Fluid resuscitation strategies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fluid resuscitation strategies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fluid resuscitation strategies US Medical PG Question 1: A 61-year-old female with congestive heart failure and type 2 diabetes is brought to the emergency room by her husband because of an altered mental status. He states he normally helps her be compliant with her medications, but he had been away for several days. On physical exam, her temperature is 37.2 C, BP 85/55, and HR 130. Serum glucose is 500 mg/dL. Which of the following is the first step in the management of this patient?
- A. IV ½ NS
- B. IV insulin
- C. Subcutaneous insulin injection
- D. IV NS (Correct Answer)
- E. IV D5W
Fluid resuscitation strategies Explanation: ***IV NS***
- The patient presents with **hypotension (85/55 mmHg)** and **tachycardia (130 bpm)**, indicating significant **volume depletion** despite a history of congestive heart failure.
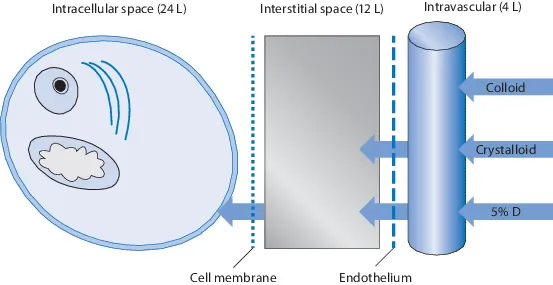
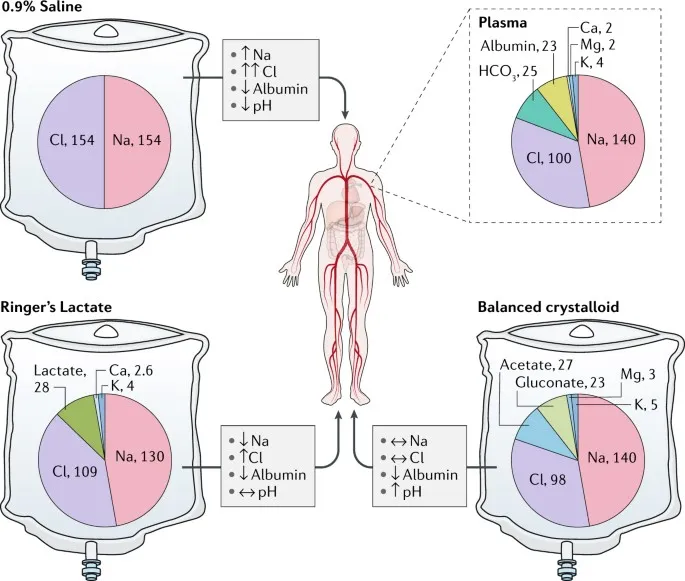
- **Isotonic intravenous fluids (e.g., normal saline)** are crucial in the initial management of **diabetic ketoacidosis (DKA)** or **hyperosmolar hyperglycemic state (HHS)** to restore intravascular volume and improve tissue perfusion.
*IV ½ NS*
- **Hypotonic solutions** such as IV ½ NS are typically used later in DKA/HHS management, once the patient's **hemodynamic stability** has been achieved and serum sodium levels are stable or elevated.
- Administering hypotonic fluids to an already **hypotensive and volume-depleted patient** could worsen hypotension and potentially lead to cerebral edema if not carefully monitored.
*IV insulin*
- While insulin is essential for correcting hyperglycemia, it is administered **after or concurrently with fluid resuscitation** to avoid worsening hypovolemia as it drives glucose and potassium into cells, potentially causing **hypokalemia** and further **hemoconcentration**.
- **Fluid resuscitation** should always precede or be initiated simultaneously with insulin therapy, especially in cases of hemodynamic instability.
*Subcutaneous insulin injection*
- **Subcutaneous insulin** is not appropriate for initial management in this critically ill patient due to its **slower onset of action** and potentially **erratic absorption** in hypotensive and poorly perfused states.
- **Intravenous insulin** is preferred in DKA/HHS for its rapid, titratable effect.
*IV D5W*
- **Dextrose 5% in water (D5W)** is a hypotonic solution primarily used when **blood glucose levels fall below 250 mg/dL** during DKA/HHS treatment to prevent hypoglycemia.
- Administering D5W in a patient with a **serum glucose of 500 mg/dL** would further elevate blood sugar and worsen the hyperosmolar state.
Fluid resuscitation strategies US Medical PG Question 2: A 50-year-old man with a history of stage 4 kidney disease was admitted to the hospital for an elective hemicolectomy. His past medical history is significant for severe diverticulitis. After the procedure he becomes septic and was placed on broad spectrum antibiotics. On morning rounds, he appear weak and complains of fatigue and nausea. His words are soft and he has difficulty answering questions. His temperature is 38.9°C (102.1°F), heart rate is 110/min, respiratory rate is 15/min, blood pressure 90/65 mm Hg, and saturation is 89% on room air. On physical exam, his mental status appears altered. He has a bruise on his left arm that spontaneously appeared overnight. His cardiac exam is positive for a weak friction rub. Blood specimens are collected and sent for evaluation. An ECG is performed (see image). What therapy will this patient most likely receive next?
- A. Send the patient for hemodialysis (Correct Answer)
- B. Perform a STAT pericardiocentesis
- C. Prepare the patient for renal transplant
- D. Treat the patient with aspirin
- E. Treat the patient with cyclophosphamide and prednisone
Fluid resuscitation strategies Explanation: ***Send the patient for hemodialysis***
- This patient presents with symptoms of **uremic encephalopathy** and **uremic pericarditis** in the context of **stage 4 kidney disease**. The altered mental status, weakness, fatigue, nausea, and the development of a bruise (which could indicate uremic coagulopathy) are suggestive of severe uremia. The ECG shows widespread **ST elevation and PR depression**, particularly noticeable in leads like II, V2-V6, which is a classic finding for pericarditis. The **weak friction rub** confirms this clinical suspicion. Hemodialysis is crucial to rapidly remove uremic toxins and resolve both uremic encephalopathy and pericarditis.
- The ECG findings, including diffuse **ST elevation** with **PR depression**, are characteristic of **pericarditis**. In a patient with end-stage renal disease, **uremia** is a common cause of pericarditis, which can be life-threatening if not promptly treated with dialysis.
*Perform a STAT pericardiocentesis*
- While the patient has pericarditis, there are no immediate signs of **cardiac tamponade**, such as muffled heart sounds, jugular venous distension, or pulsus paradoxus, that would necessitate an emergency pericardiocentesis.
- The primary treatment for **uremic pericarditis** is typically **hemodialysis** to resolve the underlying uremic state, not direct fluid removal unless tamponade is present.
*Prepare the patient for renal transplant*
- **Renal transplant** is a long-term solution for end-stage renal disease, but it is not an acute intervention for immediate life-threatening uremic complications like uremic pericarditis and encephalopathy.
- The patient needs urgent stabilization and treatment of his current acute medical issues before transplant consideration.
*Treat the patient with aspirin*
- While aspirin can be used for some forms of pericarditis, it is generally **contraindicated** in patients with **uremic pericarditis** due to the increased risk of **gastric bleeding** and potential exacerbation of uremic coagulopathy.
- The primary treatment for uremic pericarditis is **dialysis**, not anti-inflammatory medications, as the inflammation is driven by uremic toxins.
*Treat the patient with cyclophosphamide and prednisone*
- **Immunosuppressants** like cyclophosphamide and prednisone are used for autoimmune or inflammatory conditions causing pericarditis, such as systemic lupus erythematosus.
- This patient's pericarditis is clearly linked to **uremia** from kidney disease, not an autoimmune condition, making immunosuppressive therapy inappropriate and potentially harmful.
Fluid resuscitation strategies US Medical PG Question 3: A 37-year-old man is brought to the emergency department by ambulance after a motor vehicle accident. He suffered multiple deep lacerations and experienced significant blood loss during transport. In the emergency department, his temperature is 98.6°F (37°C), blood pressure is 102/68 mmHg, pulse is 112/min, and respirations are 22/min. His lacerations are sutured and he is given 2 liters of saline by large bore intravenous lines. Which of the following changes will occur in this patient's cardiac physiology due to this intervention?
- A. Increased cardiac output and unchanged right atrial pressure
- B. Decreased cardiac output and increased right atrial pressure
- C. Increased cardiac output and decreased right atrial pressure
- D. Increased cardiac output and increased right atrial pressure (Correct Answer)
- E. Decreased cardiac output and decreased right atrial pressure
Fluid resuscitation strategies Explanation: ***Increased cardiac output and increased right atrial pressure***
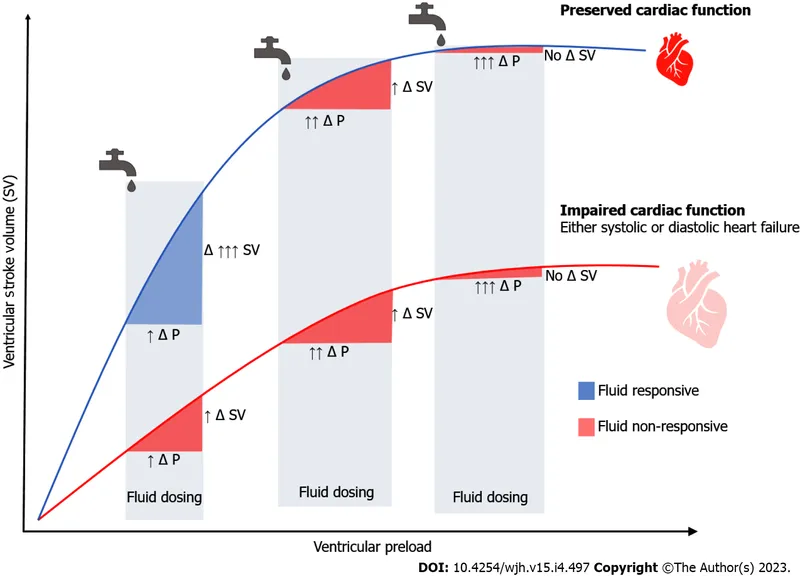
- The patient experienced significant blood loss, leading to a **decreased preload** and subsequent **reduced cardiac output**. Volume resuscitation with saline directly increases the **intravascular volume** which bolsters **venous return** and **right atrial pressure**.
- According to the **Frank-Starling mechanism**, increased right atrial pressure (a measure of preload) results in an increase in ventricular stretch and a more forceful contraction, thereby increasing **stroke volume** and **cardiac output**.
*Increased cardiac output and unchanged right atrial pressure*
- While fluid administration will increase **cardiac output** by improving preload, it will also directly lead to an increase in **right atrial pressure** due to the augmented venous return.
- An unchanged right atrial pressure would imply no significant increase in central venous volume, which contradicts the effect of a large volume fluid resuscitation.
*Decreased cardiac output and increased right atrial pressure*
- This scenario is unlikely because increasing **intravascular volume** through fluid resuscitation typically aims to raise **cardiac output** by optimizing preload, not decrease it.
- A decrease in cardiac output despite increased right atrial pressure could indicate **cardiac pump failure**, which is not suggested by the clinical picture of hypovolemic shock treated with fluids.
*Increased cardiac output and decreased right atrial pressure*
- An increase in **cardiac output** as a result of fluid resuscitation is expected, but a **decreased right atrial pressure** would contradict the mechanism of increased venous return and volume expansion.
- Decreased right atrial pressure would typically indicate ongoing volume loss or inadequate fluid resuscitation to restore central venous volume.
*Decreased cardiac output and decreased right atrial pressure*
- Both decreasing **cardiac output** and decreasing **right atrial pressure** indicate a worsening state of **hypovolemia** or an inadequate response to fluid resuscitation.
- The administration of 2 liters of saline is intended to correct the hypovolemia and improve cardiodynamics, not to worsen them.
Fluid resuscitation strategies US Medical PG Question 4: A 53-year-old diabetic man with cellulitis of the right lower limb presents to the emergency department because of symptoms of fever and chills. His pulse is 122/min, the blood pressure is 76/50 mm Hg, the respirations are 26/min, and the temperature is 40.0°C (104.0°F). His urine output is < 0.5mL/kg/h. He has warm peripheral extremities. The hemodynamic status of the patient is not improving in spite of the initiation of adequate fluid resuscitation. He is admitted to the hospital. Which of the following is the most likely laboratory profile?
- A. WBC count: 11,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 0.9 mmol/L
- B. WBC count: 1234/mm3; high CVP; blood culture: gram-negative bacteremia; blood lactate level: 1.6 mmol/L
- C. WBC count: 16,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 2.2 mmol/L (Correct Answer)
- D. WBC count: 6670/mm3; low CVP; blood culture: gram-positive bacteremia; blood lactate level: 1.1 mmol/L
- E. WBC count: 8880/mm3; high CVP; blood culture: gram-positive bacteremia; blood lactate level: 2.1 mmol/L
Fluid resuscitation strategies Explanation: ***WBC count: 16,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 2.2 mmol/L***
- This profile aligns with **septic shock** driven by gram-negative bacteria, presenting with **tachycardia**, **hypotension**, **fever**, and **poor urine output** despite fluid resuscitation.
- A **high WBC count** (leukocytosis), **low CVP** (due to vasodilation and relative hypovolemia), **gram-negative bacteremia** (common in severe sepsis), and **elevated lactate** (indicating tissue hypoperfusion) are characteristic findings.
*WBC count: 11,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 0.9 mmol/L*
- While most components suggest sepsis (WBC count and low CVP), a **lactate level of 0.9 mmol/L** is within the normal range, contradicting the severe hypoperfusion and shock observed in the patient.
- The patient's presentation with **hypotension** unresponsive to fluids and **oliguria** strongly indicates significant tissue hypoperfusion, which would typically result in a higher lactate.
*WBC count: 1234/mm3; high CVP; blood culture: gram-negative bacteremia; blood lactate level: 1.6 mmol/L*
- A **WBC count of 1234/mm3 (leukopenia)** is an atypical response for severe infection and sepsis; often, sepsis presents with leukocytosis.
- A **high CVP** indicates fluid overload or cardiac dysfunction, which is not consistent with the initial low blood pressure and the need for fluid resuscitation seen in distributive shock.
*WBC count: 6670/mm3; low central venous pressure (CVP); blood culture: gram-positive bacteremia; blood lactate level: 1.1 mmol/L*
- A **WBC count of 6670/mm3** is within the normal range and does not reflect an adequate inflammatory response to severe infection and shock.
- A **normal lactate level (1.1 mmol/L)** does not support the clinical picture of shock and tissue hypoperfusion despite the presence of gram-positive bacteremia.
*WBC count: 8880/mm3; high CVP; blood culture: gram-positive bacteremia; blood lactate level: 2.1 mmol/L*
- A **WBC count of 8880/mm3** is normal, which is unlikely in a severe sepsis presentation.
- A **high CVP** is not consistent with the distributive shock state where there is often relative hypovolemia and vasodilation leading to low CVP.
Fluid resuscitation strategies US Medical PG Question 5: Which of the following physiologic changes decreases pulmonary vascular resistance (PVR)?
- A. Inhaling the inspiratory reserve volume (IRV)
- B. Exhaling the entire vital capacity (VC)
- C. Exhaling the expiratory reserve volume (ERV)
- D. Breath holding maneuver at functional residual capacity (FRC)
- E. Inhaling the entire vital capacity (VC) (Correct Answer)
Fluid resuscitation strategies Explanation: ***Inhaling the entire vital capacity (VC)***
- As lung volume increases from FRC to TLC (which includes inhaling the entire VC), alveolar vessels are **stretched open**, and extra-alveolar vessels are **pulled open** by the increased radial traction, leading to a decrease in PVR.
- This **maximizes the cross-sectional area** of the pulmonary vascular bed, lowering resistance.
*Inhaling the inspiratory reserve volume (IRV)*
- While inhaling IRV increases lung volume, it's not the maximal inspiration of the entire VC where **PVR is typically at its lowest**.
- PVR continues to decrease as lung volume approaches total lung capacity (TLC).
*Exhaling the entire vital capacity (VC)*
- Exhaling the entire vital capacity leads to very low lung volumes, where PVR significantly **increases**.
- At low lung volumes, **alveolar vessels become compressed** and extra-alveolar vessels **narrow**, increasing resistance.
*Exhaling the expiratory reserve volume (ERV)*
- Exhaling the ERV results in a lung volume below FRC, which causes a **marked increase in PVR**.
- This is due to the **compression of alveolar vessels** and decreased radial traction on extra-alveolar vessels.
*Breath holding maneuver at functional residual capacity (FRC)*
- At FRC, the PVR is at an **intermediate level**, not its lowest.
- This is the point where the opposing forces affecting alveolar and extra-alveolar vessels are somewhat balanced, but not optimized for minimal resistance.
Fluid resuscitation strategies US Medical PG Question 6: A 27-year-old man is brought to the emergency department 30 minutes after being shot in the abdomen during a violent altercation. His temperature is 36.5°C (97.7°F), pulse is 118/min and regular, and blood pressure is 88/65 mm Hg. Examination shows cool extremities. Abdominal examination shows a 2.5-cm entrance wound in the left upper quadrant at the midclavicular line, below the left costal margin. Focused ultrasound shows free fluid in the left upper quadrant. Which of the following sets of hemodynamic changes is most likely in this patient?
Cardiac output (CO) | Pulmonary capillary wedge pressure (PCWP) | Systemic vascular resistance (SVR) | Central venous pressure (CVP)
- A. ↑ ↓ ↓ ↓
- B. ↓ ↓ ↑ ↑
- C. ↓ ↓ ↓ ↓
- D. ↓ ↓ ↑ ↓ (Correct Answer)
- E. ↓ ↑ ↑ ↑
Fluid resuscitation strategies Explanation: ***↓ ↓ ↑ ↓***
- This patient is in **hypovolemic shock** due to hemorrhage, leading to decreased **cardiac output (CO)** and **pulmonary capillary wedge pressure (PCWP)** due to reduced preload.
- The body compensates for hypovolemia by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, while **central venous pressure (CVP)** decreases due to the depleted blood volume.
*↑ ↓ ↓ ↓*
- An increased **cardiac output** is inconsistent with hypovolemic shock, where the heart's ability to pump blood is compromised by a lack of circulating volume.
- While **PCWP**, **SVR**, and **CVP** decreasing could be seen in some forms of shock, the elevated CO rules out hypovolemic shock.
*↓ ↓ ↑ ↑*
- An elevated **central venous pressure (CVP)** is inconsistent with hypovolemic shock, as CVP reflects right atrial pressure and would be low due to decreased blood volume.
- While other parameters such as **CO** and **PCWP** decreasing and **SVR** increasing can be seen in hypovolemic shock, the increased CVP suggests a different hemodynamic state, like cardiogenic shock.
*↓ ↓ ↓ ↓*
- A decrease in **systemic vascular resistance (SVR)** is characteristic of **distributive shock** (e.g., septic or neurogenic shock), not hypovolemic shock, where compensatory vasoconstriction would lead to increased SVR.
- While **CO**, **PCWP**, and **CVP** would decrease due to overall poor perfusion, the SVR response differentiates it from hypovolemic shock.
*↓ ↑ ↑ ↑*
- An elevated **pulmonary capillary wedge pressure (PCWP)** and **central venous pressure (CVP)** indicate increased fluid volume or cardiac dysfunction, which is contrary to the reduced preload seen in hypovolemic shock.
- While **cardiac output (CO)** may decrease in cardiogenic shock, the other elevated pressures point away from a primary hypovolemic cause.
Fluid resuscitation strategies US Medical PG Question 7: A 57-year-old man is admitted to the burn unit after he was brought to the emergency room following an accidental fire in his house. His past medical history is unknown due to his current clinical condition. Currently, his blood pressure is 75/40 mmHg, pulse rate is 140/min, and respiratory rate is 17/min. The patient is subsequently intubated and started on aggressive fluid resuscitation. A Swan-Ganz catheter is inserted to clarify his volume status. Which of the following hemodynamic parameters would you expect to see in this patient?
- A. Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
- B. Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔
- C. Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔
- D. Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓ (Correct Answer)
- E. Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔
Fluid resuscitation strategies Explanation: ***Cardiac output: ↓, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↓***
- The patient's **hypotension (75/40 mmHg)** and **tachycardia (140/min)**, combined with severe burns, indicate **hypovolemic shock** due to massive fluid loss from damaged capillaries.
- In response to decreased cardiac output and hypovolemia, the body compensates by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, and **pulmonary artery wedge pressure (PAWP)** will be low due to reduced intravascular volume.
*Cardiac output: ↓, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This option incorrectly suggests that systemic vascular resistance and pulmonary artery wedge pressure would be normal, which is inconsistent with **hypovolemic shock**.
- In shock, the body's compensatory mechanisms would lead to significant changes in SVR and PAWP, not maintain them at baseline.
*Cardiac output: ↑, systemic vascular resistance: ↑, pulmonary artery wedge pressure: ↔*
- Increased cardiac output is usually seen in **distributive shock** (e.g., septic shock) where vasodilation leads to reduced SVR, not increased SVR as suggested here.
- An elevated SVR coupled with an increased cardiac output would typically result in a higher blood pressure unless there is a compensatory drop in other parameters.
*Cardiac output: ↑, systemic vascular resistance: ↓, pulmonary artery wedge pressure: ↔*
- This pattern (high cardiac output, low SVR) is characteristic of **distributive shock**, such as **septic shock** or anaphylactic shock, rather than the hypovolemic shock expected in a burn patient.
- Severe burns primarily cause massive fluid shifts, leading to hypovolemia and a reduced cardiac output, not an elevated one.
*Cardiac output: ↔, systemic vascular resistance: ↔, pulmonary artery wedge pressure: ↔*
- This scenario represents **normal hemodynamic parameters**, which would not be expected in a patient experiencing severe shock from extensive burns.
- The patient's clinical presentation (hypotension, tachycardia) clearly indicates a state of hemodynamic instability.
Fluid resuscitation strategies US Medical PG Question 8: A 17-year-old previously healthy, athletic male suddenly falls unconscious while playing soccer. His athletic trainer comes to his aid and notes that he is pulseless. He begins performing CPR on the patient until the ambulance arrives but the teenager is pronounced dead when the paramedics arrived. Upon investigation of his primary care physician's office notes, it was found that the child had a recognized murmur that was ruled to be "benign." Which of the following conditions would have increased the intensity of the murmur?
- A. Inspiration
- B. Placing the patient in a squatting position
- C. Valsalva (Correct Answer)
- D. Passive leg raise
- E. Handgrip
Fluid resuscitation strategies Explanation: ***Valsalva***
- The patient's sudden death after collapsing during soccer, coupled with a previously noted "benign" murmur, strongly suggests **hypertrophic obstructive cardiomyopathy (HOCM)**, which is a common cause of sudden cardiac death in young athletes. The **Valsalva maneuver** decreases preload and left ventricular volume, thereby **increasing the left ventricular outflow tract (LVOT) obstruction** and hence the intensity of the HOCM murmur.
- This maneuver reduces venous return to the heart, leading to reduced ventricular filling and decreased stroke volume. This exacerbates the obstruction in HOCM, making the murmur louder.
*Inspiration*
- **Inspiration** typically **increases venous return to the right side of the heart**, which would generally intensify right-sided murmurs (e.g., tricuspid regurgitation).
- It would have **minimal effect or slightly decrease** the intensity of a left-sided obstructive murmur like that in HOCM, as it does not directly increase the LVOT obstruction.
*Placing the patient in a squatting position*
- Squatting increases both **preload** and **afterload** by increasing systemic vascular resistance and venous return.
- This increase in ventricular volume would **reduce the outflow tract obstruction** in HOCM, thereby **decreasing the intensity of the murmur**.
*Passive leg raise*
- A **passive leg raise** increases **venous return** and thus **preload**, leading to increased ventricular filling.
- Similar to squatting, this increased left ventricular volume would **reduce the left ventricular outflow tract obstruction** associated with HOCM, thereby **decreasing the murmur's intensity**.
*Handgrip*
- The **handgrip maneuver** primarily **increases afterload** and, to some extent, preload by increasing systemic vascular resistance.
- While it can increase the intensity of murmurs like mitral regurgitation and ventricular septal defect, it would generally **decrease or have no significant effect** on the murmur of HOCM due to the increased ventricular volume reducing the outflow obstruction.
Fluid resuscitation strategies US Medical PG Question 9: A 35-year-old woman is brought to the emergency department 45 minutes after being rescued from a house fire. On arrival, she appears confused and has shortness of breath. The patient is 165 cm (5 ft 5 in) tall and weighs 55 kg (121 lb); BMI is 20 kg/m2. Her pulse is 125/min, respirations are 29/min, and blood pressure is 105/65 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. Examination shows second and third-degree burns over the anterior surfaces of the chest and abdomen, and the anterior surface of the upper extremities. There is black debris in the mouth and nose. There are coarse breath sounds over the lung bases. Cardiac examination shows no murmurs, rubs, or gallop. Femoral and pedal pulses are palpable bilaterally. Which of the following is the most appropriate fluid regimen for this patient according to the Parkland formula?
- A. Administer 4 liters of intravenous colloids over the next 8 hours
- B. Administer 5 liters of intravenous colloids over the next 6 hours
- C. Administer 5 liters of intravenous crystalloids over the next 6 hours
- D. Administer 8 liters of intravenous colloids over the next 12 hours
- E. Administer 6 liters of intravenous crystalloids over the next 24 hours (Correct Answer)
Fluid resuscitation strategies Explanation: ***Administer 6 liters of intravenous crystalloids over the next 24 hours***
- The **Parkland formula** is 4 mL × weight (kg) × %TBSA burn. The patient's weight is 55 kg. The burns cover the anterior chest (9%), anterior abdomen (9%), and anterior surfaces of both upper extremities (4.5% + 4.5% = 9%), totaling **27% TBSA**.
- Calculation: 4 mL × 55 kg × 27% = **5,940 mL ≈ 6 liters**. Half is given in the first 8 hours (approximately 3 L), and the remaining half over the next 16 hours (approximately 3 L). Total fluid in 24 hours is approximately **6 liters of crystalloids**.
*Administer 4 liters of intravenous colloids over the next 8 hours*
- The Parkland formula primarily uses **crystalloids** (lactated Ringer's solution) for initial fluid resuscitation in burn patients, not colloids.
- Administering only 4 liters would be insufficient given the patient's 27% TBSA burn, and colloids are not first-line.
*Administer 5 liters of intravenous colloids over the next 6 hours*
- **Colloids** are not the first-line fluid for initial burn resuscitation under the Parkland formula; crystalloids are used.
- The timing of 6 hours does not align with the Parkland formula's 24-hour resuscitation period (half in first 8 hours, half in next 16 hours).
*Administer 5 liters of intravenous crystalloids over the next 6 hours*
- While **crystalloids** are appropriate, 5 liters over 6 hours represents an inappropriately rapid infusion rate that does not follow the Parkland formula timing.
- The first 8 hours should receive approximately 3 liters, not 5 liters over 6 hours, which could lead to complications such as **pulmonary edema or compartment syndrome**.
*Administer 8 liters of intravenous colloids over the next 12 hours*
- This option incorrectly specifies **colloids** instead of crystalloids as the primary fluid for burn resuscitation according to the Parkland formula.
- The volume of 8 liters exceeds the calculated requirement of 6 liters for this patient's 27% TBSA burn.
Fluid resuscitation strategies US Medical PG Question 10: A 7-year-old boy is brought to the emergency room because of severe, acute diarrhea. He is drowsy with a dull, lethargic appearance. He has sunken eyes, poor skin turgor, and dry oral mucous membranes and tongue. He has a rapid, thready pulse with a systolic blood pressure of 60 mm Hg and his respirations are 33/min. His capillary refill time is 6 sec. He has had no urine output for the past 24 hours. Which of the following is the most appropriate next step in treatment?
- A. Start IV fluid resuscitation by administering colloid solutions
- B. Provide oral rehydration therapy to correct dehydration
- C. Give initial IV bolus of 2 L of Ringer’s lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1
- D. Start IV fluid resuscitation with normal saline or Ringer’s lactate, along with monitoring of vitals and urine output (Correct Answer)
- E. Give antidiarrheal drugs
Fluid resuscitation strategies Explanation: ***Start IV fluid resuscitation with normal saline or Ringer's lactate, along with monitoring of vitals and urine output***
- This patient presents with **severe dehydration** and **hypovolemic shock** (lethargy, sunken eyes, poor skin turgor, dry mucous membranes, rapid thready pulse, hypotension [systolic BP 60 mmHg], tachypnea, prolonged capillary refill >5 seconds, and anuria).
- According to **PALS guidelines**, the immediate priority is rapid intravenous administration of **isotonic crystalloids** (normal saline or Ringer's lactate) given as **20 mL/kg boluses** over 5-20 minutes, repeated as needed based on clinical response.
- Close monitoring of vital signs, mental status, perfusion (capillary refill), and urine output is essential to assess response to resuscitation and guide further fluid management.
*Start IV fluid resuscitation by administering colloid solutions*
- While colloids (albumin, synthetic colloids) can expand intravascular volume, **isotonic crystalloids** are preferred for initial resuscitation in severe dehydration per **WHO and PALS guidelines**.
- Crystalloids are equally effective, more readily available, less expensive, and have fewer potential adverse effects compared to colloids in pediatric dehydration.
- There is no proven survival benefit of colloids over crystalloids in this clinical scenario.
*Provide oral rehydration therapy to correct dehydration*
- **Oral rehydration therapy (ORT)** is the appropriate first-line treatment for **mild to moderate dehydration** in children who can tolerate oral intake.
- However, ORT is **contraindicated** in patients with **severe dehydration** or **hypovolemic shock**, particularly those with altered mental status, inability to drink, or hemodynamic instability.
- This patient's drowsiness, hypotension, and signs of shock require immediate IV resuscitation; ORT would be too slow and potentially dangerous.
*Give initial IV bolus of 2 L of Ringer's lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1*
- A 2-liter bolus is **excessive and dangerous** for a 7-year-old child (average weight ~23 kg); the appropriate initial bolus is **20 mL/kg** (~460 mL), which can be repeated based on response.
- The **1:1:1 massive transfusion protocol** (packed RBCs, FFP, platelets) is indicated for **hemorrhagic shock** with significant blood loss, not for hypovolemic shock from dehydration.
- There is no evidence of bleeding or coagulopathy in this patient; blood products are not indicated.
*Give antidiarrheal drugs*
- **Antidiarrheal agents** (loperamide, diphenoxylate) are **contraindicated** in young children with acute infectious diarrhea, as they can prolong illness, increase risk of complications (toxic megacolon, bacterial overgrowth), and mask serious underlying conditions.
- The priority in severe dehydration is **fluid and electrolyte resuscitation**, not stopping the diarrhea.
- The diarrhea typically resolves once the underlying infection is controlled and hydration is restored.
More Fluid resuscitation strategies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.