Sepsis

On this page
🔥 The Sepsis Storm: When Immunity Becomes the Enemy
Sepsis transforms the body's protective immune response into a life-threatening cascade where inflammation spirals out of control, threatening every organ system simultaneously. You'll learn to recognize this medical emergency through subtle clinical clues, master the time-critical interventions that save lives in the first golden hour, and orchestrate the complex hemodynamic and antimicrobial strategies that guide patients from cellular crisis to recovery. This lesson builds your ability to think systematically under pressure, transforming pattern recognition into decisive action when minutes determine survival.
📌 Remember: SEPSIS - Systemic inflammatory response, Endothelial dysfunction, Perfusion compromise, Shock development, Immune dysregulation, Supporting organ failure. Each component amplifies the others in a self-perpetuating cycle.
The pathophysiology centers on cytokine storm activation, where TNF-α and IL-1β levels increase 10-100 fold within 2-4 hours of bacterial invasion. This triggers widespread endothelial dysfunction, capillary leak, and distributive shock - the hallmark triad that defines septic pathophysiology.
- Sepsis Definition Evolution
- SIRS-based (1991): Required ≥2 SIRS criteria plus infection
- Sepsis-3 (2016): Life-threatening organ dysfunction due to dysregulated host response
- qSOFA ≥2: Respiratory rate ≥22, altered mentation, SBP ≤100 mmHg
- SOFA score increase ≥2: More sensitive for ICU mortality prediction
- Mortality Benchmarks
- Sepsis: 10-15% hospital mortality
- Septic shock: 25-40% hospital mortality
- Refractory shock: >60% mortality at 48 hours
| Sepsis Stage | SOFA Score | Lactate (mmol/L) | Mortality (%) | Vasopressor Need | Fluid Requirement (L) |
|---|---|---|---|---|---|
| Sepsis | 2-5 | <2.0 | 10-15 | Rare | 1-2 |
| Severe Sepsis | 6-10 | 2.0-4.0 | 20-25 | Occasional | 2-4 |
| Septic Shock | >10 | >4.0 | 25-40 | Universal | 4-8 |
| Refractory | >15 | >8.0 | >60 | Multiple agents | >8 |
| MODS | >20 | >10.0 | >80 | Maximal support | Fluid overload |
💡 Master This: The "Golden Hour" concept in sepsis parallels trauma care - each hour delay in appropriate antibiotic administration increases mortality by 7.6%, making rapid recognition and treatment the cornerstone of survival.
Understanding sepsis epidemiology reveals 1.7 million annual cases in the US, with 270,000 deaths yearly - more than prostate cancer, breast cancer, and AIDS combined. Hospital costs exceed $24 billion annually, with average length of stay >10 days for survivors.
Connect this foundational understanding through systematic recognition tools to master the clinical identification patterns that separate survivors from statistics.
🔥 The Sepsis Storm: When Immunity Becomes the Enemy
⚡ Recognition Arsenal: The Clinical Detective's Toolkit
📌 Remember: qSOFA - Quick assessment: Respiratory rate ≥22, Altered mental status, Systolic BP ≤100. Two or more criteria predict >10% mortality risk and warrant immediate sepsis evaluation.
- qSOFA Performance Characteristics
- Sensitivity: 59% for sepsis, 74% for septic shock
- Specificity: 72% for sepsis, 84% for septic shock
- Positive predictive value: 24% in ED populations
- Negative predictive value: 92% when qSOFA <2
- SOFA Score Components (each 0-4 points)
- Respiratory: PaO₂/FiO₂ ratio (>400 = 0, <100 = 4)
- Coagulation: Platelets (>150 = 0, <20 = 4)
- Hepatic: Bilirubin (<1.2 = 0, >12 = 4)
- Cardiovascular: MAP and vasopressor requirements
- Neurologic: Glasgow Coma Scale (15 = 0, <6 = 4)
- Renal: Creatinine and urine output
| Clinical Finding | Sensitivity (%) | Specificity (%) | Likelihood Ratio+ | Likelihood Ratio- | Clinical Utility |
|---|---|---|---|---|---|
| Fever >38.3°C | 85 | 45 | 1.5 | 0.3 | Screening |
| Hypothermia <36°C | 15 | 95 | 3.0 | 0.9 | High specificity |
| Tachycardia >90 | 90 | 30 | 1.3 | 0.3 | Sensitive |
| Hypotension <90 | 45 | 90 | 4.5 | 0.6 | Late finding |
| Altered mental status | 65 | 80 | 3.3 | 0.4 | Organ dysfunction |
The SIRS criteria, while less specific than qSOFA, remain valuable for sensitivity. SIRS requires ≥2 criteria: temperature >38°C or <36°C, heart rate >90 bpm, respiratory rate >20/min, WBC >12,000 or <4,000 or >10% bands.
💡 Master This: Procalcitonin >0.5 ng/mL suggests bacterial infection with 85% sensitivity, while levels >2.0 ng/mL indicate severe sepsis with 90% specificity. Use for antibiotic stewardship - levels decreasing by >80% support de-escalation.
High-Risk Populations require modified thresholds:
- Immunocompromised: May lack fever response (30% afebrile)
- Elderly >65 years: Hypothermia more common than fever (25% vs 5%)
- Chronic illness: Baseline organ dysfunction masks early changes
- Post-operative: SIRS criteria less specific (false positive >60%)
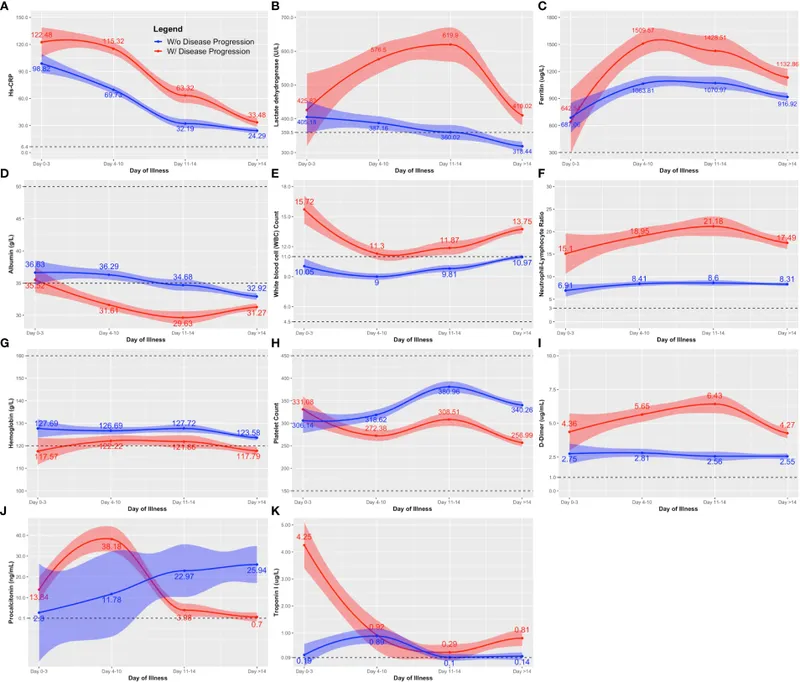
Advanced recognition incorporates biomarker integration:
- Procalcitonin: Rises within 2-4 hours, peaks at 12-24 hours
- Lactate: Reflects tissue hypoperfusion, normal <2.0 mmol/L
- CRP: Non-specific but trends useful, normal <3.0 mg/L
Connect these recognition patterns through rapid resuscitation protocols to transform early identification into life-saving interventions.
⚡ Recognition Arsenal: The Clinical Detective's Toolkit
🚀 The Golden Hour Protocol: Racing Against Cellular Death
📌 Remember: HOUR-1 - Hemodynamic assessment, Obtain cultures, Urinalysis and lactate, Resuscitate with fluids, 1 hour for antibiotics. This mnemonic captures the essential elements of early sepsis management.
- Hour-1 Bundle Components (all within 60 minutes)
- Lactate measurement: Baseline and 6-hour repeat if elevated
- Blood cultures: ≥2 sets before antibiotics (if no delay)
- Broad-spectrum antibiotics: Appropriate for suspected source
- Fluid resuscitation: 30 mL/kg crystalloid if hypotensive or lactate ≥4.0
- Vasopressors: If hypotension persists after fluid challenge
Fluid Resuscitation Strategy:
- Initial bolus: 30 mL/kg ideal body weight (~2-3 liters for 70kg adult)
- Crystalloid choice: Normal saline or balanced solutions
- Lactated Ringer's: Preferred in most cases
- Normal saline: Avoid in kidney disease (hyperchloremic acidosis)
- Reassessment markers: MAP >65 mmHg, urine output >0.5 mL/kg/hr
| Intervention | Time Target | Compliance Rate (%) | Mortality Benefit | Evidence Level | Implementation Barrier |
|---|---|---|---|---|---|
| Lactate measurement | <60 min | 85 | 15% reduction | High | Laboratory delays |
| Blood cultures | <60 min | 70 | 8% reduction | Moderate | Access issues |
| Antibiotics | <60 min | 65 | 7.6% per hour | High | Pharmacy delays |
| Fluid resuscitation | <60 min | 80 | 12% reduction | High | Volume concerns |
| Vasopressors | <60 min | 90 | 20% reduction | High | ICU availability |
Antibiotic Selection Principles:
- Empiric coverage: Gram-positive, Gram-negative, and anaerobes
- Source-directed: Urinary (fluoroquinolone), pneumonia (β-lactam + macrolide)
- Local resistance patterns: MRSA prevalence >20% = vancomycin
- Dose optimization: Loading doses for time-dependent antibiotics
💡 Master This: Dynamic fluid responsiveness assessment prevents fluid overload. Use passive leg raise (PLR) or stroke volume variation - if cardiac output increases >10%, patient is fluid responsive and benefits from additional crystalloid.
Hemodynamic Targets:
- Mean arterial pressure: ≥65 mmHg (higher if chronic hypertension)
- Central venous pressure: 8-12 mmHg (limited utility)
- Urine output: ≥0.5 mL/kg/hr over 2-hour windows
- Lactate clearance: ≥10% reduction at 6 hours
Quality Metrics and Outcomes:
- Bundle compliance >80%: Associated with 25% mortality reduction
- Time to antibiotics: Each hour delay increases mortality 7.6%
- Fluid timing: 30 mL/kg within 3 hours reduces ICU length of stay
Advanced resuscitation incorporates goal-directed therapy with ScvO₂ >70%, though recent trials show no mortality benefit over standard care when other targets are met.
Connect this systematic resuscitation approach through hemodynamic optimization strategies to master the transition from emergency stabilization to intensive care management.
🚀 The Golden Hour Protocol: Racing Against Cellular Death
🎯 Hemodynamic Command Center: Mastering the Pressure Game
📌 Remember: SHOCK - Systolic <90, Heart rate >100, Oliguria <0.5 mL/kg/hr, Cold extremities, Knowledge of lactate >2.0. These five findings define hemodynamic compromise requiring immediate intervention.
- Vasopressor Selection Hierarchy
- First-line: Norepinephrine 0.05-3.0 mcg/kg/min
- α₁-agonist: Vasoconstriction, minimal chronotropy
- β₁-agonist: Mild inotropic support
- Second-line: Vasopressin 0.01-0.04 units/min (fixed dose)
- V₁ receptor: Direct vasoconstriction
- Catecholamine-sparing: Reduces norepinephrine requirements
- Third-line: Epinephrine 0.05-2.0 mcg/kg/min
- α and β agonist: Vasoconstriction + inotropy
- Hyperglycemia risk: Monitor glucose closely
- First-line: Norepinephrine 0.05-3.0 mcg/kg/min
Hemodynamic Assessment Tools:
- Static parameters: CVP (8-12 mmHg), PAOP (12-18 mmHg)
- Dynamic parameters: SVV (<13% = fluid responsive), PPV (<13%)
- Functional assessment: Passive leg raise (>10% CO increase)
| Vasopressor | Dose Range | α-Effect | β-Effect | Advantages | Disadvantages | Cost ($/day) |
|---|---|---|---|---|---|---|
| Norepinephrine | 0.05-3.0 mcg/kg/min | ++++ | ++ | First-line, proven | Arrhythmias | 25-50 |
| Vasopressin | 0.01-0.04 units/min | +++ | 0 | NE-sparing | Fixed dose | 100-150 |
| Epinephrine | 0.05-2.0 mcg/kg/min | ++++ | ++++ | Inotropy | Hyperglycemia | 30-60 |
| Dopamine | 5-20 mcg/kg/min | ++ | +++ | Renal effects | Arrhythmogenic | 20-40 |
| Dobutamine | 2.5-20 mcg/kg/min | 0 | ++++ | Pure inotropy | Hypotension | 40-80 |
Inotropic Support Indications:
- Cardiac index <2.2 L/min/m² despite adequate preload
- Mixed venous oxygen saturation <65% with normal lactate
- Dobutamine 2.5-20 mcg/kg/min: Pure β₁-agonist for contractility
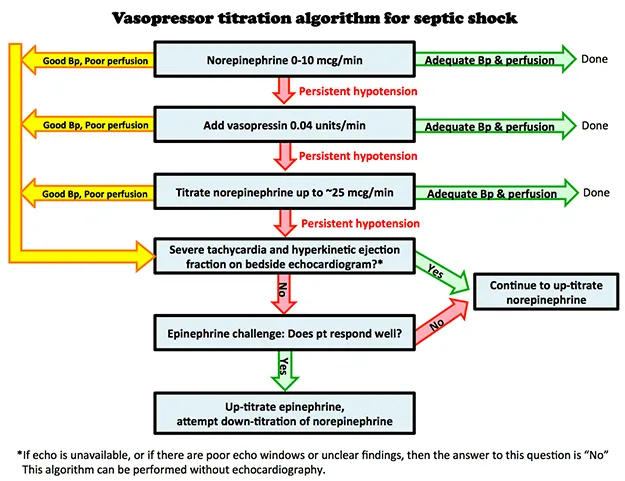
💡 Master This: Vasopressin 0.04 units/min (fixed dose) reduces norepinephrine requirements by 25-40% without improving mortality. Add when norepinephrine >0.25 mcg/kg/min to minimize catecholamine toxicity and preserve renal function.
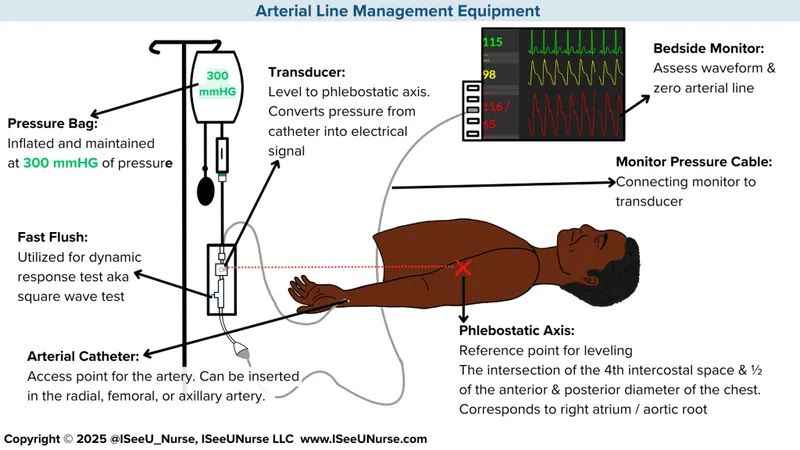
Advanced Hemodynamic Monitoring:
- Arterial line: Continuous BP, frequent ABGs, stroke volume variation
- Central venous catheter: CVP, ScvO₂, vasopressor administration
- Pulmonary artery catheter: Selected cases with refractory shock
- Echocardiography: Assess LV function, fluid responsiveness, RV strain
Hemodynamic Targets:
- Mean arterial pressure: 65-70 mmHg (higher if chronic HTN)
- Cardiac index: >2.2 L/min/m²
- Mixed venous saturation: >65%
- Lactate clearance: >10% at 6 hours, >20% at 12 hours
Weaning Strategy:
- Vasopressin first: Discontinue when NE <0.15 mcg/kg/min
- Norepinephrine: Decrease by 25-50% every 30-60 minutes
- Monitor closely: MAP, urine output, lactate trends
Connect this hemodynamic mastery through antimicrobial optimization strategies to ensure both circulatory support and infection control work synergistically for patient recovery.
🎯 Hemodynamic Command Center: Mastering the Pressure Game
🔬 Antimicrobial Warfare: Precision Strikes Against Infection
📌 Remember: ANTIBIOTICS - Administer early, Narrow when possible, Time-dependent vs concentration-dependent, Infection source, Biofilm considerations, Immune status, Organ function, Toxicity monitoring, Interaction awareness, Culture-directed, Stewardship principles.
- Empiric Antibiotic Selection by Source
- Pneumonia: Ceftriaxone + azithromycin or levofloxacin
- MRSA risk: Add vancomycin or linezolid
- Pseudomonas risk: Piperacillin-tazobactam + ciprofloxacin
- Urinary tract: Ceftriaxone or fluoroquinolone
- Complicated: Piperacillin-tazobactam or carbapenem
- Intra-abdominal: Piperacillin-tazobactam or carbapenem
- Anaerobic coverage: Metronidazole if using cephalosporin
- Skin/soft tissue: Vancomycin + piperacillin-tazobactam
- Pneumonia: Ceftriaxone + azithromycin or levofloxacin
Pharmacokinetic Optimization:
- Time-dependent killing: β-lactams, vancomycin
- Target: Time above MIC >40-70% of dosing interval
- Strategy: Continuous infusion or extended infusion
- Concentration-dependent: Fluoroquinolones, aminoglycosides
- Target: Peak/MIC ratio >8-10 or AUC/MIC >125
- Strategy: Higher doses, less frequent dosing
| Antibiotic Class | Dosing Strategy | PK/PD Target | Monitoring Parameter | Dose Adjustment | Toxicity Concern |
|---|---|---|---|---|---|
| β-lactams | Extended infusion | Time > MIC 40-70% | Clinical response | Renal function | Seizures (high dose) |
| Vancomycin | Continuous infusion | AUC/MIC > 400 | Trough 15-20 mg/L | Renal function | Nephrotoxicity |
| Fluoroquinolones | High dose | AUC/MIC > 125 | Clinical response | Renal function | QT prolongation |
| Aminoglycosides | Once daily | Peak/MIC > 8 | Peak/trough levels | Renal function | Nephro/ototoxicity |
| Linezolid | Standard dosing | Time > MIC 85% | Clinical response | None needed | Thrombocytopenia |
Resistance Pattern Recognition:
- ESBL producers: Require carbapenems (meropenem, imipenem)
- Carbapenem-resistant: Consider colistin, tigecycline, or ceftazidime-avibactam
- MRSA: Vancomycin, linezolid, daptomycin, or ceftaroline
- VRE: Linezolid, daptomycin, or tigecycline
💡 Master This: Procalcitonin-guided therapy reduces antibiotic duration by 2.4 days without increasing mortality. Stop antibiotics when PCT decreases >80% from peak or falls <0.5 ng/mL in clinically improving patients.
De-escalation Strategy:
- Timing: 48-72 hours after culture results
- Criteria: Clinical improvement + organism identification
- Approach: Narrow spectrum, oral conversion when appropriate
- Duration: 7-10 days for most infections, 5 days for pneumonia
Special Populations:
- Immunocompromised: Broader coverage, longer duration
- Renal dysfunction: Dose adjustment, avoid nephrotoxic combinations
- Hepatic impairment: Avoid hepatotoxic agents, adjust metabolism-dependent drugs
Biomarker-Guided Therapy:
- Procalcitonin >0.5 ng/mL: Bacterial infection likely
- Procalcitonin >2.0 ng/mL: Severe bacterial infection
- CRP trends: Useful for monitoring response
- White blood cell count: Less reliable in sepsis
Connect this antimicrobial precision through comprehensive organ support strategies to address the multi-system complications that define severe sepsis and septic shock.
🔬 Antimicrobial Warfare: Precision Strikes Against Infection
🛡️ The Recovery Framework: Orchestrating Multi-System Restoration
📌 Remember: RECOVERY - Respiratory support, Endocrine control, Coagulation management, Organ perfusion, Ventilator weaning, Electrolyte balance, Renal support, Yearning for homeostasis. Each component requires systematic optimization.
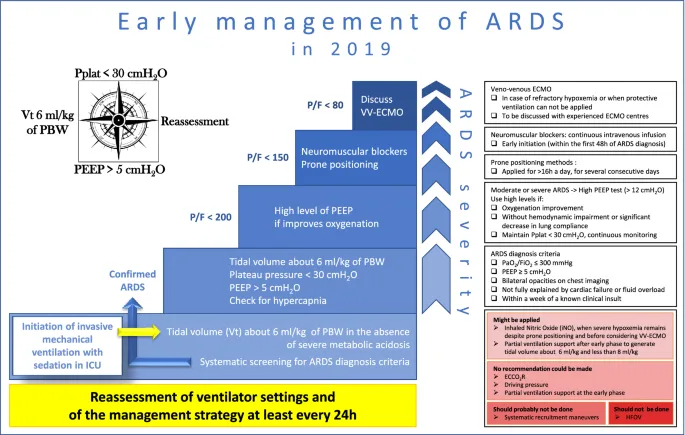
- Respiratory Support Strategy
- Mechanical ventilation: Lung-protective strategy with TV 6-8 mL/kg IBW
- PEEP optimization: 5-15 cmH₂O to maintain FiO₂ <60%
- Prone positioning: >12 hours daily if P/F ratio <150
- Mortality benefit: 16% reduction in severe ARDS
- Contraindications: Unstable spine, increased ICP
- Weaning protocol: Daily sedation vacation + spontaneous breathing trial
Renal Support Considerations:
- Indications for RRT: Oliguria >72 hours, K⁺ >6.5, pH <7.1, volume overload
- CRRT vs intermittent HD: CRRT preferred in hemodynamically unstable patients
- Dose prescription: 25-30 mL/kg/hr effluent rate for adequate clearance
| Organ System | Dysfunction Marker | Support Strategy | Target Parameter | Monitoring Frequency | Weaning Criteria |
|---|---|---|---|---|---|
| Respiratory | P/F ratio <300 | Lung protection | TV 6-8 mL/kg | Q4-6 hours | P/F >200, PEEP <8 |
| Cardiovascular | MAP <65 mmHg | Vasopressors | MAP 65-70 | Continuous | Off pressors >12h |
| Renal | Cr >2x baseline | CRRT/HD | UOP >0.5 mL/kg/hr | Q6-12 hours | Cr <1.5x baseline |
| Hepatic | Bilirubin >2 mg/dL | Supportive care | Synthetic function | Daily | Improving trends |
| Hematologic | Platelets <100K | Transfusion PRN | Plt >50K if bleeding | Daily | Plt >100K stable |
| Neurologic | GCS <13 | Sedation management | RASS -1 to 0 | Q4 hours | Alert, following commands |
Metabolic Management:
- Glucose control: Target 140-180 mg/dL (avoid tight control <110 mg/dL)
- Stress ulcer prophylaxis: PPI for high-risk patients (mechanical ventilation >48 hours)
- DVT prophylaxis: Pharmacologic unless contraindicated
- Nutrition support: Enteral preferred, start within 24-48 hours
💡 Master This: Sepsis-associated encephalopathy occurs in 70% of patients and predicts poor long-term outcomes. Minimize sedation, use dexmedetomidine over propofol when possible, and implement delirium prevention protocols with ABCDEF bundle.
Advanced Therapies for Refractory Cases:
- Extracorporeal membrane oxygenation (ECMO): Severe ARDS with P/F <50
- Plasmapheresis: Selected cases with thrombotic microangiopathy
- Immunomodulation: Hydrocortisone 200 mg/day for refractory shock
Recovery Milestones:
- Hemodynamic stability: Off vasopressors >24 hours
- Respiratory improvement: P/F ratio >200, PEEP <8 cmH₂O
- Renal recovery: Urine output >0.5 mL/kg/hr, creatinine trending down
- Neurologic recovery: Alert, following commands, delirium-free
Long-term Considerations:
- Post-intensive care syndrome (PICS): Physical, cognitive, and psychological impairments
- Sepsis survivors: 40% develop new functional limitations
- Follow-up care: ICU recovery clinic at 3-6 months
Quality Metrics:
- Ventilator-free days: Target >20 days at day 28
- ICU length of stay: Median 7-10 days for survivors
- Hospital mortality: <15% for sepsis, <30% for septic shock
This comprehensive recovery framework transforms the acute crisis of sepsis into systematic restoration of physiologic function, setting the foundation for long-term survival and quality of life.
🛡️ The Recovery Framework: Orchestrating Multi-System Restoration
Practice Questions: Sepsis
Test your understanding with these related questions
A 70-year-old woman is on hospital day 2 in the medical intensive care unit. She was admitted from the emergency department for a 2-day history of shortness of breath and fever. In the emergency department, her temperature is 39.4°C (103.0°F), the pulse is 120/min, the blood pressure is 94/54 mm Hg, the respiratory rate is 36/min, and oxygen saturation was 82% while on 4L of oxygen via a non-rebreather mask. Chest X-ray shows a right lower lobe consolidation. She was intubated, sedated, and started on broad-spectrum antibiotics for sepsis of pulmonary origin and intravenous norepinephrine for blood pressure support. Since then, her clinical condition has been stable, though her vasopressor and oxygen requirements have not improved. Today, her physician is called to the bedside because her nurse noted some slow bleeding from her intravenous line sites and around her urinary catheter. Which of the following most likely represents the results of coagulation studies for this patient?












