Post-MI secondary prevention US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Post-MI secondary prevention. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Post-MI secondary prevention US Medical PG Question 1: A 69-year-old man presents for a general follow up appointment. He states that he is doing well and wants to be sure he is healthy. The patient’s past medical history is significant for type II diabetes mellitus, peripheral vascular disease, and hypertension. His current medications include metformin, glyburide, lisinopril, metoprolol and hydrochlorothiazide. His blood pressure is 130/90 mmHg and pulse is 80/min. A fasting lipid panel was performed last week demonstrating an LDL of 85 mg/dL and triglycerides of 160 mg/dL. The patient states that he has not experienced any symptoms since his last visit. The patient’s blood glucose at this visit is 100 mg/dL. Which of the following is recommended in this patient?
- A. Begin statin therapy (Correct Answer)
- B. Increase lisinopril dose
- C. Increase HCTZ dose
- D. Discontinue metoprolol and start propranolol
- E. Increase metformin dose
Post-MI secondary prevention Explanation: **Begin statin therapy**
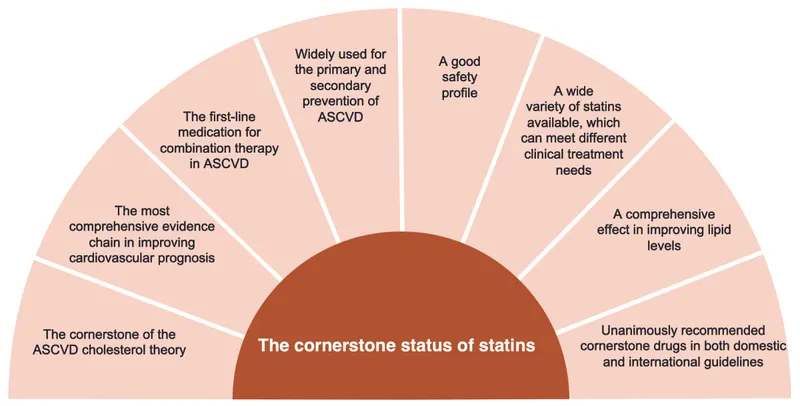
- The patient has **multiple risk factors** for cardiovascular disease including type 2 diabetes, peripheral vascular disease, and hypertension. His LDL-C of 85 mg/dL, while not excessively high, still warrants statin therapy given his high-risk profile, as guidelines recommend statin use in these patients to reduce cardiovascular events.
- Patients with a history of **atherosclerotic cardiovascular disease (ASCVD)**, which includes peripheral vascular disease, should be on a **high-intensity statin** regardless of their baseline LDL-C level, unless contraindicated.
*Increase lisinopril dose*
- The patient's blood pressure is 130/90 mmHg. While his systolic pressure is within an acceptable range for a patient with diabetes, his **diastolic pressure of 90 mmHg is slightly elevated**, but a single reading may not warrant an immediate dosage increase.
- Lisinopril is an ACE inhibitor and is already at an appropriate dose given the blood pressure. Further increasing the dose without evidence of persistent high blood pressure or other compelling indications is not the primary next step.
*Increase HCTZ dose*
- The patient is already on hydrochlorothiazide (HCTZ) for hypertension. His blood pressure is 130/90 mmHg, which is **not severely elevated**, and his medications are generally well-controlled.
- Increasing the dose of HCTZ might lead to side effects such as **electrolyte imbalances** (e.g., hypokalemia, hyponatremia) or worsening glucose control, and is not the most pressing intervention.
*Discontinue metoprolol and start propranolol*
- Metoprolol is a **selective beta-1 blocker** and is appropriate for this patient's hypertension and cardiac health, especially given his history.
- Propranolol is a **non-selective beta-blocker** and is generally less preferred in patients with diabetes or peripheral vascular disease due to potential masking of hypoglycemia symptoms and worsening peripheral circulation.
*Increase metformin dose*
- The patient's blood glucose is 100 mg/dL, indicating **good glycemic control** on his current regimen of metformin and glyburide.
- There is no indication to increase the metformin dose as his current glucose levels are within the target range, and increasing it could risk **hypoglycemia**, especially with concomitant glyburide.
Post-MI secondary prevention US Medical PG Question 2: A 55-year-old man comes to the physician because of a 4-month history of episodic, pressure-like chest pain. The chest pain occurs when he is walking up stairs and improves with rest. He has hypertension and type 2 diabetes mellitus. His father died from a myocardial infarction at the age of 50 years. Current medications include hydrochlorothiazide and metformin. His pulse is 85/min, respirations are 12/min, and blood pressure is 140/90 mm Hg. Cardiac examination shows normal heart sounds without any murmurs, rubs, or gallops. An ECG shows high amplitude of the S wave in lead V3. An exercise stress test is performed but stopped after 4 minutes because the patient experiences chest pain. An ECG obtained during the stress test shows sinus tachycardia and ST-segment depressions in leads V1–V4. Which of the following is the most appropriate long-term pharmacotherapy to reduce the frequency of symptoms in this patient?
- A. Metoprolol (Correct Answer)
- B. Clopidogrel
- C. Aspirin
- D. Nitroglycerin
- E. Isosorbide mononitrate
Post-MI secondary prevention Explanation: ***Metoprolol***
- **Beta-blockers** like metoprolol are first-line agents for **symptom relief** in stable angina by reducing myocardial oxygen demand.
- They decrease **heart rate**, **blood pressure**, and **myocardial contractility**, thereby reducing the frequency and severity of anginal episodes.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent used primarily to prevent **thrombotic events** in patients with established cardiovascular disease or acute coronary syndromes.
- It does not directly reduce the frequency of anginal symptoms, but rather prevents progression to **myocardial infarction** or **stroke**.
*Aspirin*
- **Aspirin** is an antiplatelet medication used for **secondary prevention** of cardiovascular events by inhibiting platelet aggregation.
- While crucial for reducing cardiovascular risk, it does not directly alleviate the **frequency of anginal symptoms** themselves.
*Nitroglycerin*
- **Nitroglycerin** is a short-acting nitrate used to provide **immediate relief** of anginal pain during an acute episode.
- It is not a long-term pharmacotherapy for reducing the *frequency* of symptoms.
*Isosorbide mononitrate*
- **Isosorbide mononitrate** is a long-acting nitrate used to *prevent* angina, but it is typically a **second-line agent** after beta-blockers due to potential for **tolerance** and side effects.
- While it can reduce symptom frequency, beta-blockers are generally preferred as initial long-term therapy for symptom control.
Post-MI secondary prevention US Medical PG Question 3: A 64-year-old man presents to his physician for a scheduled follow-up visit. He has chronic left-sided heart failure with systolic dysfunction. His current regular medications include captopril and digoxin, which were started after his last episode of symptomatic heart failure approximately 3 months ago. His last episode of heart failure was accompanied by atrial fibrillation, which followed an alcohol binge over a weekend. Since then he stopped drinking. He reports that he has no current symptoms at rest and is able to perform regular physical exercise without limitation. On physical examination, mild bipedal edema is noted. The physician suggested to him that he should discontinue digoxin and continue captopril and scheduled him for the next follow-up visit. Which of the following statements best justifies the suggestion made by the physician?
- A. Long-term digoxin therapy produces significant survival benefits in patients with heart failure, but at the cost of increased heart failure-related admissions.
- B. Both captopril and digoxin are likely to improve the long-term survival of the patient with heart failure, but digoxin has more severe side effects.
- C. Captopril is likely to improve the long-term survival of the patient with heart failure, unlike digoxin.
- D. Digoxin does not benefit patients with left-sided heart failure in the absence of atrial fibrillation.
- E. Digoxin is useful to treat atrial fibrillation, but does not benefit patients with systolic dysfunction who are in sinus rhythm. (Correct Answer)
Post-MI secondary prevention Explanation: ***Digoxin is useful to treat atrial fibrillation, but does not benefit patients with systolic dysfunction who are in sinus rhythm.***
- The patient's **atrial fibrillation** was likely triggered by the alcohol binge and has since resolved, suggesting he is now in **sinus rhythm**.
- Digoxin's primary benefit in heart failure with **systolic dysfunction** (HFrEF) is to control ventricular rate in patients with **atrial fibrillation**, but it does not offer survival benefit in HFrEF patients who are in **sinus rhythm** and well-managed with other therapies.
*Long-term digoxin therapy produces significant survival benefits in patients with heart failure, but at the cost of increased heart failure-related admissions.*
- This statement is incorrect; digoxin has been shown to **reduce hospital admissions** for heart failure, but it does **not provide a significant survival benefit** in patients with HFrEF in sinus rhythm.
- The main benefit of digoxin in HFrEF is to improve symptoms and quality of life, alongside reducing hospitalizations, but not prolonging life.
*Both captopril and digoxin are likely to improve the long-term survival of the patient with heart failure, but digoxin has more severe side effects.*
- **Captopril (an ACE inhibitor)** does improve **long-term survival** in heart failure, but **digoxin does not** demonstrably improve survival.
- While digoxin can have side effects, its lack of survival benefit for HFrEF in sinus rhythm is the primary reason for discontinuation, not just side effect severity.
*Captopril is likely to improve the long-term survival of the patient with heart failure, unlike digoxin.*
- This statement is partially correct that **captopril improves survival**, but it does not fully explain the physician's decision to discontinue digoxin.
- The key missing piece is the patient's current **sinus rhythm** and the lack of benefit of digoxin in that specific context for HFrEF.
*Digoxin does not benefit patients with left-sided heart failure in the absence of atrial fibrillation.*
- This statement is nearly correct, but "left-sided heart failure" is broad. It is specifically in patients with **systolic dysfunction (HFrEF)** who are in **sinus rhythm** that digoxin lacks significant benefit beyond symptom control, and does not provide survival benefit.
Post-MI secondary prevention US Medical PG Question 4: A 72-year-old man presents to the outpatient clinic today. He has New York Heart Association class III heart failure. His current medications include captopril 20 mg, furosemide 40 mg, potassium chloride 10 mg twice daily, rosuvastatin 20 mg, and aspirin 81 mg. He reports that he generally feels well and has not had any recent worsening of his symptoms. His blood pressure is 132/85 mm Hg and heart rate is 84/min. Physical examination is unremarkable except for trace pitting edema of the bilateral lower extremities. What other medication should be added to his heart failure regimen?
- A. Losartan
- B. Metoprolol tartrate
- C. Isosorbide dinitrate/hydralazine
- D. Metoprolol succinate (Correct Answer)
- E. Digoxin
Post-MI secondary prevention Explanation: ***Metoprolol succinate***
- Current guidelines recommend adding a **beta-blocker** (specifically metoprolol succinate, carvedilol, or bisoprolol) as part of guideline-directed medical therapy (GDMT) for **NYHA class II-IV heart failure with reduced ejection fraction (HFrEF)**.
- This patient is already on an **ACE inhibitor and diuretic** but is missing a **beta-blocker**, which is a cornerstone of HFrEF therapy.
- Beta-blockers **reduce mortality and morbidity** in HFrEF by counteracting chronic sympathetic activation, improving cardiac remodeling, and reducing heart rate.
- Metoprolol succinate is the **long-acting formulation** preferred for chronic heart failure management.
***Incorrect Option: Losartan***
- The patient is already on an **ACE inhibitor (captopril)**, which acts on the renin-angiotensin-aldosterone system.
- Adding an **ARB (angiotensin receptor blocker)** like losartan to an ACE inhibitor is generally not recommended due to increased risk of hyperkalemia, hypotension, and renal dysfunction without significant additional benefit.
- ARBs are typically used as an alternative when patients cannot tolerate ACE inhibitors (e.g., due to cough or angioedema).
***Incorrect Option: Metoprolol tartrate***
- While metoprolol tartrate is a beta-blocker, it is a **short-acting formulation** typically used for acute conditions like hypertension or angina.
- For **chronic heart failure management**, **long-acting beta-blockers** such as metoprolol succinate are preferred due to sustained therapeutic levels, better adherence, and proven mortality benefit in clinical trials.
***Incorrect Option: Isosorbide dinitrate/hydralazine***
- This combination is primarily indicated for **African American patients with NYHA class III-IV HFrEF** who remain symptomatic despite optimal therapy, or as an alternative in patients who cannot tolerate ACE inhibitors/ARBs.
- While the patient has class III heart failure, he is **not yet on a beta-blocker**, which is a more fundamental component of GDMT and should be added first.
- This combination is typically added as a fourth-line agent.
***Incorrect Option: Digoxin***
- Digoxin is considered for patients with **HFrEF who remain symptomatic** despite optimized therapy with ACE inhibitors/ARBs, beta-blockers, and mineralocorticoid receptor antagonists (MRAs).
- It primarily helps **improve symptoms and reduce hospitalizations** but does not reduce mortality.
- Since this patient is not yet on a beta-blocker, adding the beta-blocker takes priority.
Post-MI secondary prevention US Medical PG Question 5: A 49-year-old man with a past medical history of hypertension on amlodipine presents to your office to discuss ways to lessen his risk of complications from heart disease. After a long discussion, he decides to significantly decrease his intake of trans fats in an attempt to lower his risk of coronary artery disease. Which type of prevention is this patient initiating?
- A. Secondary prevention
- B. Delayed prevention
- C. Quaternary prevention
- D. Tertiary prevention
- E. Primary prevention (Correct Answer)
Post-MI secondary prevention Explanation: ***Primary prevention***
- This patient is initiating primary prevention by **modifying lifestyle choices** (decreasing trans fats) to **prevent the initial onset of coronary artery disease**, as he has a risk factor (hypertension) but no established heart disease.
- Primary prevention focuses on **preventing disease before it occurs** through health promotion and risk reduction.
*Secondary prevention*
- Secondary prevention involves **early detection and treatment of existing disease** to prevent progression or recurrence.
- Examples include **screening tests** like mammography or **medications for individuals already diagnosed** with a condition.
*Delayed prevention*
- This is **not a recognized category** of prevention in public health or medical practice.
- Prevention stages are typically classified as primary, secondary, tertiary, and sometimes quaternary.
*Quaternary prevention*
- Quaternary prevention aims to **protect patients from medical interventions** that may cause harm, such as over-medicalization or unnecessary procedures.
- It focuses on **reducing the burden of iatrogenic disease** and ensuring appropriate care.
*Tertiary prevention*
- Tertiary prevention focuses on **reducing the impact of an existing disease** or disability through rehabilitation and managing complications.
- It applies to patients who **already have an established disease** and seeks to improve their quality of life and functionality.
Post-MI secondary prevention US Medical PG Question 6: A 57-year-old man presents to the emergency department for evaluation of slurred speech and left arm and leg weakness over the last 3 hours. History reveals hypertension that is being treated with hydrochlorothiazide. Vital signs include: blood pressure of 110/70 mm Hg, heart rate 104/min, respiratory rate 18/min, and temperature 36.6°C (98.0°F). Physical examination reveals 2/5 strength in both left upper and lower extremities. After 2 hours, the patient’s symptoms suddenly disappear. An electrocardiogram (ECG) is obtained (see image). Which of the following medications could prevent ischemic attacks in this patient in the future?
- A. Warfarin (Correct Answer)
- B. Acetylsalicylic acid
- C. Enoxaparin
- D. Heparin
- E. Clopidogrel
Post-MI secondary prevention Explanation: ***Warfarin***
- The patient experienced a **transient ischemic attack (TIA)** due to the sudden onset of neurological symptoms that resolved completely. The ECG shows **atrial fibrillation (AFib)**, characterized by an irregularly irregular rhythm and absence of P waves, which is a significant risk factor for cardioembolic stroke.
- **Oral anticoagulation** is essential for preventing ischemic stroke in patients with AFib. While **direct oral anticoagulants (DOACs)** such as apixaban, rivaroxaban, or dabigatran are now preferred as first-line therapy per current guidelines, **warfarin** remains an effective alternative and is the only oral anticoagulant option listed here.
- Warfarin prevents the formation of blood clots in the heart chambers by inhibiting vitamin K-dependent clotting factors, thereby reducing the risk of cardioembolic stroke.
*Acetylsalicylic acid*
- **Aspirin (acetylsalicylic acid)** is an antiplatelet agent used for primary and secondary prevention of ischemic stroke, particularly in patients with non-cardioembolic causes.
- While aspirin can be used in some cases, its efficacy in preventing stroke in patients with AFib is **significantly lower than that of oral anticoagulants** like warfarin or DOACs (reduces stroke risk by ~20% vs ~60-70% with anticoagulation).
*Enoxaparin*
- **Enoxaparin** is a low molecular weight heparin, an anticoagulant typically used for the **acute treatment** of deep vein thrombosis (DVT) and pulmonary embolism (PE), and sometimes as a bridge to warfarin therapy.
- It is not routinely used for **long-term prevention** of ischemic stroke in patients with AFib due to its parenteral (subcutaneous) administration and the need for daily injections.
*Heparin*
- **Heparin** (unfractionated) is an anticoagulant used for acute management of thrombotic events but requires continuous intravenous infusion and close monitoring of aPTT.
- Similar to enoxaparin, it is not practical or recommended for **long-term outpatient prophylaxis** against stroke in AFib.
*Clopidogrel*
- **Clopidogrel** is an antiplatelet agent that inhibits platelet aggregation via P2Y12 receptor blockade and is used in patients with atherosclerotic disease or as an alternative to aspirin in certain circumstances.
- It works by a different mechanism than anticoagulants and is generally **less effective than warfarin or DOACs** for preventing cardioembolic stroke from AFib (similar efficacy to aspirin alone).
Post-MI secondary prevention US Medical PG Question 7: A 56-year-old woman comes to the physician for follow-up after a measurement of elevated blood pressure at her last visit three months ago. She works as a high school teacher at a local school. She says that she mostly eats cafeteria food and take-out. She denies any regular physical activity. She does not smoke or use any recreational drugs. She drinks 2 to 3 glasses of wine per day. She has hypercholesterolemia for which she takes atorvastatin. Her height is 165 cm (5 ft 5 in), weight is 82 kg (181 lb), and BMI is 30.1 kg/m2. Her pulse is 67/min, respirations are 18/min, and blood pressure is 152/87 mm Hg on the right arm and 155/92 mm Hg on the left arm. She would like to try lifestyle modifications to improve her blood pressure before considering pharmacologic therapy. Which of the following lifestyle modifications is most likely to result in the greatest reduction of this patient's systolic blood pressure?
- A. Walking for 30 minutes, 5 days per week
- B. Reducing sodium intake to less than 2.4 g per day
- C. Losing 15 kg (33 lb) of body weight (Correct Answer)
- D. Adopting a DASH diet
- E. Decreasing alcohol consumption to maximum of one drink per day
Post-MI secondary prevention Explanation: ***Losing 15 kg (33 lb) of body weight***
- **Weight reduction** is the most effective lifestyle modification for lowering blood pressure, correlating directly with the amount of weight lost.
- A loss of 15 kg (33 lb) in this patient, who is **obese (BMI 30.1)**, could significantly reduce her systolic blood pressure, potentially by 5-20 mmHg per 10 kg weight loss.
*Walking for 30 minutes, 5 days per week*
- Regular **aerobic physical activity** is beneficial for blood pressure reduction, typically resulting in a 4-9 mmHg decrease in systolic pressure.
- While helpful, the magnitude of reduction from exercise alone is generally less than that achieved with significant weight loss in an obese individual.
*Reducing sodium intake to less than 2.4 g per day*
- **Sodium restriction** is an effective strategy, often leading to a 2-8 mmHg reduction in systolic blood pressure.
- Given the patient's diet of cafeteria and take-out food, high sodium intake is likely, making this a relevant intervention, but typically less impactful than substantial weight loss.
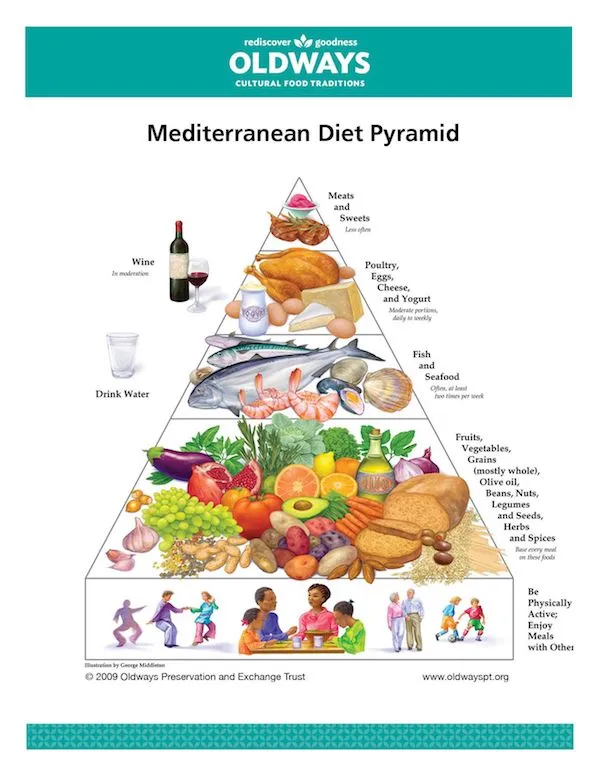
*Adopting a DASH diet*
- The **Dietary Approaches to Stop Hypertension (DASH) diet** emphasizes fruits, vegetables, and low-fat dairy, and can significantly lower blood pressure, by 8-14 mmHg.
- This diet is highly effective, but for an obese individual, the blood pressure reduction from achieving a healthy weight is often greater.
*Decreasing alcohol consumption to maximum of one drink per day*
- Reducing **excessive alcohol intake** can decrease systolic blood pressure by 2-4 mmHg, as the patient reports 2-3 glasses of wine daily.
- While beneficial, this reduction is likely to be less substantial compared to major weight loss or other dietary changes.
Post-MI secondary prevention US Medical PG Question 8: A 73-year-old man presents to the outpatient clinic complaining of chest pain with exertion. He states that resting for a few minutes usually resolves the chest pain. Currently, he takes 81 mg of aspirin daily. He has a blood pressure of 127/85 mm Hg and heart rate of 75/min. Physical examination reveals regular heart sounds and clear lung sounds bilateral. Which medication regimen below should be added?
- A. Metoprolol and a statin daily. Sublingual nitroglycerin as needed. (Correct Answer)
- B. Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.
- C. Amlodipine and a statin daily. Sublingual nitroglycerin as needed.
- D. Amlodipine daily. Sublingual nitroglycerin as needed.
- E. Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.
Post-MI secondary prevention Explanation: ***Metoprolol and a statin daily. Sublingual nitroglycerin as needed.***
- This patient presents with symptoms consistent with **stable angina** (**chest pain with exertion, relieved by rest**). The recommended medical therapy includes **antiplatelet agents** (aspirin, already prescribed), **beta-blockers** (metoprolol) for symptom control and improved survival post-MI, and **high-intensity statins** for lipid management and plaque stabilization. **Sublingual nitroglycerin** is crucial for acute symptom relief.
- Beta-blockers like metoprolol decrease myocardial **oxygen demand** by reducing heart rate and contractility, effectively treating angina. Statins are essential for **atherosclerosis management**.
*Clopidogrel and amlodipine daily. Sublingual nitroglycerin as needed.*
- While clopidogrel is an **antiplatelet agent**, aspirin is typically the first-line choice for stable angina unless there's an intolerance or compelling reason for dual antiplatelet therapy (e.g., recent stent placement), which is not indicated here.
- Amlodipine, a **calcium channel blocker**, can be used for angina but is usually a second-line agent if beta-blockers are contraindicated or insufficient; it doesn't offer the mortality benefit seen with beta-blockers post-MI.
*Amlodipine and a statin daily. Sublingual nitroglycerin as needed.*
- This regimen includes a **statin** and sublingual nitroglycerin, which are appropriate. However, it uses amlodipine instead of a beta-blocker, which is generally the preferred initial therapy for angina due to its benefits in reducing myocardial oxygen demand and improving outcomes, especially in patients with a history of MI or heart failure.
- Beta-blockers provide superior **mortality reduction benefits** in patients with coronary artery disease compared to calcium channel blockers.
*Amlodipine daily. Sublingual nitroglycerin as needed.*
- This option misses two critical components of comprehensive treatment for stable angina: a **statin** for lipid management and plaque stabilization, and a **beta-blocker** for primary symptom control and long-term cardiac protection.
- Relying solely on amlodipine and sublingual nitroglycerin would leave the patient incompletely treated for their underlying **coronary artery disease**.
*Metoprolol and ranolazine daily. Sublingual nitroglycerin as needed.*
- This option lacks a **statin**, which is a cornerstone of therapy for stable angina to manage atherosclerosis.
- While metoprolol is appropriate and ranolazine can be used as an add-on therapy for refractory angina, it's not typically a first-line agent and doesn't replace the need for a statin.
Post-MI secondary prevention US Medical PG Question 9: A 70-year-old man with diabetes, hypertension, and chronic kidney disease (eGFR 35 mL/min/1.73m²) presents with NSTEMI. Troponin is elevated at 8.5 ng/mL. ECG shows 2mm ST depression in V2-V5. GRACE score is 165 (high risk). He is hemodynamically stable. Cardiologist recommends early invasive strategy within 24 hours. Nephrologist is concerned about contrast-induced nephropathy potentially requiring dialysis. Patient is on metformin. Evaluate the management strategy integrating multiple specialist perspectives and evidence.
- A. Proceed with angiography within 24 hours using iso-osmolar contrast and intravenous hydration, hold metformin (Correct Answer)
- B. Perform coronary CT angiography as alternative to invasive angiography
- C. Delay catheterization for 72 hours to optimize renal function with hydration
- D. Prophylactic hemodialysis before and after catheterization to remove contrast
- E. Medical management only with dual antiplatelet therapy, avoid catheterization
Post-MI secondary prevention Explanation: ***Proceed with angiography within 24 hours using iso-osmolar contrast and intravenous hydration, hold metformin***
- High-risk NSTEMI patients with a **GRACE score >140** benefit from an **early invasive strategy** within 24 hours to reduce ischemic events and mortality.
- Renal protection is maximized through **pre-procedural hydration** and **iso-osmolar contrast**, while **metformin** must be held to avoid the risk of lactic acidosis if acute kidney injury occurs.
*Perform coronary CT angiography as alternative to invasive angiography*
- **Coronary CTA** is primarily used for ruling out coronary artery disease in low-to-intermediate risk stable patients, not for high-risk **NSTEMI**.
- This modality still requires **iodinated contrast** and does not provide the therapeutic benefit of percutaneous coronary intervention (**PCI**).
*Delay catheterization for 72 hours to optimize renal function with hydration*
- Delaying the procedure in a high-risk patient increases the risk of **re-infarction** and **cardiovascular death**, outweighing the minor benefits of prolonged hydration.
- Evidence suggests that optimization of renal status should happen concurrently with the preparation for **early intervention** in high-risk ACS.
*Prophylactic hemodialysis before and after catheterization to remove contrast*
- **Prophylactic hemodialysis** has not been proven to prevent contrast-induced nephropathy and may actually increase the risk of adverse events.
- High-volume **intravenous hydration** with isotonic saline remains the gold standard for preventing renal injury in patients with **CKD**.
*Medical management only with dual antiplatelet therapy, avoid catheterization*
- While **dual antiplatelet therapy** is essential, medical management alone is inferior to an invasive strategy in patients with **high GRACE scores**.
- Avoiding catheterization based solely on **renal impairment** results in "renalism," where patients are undertreated for their life-threatening cardiac condition.
Post-MI secondary prevention US Medical PG Question 10: A 58-year-old woman with anterior STEMI underwent primary PCI with drug-eluting stent placement. Post-procedure echocardiogram shows left ventricular ejection fraction of 30% with apical akinesis. She is started on aspirin, ticagrelor, high-intensity statin, and ACE inhibitor. On hospital day 3, she develops atrial fibrillation with rapid ventricular response. CHA2DS2-VASc score is 4. Creatinine is normal. Evaluate the optimal antithrombotic strategy balancing ischemic and bleeding risk.
- A. Triple therapy with aspirin, ticagrelor, and apixaban indefinitely
- B. Triple therapy for 6 months, then aspirin and apixaban indefinitely
- C. Aspirin and ticagrelor only, hold anticoagulation due to bleeding risk
- D. Warfarin with INR 2-3 plus aspirin, discontinue ticagrelor
- E. Triple therapy for 1 month, then apixaban and clopidogrel for 11 months, then apixaban alone (Correct Answer)
Post-MI secondary prevention Explanation: ***Triple therapy for 1 month, then apixaban and clopidogrel for 11 months, then apixaban alone***
- In patients with **Atrial Fibrillation** (CHA2DS2-VASc ≥2) undergoing **PCI**, current guidelines recommend minimizing the duration of **triple therapy** (aspirin, P2Y12 inhibitor, and anticoagulant) to 1 week to 1 month to reduce **bleeding risk**.
- Transitioning to **dual therapy** with a **NOAC** (like apixaban) and a P2Y12 inhibitor (preferably **clopidogrel**) for up to 12 months, followed by NOAC monotherapy, provides an optimal balance between preventing **stent thrombosis** and systemic **thromboembolism**.
*Triple therapy with aspirin, ticagrelor, and apixaban indefinitely*
- Indefinite **triple therapy** carries a prohibitively high risk of life-threatening **major bleeding** without added benefit for stroke prevention.
- **Ticagrelor** is generally avoided in triple therapy regimens due to a significantly higher bleeding profile compared to **clopidogrel**.
*Triple therapy for 6 months, then aspirin and apixaban indefinitely*
- **Triple therapy** for 6 months is rarely indicated and significantly increases the risk of **gastrointestinal and intracranial hemorrhage** compared to the 1-month strategy.
- Aspirin is usually discontinued after the first year in favor of **anticoagulant monotherapy**, as the latter is sufficient for both AF and stable CAD protection.
*Aspirin and ticagrelor only, hold anticoagulation due to bleeding risk*
- This approach leaves the patient with a high **CHA2DS2-VASc score of 4** unprotected against **cardioembolic stroke**, which carries high morbidity and mortality.
- Dual antiplatelet therapy (DAPT) alone is significantly less effective than **oral anticoagulants** for stroke prevention in the setting of atrial fibrillation.
*Warfarin with INR 2-3 plus aspirin, discontinue ticagrelor*
- **NOACs** (like apixaban) are now preferred over **Warfarin** for non-valvular AF due to a superior safety profile, including a lower risk of **intracranial hemorrhage**.
- Discontinuing the P2Y12 inhibitor (ticagrelor) immediately post-PCI in favor of aspirin and warfarin significantly increases the risk of **stent thrombosis**.
More Post-MI secondary prevention US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.