Hemorrhagic stroke management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hemorrhagic stroke management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
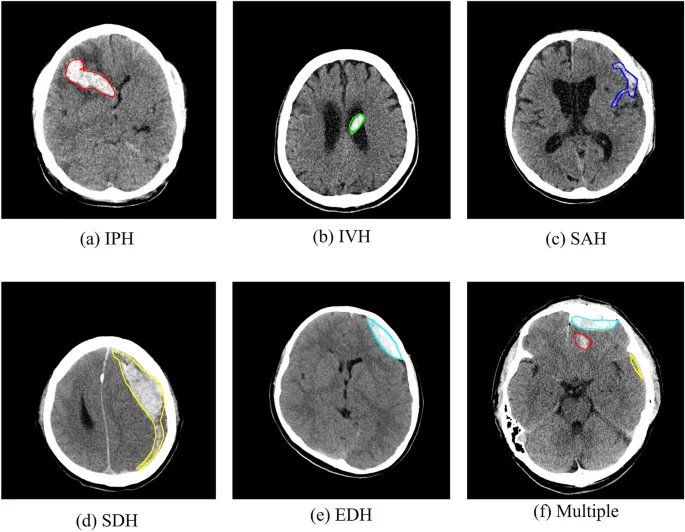
Hemorrhagic stroke management US Medical PG Question 1: A 67-year-old man presents to the emergency department for a headache. The patient states his symptoms started thirty minutes ago. He states he experienced a sudden and severe headache while painting his house, causing him to fall off the ladder and hit his head. He has also experienced two episodes of vomiting and difficulty walking since the fall. The patient has a past medical history of hypertension, obesity, and atrial fibrillation. His current medications include lisinopril, rivaroxaban, atorvastatin, and metformin. His temperature is 99.5°F (37.5°C), blood pressure is 150/105 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. On physical exam, the patient localizes his headache to the back of his head. Cardiac exam reveals a normal rate and rhythm. Pulmonary exam reveals minor bibasilar crackles. Neurological exam is notable for minor weakness of the muscles of facial expression. Examination of cranial nerve three reveals a notable nystagmus. Heel to shin exam is abnormal bilaterally. The patient's gait is notably ataxic. A non-contrast CT scan of the head is currently pending. Which of the following is the most likely diagnosis?
- A. Pontine hemorrhage
- B. Cerebellar hemorrhage (Correct Answer)
- C. Subarachnoid hemorrhage
- D. Thalamic hemorrhage
- E. Subdural hematoma
Hemorrhagic stroke management Explanation: ***Cerebellar hemorrhage***
- The sudden onset of a **severe headache**, localized to the back of the head, combined with **ataxia**, nystagmus, and minor facial weakness, in a patient on **anticoagulation** (rivaroxaban) for atrial fibrillation, strongly suggests a cerebellar hemorrhage.
- **Vomiting** and **difficulty walking** are common symptoms due to the cerebellar involvement and increased intracranial pressure.
*Pontine hemorrhage*
- Pontine hemorrhages typically present with **quadriplegia**, profound **coma**, and **pinpoint pupils**, which are not observed in this patient.
- While it can cause sudden headache and vomiting, the specific neurological deficits (ataxia, nystagmus, mild facial weakness) are less characteristic of a pontine lesion.
*Subarachnoid hemorrhage*
- Characterized by a **"thunderclap" headache** (sudden and severe), often described as the "worst headache of my life," and can cause focal neurological deficits depending on the location of rupture.
- While the sudden onset and severity fit, the specific cerebellar signs (**nystagmus**, **ataxia**, posterior headache) point more directly to a cerebellar lesion, and the fall causing head trauma suggests a hemorrhage within the brain parenchyma.
*Thalamic hemorrhage*
- Thalamic hemorrhages commonly present with **contralateral hemisensory loss**, hemiparesis, and sometimes pupillary abnormalities.
- The patient's presentation with prominent **ataxia**, nystagmus, and posterior headache is less typical for a thalamic hemorrhage.
*Subdural hematoma*
- Subdural hematomas usually result from **trauma** and can have a more **insidious onset** (especially chronic subdural hematomas in elderly or anticoagulated patients).
- While the fall might suggest this, the acute onset of severe headache and the specific neurological signs like **ataxia** and nystagmus are more indicative of an intraparenchymal hemorrhage (like cerebellar) rather than a subdural collection compressing the brain surface.
Hemorrhagic stroke management US Medical PG Question 2: A 48-year-old man presents to the ER with a sudden-onset, severe headache. He is vomiting and appears confused. His wife, who accompanied him, says that he has not had any trauma, and that the patient has no relevant family history. He undergoes a non-contrast head CT that shows blood between the arachnoid and pia mater. What is the most likely complication from this condition?
- A. Hemorrhagic shock
- B. Arterial Vasospasm (Correct Answer)
- C. Renal failure
- D. Bacterial Meningitis
- E. Blindness
Hemorrhagic stroke management Explanation: **Arterial Vasospasm**
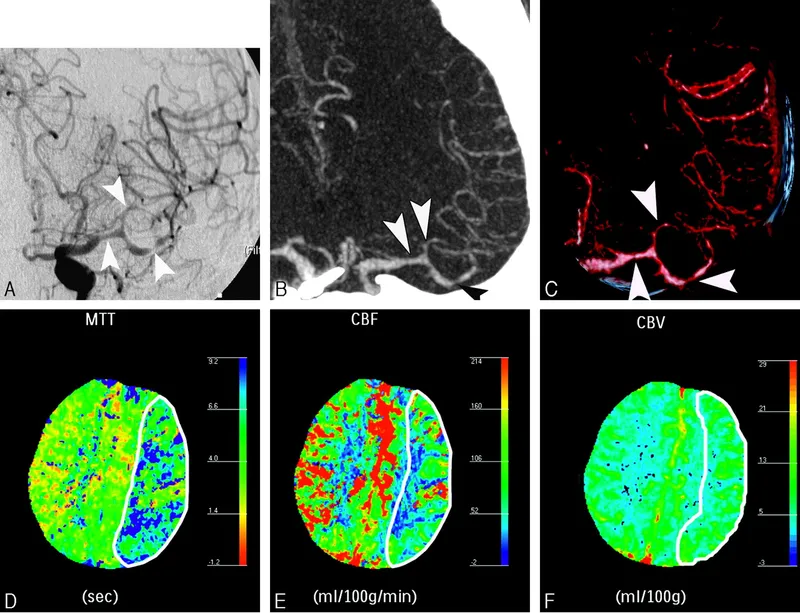
- **Arterial vasospasm** is a major delayed complication of **subarachnoid hemorrhage (SAH)**, typically occurring 3-14 days after the initial bleed.
- The presence of blood products in the subarachnoid space can irritate cerebral arteries, leading to their narrowing and subsequent **delayed cerebral ischemia** or infarction.
*Hemorrhagic shock*
- **Subarachnoid hemorrhage (SAH)** typically involves bleeding within the confines of the skull, which is usually not extensive enough to cause systemic **hypovolemia** or **hemorrhagic shock**.
- **Hemorrhagic shock** would require significant external blood loss or internal bleeding into a large body cavity, which is not characteristic of an isolated SAH.
*Renal failure*
- **Renal failure** is not a direct or common complication of **subarachnoid hemorrhage (SAH)**.
- While systemic complications can sometimes arise in critically ill patients, there is no direct pathophysiological link between SAH and primary kidney injury.
*Bacterial Meningitis*
- The presence of blood in the **subarachnoid space** can cause a **chemical meningitis** due to irritation, mimicking some symptoms of bacterial meningitis.
- However, it does not typically predispose to **bacterial infection** unless there's an iatrogenic cause (e.g., lumbar puncture contamination).
*Blindness*
- While damage to the **optic nerves** or visual pathways can occur with severe neurological events or increased intracranial pressure, **blindness** is not a common or direct complication specifically arising from the bleed itself or its immediate sequelae in SAH.
- Visual disturbances are possible due to elevated **intracranial pressure** or specific anatomical lesion, but not primary blindness.
Hemorrhagic stroke management US Medical PG Question 3: A 72-year-old woman is brought to the emergency department by her son after he noticed that she was slurring her speech. He also noticed that she appeared to have difficulty using her fork about halfway through dinner when the speech problems started. He brought her to the emergency department immediately and he estimates that only 1 hour has passed since the beginning of the symptoms. An immediate exam is conducted. A medication is administered to ameliorate the effects of this patient's condition that would not be available for use if the patient had presented significantly later. An hour later the patient's condition becomes significantly worse and new deficits are found. Which of the following agents should be used at this point?
- A. Protamine sulfate
- B. Antivenin
- C. Aminocaproic acid
- D. Plasma transfusion (Correct Answer)
- E. Vitamin K
Hemorrhagic stroke management Explanation: ***Plasma transfusion***
- The patient's clinical presentation (acute focal neurological deficits within 1 hour) indicates **ischemic stroke**, and the "medication administered to ameliorate effects...not available if presented significantly later" is **tissue plasminogen activator (tPA/alteplase)**, which must be given within 3-4.5 hours of symptom onset.
- The subsequent **worsening with new deficits** after initial tPA administration strongly suggests **hemorrhagic transformation** of the ischemic stroke, a known complication of thrombolytic therapy.
- **Fresh frozen plasma (FFP)** is the appropriate treatment because tPA depletes **fibrinogen and clotting factors** through systemic fibrinolysis, and FFP directly replaces these consumed clotting factors to help control bleeding.
- Management of tPA-related hemorrhage includes: stopping tPA, emergent neuroimaging, and administration of **cryoprecipitate** (to replace fibrinogen) and/or **FFP** (to replace clotting factors).
*Aminocaproic acid*
- **Aminocaproic acid** is an antifibrinolytic agent that inhibits plasminogen activation.
- While it can theoretically help in fibrinolytic-related bleeding, it is **NOT first-line therapy** for tPA-associated hemorrhagic transformation.
- **Cryoprecipitate and FFP** are preferred because they directly replace the fibrinogen and clotting factors depleted by tPA, addressing the underlying coagulopathy.
*Protamine sulfate*
- **Protamine sulfate** reverses **heparin** anticoagulation by binding to and inactivating heparin.
- This patient received tPA (a thrombolytic), not heparin, so protamine would not be effective.
*Antivenin*
- **Antivenin** is used to neutralize venom from snake or spider bites.
- This patient's presentation is consistent with stroke and tPA complication, not envenomation.
*Vitamin K*
- **Vitamin K** reverses **warfarin** by promoting hepatic synthesis of vitamin K-dependent clotting factors (II, VII, IX, X).
- Warfarin reversal takes hours to days; in acute bleeding, **FFP or prothrombin complex concentrate (PCC)** provides immediate factor replacement.
- This patient's complication is related to tPA (thrombolytic), not warfarin.
Hemorrhagic stroke management US Medical PG Question 4: A 69-year-old male presents to the emergency department for slurred speech and an inability to use his right arm which occurred while he was eating dinner. The patient arrived at the emergency department within one hour. A CT scan was performed of the head and did not reveal any signs of hemorrhage. The patient is given thrombolytics and is then managed on the neurology floor. Three days later, the patient is recovering and is stable. He seems depressed but is doing well with his symptoms gradually improving as compared to his initial presentation. The patient complains of neck pain that has worsened slowly over the past few days for which he is being given ibuprofen. Laboratory values are ordered and return as indicated below:
Serum:
Na+: 130 mEq/L
K+: 3.7 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 7 mg/dL
Glucose: 70 mg/dL
Creatinine: 0.9 mg/dL
Ca2+: 9.7 mg/dL
Urine:
Appearance: dark
Glucose: negative
WBC: 0/hpf
Bacterial: none
Na+: 320 mEq/L/24 hours
His temperature is 99.5°F (37.5°C), pulse is 95/min, blood pressure is 129/70 mmHg, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Demeclocycline
- B. Fluid restriction (Correct Answer)
- C. Oral salt tablets
- D. Continue conservative management
- E. Conivaptan
Hemorrhagic stroke management Explanation: ***Fluid restriction***
- The patient presents with **hyponatremia** (Na+ 130 mEq/L) and elevated urine sodium (320 mEq/L/24 hours) in the setting of recent stroke and possible SIADH (**Syndrome of Inappropriate Antidiuretic Hormone secretion**).
- **Fluid restriction** is the initial and most crucial step in managing euvolemic hyponatremia due to SIADH, reducing water intake to allow the kidney to excrete excess water and correct serum sodium.
*Demeclocycline*
- **Demeclocycline** is a tetracycline derivative that inhibits the action of ADH on renal tubules, used in chronic or refractory cases of SIADH.
- It is *not* the first-line treatment for acute, moderate hyponatremia, especially when fluid restriction has not yet been attempted.
*Oral salt tablets*
- **Oral salt tablets** would increase the solute load but would also draw water, potentially worsening hyponatremia if unrestricted fluid intake persists in SIADH.
- This intervention is generally not appropriate for **euvolemic hyponatremia** where the primary issue is excess free water.
*Continue conservative management*
- With a sodium level of 130 mEq/L, this is considered **mild to moderate hyponatremia** and requires active intervention to prevent potential neurological complications.
- Simply continuing conservative management without addressing the underlying **hyponatremia** or its cause would be inadequate and potentially harmful.
*Conivaptan*
- **Conivaptan** is an ADH receptor antagonist that can be used for persistent or significant hyponatremia in SIADH.
- It is typically reserved for more severe or refractory cases of hyponatremia and is usually administered intravenously, making it less suitable as a first-line outpatient management strategy.
Hemorrhagic stroke management US Medical PG Question 5: A new treatment for hemorrhagic stroke, which is a life-threatening clinical condition that occurs when a diseased blood vessel in the brain ruptures or leaks, was evaluated as soon as it hit the market by an international group of neurology specialists. In those treated with the new drug, a good outcome was achieved in 30%, while those treated with the current standard of care had a good outcome in just 10% of cases. The clinicians involved in this cohort study concluded that the newer drug is more effective and prompted for urgent changes in the guidelines addressing hemorrhagic stroke incidents. According to the aforementioned percentages, how many patients must be treated with the new drug to see 1 additional good outcome?
- A. 5 (Correct Answer)
- B. 30
- C. 20
- D. 15
- E. 10
Hemorrhagic stroke management Explanation: ***Correct: 5***
- This is calculated using the concept of **Number Needed to Treat (NNT)**, which tells us how many patients need to receive the new treatment to see one additional good outcome compared to standard care.
- The **Absolute Risk Reduction (ARR)** is the difference in good outcome rates: 30% - 10% = 20% (or 0.20 as a proportion).
- **NNT = 1 / ARR = 1 / 0.20 = 5**
- Therefore, treating 5 patients with the new drug will result in 1 additional patient with a good outcome compared to standard care.
*Incorrect: 30*
- This represents the **percentage of patients** who achieved a good outcome with the new drug, not the number needed to treat.
- It does not account for the baseline effectiveness of standard treatment, which is essential for calculating the marginal benefit.
- This is the absolute event rate in the treatment group, not a comparative measure.
*Incorrect: 20*
- This is the **Absolute Risk Reduction (ARR)** expressed as a percentage (30% - 10% = 20%).
- While this is a key component in calculating NNT, it is not the NNT itself.
- The NNT requires taking the reciprocal of the ARR when expressed as a proportion: 1/0.20 = 5.
*Incorrect: 15*
- This number does not correspond to any standard epidemiological or biostatistical measure in this context.
- It is neither the ARR, NNT, relative risk, nor any other interpretable value from the given data.
- This is an arbitrary distractor with no mathematical basis.
*Incorrect: 10*
- This represents the **percentage of patients** who achieved a good outcome with standard care (the control group).
- It is the baseline event rate, not a measure of treatment effect or comparative effectiveness.
- Like option 30, it does not reflect the additional benefit from the new treatment.
Hemorrhagic stroke management US Medical PG Question 6: A 74-year-old man presents to the emergency department by paramedics for slurred speech and weakness in the left arm and leg for 1 hour. The patient was playing with his grandson when the symptoms started and his wife immediately called an ambulance. There is no history of head trauma or recent surgery. The patient takes captopril for hypertension. The vital signs include: pulse 110/min, respiratory rate 22/min, and blood pressure 200/105 mm Hg. The physical examination shows that the patient is alert and conscious, but speech is impaired. Muscle strength is 0/5 in the left arm and leg and 5/5 in the right arm and leg. A non-contrast CT of the head shows no evidence of intracranial bleeding. The lab results are as follows:
Serum glucose 90 mg/dL
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 1.3 mg/dL
Blood urea nitrogen 20 mg/dL
Cholesterol, total 240 mg/dL
HDL-cholesterol 38 mg/dL
LDL-cholesterol 100 mg/dL
Triglycerides 190 mg/dL
Hemoglobin (Hb%) 15.3 g/dL
Mean corpuscular volume (MCV) 83 fL
Reticulocyte count 0.8%
Erythrocyte count 5.3 million/mm3
Platelet count 130,000/mm3
Partial thromboplastin time (aPTT) 30 sec
Prothrombin time (PT) 12 sec
Although he is within the time frame for the standard therapy of the most likely condition, the treatment cannot be started because of which of the following contraindications?
- A. A platelet count of 130,000/mm3
- B. Age of 74 years
- C. Cholesterol level of 240 mg/dL
- D. Creatinine level of 1.3 mg/dL
- E. Systolic blood pressure of 200 mm Hg (Correct Answer)
Hemorrhagic stroke management Explanation: ***Systolic blood pressure of 200 mm Hg***
- The patient presents with symptoms highly suggestive of an **acute ischemic stroke**, including **slurred speech** and **left-sided weakness**.
- For patients with acute ischemic stroke who are candidates for **thrombolytic therapy (e.g., alteplase)**, a **systolic blood pressure consistently >185 mm Hg or diastolic >110 mm Hg is a contraindication** due to increased risk of hemorrhagic transformation.
*A platelet count of 130,000/mm3*
- A platelet count of 130,000/mm³ is above the **contraindication threshold for thrombolytic therapy**, which is typically <100,000/mm³.
- Therefore, this platelet count would **not prevent** the initiation of tPA.
*Age of 74 years*
- While older age was once considered a relative contraindication, current guidelines **do not consider age alone (including 74 years old) as an absolute contraindication** for thrombolytic therapy in acute ischemic stroke.
- Eligibility is determined by a comprehensive risk-benefit assessment, not solely by age.
*Cholesterol level of 240 mg/dL*
- An elevated **cholesterol level** is a **risk factor for atherosclerosis** and ischemic stroke, but it is **not a contraindication for acute thrombolytic therapy**.
- It relates to the underlying cause of the stroke rather than the immediate treatment decision.
*Creatinine level of 1.3 mg/dL*
- A **creatinine level of 1.3 mg/dL** indicates **mild renal impairment**, but it is **not a contraindication for thrombolytic therapy**.
- Renal function more significantly impacts the use of certain anticoagulants, but not typically alteplase in the acute setting.
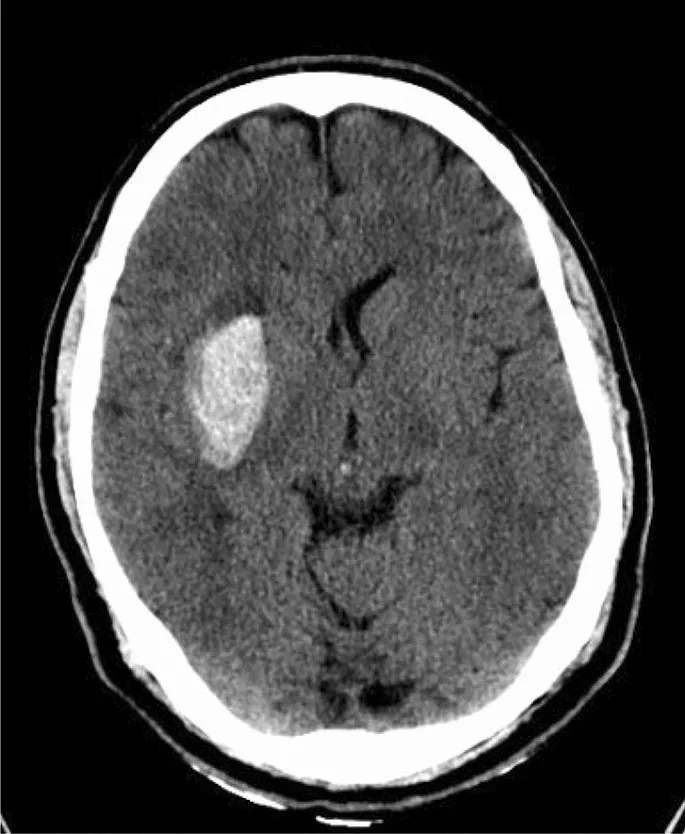
Hemorrhagic stroke management US Medical PG Question 7: A 23-year-old man presents with a blunt force injury to the head from a baseball bat. He is currently unconscious, although his friends say he was awake and speaking with them en route to the hospital. He has no significant past medical history and takes no current medications. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 165/85 mm Hg, pulse 50/min, and respiratory rate 19/min. On physical examination, there is a blunt force injury to the left temporoparietal region approximately 10.1–12.7 cm (4–5 in) in diameter. There is anisocoria of the left pupil, which is unresponsive to light. The patient is intubated and fluid resuscitation is initiated. A noncontrast computed tomography (CT) scan of the head is acquired and shown in the exhibit (see image). Which of the following is the most appropriate medical treatment for this patient?
- A. Placement of a ventriculoperitoneal (VP) shunt
- B. Acetazolamide
- C. Placing the head of the bed at 0 degrees
- D. Maintain a PaCO2 of 24 mm Hg
- E. Mannitol (Correct Answer)
Hemorrhagic stroke management Explanation: ***Mannitol***
- The patient presents with classic signs of **epidural hematoma** (lucid interval, ipsilateral pupillary dilation, contralateral hemiparesis), and the CT scan confirms a large, biconvex hemorrhage compressing the brain.
- **Mannitol** is an osmotic diuretic used to rapidly **reduce intracranial pressure (ICP)** by drawing water from the brain into the vasculature, which can be life-saving in cases of acute brain herniation.
*Placement of a ventriculoperitoneal (VP) shunt*
- A VP shunt is used for long-term management of **hydrocephalus** due to impaired CSF absorption or flow, not for acute, traumatic hemorrhage and mass effect.
- Placing a shunt would not address the immediate, life-threatening mass effect from the epidural hematoma.
*Acetazolamide*
- **Acetazolamide** is a carbonic anhydrase inhibitor that reduces CSF production, primarily used for conditions like chronic **idiopathic intracranial hypertension** (pseudotumor cerebri) or hydrocephalus.
- It is not an effective treatment for the rapid reduction of ICP in the setting of acute intracranial hemorrhage and mass effect.
*Placing the head of the bed at 0 degrees*
- Keeping the head of the bed flat (at 0 degrees) is generally discouraged in patients with **elevated ICP** as it can worsen cerebral venous outflow and increase ICP.
- Elevating the head of the bed to **30 degrees** is standard practice to promote venous drainage and reduce ICP.
*Maintain a PaCO2 of 24 mm Hg*
- While **hyperventilation** to lower PaCO2 can cause cerebral vasoconstriction and reduce ICP, maintaining a PaCO2 as low as 24 mm Hg (severe hyperventilation) is typically reserved for **brief periods** in severe, refractory ICP elevation.
- Prolonged severe hyperventilation can lead to **cerebral ischemia** due to excessive vasoconstriction and is generally not the first-line or sustained management strategy.
Hemorrhagic stroke management US Medical PG Question 8: A 44-year-old man comes to the emergency department because of a severe headache and blurry vision for the past 3 hours. He has hypertension treated with hydrochlorothiazide. He has missed taking his medication for the past week as he was traveling. He is only oriented to time and person. His temperature is 37.1°C (98.8°F), pulse is 92/min and regular, and blood pressure is 245/115 mm Hg. Cardiopulmonary examination shows no abnormalities. Fundoscopy shows bilateral retinal hemorrhages and exudates. Neurologic examination shows no focal findings. A complete blood count and serum concentrations of electrolytes, glucose, and creatinine are within the reference range. A CT scan of the brain shows no abnormalities. Which of the following is the most appropriate pharmacotherapy?
- A. Sublingual nifedipine
- B. Oral captopril
- C. Intravenous nitroprusside (Correct Answer)
- D. Oral clonidine
- E. Intravenous mannitol
Hemorrhagic stroke management Explanation: ***Intravenous nitroprusside***
- The patient presents with **hypertensive emergency**, characterized by **severe hypertension** (245/115 mmHg) with **acute end-organ damage**, including altered mental status and retinal hemorrhages/exudates.
- **Intravenous nitroprusside** is a potent, rapidly acting vasodilator making it an excellent choice for immediate and controlled reduction of blood pressure in such critical situations.
*Sublingual nifedipine*
- **Sublingual nifedipine** can cause a sudden and uncontrolled drop in blood pressure, leading to **ischemia** due to inadequate perfusion of vital organs.
- It also has a less predictable and slower onset of action compared to intravenous agents, making it unsuitable for acute hypertensive emergencies.
*Oral captopril*
- **Oral captopril** has a slower onset of action and is less suitable for the acute management of a **hypertensive emergency** where immediate and precise blood pressure control is crucial.
- While an ACE inhibitor, its oral administration does not provide the rapid titratability needed to safely lower dangerously high blood pressures.
*Oral clonidine*
- **Oral clonidine** also has a relatively slow onset of action and its effects can be variable, making it less ideal for the acute, emergent management of **severe hypertension** with end-organ damage.
- It is more appropriate for urgent but non-emergent hypertension or chronic management, not for situations requiring immediate and controlled blood pressure reduction.
*Intravenous mannitol*
- **Intravenous mannitol** is an osmotic diuretic primarily used to reduce **intracranial pressure** or to promote diuresis.
- It does not directly lower blood pressure effectively in a hypertensive emergency and is not a primary antihypertensive agent.
Hemorrhagic stroke management US Medical PG Question 9: A 48-year-old woman is brought to the emergency department because of a 1-hour history of sudden-onset headache associated with nausea and vomiting. The patient reports she was sitting at her desk when the headache began. The headache is global and radiates to her neck. She has hypertension. She has smoked one pack of cigarettes daily for the last 10 years. She drinks alcohol occasionally. Her father had a stroke at the age 58 years. Current medications include hydrochlorothiazide. She is in severe distress. She is alert and oriented to person, place, and time. Her temperature is 38.2°C (100.8°F), pulse is 89/min, respirations are 19/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities. Cranial nerves II–XII are intact. She has no focal motor or sensory deficits. She flexes her hips and knees when her neck is flexed while lying in a supine position. A CT scan of the head is shown. Which of the following is the most appropriate intervention?
- A. Perform burr hole surgery
- B. Administer intravenous alteplase
- C. Administer intravenous vancomycin and ceftriaxone
- D. Perform surgical clipping (Correct Answer)
- E. Perform decompressive craniectomy
Hemorrhagic stroke management Explanation: ***Perform surgical clipping***
- The clinical presentation of **sudden-onset severe headache** ("thunderclap headache"), **nausea, vomiting, neck stiffness (positive Brudzinski's sign)**, and the CT scan showing **blood in the subarachnoid space** strongly indicate a **subarachnoid hemorrhage (SAH)** from a ruptured cerebral aneurysm.
- Definitive treatment requires **securing the aneurysm** to prevent **rebleeding**, which carries 40-50% mortality. Modern management includes **endovascular coiling** (first-line for most cases) or **surgical clipping**.
- **Surgical clipping** involves placing a metal clip across the aneurysm neck to exclude it from circulation. It remains the preferred approach for certain aneurysm locations (MCA), wide-necked aneurysms, or when accompanied by hematoma requiring evacuation.
- Among the options provided, surgical clipping is the only definitive intervention that secures the ruptured aneurysm.
*Perform burr hole surgery*
- **Burr hole surgery** is used for draining **subdural hematomas** or accessing the brain for procedures like biopsy or external ventricular drain placement.
- While burr holes may be needed for complications of SAH (e.g., hydrocephalus requiring EVD), this is not the primary intervention for securing the ruptured aneurysm itself.
*Administer intravenous alteplase*
- **Alteplase** (tPA) is a **thrombolytic agent** used for **acute ischemic stroke** within 4.5 hours of symptom onset.
- Administering thrombolytics in **hemorrhagic stroke** (like SAH) is **absolutely contraindicated** as it would worsen bleeding and cause catastrophic neurological deterioration or death.
*Administer intravenous vancomycin and ceftriaxone*
- **Vancomycin and ceftriaxone** treat **bacterial meningitis**, which can present with headache, fever, and meningeal signs.
- Although the patient has low-grade fever (likely from blood irritating meninges, not infection) and neck stiffness, the **sudden-onset thunderclap headache** and **CT findings of SAH** make ruptured aneurysm the diagnosis, not meningitis. The fever in SAH is typically from aseptic meningeal irritation.
*Perform decompressive craniectomy*
- **Decompressive craniectomy** removes skull bone to relieve **elevated intracranial pressure** from massive brain swelling (severe TBI, malignant MCA infarction).
- While SAH can cause elevated ICP, craniectomy does not secure the aneurysm. The immediate priority is preventing **rebleeding** by securing the aneurysm source, not managing secondary complications.
Hemorrhagic stroke management US Medical PG Question 10: A 65-year-old man presents to the emergency department for sudden weakness. He was doing mechanical work on his car where he acutely developed right-leg weakness and fell to the ground. He is accompanied by his wife, who said that this has never happened before. He was last seen neurologically normal approximately 2 hours prior to presentation. His past medical history is significant for hypertension and type II diabetes. His temperature is 98.8°F (37.1°C), blood pressure is 177/108 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 99% on room air. Neurological exam reveals that he is having trouble speaking and has profound weakness of his right upper and lower extremity. Which of the following is the best next step in management?
- A. Thrombolytics
- B. Noncontrast head CT (Correct Answer)
- C. CT angiogram
- D. MRI of the head
- E. Aspirin
Hemorrhagic stroke management Explanation: ***Noncontrast head CT***
- A **noncontrast head CT** is the most crucial initial step in managing acute stroke symptoms because it can rapidly rule out an **intracranial hemorrhage**.
- Distinguishing between ischemic stroke and hemorrhagic stroke is critical, as the management strategies are vastly different and administering thrombolytics in the presence of hemorrhage can be fatal.
*Thrombolytics*
- **Thrombolytics** can only be administered after an **intracranial hemorrhage** has been excluded via noncontrast head CT.
- Administering thrombolytics without imaging could worsen a hemorrhagic stroke, causing significant harm or death.
*CT angiogram*
- A **CT angiogram** is used to identify large vessel occlusions in ischemic stroke and is typically performed after a noncontrast CT rules out hemorrhage.
- This imaging is crucial for determining eligibility for **endovascular thrombectomy** but is not the very first diagnostic step.
*MRI of the head*
- An **MRI of the head** is more sensitive for detecting acute ischemic changes but takes longer to perform and is often not readily available in the acute emergency setting.
- It is not the initial imaging of choice for ruling out hemorrhage due to its longer acquisition time compared to CT.
*Aspirin*
- **Aspirin** is indicated for acute ischemic stroke but should only be given after an **intracranial hemorrhage** has been ruled out.
- Like thrombolytics, aspirin could exacerbate a hemorrhagic stroke and is thus deferred until initial imaging is complete.
More Hemorrhagic stroke management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.