Ischemic vs hemorrhagic stroke differentiation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ischemic vs hemorrhagic stroke differentiation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 1: A 48-year-old man presents to the ER with a sudden-onset, severe headache. He is vomiting and appears confused. His wife, who accompanied him, says that he has not had any trauma, and that the patient has no relevant family history. He undergoes a non-contrast head CT that shows blood between the arachnoid and pia mater. What is the most likely complication from this condition?
- A. Hemorrhagic shock
- B. Arterial Vasospasm (Correct Answer)
- C. Renal failure
- D. Bacterial Meningitis
- E. Blindness
Ischemic vs hemorrhagic stroke differentiation Explanation: **Arterial Vasospasm**
- **Arterial vasospasm** is a major delayed complication of **subarachnoid hemorrhage (SAH)**, typically occurring 3-14 days after the initial bleed.
- The presence of blood products in the subarachnoid space can irritate cerebral arteries, leading to their narrowing and subsequent **delayed cerebral ischemia** or infarction.
*Hemorrhagic shock*
- **Subarachnoid hemorrhage (SAH)** typically involves bleeding within the confines of the skull, which is usually not extensive enough to cause systemic **hypovolemia** or **hemorrhagic shock**.
- **Hemorrhagic shock** would require significant external blood loss or internal bleeding into a large body cavity, which is not characteristic of an isolated SAH.
*Renal failure*
- **Renal failure** is not a direct or common complication of **subarachnoid hemorrhage (SAH)**.
- While systemic complications can sometimes arise in critically ill patients, there is no direct pathophysiological link between SAH and primary kidney injury.
*Bacterial Meningitis*
- The presence of blood in the **subarachnoid space** can cause a **chemical meningitis** due to irritation, mimicking some symptoms of bacterial meningitis.
- However, it does not typically predispose to **bacterial infection** unless there's an iatrogenic cause (e.g., lumbar puncture contamination).
*Blindness*
- While damage to the **optic nerves** or visual pathways can occur with severe neurological events or increased intracranial pressure, **blindness** is not a common or direct complication specifically arising from the bleed itself or its immediate sequelae in SAH.
- Visual disturbances are possible due to elevated **intracranial pressure** or specific anatomical lesion, but not primary blindness.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 2: A 69-year-old man is brought in by his wife with acute onset aphasia for the past 5 hours. The patient's wife says that they were sitting having dinner when suddenly he was not able to speak. They delayed coming to the hospital because he had a similar episode 2 months ago which resolved within an hour. His past medical history is significant for hypercholesterolemia, managed with rosuvastatin, and a myocardial infarction (MI) 2 months ago, status post percutaneous transluminal coronary angioplasty complicated by residual angina. His family history is significant for his father who died of MI at age 60. The patient reports a 15-pack-year smoking history but denies any alcohol or recreational drug use. The vital signs include: temperature 37.0℃ (98.6℉), blood pressure 125/85 mm Hg, pulse 96/min, and respiratory rate 19/min. On physical examination, the patient has expressive aphasia. There is a weakness of the right-sided lower facial muscles. The strength in his upper and lower extremities is 4/5 on the right and 5/5 on the left. There is also a decreased sensation on his right side. A noncontrast computed tomography (CT) scan of the head is unremarkable. CT angiography (CTA) and diffusion-weighted magnetic resonance imaging (MRI) of the brain are acquired, and the findings are shown in the exhibit (see image). Which of the following is the best course of treatment in this patient?
- A. Aspirin
- B. Mannitol
- C. Mechanical thrombectomy (Correct Answer)
- D. IV tPA
- E. Low molecular weight heparin
Ischemic vs hemorrhagic stroke differentiation Explanation: ***Mechanical thrombectomy***
- The patient presents with **acute ischemic stroke** symptoms (aphasia, right-sided weakness, sensory deficits) at **5 hours from symptom onset**. Imaging (CTA showing large vessel occlusion and MRI confirming diffusion restriction) demonstrates a **large vessel occlusion**, making him a candidate for **mechanical thrombectomy**.
- Since the patient is **beyond the 4.5-hour window for IV tPA**, mechanical thrombectomy is the **primary reperfusion therapy** indicated for large vessel occlusion strokes up to **24 hours** (with appropriate imaging showing salvageable tissue).
- Mechanical thrombectomy offers the best chance for complete recanalization and improved neurological outcomes in large vessel occlusion strokes, particularly when IV tPA is not an option.
*Aspirin*
- While **aspirin** is crucial for **secondary stroke prevention**, it is not the primary acute treatment for a large vessel occlusion stroke due to its limited ability to achieve rapid and complete recanalization.
- Aspirin (or other antiplatelet therapy) is typically initiated **within 24-48 hours after stroke onset**, but only after excluding hemorrhagic transformation and after acute reperfusion therapies have been considered or completed.
*Mannitol*
- **Mannitol** is an osmotic diuretic used to reduce **intracranial pressure (ICP)** in cases of severe cerebral edema, which can be a complication of large ischemic strokes.
- It is not a primary treatment for the acute ischemic event itself, but rather a supportive measure used to manage life-threatening complications if **cerebral edema** develops and causes significant mass effect or herniation risk.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is the first-line pharmacologic treatment for acute ischemic stroke if administered **within 4.5 hours of symptom onset** in eligible patients.
- This patient presents at **5 hours**, which is **beyond the approved time window** for IV tPA administration, making him **ineligible** for thrombolytic therapy.
- Even if within the time window, patients with large vessel occlusion often require mechanical thrombectomy in addition to or instead of IV tPA for optimal outcomes.
*Low molecular weight heparin*
- **Low molecular weight heparin (LMWH)** is primarily used for **deep vein thrombosis (DVT)** prophylaxis in immobilized patients or for the treatment of established DVT/pulmonary embolism.
- It is generally **not recommended for acute ischemic stroke treatment** due to an increased risk of hemorrhagic transformation without proven benefit in recanalization or clinical outcomes.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 3: A 60-year-old male is admitted to the ICU for severe hypertension complicated by a headache. The patient has a past medical history of insulin-controlled diabetes, hypertension, and hyperlipidemia. He smokes 2 packs of cigarettes per day. He states that he forgot to take his medications yesterday and started getting a headache about one hour ago. His vitals on admission are the following: blood pressure of 160/110 mmHg, pulse 95/min, temperature 98.6 deg F (37.2 deg C), and respirations 20/min. On exam, the patient has an audible abdominal bruit. After administration of antihypertensive medications, the patient has a blood pressure of 178/120 mmHg. The patient reports his headache has increased to a 10/10 pain level, that he has trouble seeing, and he can't move his extremities. After stabilizing the patient, what is the best next step to diagnose the patient's condition?
- A. Doppler ultrasound of the carotids
- B. CT head with intravenous contrast
- C. MRI head without intravenous contrast
- D. CT head without intravenous contrast (Correct Answer)
- E. MRI head with intravenous contrast
Ischemic vs hemorrhagic stroke differentiation Explanation: ***CT head without intravenous contrast***
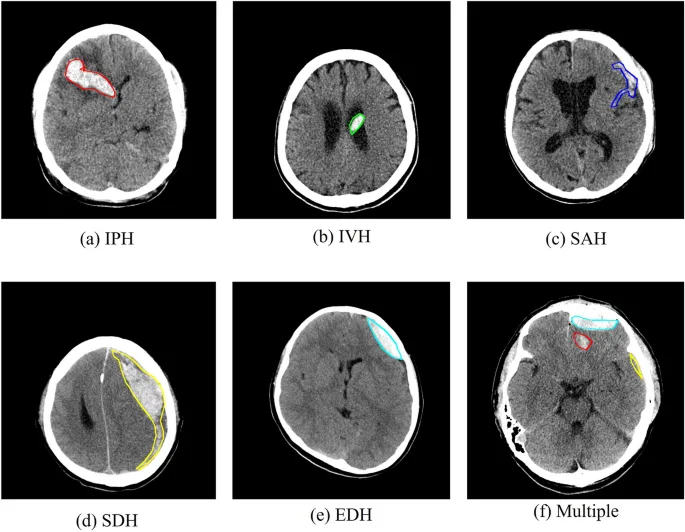
- The sudden onset of severe headache, visual disturbances, and neurological deficits (inability to move extremities), coupled with uncontrolled severe hypertension despite initial treatment, is highly suggestive of an **intracranial pathology**, most likely a **hemorrhagic stroke**.
- A **non-contrast CT scan of the head** is the **gold standard** for rapidly identifying acute intracranial hemorrhage, as it can be performed quickly and is readily available in emergency settings.
*Doppler ultrasound of the carotids*
- This test is primarily used to evaluate **carotid artery stenosis** due to atherosclerosis, which can lead to ischemic stroke.
- While the patient has risk factors for atherosclerosis, his acute presentation with severe central neurological symptoms points more towards an acute intracranial event rather than carotid disease.
*CT head with intravenous contrast*
- While a contrast CT can be useful for identifying tumors, abscesses, or vascular malformations, it is **contraindicated in the initial assessment of acute stroke** if an intracranial hemorrhage is suspected.
- Contrast can sometimes obscure subtle bleeds or complicate the interpretation of acute hemorrhage, and it also carries a risk of **contrast-induced nephropathy**, especially in a patient with diabetes.
*MRI head without intravenous contrast*
- An MRI provides superior soft tissue resolution compared to CT and is excellent for detecting ischemic strokes in later stages, as well as subtle hemorrhages, tumors, and other conditions.
- However, it is **less available, takes longer to perform**, and is often not the first choice in an acute neurological emergency where time is critical, particularly when differentiating between ischemic and hemorrhagic stroke.
*MRI head with intravenous contrast*
- Similar to a contrast CT, an MRI with contrast is generally **not the initial imaging choice for acute stroke** due to time constraints and the need to quickly rule out hemorrhage before considering contrast administration.
- Contrast agents for MRI, such as gadolinium, have their own risks, including **nephrogenic systemic fibrosis** in patients with renal impairment, which is a concern in a diabetic patient.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 4: A 53-year-old man is brought to the emergency department for confusion. He was in his usual state of health until about 3 hours ago when he tried to use his sandwich to turn off the TV. He also complained to his wife that he had a severe headache. Past medical history is notable for hypertension, which has been difficult to control on multiple medications. His temperature is 36.7°C (98°F), the pulse is 70/min, and the blood pressure is 206/132 mm Hg. On physical exam he is alert and oriented only to himself, repeating over and over that his head hurts. The physical exam is otherwise unremarkable and his neurologic exam is nonfocal. The noncontrast CT scan of the patient's head is shown and reveals an acute intraparenchymal hemorrhage in the basal ganglia. Which of the following diagnostic tests would be most helpful in determining the underlying cause of this patient's hemorrhage?
- A. Lumbar puncture
- B. Electroencephalogram (EEG)
- C. MRI of the brain
- D. CT angiography of the neck
- E. CT angiography of the brain (Correct Answer)
Ischemic vs hemorrhagic stroke differentiation Explanation: ***CT angiography of the brain***
- Following identification of an **intracerebral hemorrhage** on noncontrast CT, **CT angiography (CTA) of the brain** is the most appropriate next diagnostic test to identify underlying vascular abnormalities such as **arteriovenous malformations (AVMs)**, **aneurysms**, **dural arteriovenous fistulas**, or **moyamoya disease**.
- While this patient has severe hypertension (a common cause of basal ganglia hemorrhage), CTA should still be performed to rule out secondary causes, particularly in patients under 70 years old or those with atypical features.
- CTA can be performed rapidly in the acute setting and has high sensitivity for detecting vascular lesions that may require specific treatment.
*MRI of the brain*
- MRI with specialized sequences (GRE, SWI, FLAIR) can provide detailed information about **chronic microhemorrhages**, **cerebral amyloid angiopathy**, **underlying tumors**, or **cavernomas**.
- However, MRI is typically performed **after CTA** in the workup of intracerebral hemorrhage, not as the immediate next step.
- MRI is less readily available in the acute setting and takes longer to perform than CTA.
*CT angiography of the neck*
- This test visualizes the **carotid and vertebral arteries** in the neck to detect **stenosis**, **dissection**, or **atherosclerotic disease**.
- It is not directly useful for identifying the cause of an **intraparenchymal hemorrhage** within the brain substance itself.
*Lumbar puncture*
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** and is primarily used for suspected **subarachnoid hemorrhage** (when CT is negative), **meningitis**, or **encephalitis**.
- It is **contraindicated** in patients with significant intraparenchymal hemorrhage due to risk of herniation from increased intracranial pressure.
*Electroencephalogram (EEG)*
- EEG measures **electrical activity in the brain** and is used to diagnose **seizure disorders** or evaluate altered mental status from metabolic or epileptic causes.
- While confusion can result from seizures, the primary pathology is the **intracerebral hemorrhage** identified on CT, which EEG cannot diagnose or characterize.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 5: A 73-year-old man is brought to the emergency department by ambulance after being found to be non-communicative by his family during dinner. On presentation he appears to be alert, though he is confused and cannot follow instructions. When he tries to speak, he vocalizes a string of fluent but unintelligible syllables. Given this presentation, his physician decides to administer tissue plasminogen activator to this patient. This intervention best represents which of the following principles?
- A. Tertiary prevention
- B. Primary prevention
- C. This does not represent prevention (Correct Answer)
- D. Quaternary prevention
- E. Secondary prevention
Ischemic vs hemorrhagic stroke differentiation Explanation: ***This does not represent prevention***
- The administration of **tissue plasminogen activator (tPA)** during an **acute stroke** is a **therapeutic intervention**, not a form of prevention.
- **Prevention** refers to actions taken to prevent disease occurrence, detect it early, or prevent complications after recovery. Treating an acute, symptomatic event is **acute treatment**, not prevention.
- This is an active medical intervention to treat an ongoing, symptomatic disease process (acute ischemic stroke), which falls under **therapeutic management** rather than any category of prevention.
*Secondary prevention*
- **Secondary prevention** involves **early detection** and treatment of asymptomatic or minimally symptomatic disease to prevent progression (e.g., screening mammography, colonoscopy).
- For stroke specifically, secondary prevention would include interventions **after** the acute event to **prevent recurrence**, such as starting antiplatelet therapy (aspirin, clopidogrel), anticoagulation for atrial fibrillation, statin therapy, or carotid endarterectomy after TIA.
- tPA is given during the acute symptomatic phase, making it treatment rather than secondary prevention.
*Tertiary prevention*
- **Tertiary prevention** focuses on **rehabilitation** and managing established disease to prevent complications and improve quality of life.
- Examples after stroke include physical therapy, occupational therapy, speech therapy, and managing post-stroke complications like depression or spasticity.
- This occurs in the recovery phase, not during acute treatment.
*Primary prevention*
- **Primary prevention** aims to prevent disease before it occurs in healthy individuals.
- Examples include controlling hypertension, managing diabetes, smoking cessation, exercise, and healthy diet - all interventions that reduce stroke risk **before** any event occurs.
*Quaternary prevention*
- **Quaternary prevention** protects patients from **overmedicalization** and excessive or harmful medical interventions.
- It involves avoiding unnecessary testing or treatment that may cause more harm than benefit.
- Administering tPA for acute stroke (when indicated) is evidence-based treatment, not overtreatment.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 6: A 75-year-old woman presents with sudden loss of vision. She says that she was reading when suddenly she was not able to see the print on half of the page. Her symptoms started 4 hours ago and are accompanied by a severe posterior headache. Vital signs reveal the following: blood pressure 119/76 mm Hg, pulse 89/min, SpO2 98% on room air. The patient was unable to recognize her niece when she arrived to see her. A noncontrast CT of the head shows no evidence of hemorrhagic stroke. What is the most likely diagnosis in this patient?
- A. Lacunar stroke
- B. Middle cerebral artery stroke
- C. Vertebrobasilar stroke
- D. Subarachnoid hemorrhage
- E. Posterior cerebral artery stroke (Correct Answer)
Ischemic vs hemorrhagic stroke differentiation Explanation: ***Posterior cerebral artery stroke***
- The sudden severe posterior headache along with **unilateral vision loss** and **prosopagnosia** (inability to recognize familiar faces) are characteristic signs of a **posterior cerebral artery (PCA) stroke**.
- PCA occlusion often affects the **occipital lobe** (vision) and can extend to the **temporal lobe** (facial recognition).
*Lacunar stroke*
- This type of stroke results from the occlusion of small penetrating arteries and typically causes **pure motor** or **pure sensory deficits**, not complex visual or recognition problems.
- While headache can occur, the specific combination of symptoms points away from a lacunar infarct.
*Middle cerebral artery stroke*
- MCA stroke commonly presents with **contralateral hemiparesis**, **aphasia** (if dominant hemisphere), and **hemianopia** but usually not isolated unilateral vision loss or severe posterior headache with prosopagnosia.
- The symptoms are more consistent with involvement of the posterior circulation.
*Vertebrobasilar stroke*
- A vertebrobasilar stroke can cause **visual disturbances**, but it is typically associated with other **brainstem symptoms** like vertigo, ataxia, or cranial nerve deficits, which are not described here.
- The specific presentation of unilateral vision loss and prosopagnosia is less typical for a vertebrobasilar stroke affecting widespread brainstem structures.
*Subarachnoid hemorrhage*
- While a **sudden severe headache (thunderclap headache)** is a hallmark of SAH, it usually presents with meningeal irritation symptoms like **neck stiffness** and often altered mental status, and the visual deficits are usually different (e.g., oculomotor nerve palsy).
- The patient's focal neurological deficits, specifically prosopagnosia and unilateral visual field loss, are more indicative of an ischemic event in a specific vascular territory.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 7: A 72-year-old man is brought into clinic by his daughter for increasing confusion. The daughter states that over the past 2 weeks, she has noticed that the patient “seems to stare off into space.” She reports he has multiple episodes a day during which he will walk into a room and forget why. She is also worried about his balance. She endorses that he has had several falls, the worst being 3 weeks ago when he tripped on the sidewalk getting the mail. The patient denies loss of consciousness, pre-syncope, chest pain, palpitations, urinary incontinence, or bowel incontinence. He complains of headache but denies dizziness. He reports nausea and a few episodes of non-bloody emesis but denies abdominal pain, constipation, or diarrhea. The patient’s medical history is significant for atrial fibrillation, diabetes, hypertension, hyperlipidemia, and osteoarthritis. He takes aspirin, warfarin, insulin, lisinopril, simvastatin, and ibuprofen. He drinks a half glass of whisky after dinner every night and smokes a cigar on the weekends. On physical examination, he is oriented to name and place but not to date. He is unable to spell "world" backward. When asked to remember 3 words, he recalls only 2. There are no motor or sensory deficits. Which of the following is the most likely diagnosis?
- A. Ischemic stroke
- B. Subdural hematoma (Correct Answer)
- C. Vitamin B12 deficiency
- D. Alzheimer disease
- E. Normal pressure hydrocephalus
Ischemic vs hemorrhagic stroke differentiation Explanation: ***Subdural hematoma***
- The patient's presentation with **gradual onset of confusion**, increasing forgetfulness, and **balance issues with falls** over a couple of weeks, especially after a fall three weeks prior, is highly suggestive of a subdural hematoma.
- His use of **warfarin** and **aspirin** significantly increases his risk for bleeding, and the **headache and nausea/vomiting** are common symptoms of increased intracranial pressure.
*Ischemic stroke*
- An ischemic stroke typically presents with **acute, focal neurological deficits**, which are not described here.
- While the patient has risk factors for stroke (atrial fibrillation, hypertension, diabetes), the **gradual onset** of symptoms over weeks makes it less likely.
*Vitamin B12 deficiency*
- Vitamin B12 deficiency can cause **cognitive impairment** and neurological symptoms, but it usually develops **insidiously over months to years**, not acutely over 2 weeks.
- It is also associated with **peripheral neuropathy and megaloblastic anemia**, which are not reported.
*Alzheimer disease*
- Alzheimer's disease causes **progressive cognitive decline** over many years, starting with memory issues that gradually worsen.
- The **relatively rapid 2-week progression** of symptoms and the clear precipitating factor of a fall make Alzheimer's less likely in this acute context.
*Normal pressure hydrocephalus*
- Normal pressure hydrocephalus (NPH) classically presents with a triad of **gait disturbance, urinary incontinence, and dementia**.
- While the patient has gait issues and cognitive changes, the **absence of urinary incontinence** and the relatively rapid onset after a fall makes NPH less probable.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 8: A 48-year-old woman presents with acute stroke symptoms 18 hours ago. MRI shows a right MCA M1 occlusion with large penumbra on perfusion imaging (mismatch ratio >1.8) and small infarct core (25 mL). Her NIHSS is 16. She has no significant comorbidities. Her family is concerned about disability but wants to pursue treatment if reasonable chance of benefit exists. Synthesize the evidence and evaluate the treatment approach.
- A. Intravenous alteplase as salvageable tissue is present
- B. Intra-arterial thrombolysis combined with mechanical device
- C. No intervention as she is outside the standard treatment window
- D. Mechanical thrombectomy based on perfusion imaging criteria (Correct Answer)
- E. Medical management with antiplatelet and early rehabilitation
Ischemic vs hemorrhagic stroke differentiation Explanation: ***Mechanical thrombectomy based on perfusion imaging criteria***
- For patients with large vessel occlusion (LVO) in the extended 6–24 hour window, **DAWN** and **DEFUSE-3** trials demonstrated significant functional benefit when clinical-core mismatch is present.
- This patient satisfies criteria with an **M1 occlusion**, a **small infarct core (<70 mL)**, and a **large mismatch ratio (>1.8)**, indicating substantial salvageable penumbra.
*Intravenous alteplase as salvageable tissue is present*
- The therapeutic window for **IV alteplase** is strictly limited to within **4.5 hours** of symptom onset; it is not recommended at 18 hours due to high hemorrhage risk.
- While salvageable tissue exists, chemical thrombolysis is less effective than mechanical intervention for **proximal M1 occlusions** and is unsafe in this late window.
*Intra-arterial thrombolysis combined with mechanical device*
- **Intra-arterial thrombolysis** is generally superseded by modern **stent retrievers** and aspiration catheters which provide faster and more complete recanalization.
- Current guidelines prioritize standalone **mechanical thrombectomy** in the late window to minimize procedural risks and intracranial hemorrhage.
*No intervention as she is outside the standard treatment window*
- The "Time is Brain" concept has evolved into "Tissue is Brain," where **perfusion imaging** identifies candidates who benefit regardless of the traditional 6-hour clock.
- Denying treatment based solely on the 18-hour timeframe ignores high-level evidence from the **DAWN** trial showing benefit up to 24 hours.
*Medical management with antiplatelet and early rehabilitation*
- Standard **medical management** (aspirin/heparin) for an M1 occlusion with a high **NIHSS score (16)** usually results in poor functional outcomes and severe disability.
- While rehabilitation is essential, it does not address the underlying **large vessel occlusion** which can be reversed with mechanical intervention to prevent infarct expansion.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 9: A 55-year-old man undergoes successful thrombectomy for left MCA occlusion. Post-procedure, he develops progressive lethargy and his blood pressure increases to 180/100 mmHg. CT shows hyperdensity in the treated territory without hemorrhage, and his symptoms worsen over 4 hours despite blood pressure control. Evaluate the most likely diagnosis and management priority.
- A. Hemorrhagic transformation; reverse anticoagulation immediately
- B. Cerebral edema from large infarction; emergent decompressive hemicraniectomy
- C. Reperfusion injury; start high-dose corticosteroids and osmotic therapy
- D. Contrast extravasation from blood-brain barrier disruption; supportive care and avoid aggressive BP lowering (Correct Answer)
- E. Recurrent arterial occlusion; emergent repeat angiography and thrombectomy
Ischemic vs hemorrhagic stroke differentiation Explanation: ***Contrast extravasation from blood-brain barrier disruption; supportive care and avoid aggressive BP lowering***
- Post-thrombectomy **hyperdensity** on CT often represents contrast that leaked through an ischemic **blood-brain barrier**, which can mimic hemorrhage but lacks significant **mass effect**.
- Management is **supportive care** because the contrast is typically reabsorbed within 24–48 hours; avoiding aggressive **blood pressure lowering** prevents secondary ischemia in the penumbra.
*Hemorrhagic transformation; reverse anticoagulation immediately*
- While **hemorrhagic transformation** is a risk, true blood usually demonstrates higher density earlier and is associated with rapid clinical decline and **midline shift**.
- Reversing anticoagulation without confirming blood on a follow-up **dual-energy CT** or MRI may lead to **stent thrombosis** or re-occlusion.
*Cerebral edema from large infarction; emergent decompressive hemicraniectomy*
- **Cerebral edema** typically peaks between 72–96 hours post-stroke; a presentation within 4 hours is too acute for **malignant MCA syndrome**.
- While edema causes lethargy, the hyperdensity on CT more specifically points toward **contrast staining** or blood rather than simple cytotoxic edema.
*Reperfusion injury; start high-dose corticosteroids and osmotic therapy*
- **Corticosteroids** are not indicated for stroke-related edema or reperfusion injury as they do not improve outcomes and may increase **infection risk**.
- **Osmotic therapy** is reserved for patients with clear clinical or radiologic signs of **elevated intracranial pressure**, not isolated hyperdensity on CT.
*Recurrent arterial occlusion; emergent repeat angiography and thrombectomy*
- **Recurrent occlusion** usually presents with a sudden recurrence of the original **focal neurological deficits** (e.g., hemiplegia, aphasia) rather than progressive lethargy.
- The presence of **hyperdensity** in the stroke territory on CT is specifically indicative of material (contrast or blood) being present, which is not a feature of a simple **re-occlusion**.
Ischemic vs hemorrhagic stroke differentiation US Medical PG Question 10: An 80-year-old woman with atrial fibrillation presents 2 hours after acute ischemic stroke. NIHSS is 22. Imaging shows large left MCA territory infarction involving >1/3 of MCA territory with basilar artery occlusion. She lives alone but was independent before this event. Her family requests all possible interventions. Evaluate the management approach considering benefits versus risks.
- A. Comfort measures only given poor prognosis and age
- B. Thrombolysis alone as thrombectomy unlikely to benefit with established large infarction
- C. Proceed with thrombolysis and thrombectomy given the therapeutic window
- D. Thrombectomy only for basilar occlusion, avoid thrombolysis due to large infarction (Correct Answer)
- E. Delay intervention and repeat imaging in 6 hours to assess progression
Ischemic vs hemorrhagic stroke differentiation Explanation: ***Thrombectomy only for basilar occlusion, avoid thrombolysis due to large infarction***
- Intravenous **thrombolysis (IV alteplase)** is generally contraindicated or highly risky when imaging shows an established infarction involving **>1/3 of the MCA territory** due to the high risk of **hemorrhagic transformation**.
- **Basilar artery occlusion** is a life-threatening emergency with a broader treatment window; mechanical **thrombectomy** can be lifesaving and is indicated even if thrombolysis is withheld.
*Comfort measures only given poor prognosis and age*
- Age is not a primary contraindication for intervention, especially since the patient was **independent** prior to the event (low **pre-stroke mRS**).
- Family requests all possible interventions, and **basilar occlusion** has a catastrophic natural history that may be mitigated by mechanical intervention.
*Thrombolysis alone as thrombectomy unlikely to benefit with established large infarction*
- Thrombolysis is dangerous in this context due to the **large infarct volume** seen on imaging, which increases the likelihood of fatal **intracerebral hemorrhage**.
- Thrombolysis is notably less effective for large vessel occlusions compared to **mechanical thrombectomy**, which is the gold standard for **basilar artery** recanalization.
*Proceed with thrombolysis and thrombectomy given the therapeutic window*
- While the patient is within the 4.5-hour window for thrombolysis, the presence of **established early ischemic changes** (>1/3 MCA territory) is a relative contraindication.
- Attempting both increases the risk of **secondary hemorrhage** in the damaged MCA territory without providing significant additional benefit over thrombectomy alone for the **basilar occlusion**.
*Delay intervention and repeat imaging in 6 hours to assess progression*
- Delaying treatment in the setting of **basilar artery occlusion** is inappropriate, as "time is brain" and outcomes worsen significantly with every minute of **brainstem ischemia**.
- Immediate decision-making is required based on the initial imaging, which already confirmed the **large-vessel occlusion** needing intervention.
More Ischemic vs hemorrhagic stroke differentiation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.