Thrombolysis inclusion/exclusion criteria US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thrombolysis inclusion/exclusion criteria. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 1: A 74-year-old man is rushed to the emergency department with left-sided weakness, facial deviation, and slurred speech. His wife first noticed these changes about an hour ago. The patient is having difficulty communicating. He can answer questions by nodding his head, and his wife is providing detailed information. He denies fever, loss of consciousness, head injury, bleeding, or seizures. Past medical history is significant for diabetes mellitus, hypertension, hyperlipidemia, ischemic heart disease, chronic kidney disease, and osteoarthritis. He had a heart attack 6 weeks ago. Baseline creatinine is 2.5 mg/dL, and he is not on hemodialysis. Medications include aspirin, clopidogrel, metoprolol, ramipril, rosuvastatin, and insulin detemir. Blood pressure is 175/95 mm Hg and the heart rate is 121/min. Muscle strength is decreased in both the upper and lower extremities on the left-side. A forehead sparing left sided facial weakness is also appreciated. An ECG reveals atrial fibrillation. An urgent head CT shows a hypodense area in the right parietal cortex with no indication of hemorrhage. Treatment with tissue plasminogen activator (tPA) is deferred due to which condition?
- A. History of myocardial infarction 6 weeks ago (Correct Answer)
- B. Chronic kidney disease
- C. Atrial fibrillation on electrocardiogram
- D. Raised blood pressures
- E. Aspirin and clopidogrel use
Thrombolysis inclusion/exclusion criteria Explanation: ***History of myocardial infarction 6 weeks ago***
- Recent **myocardial infarction (MI)**, especially within the last 3 months, is a relative contraindication for tPA due to the increased risk of hemorrhage. The patient's MI 6 weeks ago falls within this critical window.
- While not an absolute contraindication, the increased risk of hemorrhagic complications from tPA outweighs potential benefits in this specific scenario.
*Chronic kidney disease*
- **Chronic kidney disease (CKD)** itself is not a contraindication to tPA administration.
- The elevated creatinine and CKD stage do not directly increase the risk of hemorrhage from tPA in the absence of other bleeding diatheses.
*Atrial fibrillation on electrocardiogram*
- **Atrial fibrillation (AFib)** is a common cause of embolic stroke and does not contraindicate tPA.
- In fact, identifying AFib helps confirm the likely cardioembolic etiology of the stroke, making tPA a potentially beneficial treatment if other contraindications are absent.
*Raised blood pressures*
- While BP above 185/110 mm Hg is an absolute contraindication for tPA, the patient's current BP of **175/95 mm Hg** can typically be managed pharmacologically to below the threshold before tPA administration.
- **Hypertension** itself can be treated to enable tPA, it is not an intrinsic contraindication provided it can be lowered.
*Aspirin and clopidogrel use*
- Concurrent use of **antiplatelet agents** like aspirin and clopidogrel is not an absolute or relative contraindication for tPA.
- The combination of antiplatelets does not significantly increase the risk of hemorrhage with tPA to the extent that it would prompt deferral.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 2: A researcher is investigating the risk of symptomatic intracerebral hemorrhage associated with tissue plasminogen activator (tPA) treatment in severe ischemic stroke. The outcomes of a large randomized controlled trial of ischemic stroke patients, some of whom were randomized to tPA, is shown:
Symptomatic intracerebral hemorrhage No symptomatic intracerebral hemorrhage
Received tPA 12 188
Did not receive tPA 25 475
Based on this data, how many patients with severe ischemic stroke would need to be treated with tPA, on average, to contribute to one case of symptomatic intracerebral hemorrhage?
- A. 13
- B. 6
- C. 0.01
- D. 1.2
- E. 100 (Correct Answer)
Thrombolysis inclusion/exclusion criteria Explanation: ***100***
- To calculate the number needed to harm (NNH), first determine the **absolute risk reduction/increase (ARR/ARI)** for symptomatic intracerebral hemorrhage.
- The **risk in the tPA group** is 12 (hemorrhages) / (12 + 188) (total tPA patients) = 12/200 = 0.06. The **risk in the control group** is 25 (hemorrhages) / (25 + 475) (total control patients) = 25/500 = 0.05.
- The **ARI = Risk in tPA group - Risk in control group = 0.06 - 0.05 = 0.01**.
- The NNH is the reciprocal of the ARI: **NNH = 1 / ARI = 1 / 0.01 = 100**. This means 100 patients need to be treated for one additional case of symptomatic intracerebral hemorrhage due to tPA.
*13*
- This value does not represent the correct calculation for the **Number Needed to Harm (NNH)**.
- It likely results from an incorrect application of the data or a misinterpretation of the NNH formula.
*6*
- This number is incorrect and does not reflect the **NNH** based on the provided data.
- It might represent a calculation based on a different metric or a miscalculation of the **absolute risk increase**.
*0.01*
- This value represents the **absolute risk increase (ARI)** (0.06 - 0.05 = 0.01) of symptomatic intracerebral hemorrhage with tPA, not the **Number Needed to Harm (NNH)**.
- The NNH is the reciprocal of the ARI, which would be 1/0.01 = 100.
*1.2*
- This value is not derived from the standard calculation of **Number Needed to Harm (NNH)**.
- It may be the result of a miscalculation or an attempt to compare the relative risks, rather than addressing the question of treatment impact per case.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 3: A 77-year-old woman is brought by ambulance to the emergency department after she developed weakness of her right arm along with a right-sided facial droop. By the time the ambulance arrived, she was having difficulty speaking. Past medical history is significant for hypertension, diabetes mellitus type II, and hyperlipidemia. She takes lisinopril, hydrochlorothiazide, metformin, and atorvastatin. On arrival to the emergency department, her vital signs are within normal limits. On physical examination, she is awake and alert but the right side of her mouth is dropping, making it difficult for her to speak clearly. Her heart has a regular rate and rhythm and her lungs are clear to auscultation bilaterally. Fingerstick glucose is 85 mg/dL. Her right upper extremity strength is 2/5 and her left upper extremity strength is 5/5. Which of the following is the best next step in management?
- A. Obtain transcranial doppler
- B. Start tissue plasminogen activator (tPA)
- C. Consult cardiology
- D. Intubate the patient
- E. Obtain noncontrast CT of the brain (Correct Answer)
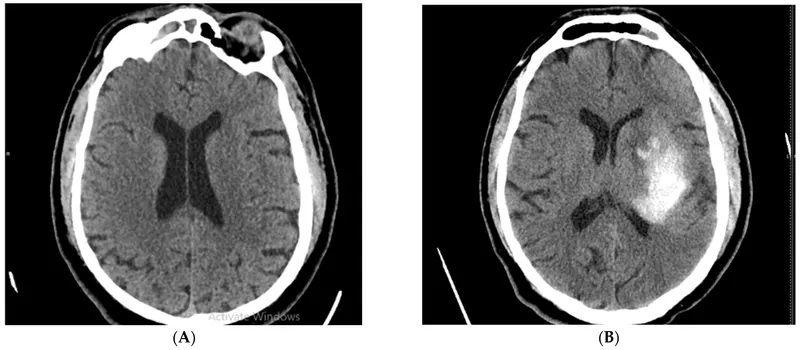
Thrombolysis inclusion/exclusion criteria Explanation: ***Obtain noncontrast CT of the brain***
- An **urgent noncontrast CT of the brain** is the **most crucial initial step** in managing acute neurological deficits suggestive of stroke.
- This imaging is essential to **rule out hemorrhagic stroke** before considering thrombolytic therapy like tPA.
*Obtain transcranial doppler*
- **Transcranial Doppler (TCD)** can be used to assess cerebral blood flow and identify vascular stenosis but is not the immediate first-line diagnostic imaging for an acute stroke presentation.
- TCD is typically performed **after initial imaging** to determine the presence of large vessel occlusion or monitor for vasospasm, not to differentiate between ischemic and hemorrhagic stroke.
*Start tissue plasminogen activator (tPA)*
- While **tPA** is a treatment for acute ischemic stroke, it is **contraindicated in hemorrhagic stroke**.
- Without a **noncontrast CT scan to rule out hemorrhage**, administering tPA can be life-threatening.
*Consult cardiology*
- Consulting cardiology is important for evaluating potential cardiac sources of emboli (e.g., atrial fibrillation) as a cause of stroke but it is **not the immediate next step** in managing acute stroke symptoms.
- The **immediate priority is diagnosing the type of stroke** and determining eligibility for acute interventions.
*Intubate the patient*
- **Intubation** is reserved for patients with compromise of their **airway, breathing, or circulation (ABCs)**, or a significantly decreased level of consciousness (e.g., GCS < 8).
- This patient is described as **awake and alert**, making intubation unnecessary at this stage.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 4: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
Thrombolysis inclusion/exclusion criteria Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 5: A 48-year-old woman presents with acute stroke symptoms 18 hours ago. MRI shows a right MCA M1 occlusion with large penumbra on perfusion imaging (mismatch ratio >1.8) and small infarct core (25 mL). Her NIHSS is 16. She has no significant comorbidities. Her family is concerned about disability but wants to pursue treatment if reasonable chance of benefit exists. Synthesize the evidence and evaluate the treatment approach.
- A. Intravenous alteplase as salvageable tissue is present
- B. Intra-arterial thrombolysis combined with mechanical device
- C. No intervention as she is outside the standard treatment window
- D. Mechanical thrombectomy based on perfusion imaging criteria (Correct Answer)
- E. Medical management with antiplatelet and early rehabilitation
Thrombolysis inclusion/exclusion criteria Explanation: ***Mechanical thrombectomy based on perfusion imaging criteria***
- For patients with large vessel occlusion (LVO) in the extended 6–24 hour window, **DAWN** and **DEFUSE-3** trials demonstrated significant functional benefit when clinical-core mismatch is present.
- This patient satisfies criteria with an **M1 occlusion**, a **small infarct core (<70 mL)**, and a **large mismatch ratio (>1.8)**, indicating substantial salvageable penumbra.
*Intravenous alteplase as salvageable tissue is present*
- The therapeutic window for **IV alteplase** is strictly limited to within **4.5 hours** of symptom onset; it is not recommended at 18 hours due to high hemorrhage risk.
- While salvageable tissue exists, chemical thrombolysis is less effective than mechanical intervention for **proximal M1 occlusions** and is unsafe in this late window.
*Intra-arterial thrombolysis combined with mechanical device*
- **Intra-arterial thrombolysis** is generally superseded by modern **stent retrievers** and aspiration catheters which provide faster and more complete recanalization.
- Current guidelines prioritize standalone **mechanical thrombectomy** in the late window to minimize procedural risks and intracranial hemorrhage.
*No intervention as she is outside the standard treatment window*
- The "Time is Brain" concept has evolved into "Tissue is Brain," where **perfusion imaging** identifies candidates who benefit regardless of the traditional 6-hour clock.
- Denying treatment based solely on the 18-hour timeframe ignores high-level evidence from the **DAWN** trial showing benefit up to 24 hours.
*Medical management with antiplatelet and early rehabilitation*
- Standard **medical management** (aspirin/heparin) for an M1 occlusion with a high **NIHSS score (16)** usually results in poor functional outcomes and severe disability.
- While rehabilitation is essential, it does not address the underlying **large vessel occlusion** which can be reversed with mechanical intervention to prevent infarct expansion.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 6: A 55-year-old man undergoes successful thrombectomy for left MCA occlusion. Post-procedure, he develops progressive lethargy and his blood pressure increases to 180/100 mmHg. CT shows hyperdensity in the treated territory without hemorrhage, and his symptoms worsen over 4 hours despite blood pressure control. Evaluate the most likely diagnosis and management priority.
- A. Hemorrhagic transformation; reverse anticoagulation immediately
- B. Cerebral edema from large infarction; emergent decompressive hemicraniectomy
- C. Reperfusion injury; start high-dose corticosteroids and osmotic therapy
- D. Contrast extravasation from blood-brain barrier disruption; supportive care and avoid aggressive BP lowering (Correct Answer)
- E. Recurrent arterial occlusion; emergent repeat angiography and thrombectomy
Thrombolysis inclusion/exclusion criteria Explanation: ***Contrast extravasation from blood-brain barrier disruption; supportive care and avoid aggressive BP lowering***
- Post-thrombectomy **hyperdensity** on CT often represents contrast that leaked through an ischemic **blood-brain barrier**, which can mimic hemorrhage but lacks significant **mass effect**.
- Management is **supportive care** because the contrast is typically reabsorbed within 24–48 hours; avoiding aggressive **blood pressure lowering** prevents secondary ischemia in the penumbra.
*Hemorrhagic transformation; reverse anticoagulation immediately*
- While **hemorrhagic transformation** is a risk, true blood usually demonstrates higher density earlier and is associated with rapid clinical decline and **midline shift**.
- Reversing anticoagulation without confirming blood on a follow-up **dual-energy CT** or MRI may lead to **stent thrombosis** or re-occlusion.
*Cerebral edema from large infarction; emergent decompressive hemicraniectomy*
- **Cerebral edema** typically peaks between 72–96 hours post-stroke; a presentation within 4 hours is too acute for **malignant MCA syndrome**.
- While edema causes lethargy, the hyperdensity on CT more specifically points toward **contrast staining** or blood rather than simple cytotoxic edema.
*Reperfusion injury; start high-dose corticosteroids and osmotic therapy*
- **Corticosteroids** are not indicated for stroke-related edema or reperfusion injury as they do not improve outcomes and may increase **infection risk**.
- **Osmotic therapy** is reserved for patients with clear clinical or radiologic signs of **elevated intracranial pressure**, not isolated hyperdensity on CT.
*Recurrent arterial occlusion; emergent repeat angiography and thrombectomy*
- **Recurrent occlusion** usually presents with a sudden recurrence of the original **focal neurological deficits** (e.g., hemiplegia, aphasia) rather than progressive lethargy.
- The presence of **hyperdensity** in the stroke territory on CT is specifically indicative of material (contrast or blood) being present, which is not a feature of a simple **re-occlusion**.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 7: An 80-year-old woman with atrial fibrillation presents 2 hours after acute ischemic stroke. NIHSS is 22. Imaging shows large left MCA territory infarction involving >1/3 of MCA territory with basilar artery occlusion. She lives alone but was independent before this event. Her family requests all possible interventions. Evaluate the management approach considering benefits versus risks.
- A. Comfort measures only given poor prognosis and age
- B. Thrombolysis alone as thrombectomy unlikely to benefit with established large infarction
- C. Proceed with thrombolysis and thrombectomy given the therapeutic window
- D. Thrombectomy only for basilar occlusion, avoid thrombolysis due to large infarction (Correct Answer)
- E. Delay intervention and repeat imaging in 6 hours to assess progression
Thrombolysis inclusion/exclusion criteria Explanation: ***Thrombectomy only for basilar occlusion, avoid thrombolysis due to large infarction***
- Intravenous **thrombolysis (IV alteplase)** is generally contraindicated or highly risky when imaging shows an established infarction involving **>1/3 of the MCA territory** due to the high risk of **hemorrhagic transformation**.
- **Basilar artery occlusion** is a life-threatening emergency with a broader treatment window; mechanical **thrombectomy** can be lifesaving and is indicated even if thrombolysis is withheld.
*Comfort measures only given poor prognosis and age*
- Age is not a primary contraindication for intervention, especially since the patient was **independent** prior to the event (low **pre-stroke mRS**).
- Family requests all possible interventions, and **basilar occlusion** has a catastrophic natural history that may be mitigated by mechanical intervention.
*Thrombolysis alone as thrombectomy unlikely to benefit with established large infarction*
- Thrombolysis is dangerous in this context due to the **large infarct volume** seen on imaging, which increases the likelihood of fatal **intracerebral hemorrhage**.
- Thrombolysis is notably less effective for large vessel occlusions compared to **mechanical thrombectomy**, which is the gold standard for **basilar artery** recanalization.
*Proceed with thrombolysis and thrombectomy given the therapeutic window*
- While the patient is within the 4.5-hour window for thrombolysis, the presence of **established early ischemic changes** (>1/3 MCA territory) is a relative contraindication.
- Attempting both increases the risk of **secondary hemorrhage** in the damaged MCA territory without providing significant additional benefit over thrombectomy alone for the **basilar occlusion**.
*Delay intervention and repeat imaging in 6 hours to assess progression*
- Delaying treatment in the setting of **basilar artery occlusion** is inappropriate, as "time is brain" and outcomes worsen significantly with every minute of **brainstem ischemia**.
- Immediate decision-making is required based on the initial imaging, which already confirmed the **large-vessel occlusion** needing intervention.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 8: A 58-year-old woman with history of TIA 3 weeks ago presents with acute ischemic stroke. Imaging reveals new right MCA infarction and severe (70-99%) symptomatic right carotid stenosis. She received alteplase 6 hours ago with partial improvement. Her NIHSS improved from 14 to 8. Analyze the optimal timing for carotid revascularization.
- A. Wait 4-6 weeks to reduce hemorrhagic transformation risk
- B. Carotid stenting immediately after thrombolysis
- C. Emergent carotid endarterectomy within 24 hours
- D. Carotid endarterectomy within 2 weeks of symptom onset (Correct Answer)
- E. Medical management only due to recent thrombolysis
Thrombolysis inclusion/exclusion criteria Explanation: ***Carotid endarterectomy within 2 weeks of symptom onset***
- For patients with **symptomatic carotid stenosis** (70-99%), early revascularization within **2 weeks** (ideally within 48 hours to 7 days) provides the maximum benefit in preventing recurrent stroke.
- Current guidelines suggest that once the patient is **neurologically stable** and the infarct size is not massive, the risk of recurrence outweighs the risk of **hemorrhagic transformation**.
*Wait 4-6 weeks to reduce hemorrhagic transformation risk*
- This represents older clinical practice; modern evidence shows the risk of **recurrent stroke** is highest in the first 2 weeks, making this delay dangerous.
- Waiting this long is only typically reserved for patients with a **large territory infarct** (high NIHSS) or those at very high risk for bleeding complications.
*Carotid stenting immediately after thrombolysis*
- Immediate stenting right after **alteplase** administration increases the risk of **intracranial hemorrhage** and local bleeding at the access site due to systemic fibrinolysis.
- While **Carotid Artery Stenting (CAS)** is an alternative, it is generally not preferred over **Carotid Endarterectomy (CEA)** in older patients unless specific surgical contraindications exist.
*Emergent carotid endarterectomy within 24 hours*
- Performing surgery within the first 24 hours after **thrombolytic therapy** carries a significant risk of **hemorrhagic transformation** of the fresh infarct.
- Most surgeons prefer to wait at least **24-48 hours** post-alteplase to ensure the fibrinolytic effects have resolved and the patient's neurological status is stable.
*Medical management only due to recent thrombolysis*
- Medical management alone is insufficient for **symptomatic stenosis >70%**, as the risk of a disabling stroke remains high without mechanical intervention.
- **Dual antiplatelet therapy** and statins are vital, but they serve as an adjunct to, rather than a replacement for, **surgical revascularization** in fit patients.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 9: A 62-year-old man received IV alteplase 45 minutes ago for acute ischemic stroke. He now develops sudden severe headache, vomiting, and decreased level of consciousness. His blood pressure is 190/110 mmHg. Analyze the most critical immediate steps in management.
- A. Stop alteplase, observe, and repeat CT in 24 hours
- B. Administer labetalol for blood pressure and continue monitoring
- C. Obtain emergent CT head, stop alteplase, give cryoprecipitate and tranexamic acid (Correct Answer)
- D. Continue alteplase and give mannitol for cerebral edema
- E. Give protamine sulfate and arrange for neurosurgical consultation
Thrombolysis inclusion/exclusion criteria Explanation: ***Obtain emergent CT head, stop alteplase, give cryoprecipitate and tranexamic acid***
- Sudden headache and neurologic decline during **alteplase** infusion are hallmarks of **symptomatic intracranial hemorrhage (sICH)**, necessitating immediate cessation of the drug and diagnostic imaging.
- Reversal of fibrinolysis is critical; **cryoprecipitate** provides **fibrinogen** and Factor VIII, while **tranexamic acid** or aminocaproic acid inhibits further fibrinolysis.
*Stop alteplase, observe, and repeat CT in 24 hours*
- Delaying a CT scan for 24 hours is inappropriate for an acute neurological change, as active bleeding requires **emergent intervention**.
- Observation alone is insufficient; **active reversal** of coagulopathy is needed to prevent hematoma expansion and brain herniation.
*Administer labetalol for blood pressure and continue monitoring*
- While **blood pressure management** is important (targeting <180/105 mmHg), it is secondary to stopping the thrombolytic and confirming hemorrhage.
- Monitoring without stopping the infusion would allow the **thrombolytic agent** to continue exacerbating the intracranial bleed.
*Continue alteplase and give mannitol for cerebral edema*
- Continuing **alteplase** in the setting of suspected hemorrhage is contraindicated and life-threatening.
- **Mannitol** addresses intracranial pressure but does not treat the underlying **coagulopathy** causing the hemorrhage.
*Give protamine sulfate and arrange for neurosurgical consultation*
- **Protamine sulfate** is the reversal agent for **heparin**, not alteplase, and has no effect on fibrinolysis.
- While neurosurgical consultation is necessary, the medical reversal of the **thrombolytic effect** with blood products is the most immediate priority.
Thrombolysis inclusion/exclusion criteria US Medical PG Question 10: A 70-year-old diabetic man presents 5 hours after waking with right arm weakness. He was last seen normal 9 hours ago before sleep. MRI shows acute left MCA territory infarction with DWI-FLAIR mismatch and perfusion imaging showing salvageable tissue. CTA shows M1 segment occlusion. His NIHSS is 12. Analyze the appropriate intervention.
- A. Intravenous alteplase based on wake-up stroke protocol
- B. Dual antiplatelet therapy and observation
- C. No reperfusion therapy due to unknown time of onset
- D. Mechanical thrombectomy based on imaging criteria (Correct Answer)
- E. Intra-arterial thrombolysis within 6 hours
Thrombolysis inclusion/exclusion criteria Explanation: ***Mechanical thrombectomy based on imaging criteria***
- Guidelines from the **DAWN** and **DEFUSE-3** trials support **mechanical thrombectomy** for large vessel occlusions (M1 segment) up to 24 hours if there is evidence of **salvageable tissue** on perfusion imaging.
- This patient satisfies criteria due to a significant **NIHSS score (12)**, a demonstrated **DWI-FLAIR mismatch**, and a visible **large vessel occlusion (LVO)** on CTA.
*Intravenous alteplase based on wake-up stroke protocol*
- While **IV alteplase** can be considered for wake-up strokes with **DWI-FLAIR mismatch**, the "last seen normal" time of 9 hours exceeds the standard **4.5-hour** window for chemical thrombolysis.
- Even if administered, it is often ineffective for **large vessel occlusions** like an M1 segment block, which requires mechanical intervention.
*Dual antiplatelet therapy and observation*
- **Dual antiplatelet therapy (DAPT)** is indicated for minor stroke or high-risk TIA, but is insufficient for a patient with an **NIHSS of 12** and a major arterial occlusion.
- Observation alone ignores the opportunity for **reperfusion**, leading to poor outcomes and permanent disability in the setting of **salvageable penumbra**.
*No reperfusion therapy due to unknown time of onset*
- The concept of "time is brain" has evolved to "tissue is brain," meaning **reperfusion** depends on physiological imaging rather than just the clock.
- Modern protocols allow for intervention in **unknown onset** strokes if specialized imaging like **MRI or perfusion studies** show viable tissue.
*Intra-arterial thrombolysis within 6 hours*
- **Intra-arterial thrombolysis** has largely been superseded by **mechanical thrombectomy**, which shows superior efficacy for proximal **large vessel occlusions**.
- The treatment window for this specific intervention would also be less favorable compared to the 24-hour window established for **thrombectomy**.
More Thrombolysis inclusion/exclusion criteria US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.