Sepsis-induced organ dysfunction management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sepsis-induced organ dysfunction management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sepsis-induced organ dysfunction management US Medical PG Question 1: A previously healthy 35-year-old woman is brought into the emergency department after being found unresponsive by her husband. Her husband finds an empty bottle of diazepam tablets in her pocket. She is stuporous. At the hospital, her blood pressure is 90/40 mm Hg, the pulse is 58/min, and the respirations are 6/min. The examination of the pupils shows normal size and reactivity to light. Deep tendon reflexes are 1+ bilaterally. Babinski sign is absent. All 4 extremities are hypotonic. The patient is intubated and taken to the critical care unit for mechanical ventilation and treatment. Regarding the prevention of pneumonia in this patient, which of the following strategies is most likely to achieve this goal?
- A. Nasogastric tube insertion
- B. Daily evaluation for ventilator weaning
- C. Subglottic drainage of secretions (Correct Answer)
- D. Oropharynx and gut antibacterial decontamination
- E. Prone positioning during mechanical ventilation
Sepsis-induced organ dysfunction management Explanation: ***Subglottic drainage of secretions***
- This is a highly effective strategy to prevent **ventilator-associated pneumonia (VAP)** by continuously removing secretions that pool above the endotracheal tube cuff before they can be aspirated.
- Endotracheal tubes with a **subglottic secretion drainage port** reduce VAP incidence by preventing microaspiration of contaminated oropharyngeal secretions into the lower respiratory tract.
- This is a **specific mechanical intervention** that directly addresses one of the key pathogenic mechanisms of VAP.
*Nasogastric tube insertion*
- While an NG tube may be needed for feeding or gastric decompression, it does not directly prevent VAP and may **increase aspiration risk** by compromising the lower esophageal sphincter.
- NG tubes can promote gastroesophageal reflux and provide a conduit for bacterial migration.
*Daily evaluation for ventilator weaning*
- This is also a **critical component of VAP prevention** as part of the ventilator bundle, since reducing duration of mechanical ventilation is the most effective overall strategy to prevent VAP.
- However, in this question asking for a strategy to prevent pneumonia in an intubated patient, subglottic drainage is the more specific technical intervention, whereas daily weaning assessment is a broader protocol that reduces exposure time.
- Both strategies are important; subglottic drainage addresses the "how" of prevention during intubation, while weaning protocols address the "duration" of risk exposure.
*Oropharynx and gut antibacterial decontamination*
- Selective digestive decontamination (SDD) aims to reduce bacterial colonization, but evidence for routine use is mixed and raises concerns about **antimicrobial resistance**.
- Not universally recommended as a primary VAP prevention strategy in most guidelines.
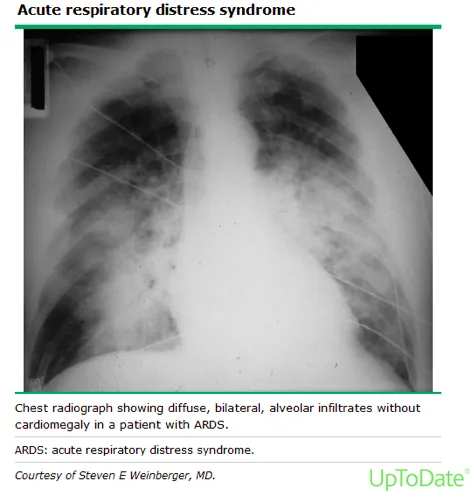
*Prone positioning during mechanical ventilation*
- **Prone positioning** is primarily indicated for improving oxygenation in **Acute Respiratory Distress Syndrome (ARDS)**, not for VAP prevention.
- While it may improve secretion drainage, it is not a standard VAP prevention measure and carries its own risks and logistical challenges.
Sepsis-induced organ dysfunction management US Medical PG Question 2: You are called to a hemodialysis suite. The patient is a 61-year-old man with a history of hypertension, hypercholesterolemia, and type-2 diabetes mellitus-induced end-stage renal disease who has required hemodialysis for the past year. His current hemodialysis session is nearing the end when the nurse notices that his blood pressure has dropped to 88/60 mm Hg from his normal of 142/90 mm Hg. The patient denies any shortness of breath or chest pain. He took his daily bisoprolol, metformin, and insulin this morning before coming to the hospital. On examination, the patient’s blood pressure is 92/60 mm Hg, and his heart rate is 119/min. Chest auscultation is unremarkable. What is the most appropriate next management step?
- A. Infuse 1 liter of 0.9% saline
- B. Administer intravenous calcium gluconate
- C. Transfuse the patient with 1 unit of packed red blood cells
- D. Stop ultrafiltration and decrease blood flow into the machine (Correct Answer)
- E. Start the patient on an epinephrine drip
Sepsis-induced organ dysfunction management Explanation: ***Stop ultrafiltration and decrease blood flow into the machine***
- The patient's **hypotension** and **tachycardia** during hemodialysis strongly suggest **intradialytic hypotension**, which is often caused by excessive fluid removal (ultrafiltration) or rapid fluid shifts.
- **Stopping ultrafiltration** and **reducing blood flow** allows for gradual re-equilibration of fluid and helps stabilize blood pressure without adding more fluid to a patient with end-stage renal disease.
*Infuse 1 liter of 0.9% saline*
- Administering a large volume of saline is generally **contraindicated in ESRD patients** given their inability to excrete fluid, which could lead to **fluid overload** and pulmonary edema.
- While fluid resuscitation might be considered for severe hypotension, the initial step in intradialytic hypotension is to adjust the dialysis settings.
*Administer intravenous calcium gluconate*
- **Calcium gluconate** is primarily used to stabilize the cardiac membrane in cases of **severe hyperkalemia**, which is not indicated by the current clinical picture.
- There is no mention of ECG changes or lab results to suggest hyperkalemia.
*Transfuse the patient with 1 unit of packed red blood cells*
- There is no clinical evidence of **acute blood loss** or **severe anemia** presenting with hypovolemic shock.
- Transfusion is an intervention for significant blood loss or severe anemia, not for intradialytic hypotension caused by fluid shifts.
*Start the patient on an epinephrine drip*
- **Vasopressors** like epinephrine are typically reserved for **refractory hypotension** after more conservative measures have failed, or in cases of **septic shock** or **anaphylaxis**.
- Initiating a powerful vasopressor as a first step without addressing the potential underlying cause related to dialysis is inappropriate.
Sepsis-induced organ dysfunction management US Medical PG Question 3: A 61-year-old female with congestive heart failure and type 2 diabetes is brought to the emergency room by her husband because of an altered mental status. He states he normally helps her be compliant with her medications, but he had been away for several days. On physical exam, her temperature is 37.2 C, BP 85/55, and HR 130. Serum glucose is 500 mg/dL. Which of the following is the first step in the management of this patient?
- A. IV ½ NS
- B. IV insulin
- C. Subcutaneous insulin injection
- D. IV NS (Correct Answer)
- E. IV D5W
Sepsis-induced organ dysfunction management Explanation: ***IV NS***
- The patient presents with **hypotension (85/55 mmHg)** and **tachycardia (130 bpm)**, indicating significant **volume depletion** despite a history of congestive heart failure.
- **Isotonic intravenous fluids (e.g., normal saline)** are crucial in the initial management of **diabetic ketoacidosis (DKA)** or **hyperosmolar hyperglycemic state (HHS)** to restore intravascular volume and improve tissue perfusion.
*IV ½ NS*
- **Hypotonic solutions** such as IV ½ NS are typically used later in DKA/HHS management, once the patient's **hemodynamic stability** has been achieved and serum sodium levels are stable or elevated.
- Administering hypotonic fluids to an already **hypotensive and volume-depleted patient** could worsen hypotension and potentially lead to cerebral edema if not carefully monitored.
*IV insulin*
- While insulin is essential for correcting hyperglycemia, it is administered **after or concurrently with fluid resuscitation** to avoid worsening hypovolemia as it drives glucose and potassium into cells, potentially causing **hypokalemia** and further **hemoconcentration**.
- **Fluid resuscitation** should always precede or be initiated simultaneously with insulin therapy, especially in cases of hemodynamic instability.
*Subcutaneous insulin injection*
- **Subcutaneous insulin** is not appropriate for initial management in this critically ill patient due to its **slower onset of action** and potentially **erratic absorption** in hypotensive and poorly perfused states.
- **Intravenous insulin** is preferred in DKA/HHS for its rapid, titratable effect.
*IV D5W*
- **Dextrose 5% in water (D5W)** is a hypotonic solution primarily used when **blood glucose levels fall below 250 mg/dL** during DKA/HHS treatment to prevent hypoglycemia.
- Administering D5W in a patient with a **serum glucose of 500 mg/dL** would further elevate blood sugar and worsen the hyperosmolar state.
Sepsis-induced organ dysfunction management US Medical PG Question 4: A 70-year-old man with a recent above-the-knee amputation of the left lower extremity, due to wet gangrene secondary to refractory peripheral artery disease, presents with weakness and dizziness. He says that the symptoms began acutely 24 hours after surgery and have not improved. The amputation was complicated by substantial blood loss. He was placed on empiric antibiotic therapy with ciprofloxacin and clindamycin before the procedure, and blood and wound culture results are still pending. The medical history is significant for type 2 diabetes mellitus and hypertension. Current medications are metformin and lisinopril. The family history is significant for type 2 diabetes mellitus in both parents. Review of symptoms is significant for palpitations and a mild headache for the past 24 hours. His temperature is 38.2°C (100.8°F); blood pressure, 120/70 mm Hg (supine); pulse, 102/min; respiratory rate, 16/min; and oxygen saturation, 99% on room air. When standing, the blood pressure is 90/65 mm Hg and the pulse is 115/min. On physical examination, the patient appears pale and listless. The surgical amputation site does not show any signs of ongoing blood loss or infection. Laboratory tests and an ECG are pending. Which of the following is the next best step in management?
- A. Administer IV fluids
- B. Administer oral fludrocortisone
- C. Administer IV norepinephrine
- D. Administer oral midodrine
- E. Administer IV fluids and withhold lisinopril (Correct Answer)
Sepsis-induced organ dysfunction management Explanation: ***Administer IV fluids and withhold lisinopril***
- The patient's **postural orthostatic hypotension** (blood pressure drop upon standing) and symptoms (weakness, dizziness, palpitations, pallor) following significant blood loss during surgery strongly suggest **hypovolemia**, which should be managed immediately with IV fluids.
- **Lisinopril**, an ACE inhibitor, can exacerbate hypotension by blocking angiotensin II-mediated vasoconstriction and aldosterone secretion, so withholding it is crucial in this hypotensive patient.
*Administer IV fluids*
- While administration of IV fluids is a correct component of management for hypovolemia, it is incomplete without addressing potential medication-induced hypotension in this patient.
- Simply administering IV fluids without withholding **lisinopril** may lead to suboptimal correction of the patient's hypotension.
*Administer oral fludrocortisone*
- **Fludrocortisone** is a mineralocorticoid used primarily for chronic orthostatic hypotension, such as in autonomic dysfunction, and would not be appropriate for acute, likely hypovolemia-induced hypotension in a postoperative setting.
- Its effects are not immediate, and it does not address the acute fluid deficit or the potential exacerbating effect of **lisinopril**.
*Administer IV norepinephrine*
- **Norepinephrine** is a potent vasopressor used in distributive or cardiogenic shock, which is not indicated as the initial management for suspected hypovolemia.
- Administering vasopressors in an unresuscitated hypovolemic patient can be dangerous, as it can worsen tissue perfusion by increasing systemic vascular resistance without adequate intravascular volume.
*Administer oral midodrine*
- **Midodrine** is an alpha-1 adrenergic agonist used for chronic orthostatic hypotension to increase peripheral vascular tone, similar to fludrocortisone.
- It works slowly and is not indicated for the acute management of hypovolemic shock or postoperative hypotension.
Sepsis-induced organ dysfunction management US Medical PG Question 5: A 14-year-old female with no past medical history presents to the emergency department with nausea and abdominal pain. On physical examination, her blood pressure is 78/65, her respiratory rate is 30, her breath has a fruity odor, and capillary refill is > 3 seconds. Serum glucose is 820 mg/dL. After starting IV fluids, what is the next best step in the management of this patient?
- A. Intravenous Dextrose in water
- B. Subcutaneous insulin glargine
- C. Intravenous regular insulin (Correct Answer)
- D. Intravenous glucagon
- E. Subcutaneous insulin lispro
Sepsis-induced organ dysfunction management Explanation: ***Intravenous regular insulin***
- The patient presents with **diabetic ketoacidosis (DKA)**, characterized by **hyperglycemia**, **fruity breath** (due to ketones), and **hypotension**. Prompt administration of **intravenous regular insulin** is crucial to lower blood glucose and resolve ketoacidosis.
- **Regular insulin** is preferred intravenously due to its **rapid onset** and short duration of action, allowing for precise titration and continuous adjustment based on glucose levels.
*Intravenous Dextrose in water*
- **Dextrose** would further increase the already severely elevated blood glucose level in a patient with DKA, worsening the metabolic derangements.
- Dextrose is typically initiated only after blood glucose drops to safe levels (<200 mg/dL) to prevent **hypoglycemia** during insulin infusion.
*Subcutaneous insulin glargine*
- **Insulin glargine** is a **long-acting insulin** designed for basal insulin coverage, not for acute management of severe hyperglycemia or DKA.
- Its **slow onset of action** and prolonged effect make it unsuitable for the urgent and rapid glucose reduction required in DKA.
*Intravenous glucagon*
- **Glucagon** is a hormone that **raises blood glucose levels**, counteracting the effects of insulin.
- Administering glucagon would exacerbate the severe hyperglycemia present in DKA and is used only in cases of severe hypoglycemia.
*Subcutaneous insulin lispro*
- **Insulin lispro** is a **rapid-acting insulin analog** but is typically given subcutaneously.
- While faster than regular insulin subcutaneously, the **subcutaneous route** has variable absorption in critically ill patients, and the immediate and precisely controllable effect of intravenous regular insulin is needed in DKA.
Sepsis-induced organ dysfunction management US Medical PG Question 6: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
Sepsis-induced organ dysfunction management Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
Sepsis-induced organ dysfunction management US Medical PG Question 7: A 23-year-old man presents with a blunt force injury to the head from a baseball bat. He is currently unconscious, although his friends say he was awake and speaking with them en route to the hospital. He has no significant past medical history and takes no current medications. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 165/85 mm Hg, pulse 50/min, and respiratory rate 19/min. On physical examination, there is a blunt force injury to the left temporoparietal region approximately 10.1–12.7 cm (4–5 in) in diameter. There is anisocoria of the left pupil, which is unresponsive to light. The patient is intubated and fluid resuscitation is initiated. A noncontrast computed tomography (CT) scan of the head is acquired and shown in the exhibit (see image). Which of the following is the most appropriate medical treatment for this patient?
- A. Placement of a ventriculoperitoneal (VP) shunt
- B. Acetazolamide
- C. Placing the head of the bed at 0 degrees
- D. Maintain a PaCO2 of 24 mm Hg
- E. Mannitol (Correct Answer)
Sepsis-induced organ dysfunction management Explanation: ***Mannitol***
- The patient presents with classic signs of **epidural hematoma** (lucid interval, ipsilateral pupillary dilation, contralateral hemiparesis), and the CT scan confirms a large, biconvex hemorrhage compressing the brain.
- **Mannitol** is an osmotic diuretic used to rapidly **reduce intracranial pressure (ICP)** by drawing water from the brain into the vasculature, which can be life-saving in cases of acute brain herniation.
*Placement of a ventriculoperitoneal (VP) shunt*
- A VP shunt is used for long-term management of **hydrocephalus** due to impaired CSF absorption or flow, not for acute, traumatic hemorrhage and mass effect.
- Placing a shunt would not address the immediate, life-threatening mass effect from the epidural hematoma.
*Acetazolamide*
- **Acetazolamide** is a carbonic anhydrase inhibitor that reduces CSF production, primarily used for conditions like chronic **idiopathic intracranial hypertension** (pseudotumor cerebri) or hydrocephalus.
- It is not an effective treatment for the rapid reduction of ICP in the setting of acute intracranial hemorrhage and mass effect.
*Placing the head of the bed at 0 degrees*
- Keeping the head of the bed flat (at 0 degrees) is generally discouraged in patients with **elevated ICP** as it can worsen cerebral venous outflow and increase ICP.
- Elevating the head of the bed to **30 degrees** is standard practice to promote venous drainage and reduce ICP.
*Maintain a PaCO2 of 24 mm Hg*
- While **hyperventilation** to lower PaCO2 can cause cerebral vasoconstriction and reduce ICP, maintaining a PaCO2 as low as 24 mm Hg (severe hyperventilation) is typically reserved for **brief periods** in severe, refractory ICP elevation.
- Prolonged severe hyperventilation can lead to **cerebral ischemia** due to excessive vasoconstriction and is generally not the first-line or sustained management strategy.
Sepsis-induced organ dysfunction management US Medical PG Question 8: A 26-year-old G1P0 woman at 32-weeks gestation presents for follow-up ultrasound. She was diagnosed with gestational diabetes during her second trimester, but admits to poor glucose control and non-adherence to insulin therapy. Fetal ultrasound reveals an asymmetric, enlarged interventricular septum, left ventricular outflow tract obstruction, and significantly reduced ejection fraction. Which of the following is the most appropriate step in management after delivery?
- A. Medical management (Correct Answer)
- B. Cardiac catheterization
- C. Cardiac magnetic resonance imaging
- D. Chest radiograph
- E. Immediate surgical intervention
Sepsis-induced organ dysfunction management Explanation: ***Medical management***
- Asymmetric interventricular septal hypertrophy in infants of diabetic mothers is a transient phenomenon, primarily managed with **beta-blockers** to improve ventricular outflow.
- The condition typically **resolves spontaneously** within weeks to months as the infant's heart adapts to the extra-uterine environment and insulin levels normalize.
*Cardiac catheterization*
- This is an **invasive procedure** used primarily for diagnostic purposes or for certain interventional treatments, not typically the first-line for transient septal hypertrophy.
- It would carry unnecessary risks for an infant with a condition that is likely to resolve with medical management.
*Cardiac magnetic resonance imaging*
- While it provides detailed anatomical and functional information, **CMR is not usually indicated** for initial management of this specific condition in neonates.
- An echocardiogram has already provided sufficient diagnostic information to guide initial therapy.
*Chest radiograph*
- A chest radiograph provides information about **lung fields and heart size/shape**, but it offers very limited detail regarding specific cardiac structural abnormalities or function.
- It would not be helpful for characterizing the interventricular septum or ventricular outflow tract.
*Immediate surgical intervention*
- **Surgical myectomy** is reserved for severe, persistent left ventricular outflow tract obstruction that is *unresponsive* to maximal medical therapy and is causing significant symptoms or hemodynamic compromise.
- Given the transient nature of the condition associated with maternal diabetes, immediate surgery would be premature and overly aggressive.
Sepsis-induced organ dysfunction management US Medical PG Question 9: A 38-year-old previously healthy woman develops septic shock from necrotizing fasciitis of the lower extremity. Despite three debridements, broad-spectrum antibiotics (vancomycin, meropenem, clindamycin), IVIG, and aggressive critical care support, she develops refractory shock requiring norepinephrine 1.2 mcg/kg/min, vasopressin 0.04 units/min, and epinephrine 0.1 mcg/kg/min. Lactate is 15 mmol/L. Surgical team recommends hemipelvectomy as last option for source control. Family is devastated. ICU team notes SOFA score of 18. Synthesize an approach to management and decision-making.
- A. Transfer to ECMO center for consideration of VA-ECMO as bridge to hemipelvectomy
- B. Multidisciplinary meeting with surgery, ICU, palliative care, and family to discuss realistic outcomes, quality of life, and patient values before decision (Correct Answer)
- C. Continue medical management for 24 hours and proceed with hemipelvectomy only if shock improves
- D. Decline surgery based on futility given SOFA score >15 and initiate comfort care
- E. Proceed with hemipelvectomy immediately as only chance for survival with informed consent from family
Sepsis-induced organ dysfunction management Explanation: ***Multidisciplinary meeting with surgery, ICU, palliative care, and family to discuss realistic outcomes, quality of life, and patient values before decision***
- In high-acuity cases with refractory shock and high **SOFA scores (>15)**, shared decision-making is essential to align surgical intervention with the patient’s **goals of care**.
- This approach ensures that the **prognosis**, which carries a high risk of mortality and morbidity from **hemipelvectomy**, is transparently communicated by the entire medical team.
*Transfer to ECMO center for consideration of VA-ECMO as bridge to hemipelvectomy*
- **VA-ECMO** is generally not indicated in septic shock with refractory vasoplegia and severe multi-organ failure as it doesn't solve the **source control** issue.
- The logistics and physiological stress of a transfer in the setting of **1.2 mcg/kg/min norepinephrine** would be highly unstable and likely fatal.
*Continue medical management for 24 hours and proceed with hemipelvectomy only if shock improves*
- Delaying source control in **necrotizing fasciitis** while shock is worsening usually leads to death, as medical management alone cannot overcome the focus of infection.
- Waiting for improvement in the setting of a **lactate of 15 mmol/L** and triple vasopressors is unrealistic without definitive surgical intervention.
*Decline surgery based on futility given SOFA score >15 and initiate comfort care*
- While the **SOFA score** indicates a very high mortality risk, unilateral physician declaration of **medical futility** is ethically complex and can damage family trust.
- Comfort care should remain a possibility, but first requires a thorough **interdisciplinary discussion** to ensure legal and ethical standards are met.
*Proceed with hemipelvectomy immediately as only chance for survival with informed consent from family*
- Performing such a **mutilating surgery** without a detailed discussion of the expected **quality of life** and long-term functional loss is poor surgical practice.
- Immediate surgery without addressing the massive **operative mortality** risk ignores the patient's potential preference for a dignified death over a futile procedure.
Sepsis-induced organ dysfunction management US Medical PG Question 10: A 52-year-old woman with septic shock from intra-abdominal infection undergoes emergency exploratory laparotomy for perforated diverticulitis with fecal peritonitis. Surgery reveals extensive contamination requiring damage control approach. Postoperatively, she requires norepinephrine 0.8 mcg/kg/min plus vasopressin 0.04 units/min, has lactate of 8.5 mmol/L, temperature 35.2°C, INR 2.8, pH 7.18, and base deficit -12. Planned return to OR is in 48 hours. Evaluate the priority interventions to optimize outcome.
- A. Immediate return to OR for definitive repair and anastomosis
- B. Start therapeutic hypothermia and delay reoperation until hemodynamically stable off vasopressors
- C. Initiate high-dose vasopressors to maintain MAP >75 mmHg and early enteral nutrition
- D. Administer massive transfusion protocol and emergency re-exploration within 6 hours
- E. Aggressive rewarming, correction of coagulopathy, ongoing resuscitation, and source control at planned reoperation (Correct Answer)
Sepsis-induced organ dysfunction management Explanation: ***Aggressive rewarming, correction of coagulopathy, ongoing resuscitation, and source control at planned reoperation***
- This patient presents with the **lethal triad** (coagulopathy, acidosis, and hypothermia) in the setting of **septic shock**, necessitating physiologic stabilization before definitive surgery.
- The gold standard for **damage control** is to stabilize the patient in the ICU by correcting **base deficit**, improving **lactate clearance**, and restoring normal temperature and coagulation parameters.
*Immediate return to OR for definitive repair and anastomosis*
- Attempting **definitive repair** or anastomosis in an unstable patient with fecal peritonitis and high-dose **vasopressor requirements** carries a prohibited risk of dehiscence and death.
- Surgery should be limited to **staged re-intervention** only after the metabolic and physiologic insults have been partially reversed.
*Start therapeutic hypothermia and delay reoperation until hemodynamically stable off vasopressors*
- **Hypothermia** is a component of the lethal triad that worsens **coagulopathy** by inhibiting the clotting cascade; metabolic rewarming is required, not cooling.
- While stability is the goal, waiting to be completely off vasopressors might dangerously delay **source control** if the infection is driving the shock.
*Initiate high-dose vasopressors to maintain MAP >75 mmHg and early enteral nutrition*
- Focus should be on **volume resuscitation** and reversing tissue hypoxia (lactate) rather than solely escalating vasopressors, which can cause **mesenteric ischemia**.
- **Early enteral nutrition** is contraindicated in the immediate postoperative phase of an open abdomen with significant **hemodynamic instability** and high pressor requirements.
*Administer massive transfusion protocol and emergency re-exploration within 6 hours*
- **Massive transfusion protocol** is typically reserved for active, uncontrolled hemorrhage, whereas this patient primarily requires reversal of **septic shock** and metabolic derangements.
- **Re-exploration within 6 hours** is too early for a damage control patient who has not yet been adequately rewarmed or had their **acidosis** corrected.
More Sepsis-induced organ dysfunction management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.