fatigue, and subjective fevers in a patient who works outdoors (logger) are highly suggestive of **Lyme disease**.
- Lyme disease is caused by **_Borrelia burgdorferi_**, which is a **spirochete** transmitted by ticks.
*A gram-positive, spore-forming rod*
- This description typically refers to bacteria like **_Clostridium_** or **_Bacillus_** species.
- These organisms are generally associated with conditions like **tetanus**, **botulism**, or **anthrax**, which do not match the migratory joint pain and fatigue described.
*ssDNA virus of the Parvoviridae family*
- The most common human pathogen in this family is **Parvovirus B19**, which causes **fifth disease** (erythema infectiosum).
- While Parvovirus B19 can cause **arthralgia** and **arthritis**, especially in adults, it typically presents with a characteristic **slapped-cheek rash** and is less commonly associated with a prolonged, migratory joint pain pattern in this context.
*A gram-positive cocci in chains*
- This describes organisms like **_Streptococcus pyogenes_**, which can cause **rheumatic fever** leading to migratory polyarthritis.
- However, rheumatic fever typically follows a **streptococcal pharyngitis** and has other characteristic features like carditis or chorea not mentioned here.
*A gram-negative diplococci*
- This describes organisms like **_Neisseria gonorrhoeae_** or **_Neisseria meningitidis_**.
- **Disseminated gonococcal infection** can cause migratory polyarthralgia, but it is typically associated with a history of sexually transmitted infection and often presents with tenosynovitis or skin lesions, which are not mentioned.
Borrelia species US Medical PG Question 7: A 29-year-old woman presents with a skin rash that has spread on her arm over the last few days. She also complains of fever, headache, joint pain, and stiffness of the neck associated with the onset of the rash. On physical examination, there is an annular, red rash with a clear area in the center similar to a bull’s-eye (see image). The patient says she went on a camping trip to Connecticut last month but does not remember being bitten by an insect. Which of the following could result if this condition remains untreated in this patient?
- A. Necrotizing fasciitis
- B. Third-degree heart block
- C. Pseudomembranous colitis
- D. Subacute sclerosing panencephalitis
- E. Bell’s palsy (Correct Answer)
Borrelia species Explanation: ***Bell's palsy***
- The patient presents with classic symptoms of **Lyme disease**, including a **bull's-eye rash (erythema migrans)**, fever, headache, joint pain, and a history of exposure in an endemic area (Connecticut).
- If untreated, Lyme disease can progress to involve the nervous system (stage 2), leading to complications like **facial nerve palsy (Bell's palsy)**, other cranial neuropathies, meningitis, and radiculoneuropathy.
*Necrotizing fasciitis*
- This is a severe, rapidly spreading bacterial infection of the **fascia** and subcutaneous tissues, characterized by intense pain, swelling, erythema, and systemic toxicity.
- It does not present with an erythema migrans rash or the constellation of symptoms seen in this patient, and is typically caused by Group A Streptococcus or polymicrobial infections following skin trauma.
*Third-degree heart block*
- While **Lyme carditis** is a recognized complication of untreated Lyme disease and can cause **AV heart block** (including third-degree block), it is less common than the neurological manifestations.
- Lyme carditis typically occurs in stage 2 (early disseminated disease) and presents with palpitations, dyspnea, chest pain, or syncope.
- However, **neurological complications** like Bell's palsy are more frequent and characteristic of untreated Lyme disease.
*Pseudomembranous colitis*
- This condition is an inflammation of the colon caused by toxins produced by **Clostridioides difficile**, typically following antibiotic use.
- Its symptoms include severe watery diarrhea, abdominal pain, and fever, none of which are present in this case and are unrelated to Lyme disease.
*Subacute sclerosing panencephalitis*
- This is a rare, fatal, progressive neurodegenerative disease of the central nervous system caused by a persistent infection with the **measles virus**.
- It would not be a complication of untreated Lyme disease, which is caused by **Borrelia burgdorferi** (a spirochete bacteria) and presents with distinct neurological sequelae such as cranial neuropathies and lymphocytic meningitis.
Borrelia species US Medical PG Question 8: A 29-year-old man comes to the physician because of a 3-day history of a swollen right knee. Over the past several weeks, he has had similar episodes affecting the right knee and sometimes also the left elbow, in which the swelling lasted an average of 5 days. He has a history of a rash that subsided 2 months ago. He lives in Connecticut with his wife and works as a landscaper. His temperature is 37.8°C (100°F), pulse is 90/min, respirations are 12/min, and blood pressure is 110/75 mm Hg. Physical examination shows a tender and warm right knee; range of motion is limited by pain. The remainder of the examination shows no abnormalities. His hematocrit is 44%, leukocyte count is 10,300/mm3, and platelet count is 145,000/mm3. Serum electrolyte concentrations are within normal limits. Arthrocentesis is performed and the synovial fluid is cloudy. Gram stain is negative. Analysis of the synovial fluid shows a leukocyte count of 70,000/mm3 and 80% neutrophils. Serologic testing confirms the diagnosis. Which of the following is the most likely cause?
- A. Rheumatoid arthritis
- B. Neisseria gonorrhoeae
- C. Borrelia burgdorferi (Correct Answer)
- D. Campylobacter jejuni
- E. Osteoarthritis
Borrelia species Explanation: ***Borrelia burgdorferi***
- The patient's **migratory polyarthritis** (affecting knee and elbow intermittently), history of a **rash** (consistent with erythema migrans), and residence in an **endemic area** (Connecticut) strongly suggest **Lyme disease**.
- **Synovial fluid analysis** showing high leukocyte count with neutrophilic predominance is typical of inflammatory arthritis, including Lyme arthritis, and **serologic testing** will confirm the presence of *Borrelia burgdorferi* antibodies.
*Rheumatoid arthritis*
- While rheumatoid arthritis causes inflammatory polyarthritis, it typically presents with **symmetrical joint involvement**, morning stiffness, and often involves smaller joints first, which is not described.
- The presence of a preceding **rash** and resolution within weeks is not characteristic of rheumatoid arthritis.
*Neisseria gonorrhoeae*
- **Disseminated gonococcal infection** can cause migratory polyarthralgia or septic arthritis, but it is typically associated with a history of recent unprotected sexual activity and often with tenosynovitis or dermatitis (pustular or vesicular lesions).
- While gram stain is negative in this case, gonococcal arthritis usually has a more rapid onset and systemic symptoms.
*Campylobacter jejuni*
- *Campylobacter jejuni* is a common cause of **reactive arthritis**, which can cause inflammatory joint pain after a gastrointestinal infection.
- However, reactive arthritis typically involves the **lower extremities** and has a specific pattern of oligoarthritis, often with enthesitis or dactylitis, and the preceding rash and geographical factors do not fit.
*Osteoarthritis*
- Osteoarthritis is a **degenerative joint disease** characterized by pain that worsens with activity and improves with rest, and typically affects older individuals.
- It does not present with a preceding **rash**, migratory inflammatory episodes, or a highly inflammatory synovial fluid (high leukocyte count with neutrophilic predominance).
Borrelia species US Medical PG Question 9: A 24-year-old female comes to the physician because of flu-like symptoms and a new rash for 2 days. She denies contacts with sick individuals or recent travel abroad, but recently went camping in Vermont. Vital signs are within normal limits. Examination of the lateral right thigh shows a circular red ring with central clearing. Which of the following is the natural reservoir of the pathogen responsible for this patient's symptoms?
- A. Rat
- B. Rabbit
- C. Tick
- D. Mouse (Correct Answer)
- E. Flea
Borrelia species Explanation: ***Mouse***
- The patient's symptoms, including **flu-like illness** and a **circular red rash with central clearing** (erythema migrans) after camping in Vermont, are classic for **Lyme disease**.
- The causative agent, *Borrelia burgdorferi*, is primarily maintained in **white-footed mice** (genus *Peromyscus*) in its natural reservoir during its larval and nymphal stages.
*Rat*
- While **rats** can carry and transmit various diseases, they are not the primary natural reservoir for *Borrelia burgdorferi*, the pathogen responsible for Lyme disease.
- Diseases associated with rats often include **leptospirosis** and **plague**, which present with different clinical pictures.
*Rabbit*
- **Rabbits** are known reservoirs for diseases like **tularemia** (*Francisella tularensis*), which can cause fever, skin lesions, and lymphadenopathy, but typically not the characteristic **erythema migrans** rash.
- They are not a significant natural reservoir for *Borrelia burgdorferi*.
*Tick*
- The **tick** (specifically *Ixodes scapularis* or **deer tick**) is the **vector** that transmits *Borrelia burgdorferi* to humans, not the natural reservoir.
- The tick acquires the bacteria from infected animal hosts such as mice and deer.
*Flea*
- **Fleas** are vectors for diseases such as **bubonic plague** (*Yersinia pestis*) and **endemic typhus** (*Rickettsia typhi*), which do not manifest with erythema migrans.
- They are not involved in the transmission or natural history of **Lyme disease**.
Borrelia species US Medical PG Question 10: Blood cultures are sent to the laboratory and empiric treatment with intravenous vancomycin is started. Blood cultures grow gram-negative bacilli identified as Cardiobacterium hominis. Which of the following is the most appropriate next step in management?
- A. Switch to intravenous gentamicin
- B. Switch to intravenous ampicillin
- C. Switch to intravenous ceftriaxone (Correct Answer)
- D. Switch to intravenous cefazolin
- E. Add intravenous rifampin
Borrelia species Explanation: ***Switch to intravenous ceftriaxone***
- **Cardiobacterium hominis** is part of the **HACEK group** of bacteria, which are known for causing **endocarditis**.
- These organisms are typically susceptible to **beta-lactam antibiotics**, with **third-generation cephalosporins** like ceftriaxone being the drug of choice due to their excellent activity and good penetration.
*Switch to intravenous gentamicin*
- While **aminoglycosides** like gentamicin can be used in combination regimens for serious infections, they are generally **not monotherapy** for HACEK endocarditis and are associated with **nephrotoxicity** and **ototoxicity**.
- The primary treatment for HACEK endocarditis is a **beta-lactam antibiotic**, not an aminoglycoside alone.
*Switch to intravenous ampicillin*
- **Ampicillin** is a beta-lactam, but it may not consistently provide optimal coverage for all HACEK organisms, and some strains may have reduced susceptibility.
- **Third-generation cephalosporins** are preferred due to their broader and more consistent activity against this group.
*Switch to intravenous cefazolin*
- **Cefazolin** is a first-generation cephalosporin and typically has **limited activity** against gram-negative bacilli, especially those like Cardiobacterium hominis which require broader-spectrum beta-lactams.
- Its spectrum of activity is primarily against **gram-positive bacteria** and some **gram-negative cocci**.
*Add intravenous rifampin*
- **Rifampin** is primarily used for **mycobacterial infections** and in combination regimens for specific bacterial infections (e.g., bone and joint infections, prosthetic device infections) often due to resistant staphylococci.
- It is **not a first-line agent** for Cardiobacterium hominis infections and there's no indication for its use here with an organism susceptible to ceftriaxone.
More Borrelia species US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.