Secondary stroke prevention US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Secondary stroke prevention. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Secondary stroke prevention US Medical PG Question 1: A 71-year-old man comes to the physician for a routine health maintenance examination. He feels well. He goes for a 30-minute walk three times a week and does not experience any shortness of breath or chest or leg pain on exertion. He has not had any weakness, numbness, or vision disturbance. He has diabetes that is well controlled with insulin injections. He had smoked one pack of cigarettes every day for 40 years but quit 5 years ago. He appears healthy and well nourished. His temperature is 36.3°C (97.3°F), pulse is 75/min, and blood pressure is 136/78 mm Hg. Physical examination shows normal heart sounds. There are systolic bruits over the neck bilaterally. Physical and neurologic examinations show no other abnormalities. Fasting serum studies show:
Total cholesterol 210 mg/dL
HDL cholesterol 28 mg/dL
LDL cholesterol 154 mg/dL
Triglycerides 140 mg/dL
Glucose 102 mg/dL
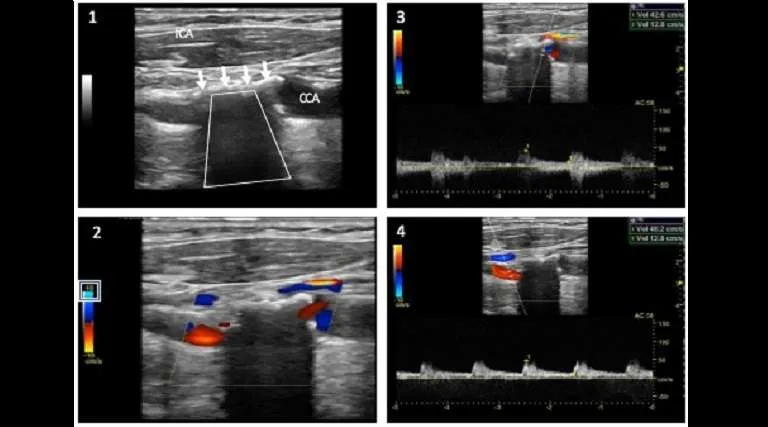
Duplex ultrasonography of the carotid arteries shows a 85% stenosis on the left and a 55% stenosis on the right side. Which of the following is the most appropriate next step in management?
- A. Carotid artery stenting
- B. Aspirin therapy only
- C. Bilateral carotid endarterectomy
- D. Left carotid endarterectomy (Correct Answer)
Secondary stroke prevention Explanation: ***Left carotid endarterectomy***
- The patient has **asymptomatic carotid artery stenosis** with a **left-sided stenosis of 85%**. For asymptomatic patients, carotid endarterectomy is indicated for stenosis between 70% and 99% if the patient has a life expectancy of at least 5 years and the periprocedural stroke and death rate is low (<3%).
- This patient, despite his age, is **active and healthy**, has no neurological deficits, and his comorbidities (well-controlled diabetes, history of smoking but quit 5 years ago) are unlikely to significantly increase surgical risk beyond the benefit of stroke prevention for severe stenosis.
*Carotid artery stenting*
- While carotid artery stenting (CAS) is an alternative to endarterectomy, it is generally preferred in patients who are **high-risk for endarterectomy** due to specific anatomical or medical comorbidities, or in cases of **restenosis after endarterectomy**.
- In asymptomatic patients, **endarterectomy** is generally favored over stenting, especially for stroke prevention, as large trials have shown a slightly higher periprocedural stroke risk with stenting.
*Aspirin therapy only*
- While **aspirin and statin therapy** are crucial for patients with carotid artery disease to reduce cardiovascular events, they are **insufficient as sole treatment** for severe asymptomatic carotid stenosis (85%).
- Medical therapy alone does not provide the same level of stroke risk reduction as interventional approaches for high-grade stenosis.
*Bilateral carotid endarterectomy*
- A **bilateral procedure** is not indicated at this time. The right carotid stenosis is 55%, which in an asymptomatic patient, is typically managed with **medical therapy** rather than surgical intervention.
- Performing endarterectomy on the right side at this time would expose the patient to unnecessary surgical risk without clear benefit for immediate stroke prevention.
Secondary stroke prevention US Medical PG Question 2: An obese 37-year-old woman is brought to the emergency department 2 hours after the onset of weakness in her left arm and leg. She fell from the stairs the day prior but did not have any loss of consciousness or nausea after the fall. She travels to Asia regularly on business; her last trip was 4 days ago. She has no history of serious illness. Her only medication is an oral contraceptive. Her temperature is 37.8°C (100°F), pulse is 113/min and regular, and blood pressure is 162/90 mm Hg. Examination shows decreased muscle strength on the left side. Deep tendon reflexes are 4+ on the left. Babinski sign is present on the left. The right lower leg is swollen, erythematous, and tender to palpation. Further evaluation is most likely to show which of the following?
- A. Atrial fibrillation
- B. Patent foramen ovale (Correct Answer)
- C. Atrial myxoma
- D. Ventricular septal defect
- E. Carotid artery dissection
Secondary stroke prevention Explanation: ***Patent foramen ovale***
- This patient presents with a **cryptogenic stroke** (stroke of undetermined cause) in the context of being **obese**, taking **oral contraceptives**, recent **long-distance travel**, and symptoms of a **deep vein thrombosis (DVT)** in her right leg.
- A **paradoxical embolism** through a **patent foramen ovale (PFO)** is a strong possibility, where a clot from the DVT could bypass the pulmonary circulation and enter the systemic circulation, leading to a stroke.
*Atrial fibrillation*
- While **atrial fibrillation** is a common cause of **embolic stroke**, the patient's pulse is described as **regular**, making this diagnosis less likely.
- There are no other indications of atrial fibrillation on physical exam, such as an irregularly irregular pulse.
*Atrial myxoma*
- An **atrial myxoma** can cause **embolic stroke** due to tumor fragments breaking off, but this is a rare cause.
- There are no other signs or symptoms suggestive of a cardiac tumor, such as constitutional symptoms or cardiac murmurs.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** typically causes a left-to-right shunt and is associated with a **loud holosystolic murmur** at the lower left sternal border.
- While a **right-to-left shunt** can occur in the presence of **pulmonary hypertension (Eisenmenger syndrome)**, there is no mention of a murmur or signs of pulmonary hypertension.
*Carotid artery dissection*
- **Carotid artery dissection** can cause stroke, often preceded by **neck pain** or **headache**, which is not reported by the patient.
- The presence of a **DVT** and associated risk factors for thromboembolism makes a paradoxical embolism a more probable cause in this clinical scenario.
Secondary stroke prevention US Medical PG Question 3: A 20-year-old man presents to the doctor's office for advice on improving his health. He admits to eating mostly junk food, and he knows that he should lose some weight. His daily physical activity is limited to walking around the college campus between classes. Except for an occasional headache for which he takes acetaminophen, he has no health concerns and takes no other medications. He denies smoking and illicit drug use, but admits to occasional beer binge drinking on weekends. He is sexually active with his current girlfriend and regularly uses condoms. His mother has type 2 diabetes mellitus and obesity, while his father has hypertension and hypercholesterolemia. The pulse is 74/min, the respiratory rate is 16/min, and the blood pressure is 130/76 mm Hg. The body mass index (BMI) is 29 kg/m2. Physical examination reveals an overweight young male, and the rest is otherwise unremarkable. The routine lab test results are as follows:
Serum Glucose (fasting) 100 mg/dL
Serum Electrolytes:
Sodium 141 mEq/L
Potassium 4.0 mEq/L
Chloride 100 mEq/L
Cholesterol, total 190 mg/dL
HDL-cholesterol 42 mg/dL
LDL-cholesterol 70 mg/dL
Triglycerides 184 mg/dL
Urinalysis:
Glucose Negative
Ketones Negative
Leukocytes Negative
Nitrites Negative
RBCs Negative
Casts Negative
Which of the following lifestyle changes would most likely benefit this patient the most?
- A. A low sodium diet
- B. Starting a multivitamin
- C. Increasing daily water intake
- D. Weight reduction (Correct Answer)
- E. Increasing dietary fiber
Secondary stroke prevention Explanation: ***Weight reduction***
- The patient has a **BMI of 29 kg/m2**, which classifies him as **overweight**, and his diet consists mostly of junk food, making weight reduction a primary and impactful lifestyle change.
- Weight loss significantly improves multiple health markers, including **blood pressure**, **lipid profile**, and **insulin sensitivity**, reducing his risk for conditions like **type 2 diabetes** and **hypertension** that run in his family.
- The patient shows early signs of **metabolic syndrome** (elevated BP, low HDL 42 mg/dL, triglycerides 184 mg/dL, impaired fasting glucose 100 mg/dL), which weight reduction directly addresses.
*A low sodium diet*
- While his father has hypertension, this patient's blood pressure is **130/76 mm Hg**, which is in the **elevated range** (120-129/<80 mm Hg), not yet meeting criteria for hypertension (≥130/80 mm Hg).
- While a low sodium diet is generally healthy and can help prevent hypertension, addressing his **overweight status** and **poor dietary habits** would yield more comprehensive benefits first.
*Starting a multivitamin*
- The patient has no symptoms or signs of **nutrient deficiencies**, and his routine lab tests are normal.
- There is generally **no strong evidence** to support routine multivitamin supplementation in otherwise healthy individuals with no specific deficiencies.
*Increasing daily water intake*
- There is no indication that the patient is **dehydrated** or has any conditions that would specifically benefit from a significant increase in water intake.
- While adequate hydration is important, it is **not the most impactful intervention** for his current health profile compared to addressing his diet and weight.
*Increasing dietary fiber*
- Increasing dietary fiber is beneficial for **digestive health** and can help with **satiety** and **cholesterol management**.
- However, his primary issue is his overall "junk food" diet and overweight status; tackling these directly through **comprehensive dietary changes** (which would include more fiber) and **weight reduction** would be more beneficial than focusing solely on fiber intake initially.
Secondary stroke prevention US Medical PG Question 4: A 71-year-old woman presents with a transient episode of right arm and hand weakness that resolved in approximately one hour. Her symptoms started while she was gardening. Her past medical history is notable for hypertension, diabetes, anxiety, and dyslipidemia. Her current medications include insulin, metformin, and fluoxetine. Examination reveals a left carotid bruit. Ultrasound duplex of her carotid arteries demonstrates right and left carotid stenosis of 35% and 50%, respectively. Which of the following is the best next step in management?
- A. Bilateral carotid endarterectomy
- B. Left carotid endarterectomy only
- C. Aspirin (Correct Answer)
- D. Observation
- E. Warfarin
Secondary stroke prevention Explanation: ***Aspirin***
- This patient suffered a **transient ischemic attack (TIA)** given her transient focal neurological deficit. Given that her carotid stenosis is **moderate (35% and 50%)**, **antiplatelet therapy** with aspirin is the initial and best next step to prevent future strokes.
- Aspirin helps prevent platelet aggregation, reducing the risk of **thrombus formation** in already stenotic vessels.
*Bilateral carotid endarterectomy*
- This is not the best next step, as **carotid endarterectomy** is generally reserved for symptomatic patients with **high-grade stenosis** (e.g., typically >70%).
- Performing bilateral procedures at once carries higher risks than staged procedures or medical management for moderate stenosis.
*Left carotid endarterectomy only*
- This is not indicated. While symptoms occurred on the right side (implying a left-sided lesion), a **left carotid endarterectomy** is primarily considered for **high-grade stenosis** in symptomatic patients.
- Her left carotid stenosis is 50%, which is considered moderate and not an immediate indication for surgery.
*Observation*
- This is inappropriate as the patient has experienced a **TIA**, indicating a high risk of future stroke.
- Without intervention, including antiplatelet therapy, the risk of a debilitating stroke is significantly increased.
*Warfarin*
- **Warfarin** is an anticoagulant used for conditions like atrial fibrillation or deep vein thrombosis but is **not the primary treatment for TIA due to carotid stenosis**.
- Its use in this context may increase the risk of bleeding without providing superior benefit to aspirin in preventing arterial clots from carotid plaques.
Secondary stroke prevention US Medical PG Question 5: A 58-year-old man presents to the clinic concerned about his health after his elder brother recently became bed-bound due to a brain condition. He has also brought a head CT scan of his brother to reference, as shown in the picture. The patient has type 2 diabetes mellitus, hypertension, osteoarthritis, and hypercholesterolemia. His medication list includes aspirin, diclofenac sodium, metformin, and ramipril. He leads a sedentary lifestyle and smokes one pack of cigarettes daily. He also drinks 4–5 cups of red wine every weekend. His BMI is 33.2 kg/m2. His blood pressure is 164/96 mm Hg, the heart rate is 84/min, and the respiratory rate is 16/min. Which of the following interventions will be most beneficial for reducing the risk of developing the disease that his brother has?
- A. Statin therapy
- B. Quit smoking
- C. Stop aspirin
- D. Blood sugar control
- E. Blood pressure control (Correct Answer)
Secondary stroke prevention Explanation: ***Blood pressure control***
- The brother's CT scan shows features of **white matter hyperintensities (WMH)**, indicative of **cerebral small vessel disease**, a significant risk factor for **neurodegenerative conditions** and dementia, which can cause a patient to become bedridden.
- **Hypertension** is the most potent and modifiable risk factor for the development and progression of WMH and other forms of cerebral small vessel disease; therefore, strict **blood pressure control** is the most beneficial intervention.
*Statin therapy*
- Statins are crucial for managing **hypercholesterolemia** and reducing the risk of **atherosclerotic cardiovascular disease** and stroke.
- While beneficial for overall vascular health, **dyslipidemia** is less strongly associated with WMH and cerebral small vessel disease than hypertension.
*Quit smoking*
- **Smoking** is a significant risk factor for **stroke**, **atherosclerosis**, and several neurodegenerative disorders.
- While important for overall health, **smoking cessation** has a less direct and immediate impact on the progression of existent WMH compared to **blood pressure control**.
*Stop aspirin*
- **Aspirin** is used for **primary or secondary prevention** of cardiovascular events due to its **antiplatelet effects**.
- There is no indication that stopping aspirin would benefit in preventing further cerebral small vessel disease; rather, it could increase the risk of other vascular events in this patient with multiple risk factors.
*Blood sugar control*
- **Type 2 diabetes mellitus** is a known risk factor for **vascular dementia** and can contribute to small vessel disease.
- While important for long-term health, the impact of **blood sugar control** on WMH progression is less substantial compared to **blood pressure control**.
Secondary stroke prevention US Medical PG Question 6: A 50-year-old man comes to the physician for his annual health maintenance examination. The patient feels well. He has a history of hypertension, for which he currently takes lisinopril. He has smoked a pack of cigarettes daily for 20 years. He drinks 5–6 beers on weekends. He is 181 cm tall (5 ft 11 in), weighs 80 kg (176.4 lbs); BMI is 24.6 kg/m2. His pulse is 75/min, blood pressure is 140/85 mm Hg, and respirations are 18/min. Physical examination is unremarkable. Laboratory studies show:
Total cholesterol 263 mg/dL
High-density lipoprotein cholesterol 36 mg/dL
Triglycerides 180 mg/dL
In addition to dietary and lifestyle modification, administration of which of the following agents is the most appropriate next step in management?
- A. Peroxisome proliferator-activated receptor alpha activator
- B. Proprotein convertase subtilisin kexin 9 inhibitor
- C. Bile acid resins
- D. HMG-CoA reductase inhibitor (Correct Answer)
- E. Cholesterol absorption inhibitor
Secondary stroke prevention Explanation: ***HMG-CoA reductase inhibitor***
- This patient has multiple **cardiovascular risk factors** (hypertension, smoking, low HDL, elevated LDL-c calculated from total cholesterol and triglycerides) and elevated LDL-c. An **HMG-CoA reductase inhibitor (statin)** is the first-line pharmacotherapy in such cases to reduce the risk of atherosclerotic cardiovascular disease events.
- Statins effectively lower **LDL-c**, which is the primary target for cholesterol reduction in patients at high risk for cardiovascular disease.
*Peroxisome proliferator-activated receptor alpha activator*
- **Fibrates** (PPAR-α activators) are primarily used to lower **triglycerides** and increase HDL, and are not the first-line choice for lowering elevated LDL-c in high-risk patients.
- They are typically reserved for severe hypertriglyceridemia not controlled by statins, or in patients intolerant to statins whose primary lipid issue is hypertriglyceridemia.
*Proprotein convertase subtilisin kexin 9 inhibitor*
- **PCSK9 inhibitors** are potent LDL-c lowering agents, but they are typically used as **adjunctive therapy** in patients with high cardiovascular risk who have not achieved adequate LDL-c reduction with maximum tolerated statin therapy, or in patients with familial hypercholesterolemia.
- Given that this patient has not yet started statin therapy, a PCSK9 inhibitor is not the initial treatment strategy.
*Bile acid resins*
- **Bile acid resins** (e.g., cholestyramine) lower LDL-c by binding to bile acids in the intestine, but they are **less effective** than statins and can sometimes increase triglycerides.
- They are generally not the first-line choice for primary LDL-c reduction due to their side effect profile (e.g., GI upset) and lower efficacy compared to statins.
*Cholesterol absorption inhibitor*
- **Ezetimibe** (a cholesterol absorption inhibitor) reduces cholesterol absorption in the small intestine, leading to lower LDL-c.
- It is often used as an **add-on therapy** to statins or as monotherapy in statin-intolerant patients, but not as the initial drug of choice when a statin is indicated and tolerated.
Secondary stroke prevention US Medical PG Question 7: A 68-year-old man is brought to the emergency department because of right-sided weakness for 2 hours. He has hypertension, dyslipidemia, and type 2 diabetes. Current medications include hydrochlorothiazide, metoprolol, amlodipine, pravastatin, and metformin. His pulse is 87/min and blood pressure is 164/98 mm Hg. Neurological examination shows right-sided weakness, facial droop, and hyperreflexia. Sensation is intact. Which of the following is the most likely cause of these findings?
- A. Lipohyalinosis of penetrating vessels (Correct Answer)
- B. Dissection of the vertebral artery
- C. Stenosis of the internal carotid artery
- D. Rupture of an intracranial aneurysm
- E. Embolism from the left atrium
Secondary stroke prevention Explanation: ***Lipohyalinosis of penetrating vessels***
- This patient presents with an acute onset of **hemiparesis**, **facial droop**, and hyperreflexia, without cortical signs like cortical sensory loss or aphasia, which is characteristic of a **lacunar stroke**.
- **Lipohyalinosis** is the most common cause of lacunar infarcts, resulting from chronic hypertension and diabetes affecting small penetrating arteries in the brain.
*Dissection of the vertebral artery*
- Vertebral artery dissection typically presents with **posterior circulation symptoms** such as vertigo, ataxia, brainstem dysfunction, and often includes severe headache or neck pain.
- The presented symptoms of pure motor hemiparesis are more indicative of an anterior circulation event involving deeper structures.
*Stenosis of the internal carotid artery*
- Significant **internal carotid artery stenosis** typically causes larger territorial infarcts by reducing blood flow or via artery-to-artery embolism to the middle cerebral artery territory.
- This would result in symptoms like **aphasia**, **cortical sensory deficits**, or **homonymous hemianopia**, which are not present here.
*Rupture of an intracranial aneurysm*
- A ruptured intracranial aneurysm usually causes a **subarachnoid hemorrhage**, leading to a sudden, severe headache ("thunderclap headache"), meningismus, and altered consciousness.
- While focal neurological deficits can occur, the primary presentation is distinct from the patient's symptoms of a gradual onset of pure motor deficit.
*Embolism from the left atrium*
- An embolism from the left atrium (e.g., due to atrial fibrillation) typically causes a **cortical infarct** involving a larger vascular territory, such as the middle cerebral artery.
- This would result in symptoms like **aphasia**, **neglect**, or **cortical sensory deficits**, which are absent in this presentation of pure motor hemiparesis.
Secondary stroke prevention US Medical PG Question 8: A 78-year-old man is brought in to the emergency department by ambulance after his wife noticed that he began slurring his speech and had developed facial asymmetry during dinner approximately 30 minutes ago. His past medical history is remarkable for hypertension and diabetes. His temperature is 99.1°F (37.3°C), blood pressure is 154/99 mmHg, pulse is 89/min, respirations are 12/min, and oxygen saturation is 98% on room air. Neurologic exam reveals right upper and lower extremity weakness and an asymmetric smile. Which of the following is the next best step in management?
- A. Alteplase
- B. MRI brain
- C. CT head (Correct Answer)
- D. Aspirin
- E. CTA head
Secondary stroke prevention Explanation: ***CT head***
- A **non-contrast CT head** is the immediate priority to differentiate between ischemic and hemorrhagic stroke, which is critical for guiding subsequent treatment decisions.
- Given the patient's acute neurological deficits (slurred speech, facial asymmetry, weakness) and vascular risk factors (hypertension, diabetes), **stroke is highly suspected**, and identifying intracerebral hemorrhage is crucial before considering thrombolytic therapy.
*Alteplase*
- **Alteplase** (tPA) is a thrombolytic agent used for acute ischemic stroke, but its administration is **contraindicated in hemorrhagic stroke**.
- Initiating alteplase without first ruling out hemorrhage with a CT scan could lead to catastrophic bleeding.
*MRI brain*
- While an **MRI brain** can provide more detailed imaging of stroke, it is typically **not the initial imaging modality** in the emergency setting due to longer acquisition times and limited availability, especially when emergent differentiation between ischemic and hemorrhagic stroke is needed.
- Its use is usually reserved for cases where the CT is inconclusive or for later evaluation.
*Aspirin*
- **Aspirin** is an antiplatelet agent used in the management of ischemic stroke, but it should **not be given until a hemorrhagic stroke has been ruled out** via CT head.
- Administering aspirin in the context of an intracerebral hemorrhage could worsen bleeding.
*CTA head*
- A **CT angiography (CTA) head** is used to visualize the cerebral vasculature and identify large vessel occlusions, which can guide thrombectomy decisions in ischemic stroke.
- However, performing a **non-contrast CT head is a prerequisite** to rule out hemorrhage before proceeding with CTA or any other advanced imaging or therapeutic interventions.
Secondary stroke prevention US Medical PG Question 9: Drug A is an experimental compound being investigated for potential use as a protectant against venous thrombosis. Binding assays reveal that the drug’s primary mechanism of action is to block carboxylation of glutamic acid residues in certain serum proteins. Drug A is most similar to which of the following:
- A. Streptokinase
- B. Bivalirudin
- C. Warfarin (Correct Answer)
- D. Heparin
- E. Rivaroxaban
Secondary stroke prevention Explanation: ***Warfarin***
- Warfarin inhibits **vitamin K epoxide reductase**, enzyme responsible for regenerating active vitamin K.
- Active vitamin K is a cofactor for the **gamma-carboxylation of glutamic acid residues** on factors II, VII, IX, X and protein C and S. Thus, warfarin blocks their activation, inhibiting coagulation.
*Steptokinase*
- **Streptokinase** is a **thrombolytic drug** that catalyzes the conversion of **plasminogen to plasmin**, an enzyme that degrades fibrin clots.
- Its mechanism of action is focused on **breaking down existing clots**, rather than preventing their formation by affecting coagulation factor synthesis.
*Bivalirudin*
- **Bivalirudin** is a direct **thrombin inhibitor**, binding directly to the active site and exosite I of thrombin to prevent its action.
- It does not interfere with the **carboxylation of glutamic acid residues** but rather directly inhibits the final common pathway of coagulation.
*Heparin*
- **Heparin** works by potentiating the action of **antithrombin III**, which in turn inactivates thrombin and factor Xa.
- Its mechanism involves accelerating the natural anticoagulant system, rather than inhibiting the **synthesis or activation of coagulation factors** through carboxylation.
*Rivaroxaban*
- **Rivaroxaban** is a **direct factor Xa inhibitor**, which blocks the activity of free and clot-bound factor Xa.
- It directly interferes with the coagulation cascade downstream of the carboxylation step, and does not affect the **vitamin K-dependent carboxylation process**.
Secondary stroke prevention US Medical PG Question 10: A 48-year-old woman presents with acute stroke symptoms 18 hours ago. MRI shows a right MCA M1 occlusion with large penumbra on perfusion imaging (mismatch ratio >1.8) and small infarct core (25 mL). Her NIHSS is 16. She has no significant comorbidities. Her family is concerned about disability but wants to pursue treatment if reasonable chance of benefit exists. Synthesize the evidence and evaluate the treatment approach.
- A. Intravenous alteplase as salvageable tissue is present
- B. Intra-arterial thrombolysis combined with mechanical device
- C. No intervention as she is outside the standard treatment window
- D. Mechanical thrombectomy based on perfusion imaging criteria (Correct Answer)
- E. Medical management with antiplatelet and early rehabilitation
Secondary stroke prevention Explanation: ***Mechanical thrombectomy based on perfusion imaging criteria***
- For patients with large vessel occlusion (LVO) in the extended 6–24 hour window, **DAWN** and **DEFUSE-3** trials demonstrated significant functional benefit when clinical-core mismatch is present.
- This patient satisfies criteria with an **M1 occlusion**, a **small infarct core (<70 mL)**, and a **large mismatch ratio (>1.8)**, indicating substantial salvageable penumbra.
*Intravenous alteplase as salvageable tissue is present*
- The therapeutic window for **IV alteplase** is strictly limited to within **4.5 hours** of symptom onset; it is not recommended at 18 hours due to high hemorrhage risk.
- While salvageable tissue exists, chemical thrombolysis is less effective than mechanical intervention for **proximal M1 occlusions** and is unsafe in this late window.
*Intra-arterial thrombolysis combined with mechanical device*
- **Intra-arterial thrombolysis** is generally superseded by modern **stent retrievers** and aspiration catheters which provide faster and more complete recanalization.
- Current guidelines prioritize standalone **mechanical thrombectomy** in the late window to minimize procedural risks and intracranial hemorrhage.
*No intervention as she is outside the standard treatment window*
- The "Time is Brain" concept has evolved into "Tissue is Brain," where **perfusion imaging** identifies candidates who benefit regardless of the traditional 6-hour clock.
- Denying treatment based solely on the 18-hour timeframe ignores high-level evidence from the **DAWN** trial showing benefit up to 24 hours.
*Medical management with antiplatelet and early rehabilitation*
- Standard **medical management** (aspirin/heparin) for an M1 occlusion with a high **NIHSS score (16)** usually results in poor functional outcomes and severe disability.
- While rehabilitation is essential, it does not address the underlying **large vessel occlusion** which can be reversed with mechanical intervention to prevent infarct expansion.
More Secondary stroke prevention US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.