Rehabilitation principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Rehabilitation principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Rehabilitation principles US Medical PG Question 1: A 68-year-old woman is brought to the emergency department by her husband because of acute confusion and sudden weakness of her left leg that lasted for about 30 minutes. One hour prior to admission, she was unable to understand words and had slurred speech for about 15 minutes. She has type 2 diabetes mellitus and hypertension. She has smoked 1 pack of cigarettes daily for 30 years. Current medications include metformin and hydrochlorothiazide. Her pulse is 110/min and irregular; blood pressure is 135/84 mmHg. Examination shows cold extremities. There is a mild bruit heard above the left carotid artery. Cardiac examination shows a grade 2/6 late systolic ejection murmur that begins with a midsystolic click. Neurological and mental status examinations show no abnormalities. An ECG shows irregularly spaced QRS complexes with no discernible P waves. Doppler ultrasonography shows mild left carotid artery stenosis. A CT scan and diffusion-weighted MRI of the brain show no abnormalities. Which of the following treatments is most likely to prevent future episodes of neurologic dysfunction in this patient?
- A. Warfarin (Correct Answer)
- B. Enalapril
- C. Alteplase
- D. Aspirin
- E. Mitral valve replacement
Rehabilitation principles Explanation: ***Warfarin***
- The patient experienced a **transient ischemic attack (TIA)** due to **atrial fibrillation** as indicated by the irregular pulse and ECG findings of irregularly spaced QRS complexes with no discernible P waves. Atrial fibrillation significantly increases the risk of stroke due to thrombus formation in the atria.
- **Warfarin**, or other oral anticoagulants (e.g., direct oral anticoagulants), is crucial for preventing future embolic events by reducing the risk of clot formation in the heart.
- The patient has a high CHADS₂-VASc score (age ≥65, hypertension, diabetes, prior TIA), making anticoagulation the standard of care.
*Mitral valve replacement*
- The patient has a grade 2/6 late systolic murmur with a midsystolic click, which is classic for **mitral valve prolapse (MVP)**. While MVP can rarely be associated with embolic events, it is typically benign and does not require surgical intervention unless there is severe mitral regurgitation with heart failure symptoms.
- The primary cause of this patient's neurologic dysfunction is **atrial fibrillation**, not structural valve disease. There are no clinical signs of severe mitral regurgitation (pulmonary edema, severe heart failure) that would warrant valve replacement.
- Anticoagulation for atrial fibrillation addresses the root cause of the embolic risk.
*Enalapril*
- Enalapril is an **ACE inhibitor** used to treat hypertension and heart failure. While managing hypertension is important for stroke prevention, it does not address the underlying thrombogenic risk from atrial fibrillation.
- Although blood pressure control is part of comprehensive stroke prevention, her transient neurological events are cardioembolic, making anticoagulation the priority for primary prevention.
*Alteplase*
- **Alteplase** (tissue plasminogen activator) is a thrombolytic agent used to treat acute ischemic stroke, typically administered within a narrow time window after symptom onset. This patient's symptoms were transient and resolved (TIA), and she is currently asymptomatic with no acute stroke on imaging.
- Administering alteplase to a patient post-TIA with no active stroke would be inappropriate and potentially harmful due to the risk of bleeding.
- Alteplase treats acute strokes; it does not prevent future events.
*Aspirin*
- **Aspirin** is an antiplatelet agent used for secondary stroke prevention in patients with atherosclerotic disease or non-cardioembolic TIAs. However, for cardioembolic events due to atrial fibrillation, aspirin alone is insufficient.
- Patients with atrial fibrillation require **anticoagulation (e.g., warfarin or DOACs)**, which is significantly more effective than antiplatelet therapy in preventing stroke from atrial fibrillation.
- The mild carotid stenosis noted is not severe enough to be the primary cause of her symptoms.
Rehabilitation principles US Medical PG Question 2: A 4-year-old boy is brought to the physician because of non-fluent speech. His mother worries that his vocabulary is limited for his age and because he cannot use simple sentences to communicate. She says he enjoys playing with his peers and parents, but he has always lagged behind in his speaking and communication. His speech is frequently not understood by strangers. He physically appears normal. His height and weight are within the normal range for his age. He responds to his name, makes eye contact, and enjoys the company of his mother. Which of the following is the most appropriate next step in management?
- A. Referral to speech therapist
- B. Evaluate response to methylphenidate
- C. Psychiatric evaluation
- D. Audiology testing (Correct Answer)
- E. Thyroid-stimulating hormone
Rehabilitation principles Explanation: ***Audiology testing***
- Before initiating any therapy for speech delay, it is crucial to rule out **hearing impairment**, as **undiagnosed hearing loss** is the most common organic cause of speech and language difficulties in children.
- **Standard practice guidelines** (AAP) recommend hearing assessment as the **first diagnostic step** in evaluating any child with speech or language delay.
- While other developmental aspects seem intact, the inability to use simple sentences at age 4 and speech that is "frequently not understood by strangers" strongly suggests the need to assess the child's ability to **receive auditory information**.
*Referral to speech therapist*
- While a **speech therapist referral** is highly appropriate for a child with significant speech delay, it should typically follow an assessment to rule out underlying organic causes like **hearing loss**.
- Without addressing potential hearing impairment, speech therapy may be less effective or miss the root cause of the communication difficulty.
*Evaluate response to methylphenidate*
- **Methylphenidate** is a stimulant medication used primarily for **attention-deficit/hyperactivity disorder (ADHD)**.
- There is no indication of ADHD symptoms in this child (e.g., inattention, hyperactivity, impulsivity), and it is not a treatment for **primary speech delay**.
*Psychiatric evaluation*
- The child's ability to respond to his name, make eye contact, and enjoy social interaction with family and peers makes a **primary psychiatric disorder** (like autism spectrum disorder) less likely to be the sole cause of the speech delay.
- Such an evaluation would typically be considered if **social communication deficits**, repetitive behaviors, or restricted interests were prominent.
*Thyroid-stimulating hormone*
- **Hypothyroidism** can cause developmental delays, including speech delay.
- However, the child's normal physical appearance, height, and weight make **congenital or acquired hypothyroidism** less likely to be the primary cause of his isolated speech delay.
Rehabilitation principles US Medical PG Question 3: A psychiatrist receives a call from a patient who expresses thoughts of harming his ex-girlfriend. The patient describes a detailed plan to attack her at her workplace. Which of the following represents the psychiatrist's most appropriate legal obligation?
- A. Warn the ex-girlfriend and notify law enforcement (Correct Answer)
- B. Only notify the patient's family
- C. Warn only law enforcement
- D. Maintain patient confidentiality
Rehabilitation principles Explanation: ***Warn the ex-girlfriend and notify law enforcement***
- This scenario directly triggers the **"duty to warn"** and **"duty to protect"** principles, primarily stemming from the **Tarasoff v. Regents of the University of California** case.
- The psychiatrist has a legal obligation to take reasonable steps to protect the identifiable victim, which includes directly warning the intended victim and informing law enforcement.
*Only notify the patient's family*
- Notifying the patient's family alone does not fulfill the **legal obligation to protect** an identifiable third party from a serious threat of harm.
- While family involvement might be part of a comprehensive safety plan, it is insufficient as the sole action in this critical situation.
*Warn only law enforcement*
- While notifying law enforcement is a crucial step, the **Tarasoff duty** specifically mandates warning the **intended victim** directly (or those who can reasonably be expected to notify the victim).
- Relying solely on law enforcement might not ensure the immediate safety of the ex-girlfriend, especially if there's a delay in their response or ability to locate her.
*Maintain patient confidentiality*
- Patient confidentiality is a cornerstone of psychiatric practice, but it is **not absolute** when there is a serious and imminent threat of harm to an identifiable individual.
- The **duty to protect** a potential victim *outweighs* the duty to maintain confidentiality in such extreme circumstances.
Rehabilitation principles US Medical PG Question 4: A 78-year-old woman is accompanied by her family for a routine visit to her primary care provider. The family states that 5 months prior, the patient had a stroke and is currently undergoing physical therapy. Today, her temperature is 98.2°F (36.8°C), blood pressure is 112/72 mmHg, pulse is 64/min, and respirations are 12/min. On exam, she is alert and oriented with no deficits in speech. Additionally, her strength and sensation are symmetric and preserved bilaterally. However, on further neurologic testing, she appears to have some difficulty with balance and a propensity to fall to her right side. Which of the following deficits does the patient also likely have?
- A. Hemiballismus
- B. Hemispatial neglect
- C. Intention tremor
- D. Contralateral eye deviation
- E. Truncal ataxia (Correct Answer)
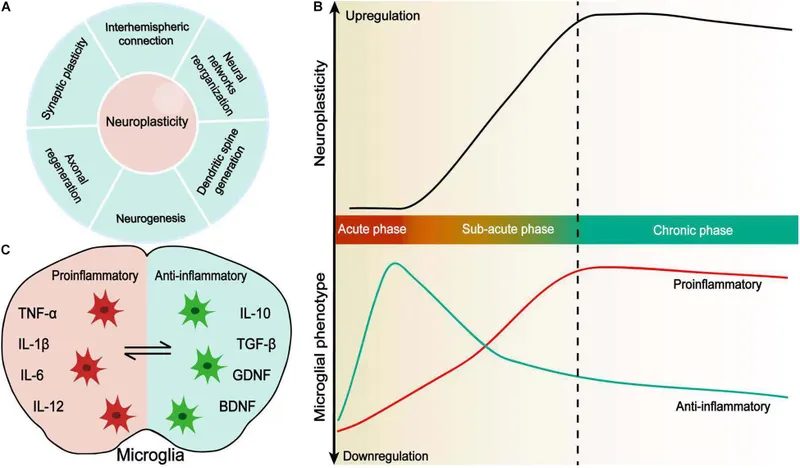
Rehabilitation principles Explanation: ***Truncal ataxia***
- This patient's symptoms of **difficulty with balance** and a **propensity to fall to her right side** are highly suggestive of truncal ataxia.
- While she had a stroke, her preserved speech, symmetric strength and sensation, and alertness rule out typical hemiparesis or aphasia, pointing towards a **cerebellar lesion** affecting balance and coordination.
*Hemiballismus*
- This condition involves **flailing, high-amplitude, involuntary movements** typically affecting one side of the body.
- The patient's description of balance issues and falling, without mention of such specific movements, makes hemiballismus less likely.
*Hemispatial neglect*
- Characterized by the **inability to attend to one side of the environment**, usually the left side following a right parietal stroke.
- The patient's presentation does not describe an indifference to one side of her visual or personal space.
*Intention tremor*
- An **intention tremor** is a tremor that worsens during purposeful movement towards a target.
- While it can be associated with cerebellar dysfunction, the primary deficit described is imbalance and falling to one side, not specifically a tremor.
*Contralateral eye deviation*
- This typically occurs in acute stroke scenarios as part of a **gaze preference**, where the eyes deviate towards the side of the lesion (or away from the hemiparesis).
- The patient is 5 months post-stroke and is alert with no acute focal deficits, making acute eye deviation unlikely as a chronic presenting symptom here.
Rehabilitation principles US Medical PG Question 5: A 78-year-old man is brought in to the emergency department by ambulance after his wife noticed that he began slurring his speech and had developed facial asymmetry during dinner approximately 30 minutes ago. His past medical history is remarkable for hypertension and diabetes. His temperature is 99.1°F (37.3°C), blood pressure is 154/99 mmHg, pulse is 89/min, respirations are 12/min, and oxygen saturation is 98% on room air. Neurologic exam reveals right upper and lower extremity weakness and an asymmetric smile. Which of the following is the next best step in management?
- A. Alteplase
- B. MRI brain
- C. CT head (Correct Answer)
- D. Aspirin
- E. CTA head
Rehabilitation principles Explanation: ***CT head***
- A **non-contrast CT head** is the immediate priority to differentiate between ischemic and hemorrhagic stroke, which is critical for guiding subsequent treatment decisions.
- Given the patient's acute neurological deficits (slurred speech, facial asymmetry, weakness) and vascular risk factors (hypertension, diabetes), **stroke is highly suspected**, and identifying intracerebral hemorrhage is crucial before considering thrombolytic therapy.
*Alteplase*
- **Alteplase** (tPA) is a thrombolytic agent used for acute ischemic stroke, but its administration is **contraindicated in hemorrhagic stroke**.
- Initiating alteplase without first ruling out hemorrhage with a CT scan could lead to catastrophic bleeding.
*MRI brain*
- While an **MRI brain** can provide more detailed imaging of stroke, it is typically **not the initial imaging modality** in the emergency setting due to longer acquisition times and limited availability, especially when emergent differentiation between ischemic and hemorrhagic stroke is needed.
- Its use is usually reserved for cases where the CT is inconclusive or for later evaluation.
*Aspirin*
- **Aspirin** is an antiplatelet agent used in the management of ischemic stroke, but it should **not be given until a hemorrhagic stroke has been ruled out** via CT head.
- Administering aspirin in the context of an intracerebral hemorrhage could worsen bleeding.
*CTA head*
- A **CT angiography (CTA) head** is used to visualize the cerebral vasculature and identify large vessel occlusions, which can guide thrombectomy decisions in ischemic stroke.
- However, performing a **non-contrast CT head is a prerequisite** to rule out hemorrhage before proceeding with CTA or any other advanced imaging or therapeutic interventions.
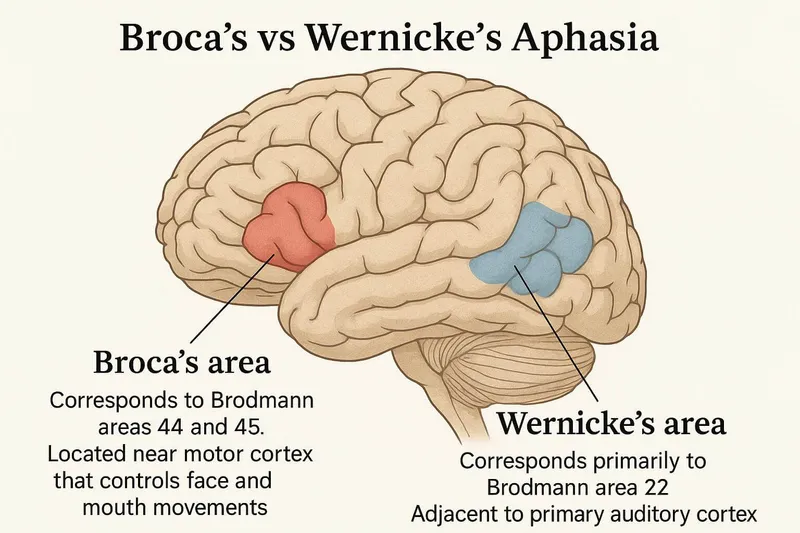
Rehabilitation principles US Medical PG Question 6: A 73-year-old man is brought to the emergency department by ambulance after being found to be non-communicative by his family during dinner. On presentation he appears to be alert, though he is confused and cannot follow instructions. When he tries to speak, he vocalizes a string of fluent but unintelligible syllables. Given this presentation, his physician decides to administer tissue plasminogen activator to this patient. This intervention best represents which of the following principles?
- A. Tertiary prevention
- B. Primary prevention
- C. This does not represent prevention (Correct Answer)
- D. Quaternary prevention
- E. Secondary prevention
Rehabilitation principles Explanation: ***This does not represent prevention***
- The administration of **tissue plasminogen activator (tPA)** during an **acute stroke** is a **therapeutic intervention**, not a form of prevention.
- **Prevention** refers to actions taken to prevent disease occurrence, detect it early, or prevent complications after recovery. Treating an acute, symptomatic event is **acute treatment**, not prevention.
- This is an active medical intervention to treat an ongoing, symptomatic disease process (acute ischemic stroke), which falls under **therapeutic management** rather than any category of prevention.
*Secondary prevention*
- **Secondary prevention** involves **early detection** and treatment of asymptomatic or minimally symptomatic disease to prevent progression (e.g., screening mammography, colonoscopy).
- For stroke specifically, secondary prevention would include interventions **after** the acute event to **prevent recurrence**, such as starting antiplatelet therapy (aspirin, clopidogrel), anticoagulation for atrial fibrillation, statin therapy, or carotid endarterectomy after TIA.
- tPA is given during the acute symptomatic phase, making it treatment rather than secondary prevention.
*Tertiary prevention*
- **Tertiary prevention** focuses on **rehabilitation** and managing established disease to prevent complications and improve quality of life.
- Examples after stroke include physical therapy, occupational therapy, speech therapy, and managing post-stroke complications like depression or spasticity.
- This occurs in the recovery phase, not during acute treatment.
*Primary prevention*
- **Primary prevention** aims to prevent disease before it occurs in healthy individuals.
- Examples include controlling hypertension, managing diabetes, smoking cessation, exercise, and healthy diet - all interventions that reduce stroke risk **before** any event occurs.
*Quaternary prevention*
- **Quaternary prevention** protects patients from **overmedicalization** and excessive or harmful medical interventions.
- It involves avoiding unnecessary testing or treatment that may cause more harm than benefit.
- Administering tPA for acute stroke (when indicated) is evidence-based treatment, not overtreatment.
Rehabilitation principles US Medical PG Question 7: A 48-year-old woman presents with acute stroke symptoms 18 hours ago. MRI shows a right MCA M1 occlusion with large penumbra on perfusion imaging (mismatch ratio >1.8) and small infarct core (25 mL). Her NIHSS is 16. She has no significant comorbidities. Her family is concerned about disability but wants to pursue treatment if reasonable chance of benefit exists. Synthesize the evidence and evaluate the treatment approach.
- A. Intravenous alteplase as salvageable tissue is present
- B. Intra-arterial thrombolysis combined with mechanical device
- C. No intervention as she is outside the standard treatment window
- D. Mechanical thrombectomy based on perfusion imaging criteria (Correct Answer)
- E. Medical management with antiplatelet and early rehabilitation
Rehabilitation principles Explanation: ***Mechanical thrombectomy based on perfusion imaging criteria***
- For patients with large vessel occlusion (LVO) in the extended 6–24 hour window, **DAWN** and **DEFUSE-3** trials demonstrated significant functional benefit when clinical-core mismatch is present.
- This patient satisfies criteria with an **M1 occlusion**, a **small infarct core (<70 mL)**, and a **large mismatch ratio (>1.8)**, indicating substantial salvageable penumbra.
*Intravenous alteplase as salvageable tissue is present*
- The therapeutic window for **IV alteplase** is strictly limited to within **4.5 hours** of symptom onset; it is not recommended at 18 hours due to high hemorrhage risk.
- While salvageable tissue exists, chemical thrombolysis is less effective than mechanical intervention for **proximal M1 occlusions** and is unsafe in this late window.
*Intra-arterial thrombolysis combined with mechanical device*
- **Intra-arterial thrombolysis** is generally superseded by modern **stent retrievers** and aspiration catheters which provide faster and more complete recanalization.
- Current guidelines prioritize standalone **mechanical thrombectomy** in the late window to minimize procedural risks and intracranial hemorrhage.
*No intervention as she is outside the standard treatment window*
- The "Time is Brain" concept has evolved into "Tissue is Brain," where **perfusion imaging** identifies candidates who benefit regardless of the traditional 6-hour clock.
- Denying treatment based solely on the 18-hour timeframe ignores high-level evidence from the **DAWN** trial showing benefit up to 24 hours.
*Medical management with antiplatelet and early rehabilitation*
- Standard **medical management** (aspirin/heparin) for an M1 occlusion with a high **NIHSS score (16)** usually results in poor functional outcomes and severe disability.
- While rehabilitation is essential, it does not address the underlying **large vessel occlusion** which can be reversed with mechanical intervention to prevent infarct expansion.
Rehabilitation principles US Medical PG Question 8: A 55-year-old man undergoes successful thrombectomy for left MCA occlusion. Post-procedure, he develops progressive lethargy and his blood pressure increases to 180/100 mmHg. CT shows hyperdensity in the treated territory without hemorrhage, and his symptoms worsen over 4 hours despite blood pressure control. Evaluate the most likely diagnosis and management priority.
- A. Hemorrhagic transformation; reverse anticoagulation immediately
- B. Cerebral edema from large infarction; emergent decompressive hemicraniectomy
- C. Reperfusion injury; start high-dose corticosteroids and osmotic therapy
- D. Contrast extravasation from blood-brain barrier disruption; supportive care and avoid aggressive BP lowering (Correct Answer)
- E. Recurrent arterial occlusion; emergent repeat angiography and thrombectomy
Rehabilitation principles Explanation: ***Contrast extravasation from blood-brain barrier disruption; supportive care and avoid aggressive BP lowering***
- Post-thrombectomy **hyperdensity** on CT often represents contrast that leaked through an ischemic **blood-brain barrier**, which can mimic hemorrhage but lacks significant **mass effect**.
- Management is **supportive care** because the contrast is typically reabsorbed within 24–48 hours; avoiding aggressive **blood pressure lowering** prevents secondary ischemia in the penumbra.
*Hemorrhagic transformation; reverse anticoagulation immediately*
- While **hemorrhagic transformation** is a risk, true blood usually demonstrates higher density earlier and is associated with rapid clinical decline and **midline shift**.
- Reversing anticoagulation without confirming blood on a follow-up **dual-energy CT** or MRI may lead to **stent thrombosis** or re-occlusion.
*Cerebral edema from large infarction; emergent decompressive hemicraniectomy*
- **Cerebral edema** typically peaks between 72–96 hours post-stroke; a presentation within 4 hours is too acute for **malignant MCA syndrome**.
- While edema causes lethargy, the hyperdensity on CT more specifically points toward **contrast staining** or blood rather than simple cytotoxic edema.
*Reperfusion injury; start high-dose corticosteroids and osmotic therapy*
- **Corticosteroids** are not indicated for stroke-related edema or reperfusion injury as they do not improve outcomes and may increase **infection risk**.
- **Osmotic therapy** is reserved for patients with clear clinical or radiologic signs of **elevated intracranial pressure**, not isolated hyperdensity on CT.
*Recurrent arterial occlusion; emergent repeat angiography and thrombectomy*
- **Recurrent occlusion** usually presents with a sudden recurrence of the original **focal neurological deficits** (e.g., hemiplegia, aphasia) rather than progressive lethargy.
- The presence of **hyperdensity** in the stroke territory on CT is specifically indicative of material (contrast or blood) being present, which is not a feature of a simple **re-occlusion**.
Rehabilitation principles US Medical PG Question 9: An 80-year-old woman with atrial fibrillation presents 2 hours after acute ischemic stroke. NIHSS is 22. Imaging shows large left MCA territory infarction involving >1/3 of MCA territory with basilar artery occlusion. She lives alone but was independent before this event. Her family requests all possible interventions. Evaluate the management approach considering benefits versus risks.
- A. Comfort measures only given poor prognosis and age
- B. Thrombolysis alone as thrombectomy unlikely to benefit with established large infarction
- C. Proceed with thrombolysis and thrombectomy given the therapeutic window
- D. Thrombectomy only for basilar occlusion, avoid thrombolysis due to large infarction (Correct Answer)
- E. Delay intervention and repeat imaging in 6 hours to assess progression
Rehabilitation principles Explanation: ***Thrombectomy only for basilar occlusion, avoid thrombolysis due to large infarction***
- Intravenous **thrombolysis (IV alteplase)** is generally contraindicated or highly risky when imaging shows an established infarction involving **>1/3 of the MCA territory** due to the high risk of **hemorrhagic transformation**.
- **Basilar artery occlusion** is a life-threatening emergency with a broader treatment window; mechanical **thrombectomy** can be lifesaving and is indicated even if thrombolysis is withheld.
*Comfort measures only given poor prognosis and age*
- Age is not a primary contraindication for intervention, especially since the patient was **independent** prior to the event (low **pre-stroke mRS**).
- Family requests all possible interventions, and **basilar occlusion** has a catastrophic natural history that may be mitigated by mechanical intervention.
*Thrombolysis alone as thrombectomy unlikely to benefit with established large infarction*
- Thrombolysis is dangerous in this context due to the **large infarct volume** seen on imaging, which increases the likelihood of fatal **intracerebral hemorrhage**.
- Thrombolysis is notably less effective for large vessel occlusions compared to **mechanical thrombectomy**, which is the gold standard for **basilar artery** recanalization.
*Proceed with thrombolysis and thrombectomy given the therapeutic window*
- While the patient is within the 4.5-hour window for thrombolysis, the presence of **established early ischemic changes** (>1/3 MCA territory) is a relative contraindication.
- Attempting both increases the risk of **secondary hemorrhage** in the damaged MCA territory without providing significant additional benefit over thrombectomy alone for the **basilar occlusion**.
*Delay intervention and repeat imaging in 6 hours to assess progression*
- Delaying treatment in the setting of **basilar artery occlusion** is inappropriate, as "time is brain" and outcomes worsen significantly with every minute of **brainstem ischemia**.
- Immediate decision-making is required based on the initial imaging, which already confirmed the **large-vessel occlusion** needing intervention.
Rehabilitation principles US Medical PG Question 10: A 58-year-old woman with history of TIA 3 weeks ago presents with acute ischemic stroke. Imaging reveals new right MCA infarction and severe (70-99%) symptomatic right carotid stenosis. She received alteplase 6 hours ago with partial improvement. Her NIHSS improved from 14 to 8. Analyze the optimal timing for carotid revascularization.
- A. Wait 4-6 weeks to reduce hemorrhagic transformation risk
- B. Carotid stenting immediately after thrombolysis
- C. Emergent carotid endarterectomy within 24 hours
- D. Carotid endarterectomy within 2 weeks of symptom onset (Correct Answer)
- E. Medical management only due to recent thrombolysis
Rehabilitation principles Explanation: ***Carotid endarterectomy within 2 weeks of symptom onset***
- For patients with **symptomatic carotid stenosis** (70-99%), early revascularization within **2 weeks** (ideally within 48 hours to 7 days) provides the maximum benefit in preventing recurrent stroke.
- Current guidelines suggest that once the patient is **neurologically stable** and the infarct size is not massive, the risk of recurrence outweighs the risk of **hemorrhagic transformation**.
*Wait 4-6 weeks to reduce hemorrhagic transformation risk*
- This represents older clinical practice; modern evidence shows the risk of **recurrent stroke** is highest in the first 2 weeks, making this delay dangerous.
- Waiting this long is only typically reserved for patients with a **large territory infarct** (high NIHSS) or those at very high risk for bleeding complications.
*Carotid stenting immediately after thrombolysis*
- Immediate stenting right after **alteplase** administration increases the risk of **intracranial hemorrhage** and local bleeding at the access site due to systemic fibrinolysis.
- While **Carotid Artery Stenting (CAS)** is an alternative, it is generally not preferred over **Carotid Endarterectomy (CEA)** in older patients unless specific surgical contraindications exist.
*Emergent carotid endarterectomy within 24 hours*
- Performing surgery within the first 24 hours after **thrombolytic therapy** carries a significant risk of **hemorrhagic transformation** of the fresh infarct.
- Most surgeons prefer to wait at least **24-48 hours** post-alteplase to ensure the fibrinolytic effects have resolved and the patient's neurological status is stable.
*Medical management only due to recent thrombolysis*
- Medical management alone is insufficient for **symptomatic stenosis >70%**, as the risk of a disabling stroke remains high without mechanical intervention.
- **Dual antiplatelet therapy** and statins are vital, but they serve as an adjunct to, rather than a replacement for, **surgical revascularization** in fit patients.
More Rehabilitation principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.