Early recognition of sepsis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Early recognition of sepsis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Early recognition of sepsis US Medical PG Question 1: A 7-year-old boy is brought to the emergency room because of severe, acute diarrhea. He is drowsy with a dull, lethargic appearance. He has sunken eyes, poor skin turgor, and dry oral mucous membranes and tongue. He has a rapid, thready pulse with a systolic blood pressure of 60 mm Hg and his respirations are 33/min. His capillary refill time is 6 sec. He has had no urine output for the past 24 hours. Which of the following is the most appropriate next step in treatment?
- A. Start IV fluid resuscitation by administering colloid solutions
- B. Provide oral rehydration therapy to correct dehydration
- C. Give initial IV bolus of 2 L of Ringer’s lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1
- D. Start IV fluid resuscitation with normal saline or Ringer’s lactate, along with monitoring of vitals and urine output (Correct Answer)
- E. Give antidiarrheal drugs
Early recognition of sepsis Explanation: ***Start IV fluid resuscitation with normal saline or Ringer's lactate, along with monitoring of vitals and urine output***
- This patient presents with **severe dehydration** and **hypovolemic shock** (lethargy, sunken eyes, poor skin turgor, dry mucous membranes, rapid thready pulse, hypotension [systolic BP 60 mmHg], tachypnea, prolonged capillary refill >5 seconds, and anuria).
- According to **PALS guidelines**, the immediate priority is rapid intravenous administration of **isotonic crystalloids** (normal saline or Ringer's lactate) given as **20 mL/kg boluses** over 5-20 minutes, repeated as needed based on clinical response.
- Close monitoring of vital signs, mental status, perfusion (capillary refill), and urine output is essential to assess response to resuscitation and guide further fluid management.
*Start IV fluid resuscitation by administering colloid solutions*
- While colloids (albumin, synthetic colloids) can expand intravascular volume, **isotonic crystalloids** are preferred for initial resuscitation in severe dehydration per **WHO and PALS guidelines**.
- Crystalloids are equally effective, more readily available, less expensive, and have fewer potential adverse effects compared to colloids in pediatric dehydration.
- There is no proven survival benefit of colloids over crystalloids in this clinical scenario.
*Provide oral rehydration therapy to correct dehydration*
- **Oral rehydration therapy (ORT)** is the appropriate first-line treatment for **mild to moderate dehydration** in children who can tolerate oral intake.
- However, ORT is **contraindicated** in patients with **severe dehydration** or **hypovolemic shock**, particularly those with altered mental status, inability to drink, or hemodynamic instability.
- This patient's drowsiness, hypotension, and signs of shock require immediate IV resuscitation; ORT would be too slow and potentially dangerous.
*Give initial IV bolus of 2 L of Ringer's lactate, followed by packed red cells, fresh frozen plasma, and platelets in a ratio of 1:1:1*
- A 2-liter bolus is **excessive and dangerous** for a 7-year-old child (average weight ~23 kg); the appropriate initial bolus is **20 mL/kg** (~460 mL), which can be repeated based on response.
- The **1:1:1 massive transfusion protocol** (packed RBCs, FFP, platelets) is indicated for **hemorrhagic shock** with significant blood loss, not for hypovolemic shock from dehydration.
- There is no evidence of bleeding or coagulopathy in this patient; blood products are not indicated.
*Give antidiarrheal drugs*
- **Antidiarrheal agents** (loperamide, diphenoxylate) are **contraindicated** in young children with acute infectious diarrhea, as they can prolong illness, increase risk of complications (toxic megacolon, bacterial overgrowth), and mask serious underlying conditions.
- The priority in severe dehydration is **fluid and electrolyte resuscitation**, not stopping the diarrhea.
- The diarrhea typically resolves once the underlying infection is controlled and hydration is restored.
Early recognition of sepsis US Medical PG Question 2: A group of investigators discovers a novel monomeric enzyme that cleaves glutamate-valine bonds in a bacterial exotoxin. The substrate binding site of the enzyme is rich in aspartate. A sample of the enzyme is added to two serum samples containing the bacterial exotoxin. One sample is assigned a test condition while the other is maintained as the control. The averaged results of several trials comparing Vmax and Km between control serum and test serum are shown.
Vmax (μmol/min) Km (mM)
Control serum 13.2 81.2
Test serum 28.8 80.9
Which of the following conditions in the test serum would best explain these findings?
- A. Presence of a reversible competitive inhibitor
- B. Increased exotoxin concentration
- C. Increased enzyme concentration (Correct Answer)
- D. Presence of an irreversible competitive inhibitor
- E. Increased serum pH
Early recognition of sepsis Explanation: ***Increased enzyme concentration***
- An increase in enzyme concentration directly leads to a higher **Vmax** because there are more active sites available to convert substrate into product.
- The **Km** (substrate concentration at half Vmax) remains unchanged as the enzyme's affinity for the substrate is not altered, only the total number of enzyme molecules.
*Presence of a reversible competitive inhibitor*
- A **competitive inhibitor** would increase the **apparent Km** (making it seem like the enzyme has lower affinity for the substrate) because it competes with the substrate for the active site.
- The **Vmax** would remain unchanged, as a sufficiently high substrate concentration can overcome the inhibition.
*Increased exotoxin concentration*
- Increasing the substrate (**exotoxin**) concentration within the range where the enzyme is not saturated would increase the reaction rate up to **Vmax**, but it would not change the intrinsic **Vmax** or **Km** of the enzyme.
- If the enzyme is already saturated, increasing substrate concentration further will not affect the rate.
*Presence of an irreversible competitive inhibitor*
- An **irreversible inhibitor** permanently binds to the enzyme, effectively reducing the concentration of functional enzyme.
- This would lead to a decrease in **Vmax** because fewer enzyme molecules are available for catalysis.
- Note: True competitive inhibitors are reversible; this option tests understanding that irreversible inhibition reduces functional enzyme concentration and thus Vmax.
*Increased serum pH*
- Changing the **pH** away from the enzyme's optimal pH would typically lead to a decrease in enzyme activity, thereby reducing the **Vmax** and potentially altering the **Km** due to changes in enzyme conformation.
- The observed increase in **Vmax** and unchanged **Km** do not align with a deviation from optimal pH.
Early recognition of sepsis US Medical PG Question 3: A 68-year-old woman presents to the hospital for an elective right hemicolectomy. She is independently mobile and does her own shopping. She has had type 2 diabetes mellitus for 20 years, essential hypertension for 15 years, and angina on exertion for 6 years. She has a 30-pack-year history of smoking. The operation was uncomplicated. On post-op day 5, she becomes confused. She has a temperature of 38.5°C (101.3°F), respiratory rate of 28/min, and oxygen saturation of 92% on 2 L of oxygen. She is tachycardic at 118/min and her blood pressure is 110/65 mm Hg. On chest auscultation, she has coarse crackles in the right lung base. Her surgical wound appears to be healing well, and her abdomen is soft and nontender. Which of the following is the most likely diagnosis?
- A. Malignant hyperthermia
- B. Drug-induced fever
- C. Multiple organ dysfunction syndrome
- D. Sepsis (Correct Answer)
- E. Non-infectious systemic inflammatory response syndrome (SIRS)
Early recognition of sepsis Explanation: ***Sepsis***
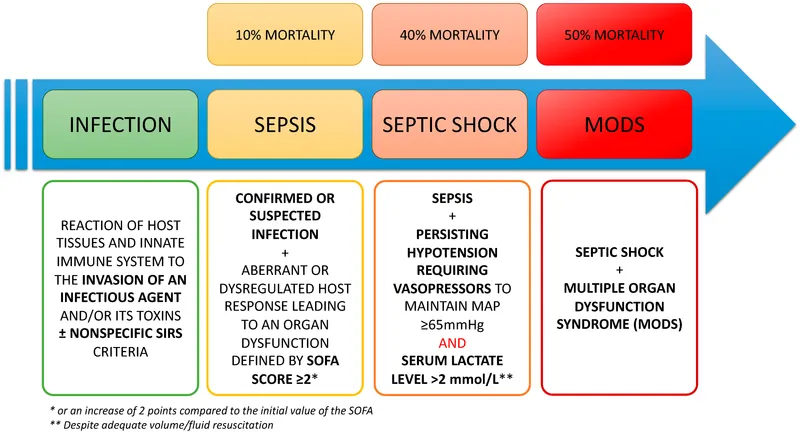
- The patient exhibits several signs of **systemic inflammatory response syndrome (SIRS)** (fever, tachycardia, tachypnea) coupled with evidence of infection (coarse crackles in the lung base suggests **pneumonia**).
- The combination of **SIRS criteria** and a likely infection source in a postoperative patient strongly points to sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection.
*Malignant hyperthermia*
- This is a rare, life-threatening condition typically triggered by **volatile anesthetic agents** or **succinylcholine** during surgery.
- It usually presents **intraoperatively or immediately postoperatively** with rapid onset of hyperthermia, muscle rigidity, and metabolic acidosis, which is not consistent with a presentation on post-op day 5.
*Drug-induced fever*
- While drug-induced fever is possible, particularly in polymedicated patients, it would be a **diagnosis of exclusion** when other more likely causes of fever, such as infection, are present.
- There are no specific clinical features in this case that strongly suggest a drug as the singular cause of fever and the systemic inflammatory response.
*Multiple organ dysfunction syndrome*
- **MODS** is the progressive failure of two or more organ systems and is often a **complication of severe sepsis or septic shock**, rather than an initial diagnosis.
- While the patient is unwell, her current presentation describes a potential precursor (sepsis) rather than established multi-organ dysfunction.
*Non-infectious systemic inflammatory response syndrome (SIRS)*
- SIRS caused by non-infectious etiologies (e.g., pancreatitis, trauma, burns) can occur, but the presence of **localized lung crackles** and a **postoperative fever** makes an infectious etiology much more likely.
- Postoperative SIRS can occur due to surgical stress, but the signs of infection (especially respiratory) shift the diagnosis towards sepsis.
Early recognition of sepsis US Medical PG Question 4: A 72-year-old male is brought from his nursing home to the emergency department for fever, chills, dyspnea, productive cough, and oliguria over the past 72 hours. He was in his normal state of health and slowly developed breathing problems and fever. His past medical history is significant for hepatitis C, hypertension, and hypercholesterolemia. His medications include bisoprolol, hydrochlorothiazide, and atorvastatin. Upon arrival to the ED, his blood pressure is 80/48 mm Hg, pulse is 120/min, a respiratory rate of 28/min, and body temperature of 39.0°C (102.2°F). Physical examination reveals decreased breathing sounds in the base of the left lung, along with increased vocal resonance, and pan-inspiratory crackles. The abdomen is mildly distended with a positive fluid wave. The patient's level of consciousness ranges from disoriented to drowsiness. He is transferred immediately to the ICU where vasoactive support is initiated. Laboratory tests show leukocytosis, neutrophilia with bands. Since admission 6 hours ago, the patient has remained anuric. Which of the following additional findings would you expect in this patient?
- A. Urine sodium > 40 mEq/L
- B. Urinary osmolality > 500 mOsmol/kg
- C. Urinary osmolality < 350 mOsmol/kg
- D. Blood urea nitrogen (BUN):Serum creatinine (Cr) ratio <15:1
- E. Blood urea nitrogen (BUN):Serum creatinine (Cr) ratio > 20:1 (Correct Answer)
Early recognition of sepsis Explanation: ***Blood urea nitrogen (BUN):Serum creatinine (Cr) ratio > 20:1***
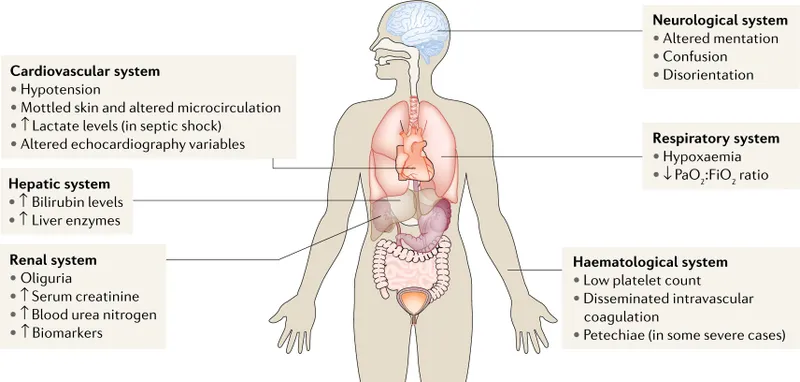
- This patient is presenting with signs of **septic shock** (fever, hypotension, altered mental status, oliguria, leukocytosis) likely due to **pneumonia**. The prolonged hypotension and poor perfusion lead to **prerenal acute kidney injury (AKI)** that may be progressing to **acute tubular necrosis (ATN)**.
- In **prerenal AKI**, reduced renal perfusion leads to increased reabsorption of urea and water in the renal tubules, resulting in a **BUN:creatinine ratio greater than 20:1**. This elevated ratio persists even as the patient transitions to ATN.
- Given **6 hours of anuria** despite vasoactive support, this suggests significant renal injury, but the BUN:Cr ratio remains the most reliable finding at this stage.
*Urine sodium > 40 mEq/L*
- A urine sodium concentration greater than 40 mEq/L is typically seen in **intrinsic AKI** (e.g., acute tubular necrosis), where tubular damage impairs sodium reabsorption.
- While this patient may be developing ATN given the prolonged anuria, in the **early phase** of septic AKI with recent hypotension, the kidneys initially attempt to conserve sodium, resulting in **low urine sodium (<20 mEq/L)**.
*Urinary osmolality > 500 mOsmol/kg*
- A urinary osmolality above 500 mOsmol/kg indicates appropriately concentrated urine, which is a compensatory mechanism in **early prerenal AKI** as the kidneys try to conserve water.
- However, given this patient has been **anuric for 6 hours** despite ICU-level vasoactive support, the kidney injury has likely progressed beyond pure prerenal state. In established ATN, the concentrating ability is impaired, and urinary osmolality would be **closer to isotonic (<350 mOsmol/kg)** rather than highly concentrated.
- The **elevated BUN:Cr ratio** is more reliable in this mixed clinical picture.
*Urinary osmolality < 350 mOsmol/kg*
- A urinary osmolality less than 350 mOsmol/kg indicates inappropriately diluted urine, which is characteristic of **established intrinsic AKI (acute tubular necrosis)**, where the kidney's concentrating ability is impaired.
- While the patient may be progressing toward ATN, the **BUN:Cr ratio elevation** develops earlier and is the most expected finding at this presentation stage.
*Blood urea nitrogen (BUN):Serum creatinine (Cr) ratio <15:1*
- A BUN:creatinine ratio less than 15:1 is typically seen in **intrinsic AKI after several days**, **normal renal function**, or conditions with decreased urea production.
- In this patient with septic shock and acute hypoperfusion leading to AKI, the ratio would be **elevated (>20:1)** due to enhanced urea reabsorption in the setting of decreased renal blood flow.
Early recognition of sepsis US Medical PG Question 5: A 72-year-old man presents to the emergency department after a fall. The patient was found lying down on the floor in his room in his retirement community. The patient has a past medical history of Alzheimer dementia and a prosthetic valve. His current medications include donepezil and warfarin. His temperature is 97.7°F (36.5°C), blood pressure is 85/50 mmHg, pulse is 160/min, respirations are 13/min, and oxygen saturation is 97% on room air. The patient is started on IV fluids and a type and screen is performed. Laboratory values are ordered as seen below.
Hemoglobin: 13 g/dL
Hematocrit: 39%
Leukocyte count: 5,500 cells/mm^3 with normal differential
Platelet count: 225,000/mm^3
INR: 2.5
AST: 10 U/L
ALT: 12 U/L
A chest radiograph and EKG are performed and are within normal limits. A full physical exam is within normal limits. The patient's vitals are repeated. His temperature is 99.5°F (37.5°C), blood pressure is 110/70 mmHg, pulse is 90/min, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. CT scan (Correct Answer)
- B. Urgent blood transfusion
- C. Fresh frozen plasma
- D. Exploratory laparoscopy
- E. Exploratory laparotomy
Early recognition of sepsis Explanation: ***CT scan***
- A patient with a **prosthetic valve** on **warfarin** and a fall is at high risk for **intracranial hemorrhage**, even without focal neurological deficits.
- While initial vitals improved after IV fluids, the mechanism of injury (fall) and medication profile warrant a **CT scan** of the head to rule out serious internal injury, especially given the history of dementia which might mask symptoms.
*Urgent blood transfusion*
- The patient's **hemoglobin (13 g/dL)** and **hematocrit (39%)** are within normal limits, indicating no acute need for blood transfusion due to hemorrhage.
- Transfusions are typically reserved for patients with significant blood loss or severe symptomatic anemia.
*Fresh frozen plasma*
- The patient's **INR of 2.5** is within the therapeutic range for a patient with a prosthetic valve on warfarin.
- There is no evidence of active bleeding or supratherapeutic anticoagulation that would necessitate the administration of **fresh frozen plasma (FFP)** to reverse anticoagulation.
*Exploratory laparoscopy*
- There are no clinical signs or symptoms, such as abdominal pain, distension, or evidence of intra-abdominal bleeding (e.g., declining hemoglobin, peritoneal signs), to suggest an indication for an **exploratory laparoscopy**.
- The patient's physical exam was described as normal.
*Exploratory laparotomy*
- Similar to laparoscopy, there is no clinical evidence of acute abdominal injury or hemorrhage, which would necessitate an **exploratory laparotomy**.
- This invasive procedure is reserved for cases with strong suspicion of significant intra-abdominal pathology or trauma.
Early recognition of sepsis US Medical PG Question 6: A 27-year-old man is brought to the emergency department by emergency medical services. The patient was an unrestrained passenger in a head-on collision that occurred 15 minutes ago and is currently unresponsive. His temperature is 99.5°F (37.5°C), blood pressure is 60/33 mmHg, pulse is 180/min, respirations are 17/min, and oxygen saturation is 95% on room air. A FAST exam demonstrates fluid in Morrison’s pouch. Laboratory values are drawn upon presentation to the ED and sent off. The patient is started on IV fluids and an initial trauma survey is started. Twenty minutes later, his blood pressure is 95/65 mmHg, and his pulse is 110/min. The patient is further stabilized and is scheduled for emergency surgery. Which of the following best represents this patient’s most likely initial laboratory values?
- A. Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3
- B. Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3
- C. Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3
- D. Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3 (Correct Answer)
- E. Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3
Early recognition of sepsis Explanation: ***Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3***
- The patient experienced significant trauma and is experiencing **hemorrhagic shock**, as evidenced by his initial **hypotension** (BP 60/33 mmHg), **tachycardia** (pulse 180/min), and positive **FAST exam** for fluid in Morrison's pouch, indicating intra-abdominal bleeding.
- The initial hemoglobin and hematocrit could be mildly decreased due to acute blood loss, but significant drops are often *not immediately apparent* as plasma volume has not yet moved into the intravascular compartment to dilute the remaining red blood cells. A hemoglobin of 11 g/dL and hematocrit of 33% are consistent with **acute blood loss** before significant hemodilution occurs. MCV of 88 µm^3 is within the normal range for **normocytic anemia** seen in acute hemorrhage.
*Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3*
- While a hemoglobin of 10 g/dL and hematocrit of 30% are consistent with anemia due to blood loss, an **MCV of 110 µm^3** (macrocytic) is not typically seen in acute hemorrhage.
- Macrocytic anemia usually results from conditions like **B12 or folate deficiency**, alcoholism, or liver disease, which are not suggested by the acute traumatic scenario.
*Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3*
- This indicates **polycythemia** (abnormally high red blood cell count), which is the opposite of what would be expected in a patient experiencing acute hemorrhagic shock.
- These values would suggest conditions like **polycythemia vera** or severe dehydration, which are not relevant in this acute trauma setting.
*Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3*
- While a hemoglobin of 7 g/dL and hematocrit of 21% represent significant anemia consistent with major blood loss, these values are typically seen *later* as **hemodilution** occurs, or in cases of chronic blood loss.
- An **MCV of 75 µm^3** (microcytic) is generally indicative of **iron deficiency anemia** or thalassemia, which develops over time and is not characteristic of acute traumatic blood loss.
*Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3*
- These values are within the **normal range** for hemoglobin and hematocrit, which would not be expected in a patient presenting with signs of **hemorrhagic shock** and a positive FAST exam indicating significant internal bleeding.
- This would suggest either very minor blood loss or that the values were taken before any bleeding had occurred or before hemodilution had a chance to manifest.
Early recognition of sepsis US Medical PG Question 7: A previously healthy 17-year-old boy is brought to the emergency department because of fever, nausea, and myalgia for the past day. His temperature is 39.5°C (103.1°F), pulse is 112/min, and blood pressure is 77/55 mm Hg. Physical examination shows scattered petechiae over the anterior chest and abdomen. Blood culture grows an organism on Thayer-Martin agar. Which of the following virulence factors of the causal organism is most likely responsible for the high mortality rate associated with it?
- A. Immunoglobulin A protease
- B. Lipooligosaccharide (Correct Answer)
- C. Toxic shock syndrome toxin-1
- D. Lipoteichoic acid
- E. Erythrogenic exotoxin A
Early recognition of sepsis Explanation: ***Lipooligosaccharide***
- The patient's presentation with **fever**, **hypotension**, and **petechiae**, along with a positive blood culture on Thayer-Martin agar, points to **meningococcemia** caused by *Neisseria meningitidis*.
- **Lipooligosaccharide (LOS)** acts as an **endotoxin**, triggering an excessive inflammatory response that leads to widespread vascular damage, **capillary leakage**, and **septic shock**, accounting for the high mortality.
*Immunoglobulin A protease*
- While *N. meningitidis* produces **IgA protease** to cleave secretory IgA and evade host defenses on mucosal surfaces, this factor is primarily involved in colonization and initial invasion rather than the systemic severity and mortality of septic shock.
- Its role is to help the bacteria **adhere and penetrate** host mucous membranes, but it does not directly cause the shock and petechiae seen in this severe presentation.
*Toxic shock syndrome toxin-1*
- **Toxic shock syndrome toxin-1 (TSST-1)** is a **superantigen** produced by *Staphylococcus aureus* that causes **toxic shock syndrome**, which can present with fever, rash, and hypotension.
- However, the organism grown on **Thayer-Martin agar** is characteristic of *Neisseria meningitidis*, not *Staphylococcus aureus*.
*Lipoteichoic acid*
- **Lipoteichoic acid** is a major component of the cell wall of **Gram-positive bacteria**, acting as a potent proinflammatory molecule and contributing to septic shock in those infections.
- *Neisseria meningitidis* is a **Gram-negative bacterium**, and therefore does not possess lipoteichoic acid.
*Erythrogenic exotoxin A*
- **Erythrogenic exotoxin A** is primarily produced by ***Streptococcus pyogenes*** and is responsible for the characteristic rash of **scarlet fever**.
- While *S. pyogenes* can cause invasive infections, the clinical picture and the specific growth on **Thayer-Martin agar** are not consistent with streptococcal infection.
Early recognition of sepsis US Medical PG Question 8: A 38-year-old previously healthy woman develops septic shock from necrotizing fasciitis of the lower extremity. Despite three debridements, broad-spectrum antibiotics (vancomycin, meropenem, clindamycin), IVIG, and aggressive critical care support, she develops refractory shock requiring norepinephrine 1.2 mcg/kg/min, vasopressin 0.04 units/min, and epinephrine 0.1 mcg/kg/min. Lactate is 15 mmol/L. Surgical team recommends hemipelvectomy as last option for source control. Family is devastated. ICU team notes SOFA score of 18. Synthesize an approach to management and decision-making.
- A. Transfer to ECMO center for consideration of VA-ECMO as bridge to hemipelvectomy
- B. Multidisciplinary meeting with surgery, ICU, palliative care, and family to discuss realistic outcomes, quality of life, and patient values before decision (Correct Answer)
- C. Continue medical management for 24 hours and proceed with hemipelvectomy only if shock improves
- D. Decline surgery based on futility given SOFA score >15 and initiate comfort care
- E. Proceed with hemipelvectomy immediately as only chance for survival with informed consent from family
Early recognition of sepsis Explanation: ***Multidisciplinary meeting with surgery, ICU, palliative care, and family to discuss realistic outcomes, quality of life, and patient values before decision***
- In high-acuity cases with refractory shock and high **SOFA scores (>15)**, shared decision-making is essential to align surgical intervention with the patient’s **goals of care**.
- This approach ensures that the **prognosis**, which carries a high risk of mortality and morbidity from **hemipelvectomy**, is transparently communicated by the entire medical team.
*Transfer to ECMO center for consideration of VA-ECMO as bridge to hemipelvectomy*
- **VA-ECMO** is generally not indicated in septic shock with refractory vasoplegia and severe multi-organ failure as it doesn't solve the **source control** issue.
- The logistics and physiological stress of a transfer in the setting of **1.2 mcg/kg/min norepinephrine** would be highly unstable and likely fatal.
*Continue medical management for 24 hours and proceed with hemipelvectomy only if shock improves*
- Delaying source control in **necrotizing fasciitis** while shock is worsening usually leads to death, as medical management alone cannot overcome the focus of infection.
- Waiting for improvement in the setting of a **lactate of 15 mmol/L** and triple vasopressors is unrealistic without definitive surgical intervention.
*Decline surgery based on futility given SOFA score >15 and initiate comfort care*
- While the **SOFA score** indicates a very high mortality risk, unilateral physician declaration of **medical futility** is ethically complex and can damage family trust.
- Comfort care should remain a possibility, but first requires a thorough **interdisciplinary discussion** to ensure legal and ethical standards are met.
*Proceed with hemipelvectomy immediately as only chance for survival with informed consent from family*
- Performing such a **mutilating surgery** without a detailed discussion of the expected **quality of life** and long-term functional loss is poor surgical practice.
- Immediate surgery without addressing the massive **operative mortality** risk ignores the patient's potential preference for a dignified death over a futile procedure.
Early recognition of sepsis US Medical PG Question 9: A 52-year-old woman with septic shock from intra-abdominal infection undergoes emergency exploratory laparotomy for perforated diverticulitis with fecal peritonitis. Surgery reveals extensive contamination requiring damage control approach. Postoperatively, she requires norepinephrine 0.8 mcg/kg/min plus vasopressin 0.04 units/min, has lactate of 8.5 mmol/L, temperature 35.2°C, INR 2.8, pH 7.18, and base deficit -12. Planned return to OR is in 48 hours. Evaluate the priority interventions to optimize outcome.
- A. Immediate return to OR for definitive repair and anastomosis
- B. Start therapeutic hypothermia and delay reoperation until hemodynamically stable off vasopressors
- C. Initiate high-dose vasopressors to maintain MAP >75 mmHg and early enteral nutrition
- D. Administer massive transfusion protocol and emergency re-exploration within 6 hours
- E. Aggressive rewarming, correction of coagulopathy, ongoing resuscitation, and source control at planned reoperation (Correct Answer)
Early recognition of sepsis Explanation: ***Aggressive rewarming, correction of coagulopathy, ongoing resuscitation, and source control at planned reoperation***
- This patient presents with the **lethal triad** (coagulopathy, acidosis, and hypothermia) in the setting of **septic shock**, necessitating physiologic stabilization before definitive surgery.
- The gold standard for **damage control** is to stabilize the patient in the ICU by correcting **base deficit**, improving **lactate clearance**, and restoring normal temperature and coagulation parameters.
*Immediate return to OR for definitive repair and anastomosis*
- Attempting **definitive repair** or anastomosis in an unstable patient with fecal peritonitis and high-dose **vasopressor requirements** carries a prohibited risk of dehiscence and death.
- Surgery should be limited to **staged re-intervention** only after the metabolic and physiologic insults have been partially reversed.
*Start therapeutic hypothermia and delay reoperation until hemodynamically stable off vasopressors*
- **Hypothermia** is a component of the lethal triad that worsens **coagulopathy** by inhibiting the clotting cascade; metabolic rewarming is required, not cooling.
- While stability is the goal, waiting to be completely off vasopressors might dangerously delay **source control** if the infection is driving the shock.
*Initiate high-dose vasopressors to maintain MAP >75 mmHg and early enteral nutrition*
- Focus should be on **volume resuscitation** and reversing tissue hypoxia (lactate) rather than solely escalating vasopressors, which can cause **mesenteric ischemia**.
- **Early enteral nutrition** is contraindicated in the immediate postoperative phase of an open abdomen with significant **hemodynamic instability** and high pressor requirements.
*Administer massive transfusion protocol and emergency re-exploration within 6 hours*
- **Massive transfusion protocol** is typically reserved for active, uncontrolled hemorrhage, whereas this patient primarily requires reversal of **septic shock** and metabolic derangements.
- **Re-exploration within 6 hours** is too early for a damage control patient who has not yet been adequately rewarmed or had their **acidosis** corrected.
Early recognition of sepsis US Medical PG Question 10: A 70-year-old man with recently diagnosed small cell lung cancer presents with septic shock from pneumonia. After initial resuscitation, he requires norepinephrine 0.6 mcg/kg/min and has a lactate of 7.8 mmol/L. His SOFA score is 14. The family requests 'everything be done,' but the patient had previously told his oncologist he would not want prolonged intensive care if his cancer prognosis was poor. Staging shows extensive-stage disease. The ICU team debates goals of care. What represents the most ethically appropriate approach to decision-making?
- A. Continue maximum therapy per family wishes as they are legal decision-makers
- B. Obtain ethics consultation to overrule family wishes based on futility
- C. Arrange urgent palliative care consultation and family meeting to discuss patient's previously expressed wishes and realistic prognosis (Correct Answer)
- D. Continue current therapy for 72 hours then reassess based on clinical trajectory
- E. Transition to comfort care based on poor oncologic prognosis and high SOFA score
Early recognition of sepsis Explanation: ***Arrange urgent palliative care consultation and family meeting to discuss patient's previously expressed wishes and realistic prognosis***
- The most ethically sound approach is to use **substituted judgment**, which prioritizes the patient's **previously expressed wishes** about avoiding prolonged intensive care.
- A **multidisciplinary family meeting** helps reconcile medical reality with patient values, ensuring informed **shared decision-making** rather than a unilateral or discordant approach.
*Continue maximum therapy per family wishes as they are legal decision-makers*
- While families are **surrogate decision-makers**, their role is to advocate for what the **patient would want**, not their own personal desires.
- Blindly following "everything be done" ignores the patient's prior statement to his oncologist and risks providing **non-beneficial treatment**.
*Obtain ethics consultation to overrule family wishes based on futility*
- The term **medical futility** is often controversial; ethics consultations are designed to **mediate conflicts** rather than simply provide a mechanism to overrule families.
- Unilateral decisions should only follow exhaustive attempts at **communication and mediation**, which have not yet occurred in this case.
*Continue current therapy for 72 hours then reassess based on clinical trajectory*
- A "time-limited trial" is a valid tool but fails to address the immediate ethical conflict regarding the **patient's autonomous refusal** of prolonged care.
- This approach may unnecessarily prolong the dying process and ignore the **prognostic alignment** required between the oncology and ICU teams.
*Transition to comfort care based on poor oncologic prognosis and high SOFA score*
- Clinicians should not unilaterally transition to **comfort care** without discussing the patient's prognosis and values with the family/surrogates first.
- While the **high SOFA score** and extensive cancer indicate a poor prognosis, the process must respect the legal and ethical requirements of **informed consent and withdrawal of care**.
More Early recognition of sepsis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.