Management of stroke complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Management of stroke complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
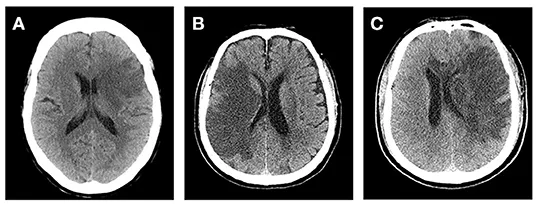
Management of stroke complications US Medical PG Question 1: A 69-year-old man is brought in by his wife with acute onset aphasia for the past 5 hours. The patient's wife says that they were sitting having dinner when suddenly he was not able to speak. They delayed coming to the hospital because he had a similar episode 2 months ago which resolved within an hour. His past medical history is significant for hypercholesterolemia, managed with rosuvastatin, and a myocardial infarction (MI) 2 months ago, status post percutaneous transluminal coronary angioplasty complicated by residual angina. His family history is significant for his father who died of MI at age 60. The patient reports a 15-pack-year smoking history but denies any alcohol or recreational drug use. The vital signs include: temperature 37.0℃ (98.6℉), blood pressure 125/85 mm Hg, pulse 96/min, and respiratory rate 19/min. On physical examination, the patient has expressive aphasia. There is a weakness of the right-sided lower facial muscles. The strength in his upper and lower extremities is 4/5 on the right and 5/5 on the left. There is also a decreased sensation on his right side. A noncontrast computed tomography (CT) scan of the head is unremarkable. CT angiography (CTA) and diffusion-weighted magnetic resonance imaging (MRI) of the brain are acquired, and the findings are shown in the exhibit (see image). Which of the following is the best course of treatment in this patient?
- A. Aspirin
- B. Mannitol
- C. Mechanical thrombectomy (Correct Answer)
- D. IV tPA
- E. Low molecular weight heparin
Management of stroke complications Explanation: ***Mechanical thrombectomy***
- The patient presents with **acute ischemic stroke** symptoms (aphasia, right-sided weakness, sensory deficits) at **5 hours from symptom onset**. Imaging (CTA showing large vessel occlusion and MRI confirming diffusion restriction) demonstrates a **large vessel occlusion**, making him a candidate for **mechanical thrombectomy**.
- Since the patient is **beyond the 4.5-hour window for IV tPA**, mechanical thrombectomy is the **primary reperfusion therapy** indicated for large vessel occlusion strokes up to **24 hours** (with appropriate imaging showing salvageable tissue).
- Mechanical thrombectomy offers the best chance for complete recanalization and improved neurological outcomes in large vessel occlusion strokes, particularly when IV tPA is not an option.
*Aspirin*
- While **aspirin** is crucial for **secondary stroke prevention**, it is not the primary acute treatment for a large vessel occlusion stroke due to its limited ability to achieve rapid and complete recanalization.
- Aspirin (or other antiplatelet therapy) is typically initiated **within 24-48 hours after stroke onset**, but only after excluding hemorrhagic transformation and after acute reperfusion therapies have been considered or completed.
*Mannitol*
- **Mannitol** is an osmotic diuretic used to reduce **intracranial pressure (ICP)** in cases of severe cerebral edema, which can be a complication of large ischemic strokes.
- It is not a primary treatment for the acute ischemic event itself, but rather a supportive measure used to manage life-threatening complications if **cerebral edema** develops and causes significant mass effect or herniation risk.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is the first-line pharmacologic treatment for acute ischemic stroke if administered **within 4.5 hours of symptom onset** in eligible patients.
- This patient presents at **5 hours**, which is **beyond the approved time window** for IV tPA administration, making him **ineligible** for thrombolytic therapy.
- Even if within the time window, patients with large vessel occlusion often require mechanical thrombectomy in addition to or instead of IV tPA for optimal outcomes.
*Low molecular weight heparin*
- **Low molecular weight heparin (LMWH)** is primarily used for **deep vein thrombosis (DVT)** prophylaxis in immobilized patients or for the treatment of established DVT/pulmonary embolism.
- It is generally **not recommended for acute ischemic stroke treatment** due to an increased risk of hemorrhagic transformation without proven benefit in recanalization or clinical outcomes.
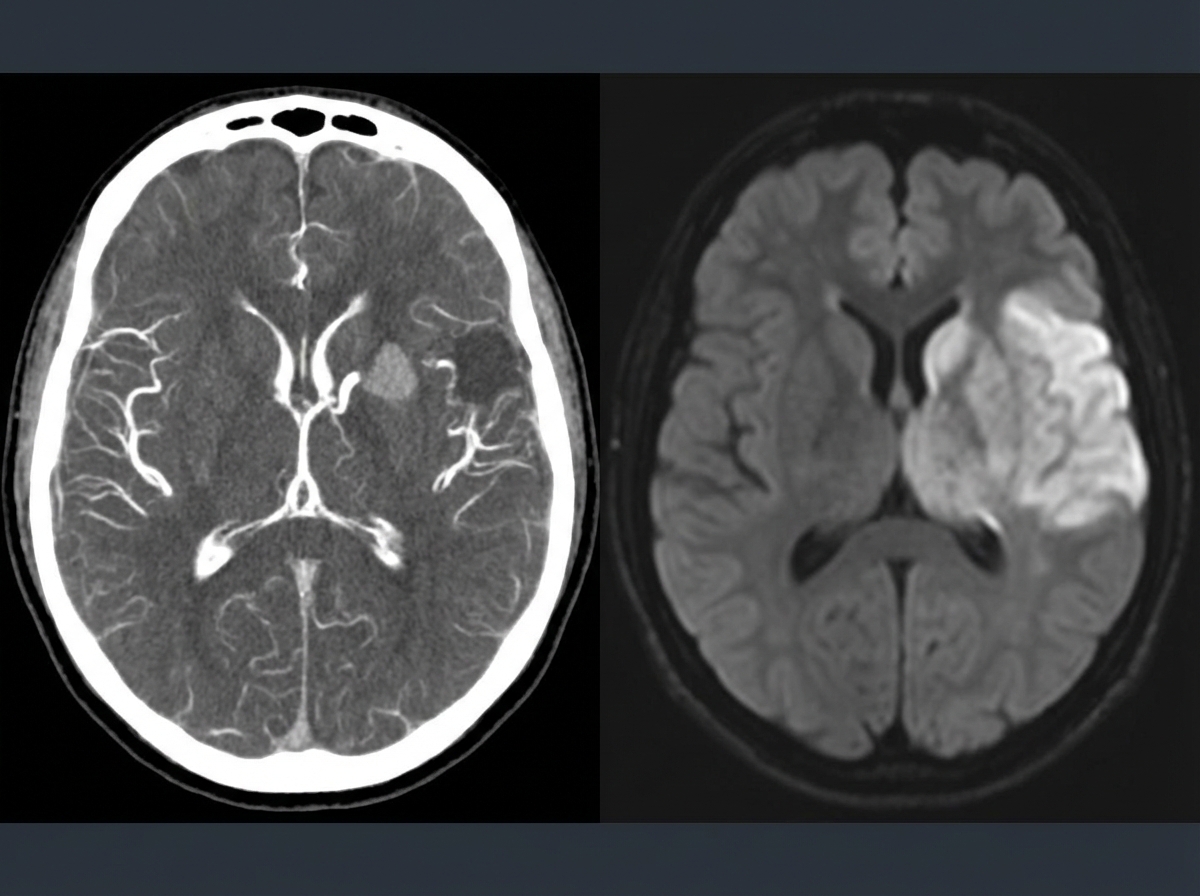
Management of stroke complications US Medical PG Question 2: A 45-year-old man presents to the emergency department with complaints of right-sided weakness and slurring of speech for 1 hour. There is no history of head trauma, myocardial infarction, recent surgery, gastrointestinal or urinary bleeding. He has hypertension, chronic atrial fibrillation, and a 20 pack-year cigarette smoking history. The medication list includes valsartan and rivaroxaban. The vital signs include: blood pressure 180/92 mm Hg, pulse 144/min and irregular, and temperature 37.2°C (99.0°F). On physical examination, there is a facial asymmetry with a deviation of angle of mouth to the left side on smiling. Muscle strength is reduced in both upper and lower limbs on the right side while on the left side it’s normal. Random blood glucose is 104 mg/dL. A complete blood count is normal. A CT scan of the head is shown in the image. What is the most appropriate next step in the management of this patient?
- A. Heparin
- B. Amiodarone
- C. Metoprolol
- D. Tissue plasminogen activator
- E. Aspirin (Correct Answer)
Management of stroke complications Explanation: ***Aspirin***
- The patient presents with acute onset **neurological deficits** (right-sided weakness, slurred speech) consistent with an **ischemic stroke** in the setting of **atrial fibrillation**.
- The CT scan shows no evidence of hemorrhage (hypodense or normal appearance), confirming **ischemic stroke**.
- While the patient is on **rivaroxaban**, the question addresses the **within-window acute management**. In the acute setting (within 1 hour of symptom onset), after ruling out hemorrhage on CT, **aspirin 325 mg** is considered as initial antiplatelet therapy for ischemic stroke.
- **Note:** Current guidelines suggest holding rivaroxaban temporarily and avoiding dual therapy (anticoagulation + antiplatelet) due to bleeding risk. However, aspirin remains the safest acute intervention among the choices provided for confirmed ischemic stroke.
*Tissue plasminogen activator (tPA)*
- **tPA** is the preferred thrombolytic for acute ischemic stroke **within 3-4.5 hours** of symptom onset.
- However, it is **absolutely contraindicated** in patients on **direct oral anticoagulants** (like rivaroxaban) due to **dramatically increased risk of intracranial hemorrhage** (up to 10-fold increase).
- Even with normal PT/INR, patients on DOACs cannot receive tPA safely without reversal agents.
*Heparin*
- **Heparin** provides additional anticoagulation on top of rivaroxaban, which would **significantly increase bleeding risk** (both intracranial and systemic).
- Not indicated in acute ischemic stroke management, especially when patient is already therapeutically anticoagulated.
- May be considered in specific scenarios (e.g., crescendo TIAs, arterial dissection) but not first-line here.
*Metoprolol*
- **Metoprolol** is a beta-blocker used for **rate control in atrial fibrillation** (patient has pulse 144/min - rapid ventricular response).
- While rate control is important, **acute blood pressure lowering in ischemic stroke can worsen cerebral perfusion** and extend the infarct.
- Current guidelines recommend **permissive hypertension** in acute stroke (allow BP up to 220/120 unless giving tPA).
- Rate control can be addressed after acute stroke management is initiated.
*Amiodarone*
- **Amiodarone** is an antiarrhythmic used for rhythm control in atrial fibrillation.
- Does **not treat the acute stroke** and is not indicated for emergency management of stroke.
- Rhythm control is not the priority in the acute stroke setting; the focus is on salvaging brain tissue and preventing further ischemia.
Management of stroke complications US Medical PG Question 3: A 69-year-old male presents to the emergency department for slurred speech and an inability to use his right arm which occurred while he was eating dinner. The patient arrived at the emergency department within one hour. A CT scan was performed of the head and did not reveal any signs of hemorrhage. The patient is given thrombolytics and is then managed on the neurology floor. Three days later, the patient is recovering and is stable. He seems depressed but is doing well with his symptoms gradually improving as compared to his initial presentation. The patient complains of neck pain that has worsened slowly over the past few days for which he is being given ibuprofen. Laboratory values are ordered and return as indicated below:
Serum:
Na+: 130 mEq/L
K+: 3.7 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 7 mg/dL
Glucose: 70 mg/dL
Creatinine: 0.9 mg/dL
Ca2+: 9.7 mg/dL
Urine:
Appearance: dark
Glucose: negative
WBC: 0/hpf
Bacterial: none
Na+: 320 mEq/L/24 hours
His temperature is 99.5°F (37.5°C), pulse is 95/min, blood pressure is 129/70 mmHg, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Demeclocycline
- B. Fluid restriction (Correct Answer)
- C. Oral salt tablets
- D. Continue conservative management
- E. Conivaptan
Management of stroke complications Explanation: ***Fluid restriction***
- The patient presents with **hyponatremia** (Na+ 130 mEq/L) and elevated urine sodium (320 mEq/L/24 hours) in the setting of recent stroke and possible SIADH (**Syndrome of Inappropriate Antidiuretic Hormone secretion**).
- **Fluid restriction** is the initial and most crucial step in managing euvolemic hyponatremia due to SIADH, reducing water intake to allow the kidney to excrete excess water and correct serum sodium.
*Demeclocycline*
- **Demeclocycline** is a tetracycline derivative that inhibits the action of ADH on renal tubules, used in chronic or refractory cases of SIADH.
- It is *not* the first-line treatment for acute, moderate hyponatremia, especially when fluid restriction has not yet been attempted.
*Oral salt tablets*
- **Oral salt tablets** would increase the solute load but would also draw water, potentially worsening hyponatremia if unrestricted fluid intake persists in SIADH.
- This intervention is generally not appropriate for **euvolemic hyponatremia** where the primary issue is excess free water.
*Continue conservative management*
- With a sodium level of 130 mEq/L, this is considered **mild to moderate hyponatremia** and requires active intervention to prevent potential neurological complications.
- Simply continuing conservative management without addressing the underlying **hyponatremia** or its cause would be inadequate and potentially harmful.
*Conivaptan*
- **Conivaptan** is an ADH receptor antagonist that can be used for persistent or significant hyponatremia in SIADH.
- It is typically reserved for more severe or refractory cases of hyponatremia and is usually administered intravenously, making it less suitable as a first-line outpatient management strategy.
Management of stroke complications US Medical PG Question 4: A 72-year-old woman comes to the emergency department 1 hour after the sudden onset of a diffuse, dull, throbbing headache. She also reports blurred vision, nausea, and one episode of vomiting. She has a history of poorly controlled hypertension. A photograph of her fundoscopic examination is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Hemorrhagic lacunar stroke
- B. Transient ischemic attack
- C. Giant cell arteritis
- D. Hypertensive emergency (Correct Answer)
- E. Epidural hematoma
Management of stroke complications Explanation: ***Hypertensive emergency***
- The patient's presentation of a **sudden headache**, along with **blurred vision** and nausea, suggests increased intracranial pressure due to severely elevated blood pressure.
- Poorly controlled hypertension is a significant risk factor, leading to possible **end-organ damage** such as hypertensive retinopathy with papilledema or hypertensive encephalopathy.
- Fundoscopic examination showing **papilledema** confirms elevated intracranial pressure, consistent with malignant hypertension.
*Hemorrhagic lacunar stroke*
- Lacunar strokes are **small subcortical infarcts** caused by occlusion of penetrating arteries and are typically **ischemic, not hemorrhagic**.
- They present with focal neurological deficits (pure motor stroke, pure sensory stroke, ataxic hemiparesis) rather than the **diffuse symptoms** and papilledema seen here.
- While hypertension is a risk factor, lacunar infarcts do not cause increased intracranial pressure or papilledema.
*Transient ischemic attack*
- Characterized by temporary neurological deficits that resolve within 24 hours, typically without severe headaches or sustained symptoms.
- Patients may experience **focal weakness or sensory changes** but would not have papilledema or signs of increased intracranial pressure.
- The persistent nature of this patient's symptoms makes TIA unlikely.
*Giant cell arteritis*
- This condition usually presents with **temporal headaches**, jaw claudication, and potential vision loss from arteritic anterior ischemic optic neuropathy.
- Vision loss in GCA is due to ischemic optic nerve damage, not papilledema from increased intracranial pressure.
- More common in older adults but is associated with systemic symptoms like fever, malaise, and elevated ESR/CRP.
*Epidural hematoma*
- Typically follows head trauma and presents with a **lucid interval**, followed by rapid deterioration from expanding hematoma.
- Usually caused by middle meningeal artery injury with classic lens-shaped hematoma on CT.
- The lack of trauma history and the chronic hypertension make this diagnosis unlikely.
Management of stroke complications US Medical PG Question 5: A 77-year-old woman is brought by ambulance to the emergency department after she developed weakness of her right arm along with a right-sided facial droop. By the time the ambulance arrived, she was having difficulty speaking. Past medical history is significant for hypertension, diabetes mellitus type II, and hyperlipidemia. She takes lisinopril, hydrochlorothiazide, metformin, and atorvastatin. On arrival to the emergency department, her vital signs are within normal limits. On physical examination, she is awake and alert but the right side of her mouth is dropping, making it difficult for her to speak clearly. Her heart has a regular rate and rhythm and her lungs are clear to auscultation bilaterally. Fingerstick glucose is 85 mg/dL. Her right upper extremity strength is 2/5 and her left upper extremity strength is 5/5. Which of the following is the best next step in management?
- A. Obtain transcranial doppler
- B. Start tissue plasminogen activator (tPA)
- C. Consult cardiology
- D. Intubate the patient
- E. Obtain noncontrast CT of the brain (Correct Answer)
Management of stroke complications Explanation: ***Obtain noncontrast CT of the brain***
- An **urgent noncontrast CT of the brain** is the **most crucial initial step** in managing acute neurological deficits suggestive of stroke.
- This imaging is essential to **rule out hemorrhagic stroke** before considering thrombolytic therapy like tPA.
*Obtain transcranial doppler*
- **Transcranial Doppler (TCD)** can be used to assess cerebral blood flow and identify vascular stenosis but is not the immediate first-line diagnostic imaging for an acute stroke presentation.
- TCD is typically performed **after initial imaging** to determine the presence of large vessel occlusion or monitor for vasospasm, not to differentiate between ischemic and hemorrhagic stroke.
*Start tissue plasminogen activator (tPA)*
- While **tPA** is a treatment for acute ischemic stroke, it is **contraindicated in hemorrhagic stroke**.
- Without a **noncontrast CT scan to rule out hemorrhage**, administering tPA can be life-threatening.
*Consult cardiology*
- Consulting cardiology is important for evaluating potential cardiac sources of emboli (e.g., atrial fibrillation) as a cause of stroke but it is **not the immediate next step** in managing acute stroke symptoms.
- The **immediate priority is diagnosing the type of stroke** and determining eligibility for acute interventions.
*Intubate the patient*
- **Intubation** is reserved for patients with compromise of their **airway, breathing, or circulation (ABCs)**, or a significantly decreased level of consciousness (e.g., GCS < 8).
- This patient is described as **awake and alert**, making intubation unnecessary at this stage.
Management of stroke complications US Medical PG Question 6: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
Management of stroke complications Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
Management of stroke complications US Medical PG Question 7: A 77-year-old man is brought to the emergency department by his wife because of headache, nausea, and vomiting for 24 hours. His wife says that over the past 2 weeks, he has been more irritable and has had trouble remembering to do routine errands. Two weeks ago, he fell during a skiing accident but did not lose consciousness. He has coronary artery disease and hypertension. He has smoked one pack of cigarettes daily for 50 years. He has had 2 glasses of wine daily since his retirement 10 years ago. Current medications include atenolol, enalapril, furosemide, atorvastatin, and aspirin. He appears acutely ill. He is oriented to person but not to place or time. His temperature is 37°C (98.6°F), pulse is 99/min, respirations are 16/min, and blood pressure is 160/90 mm Hg. During the examination, he is uncooperative and unable to answer questions. Deep tendon reflexes are 4+ on the left and 2+ on the right. Babinski's sign is present on the left. There is mild weakness of the left iliopsoas and hamstring muscles. A CT scan of the head without contrast shows a high-density, 15-mm crescentic collection across the right hemispheric convexity. Which of the following is the most appropriate next step in the management of this patient?
- A. Recombinant tissue plasminogen activator administration
- B. Obtain an Electroencephalography
- C. Obtain an MRI of the head
- D. Surgical evacuation (Correct Answer)
- E. Observation
Management of stroke complications Explanation: ***Surgical evacuation***
- The CT scan reveals a **high-density, crescentic collection**, strongly indicative of an **acute subdural hematoma**, which is causing significant neurological deficits and mass effect (e.g., increased intracranial pressure symptoms like headache, nausea, vomiting, and altered mental status, and focal neurological signs).
- Given the patient's **acute neurological decline**, significant mass effect from the 15-mm hematoma, and age, prompt **surgical evacuation** is the definitive treatment to relieve pressure and prevent further brain injury.
*Recombinant tissue plasminogen activator administration*
- **tPA** is indicated for **acute ischemic stroke**, not hemorrhagic stroke or subdural hematoma. Administering tPA in this context would be harmful, potentially worsening the hemorrhage.
- The patient's CT scan clearly shows a **hemorrhagic lesion**, not an ischemic event.
*Obtain an Electroencephalography*
- **EEG** is primarily used to evaluate **seizure disorders** or certain types of encephalopathy. While the patient has altered mental status, the primary issue identified on CT is a subdural hematoma requiring immediate intervention.
- EEG would not provide information relevant to the immediate management of an **acute subdural hematoma**.
*Obtain an MRI of the head*
- An **MRI** can provide more detailed imaging, but in the context of an **acute subdural hematoma** with significant neurological compromise, it would delay crucial and time-sensitive surgical intervention.
- The **CT scan** has already provided sufficient diagnostic information to warrant immediate surgical planning.
*Observation*
- **Observation** is not appropriate for a patient with a rapidly expanding **acute subdural hematoma** causing significant neurological deficits and a 15-mm collection, especially given the patient's age and clinical presentation.
- Delaying treatment would likely lead to further neurological deterioration, **herniation**, and potentially death.
Management of stroke complications US Medical PG Question 8: An 8-month-old boy is brought to the emergency department by his mother. She is concerned that her son has had intermittent periods of severe abdominal pain over the past several days that has been associated with emesis and "currant jelly" stool. Of note, the family lives in a rural part of the state, requiring a 2 hour drive to the nearest hospital. He currently appears to be in significant pain and has vomited twice in the past hour. On physical examination, a sausage-shaped mass is noted on palpation of the right upper quadrant of the abdomen. Ultrasound of the abdomen was consistent with a diagnosis of intussusception. An air-contrast barium enema was performed, which confirmed the diagnosis and also successfully reduced the intussusception. Which of the following is the next best step in the management of this patient?
- A. Keep patient NPO and initiate work-up to identify lead-point
- B. Admit to hospital for 24 hour observation for complications and/or recurrence (Correct Answer)
- C. Pursue urgent surgical reduction with resection of necrotic segments of bowel
- D. Repeat barium enema q6 hrs to monitor for recurrence
- E. Discharge to home with follow-up in 3 weeks in an outpatient pediatric gastroenterology clinic
Management of stroke complications Explanation: ***Admit to hospital for 24 hour observation for complications and/or recurrence***
- Following successful non-operative reduction of intussusception, there is a risk of **recurrence** (approximately 5-10%) and potential for **perforation** or other delayed complications, necessitating close hospital observation.
- The patient's presentation with significant pain and vomiting, coupled with the long travel time to the hospital, further supports the need for **hospital admission** to monitor for stability and potential early recurrence.
*Keep patient NPO and initiate work-up to identify lead-point*
- While keeping the patient NPO (nil per os) might be appropriate initially, a work-up for a **lead point** is generally performed if there are multiple recurrences or in older children, as most intussusceptions in infants are idiopathic.
- Doing this immediately without observation can delay identification of recurrence and prompt intervention.
*Pursue urgent surgical reduction with resection of necrotic segments of bowel*
- Surgical reduction is indicated if **non-operative reduction fails**, if there are signs of **perforation**, diffuse peritonitis, or if there is clinical evidence of **bowel necrosis**.
- Since the intussusception was successfully reduced by air-contrast enema and there are no signs of perforation or necrosis currently, urgent surgery is not the immediate next step.
*Repeat barium enema q6 hrs to monitor for recurrence*
- Repeated enemas carry risks such as **radiation exposure** and potential for perforation, and are not a standard monitoring strategy for recurrence.
- Clinical observation and physical examination are generally sufficient for monitoring during the initial 24-hour period.
*Discharge to home with follow-up in 3 weeks in an outpatient pediatric gastroenterology clinic*
- Discharging the patient home so soon after reduction is unsafe due to the significant risk of **early recurrence** (especially within the first 24-48 hours) or development of complications.
- A follow-up in 3 weeks is too delayed for immediate post-reduction concerns.
Management of stroke complications US Medical PG Question 9: A researcher is studying the brains of patients who recently died from stroke-related causes. One specimen has a large thrombus in an area of the brain that is important in relaying many modalities of sensory information from the periphery to the sensory cortex. Which of the following embryologic structures gave rise to the part of the brain in question?
- A. Metencephalon
- B. Diencephalon (Correct Answer)
- C. Mesencephalon
- D. Telencephalon
- E. Myelencephalon
Management of stroke complications Explanation: ***Diencephalon***
- The **thalamus**, a key relay center for sensory information to the cerebral cortex, develops from the diencephalon.
- A thrombus in this area would severely impair the transmission of **sensory modalities** from the periphery.
*Metencephalon*
- The metencephalon gives rise to the **pons** and the **cerebellum**.
- These structures are primarily involved in motor control, coordination, and respiratory regulation, not direct sensory relay to the cortex.
*Mesencephalon*
- The mesencephalon develops into the **midbrain**.
- The midbrain contains structures involved in visual and auditory reflexes, and motor control, but not the primary sensory relay described.
*Myelencephalon*
- The myelencephalon gives rise to the **medulla oblongata**.
- The medulla is crucial for vital autonomic functions (e.g., breathing, heart rate) and connects the brain to the spinal cord.
*Telencephalon*
- The telencephalon develops into the **cerebral hemispheres** (cerebral cortex, basal ganglia, hippocampus).
- While it processes sensory information, it is not the primary relay center from the periphery; that role belongs to the thalamus.
Management of stroke complications US Medical PG Question 10: A female presents with a 1 × 1 cm thyroid swelling. What is the next best step in management?
- A. I-131
- B. TSH (Correct Answer)
- C. TSH & T4
- D. T3 & T4
- E. FNAC
Management of stroke complications Explanation: ***Correct Option: TSH***
- **Thyroid-stimulating hormone (TSH)** is the most sensitive initial test to assess thyroid function when a thyroid nodule is discovered.
- An abnormal TSH level (either high or low) can guide further investigation into whether the nodule is associated with a functional thyroid disorder.
- **TSH should be the first test** according to American Thyroid Association guidelines for thyroid nodule evaluation.
*Incorrect Option: I-131*
- **I-131 (radioactive iodine therapy)** is a treatment modality for hyperthyroidism or thyroid cancer, not a diagnostic step for initial thyroid swelling evaluation.
- Administering I-131 before assessing thyroid function would be inappropriate and could lead to unnecessary or harmful intervention.
*Incorrect Option: TSH & T4*
- While TSH is crucial, adding **T4 (thyroxine)** as an initial step is often not necessary if TSH is normal, as TSH alone effectively screens for primary thyroid dysfunction.
- Measuring both TSH and T4 is typically reserved for situations where TSH is abnormal or when central hypothyroidism is suspected.
*Incorrect Option: T3 & T4*
- Measuring **T3 (triiodothyronine)** along with T4 as an initial screening for a thyroid nodule is generally not recommended.
- T3 levels are primarily used to diagnose **hyperthyroidism** or to evaluate the severity of thyrotoxicosis after an abnormal TSH and T4 have been identified.
*Incorrect Option: FNAC*
- While **Fine Needle Aspiration Cytology (FNAC)** is an essential diagnostic tool for thyroid nodules, it is typically performed after TSH assessment.
- FNAC is indicated for nodules >1 cm with suspicious ultrasound features, but **functional assessment with TSH comes first** to rule out hyperfunctioning nodules.
More Management of stroke complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.