Mechanical complications management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mechanical complications management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
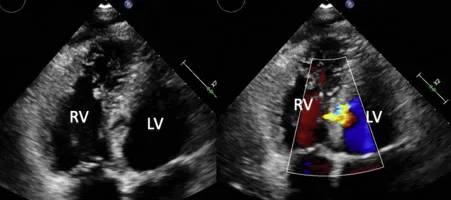
Mechanical complications management US Medical PG Question 1: A 2-year-old girl is brought to the physician by her mother for a well-child examination. Cardiac auscultation is shown. When she clenches her fist forcefully for a sustained time, the intensity of the murmur increases. Which of the following is the most likely cause of this patient's auscultation findings?
- A. Failure of the ductus arteriosus to close
- B. Defect in the atrial septum
- C. Fusion of the right and left coronary leaflets
- D. Prolapse of the mitral valve
- E. Defect in the ventricular septum (Correct Answer)
Mechanical complications management Explanation: ***Defect in the ventricular septum***
- A **ventricular septal defect (VSD)** causes a holosystolic, harsh murmur, often loudest at the **left lower sternal border**.
- **Clenching the fist forcefully increases systemic vascular resistance (afterload)**, which enhances the left-to-right shunting through a VSD, thereby **increasing the intensity** of the murmur.
*Failure of the ductus arteriosus to close*
- A **patent ductus arteriosus (PDA)** typically presents with a **continuous "machinery-like" murmur**, not one that increases with clenching a fist.
- The murmur of a PDA is usually best heard in the **pulmonary area** (left upper sternal border).
*Defect in the atrial septum*
- An **atrial septal defect (ASD)** usually causes a **systolic ejection murmur** over the pulmonic area due to increased flow across the pulmonary valve, and a **fixed split S2**.
- Its intensity is generally **not significantly altered by acute changes in systemic vascular resistance** like clenching a fist.
*Fusion of the right and left coronary leaflets*
- This description is characteristic of a **bicuspid aortic valve** leading to **aortic stenosis**.
- Aortic stenosis typically causes a **systolic ejection murmur** that **decreases** in intensity with maneuvers that increase afterload (like clenching a fist) due to reduced stroke volume.
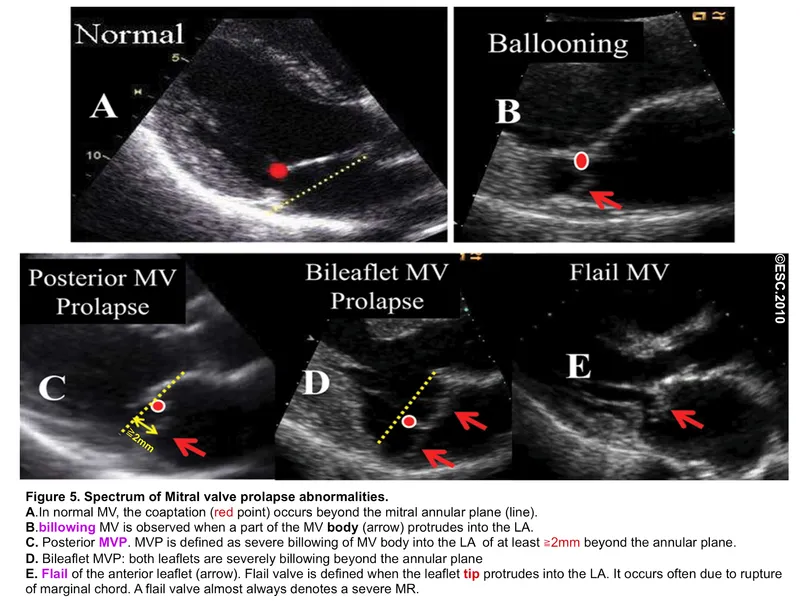
*Prolapse of the mitral valve*
- **Mitral valve prolapse (MVP)** is characterized by a **mid-systolic click** followed by a **late-systolic murmur**.
- **Increasing afterload** (clenching a fist) would typically **delay the click and shorten the murmur**, or make it softer, as it *reduces* the degree of prolapse.
Mechanical complications management US Medical PG Question 2: A 59-year-old male presents to the emergency room with shortness of breath. Ten days ago, he was in the cardiac critical care unit after receiving a balloon angioplasty and a bare metal stent for an ST-elevation myocardial infarction (STEMI). On physical examination, a holosystolic murmur is heard at the cardiac apex radiating to the axilla. You also detect an S3 and bilateral crackles in the lung bases. What is the most likely etiology of this patient's acute decompensated heart failure?
- A. Rupture of the septal papillary muscle on the right ventricle
- B. Rupture of the posteromedial papillary muscle of the left ventricle (Correct Answer)
- C. Rupture of the posterior papillary muscle on the right ventricle
- D. Rupture of the anterolateral papillary muscle of the left ventricle
- E. Rupture of the anterior papillary muscle of the right ventricle
Mechanical complications management Explanation: ***Rupture of the posteromedial papillary muscle of the left ventricle***
- The patient's presentation with acute decompensated heart failure following a STEMI, new holosystolic murmur radiating to the axilla, S3, and bilateral crackles is highly suggestive of acute **mitral regurgitation**.
- The posteromedial papillary muscle is particularly susceptible to ischemic injury and rupture after an **inferior or posterior STEMI** because it has a **single blood supply** from the posterior descending artery (PDA), making it a common complication within days to weeks post-MI.
*Rupture of the septal papillary muscle on the right ventricle*
- The right ventricle does not have "septal" papillary muscles; it has anterior, posterior, and septal papillary muscles, but a distinct "septal papillary muscle on the right ventricle" causing systemic symptoms like those described is anatomically incorrect in this context.
- Right ventricular papillary muscle rupture would primarily affect the **tricuspid valve**, leading to **tricuspid regurgitation**, which typically presents with signs of **right-sided heart failure** (e.g., jugular venous distention, hepatomegaly) rather than a murmur radiating to the axilla.
*Rupture of the posterior papillary muscle on the right ventricle*
- Rupture of a posterior papillary muscle of the right ventricle would primarily cause **tricuspid regurgitation**, not mitral regurgitation.
- This would lead to signs of **right heart failure**, and the murmur would typically be heard loudest at the **lower left sternal border**, intensifying with inspiration, not radiating to the axilla.
*Rupture of the anterolateral papillary muscle of the left ventricle*
- While rupture of the anterolateral papillary muscle can cause acute mitral regurgitation, it is **less common** than posteromedial rupture.
- This is because the anterolateral papillary muscle has a **dual blood supply** from both the left anterior descending (LAD) and circumflex arteries, making it more resistant to ischemia.
*Rupture of the anterior papillary muscle of the right ventricle*
- This would result in **tricuspid regurgitation**, not mitral regurgitation.
- Symptoms would be consistent with **right heart failure**, and the murmur's characteristics would differ from those described (e.g., location, radiation).
Mechanical complications management US Medical PG Question 3: A 35-year-old man is brought to the emergency department 20 minutes after being involved in a motor vehicle collision in which he was a restrained passenger. The patient is confused. His pulse is 140/min and blood pressure is 85/60 mm Hg. Examination shows a hand-sized hematoma on the anterior chest wall. An ECG shows sinus tachycardia. Which of the following structures is most likely injured in this patient?
- A. Papillary muscle
- B. Left main coronary artery
- C. Inferior vena cava
- D. Aortic isthmus (Correct Answer)
- E. Aortic valve
Mechanical complications management Explanation: ***Aortic isthmus***
- The **aortic isthmus** is the most common site of blunt **aortic injury** due to its relative immobility compared to the more mobile ascending aorta and arch. The deceleration forces experienced in a motor vehicle collision can cause a shearing injury at this location.
- The patient's **hypotension** and **tachycardia** are signs of significant hemorrhage, which is a common presentation of aortic injury. The chest wall hematoma also suggests significant trauma to the chest.
*Papillary muscle*
- Injury to the **papillary muscles** typically leads to severe **mitral regurgitation**, presenting with acute heart failure symptoms like pulmonary edema rather than primarily hypovolemic shock.
- While possible in trauma, the primary symptoms would involve a new significant murmur and rapid deterioration of cardiac function due to valve incompetence.
*Left main coronary artery*
- A **left main coronary artery** injury would likely lead to acute **myocardial ischemia** or infarction, manifesting as severe chest pain, ECG changes indicative of ischemia, and potentially cardiogenic shock, not hypovolemic shock.
- While trauma to the chest can cause coronary artery dissection, it is less common for blunt force to directly injure this artery without other, more widespread myocardial damage.
*Inferior vena cava*
- An injury to the **inferior vena cava (IVC)** would primarily cause severe internal bleeding, leading to hypovolemic shock. However, while possible, blunt force trauma to the chest is less likely to directly injure the retroperitoneal IVC without significant associated abdominal or lumbar spine injuries.
- The chest wall hematoma and focus on the chest suggests damage within the thoracic cavity, making an aortic injury more probable given the mechanism.
*Aortic valve*
- An injury to the **aortic valve** could cause acute **aortic regurgitation**, leading to acute heart failure and potentially cardiogenic shock with a new diastolic murmur.
- While possible, pure aortic valve injury from blunt trauma alone, without rupture of the aorta itself, is less common than aortic tear from shearing forces.
Mechanical complications management US Medical PG Question 4: A 67-year-old man presents to the emergency department with a 1-hour history of nausea and upper abdominal and substernal chest pain radiating to his lower jaw. He vomited several times before arriving at the hospital. His last visit to the primary care physician was 6 months ago during which he complained of fatigue, ‘slowing down’ on his morning walks, and abdominal pain that exacerbated by eating spicy food. His current medications include atorvastatin, metformin, insulin, omeprazole, aspirin, enalapril, nitroglycerin, and metoprolol. Today, his blood pressure is 95/72 mm Hg in his right arm and 94/73 in his left arm, heart rate is 110/min, temperature is 37.6°C (99.6°F), and respiratory rate is 30/min. On physical examination, he is diaphoretic and his skin is cool and clammy. His cardiac enzymes were elevated. He is treated appropriately and is admitted to the hospital. On day 5 of his hospital stay, he suddenly develops breathlessness. His blood pressure drops to 80/42 mm Hg. On examination, bibasilar crackles are heard. Cardiac auscultatory reveals a high pitched holosystolic murmur over the apex. Which of the following most likely lead to the deterioration of this patient’s condition?
- A. Scarring of mitral valve as a complication of childhood illness
- B. Ballooning of mitral valve into the left atrium
- C. Age-related fibrosis and calcification of the aortic valve
- D. Papillary muscle rupture leading to reflux of blood into left atrium (Correct Answer)
- E. Aortic root dilation
Mechanical complications management Explanation: **Papillary muscle rupture leading to reflux of blood into left atrium**
- The patient's initial presentation with chest pain, nausea, and elevated cardiac enzymes is consistent with an acute **myocardial infarction (MI)**. The sudden breathlessness, drop in blood pressure, bibasilar crackles (indicating **pulmonary edema**), and a **new holosystolic murmur over the apex** suggest acute **mitral regurgitation**, a common mechanical complication of MI.
- **Papillary muscle rupture**, particularly of the posterior medial papillary muscle due to its single blood supply from the posterior descending artery (often involved in inferior MIs), can lead to severe acute mitral regurgitation, causing rapid hemodynamic deterioration and **cardiogenic shock**.
*Scarring of mitral valve as a complication of childhood illness*
- **Rheumatic heart disease**, typically resulting from childhood illnesses like **streptococcal pharyngitis**, can cause mitral valve scarring (often **mitral stenosis** or chronic regurgitation). However, this would be a pre-existing condition and less likely to cause a sudden, acute decompensation solely on day 5 post-MI.
- While it can lead to cardiac issues, the sudden onset of symptoms and their direct association with a recent MI point away from a chronic, pre-existing valvular condition as the primary cause of acute decompensation.
*Ballooning of mitral valve into the left atrium*
- This describes **mitral valve prolapse (MVP)**, which is usually a chronic, benign condition, though it can cause mitral regurgitation.
- Acute, severe mitral regurgitation leading to cardiogenic shock post-MI is more characteristic of structural damage like papillary muscle rupture rather than the typical progression of MVP.
*Age-related fibrosis and calcification of the aortic valve*
- This describes **aortic stenosis**, a chronic condition characterized by obstruction of blood flow from the left ventricle.
- Aortic stenosis typically presents with a **systolic ejection murmur** best heard at the right upper sternal border, radiating to the carotids, and symptoms like angina, syncope, and dyspnea, which are different from the patient's acute presentation of a **holosystolic murmur at the apex** and pulmonary edema.
*Aortic root dilation*
- **Aortic root dilation** can lead to **aortic regurgitation**, characterized by a **diastolic decrescendo murmur**.
- While causes of aortic root dilation can include hypertension, Marfan syndrome, or syphilis, it does not explain a **holosystolic murmur at the apex** or acute mitral regurgitation secondary to an MI.
Mechanical complications management US Medical PG Question 5: An 80-year-old woman died due to the respiratory complications of lung cancer. She had been a heavy smoker, and battled COPD and adenocarcinoma of the lungs for the last 20 years. The autopsy also revealed a pathological finding in the mitral valve. Which of the following was most likely seen?
- A. Ruptured papillary muscle
- B. Destructive vegetations
- C. Discoloration of leaflets
- D. Stenosis of leaflets
- E. Non-destructive vegetations (Correct Answer)
Mechanical complications management Explanation: ***Non-destructive vegetations***
- The patient's age (80 years old), history of **lung cancer**, and prolonged illness are all factors associated with **non-bacterial thrombotic endocarditis (NBTE)**.
- NBTE, also known as **marantic endocarditis**, involves the formation of sterile, non-destructive vegetations on heart valves, commonly linked to **malignancy** and **hypercoagulable states**.
*Ruptured papillary muscle*
- This is typically a complication of an **acute myocardial infarction**, not specifically associated with cancer or COPD.
- Would lead to **acute severe mitral regurgitation**, presenting with more acute cardiac symptoms.
*Destructive vegetations*
- **Destructive vegetations** are characteristic of **infective endocarditis**, which typically presents with fever, new murmurs, and signs of infection, none of which are mentioned.
- There is no indication of bacterial infection or other conditions predisposing to infective endocarditis.
*Discoloration of leaflets*
- While other forms of valve disease or post-mortem changes might cause discoloration, it is not a specific pathological finding related to the patient's underlying conditions in the way that NBTE vegetations are.
- Discoloration alone does not represent a primary disease process of the valve.
*Stenosis of leaflets*
- **Mitral stenosis** is more commonly caused by **rheumatic heart disease** or age-related calcification, which is not indicated by the patient's history.
- While severe calcification can occur with age, the presence of **malignancy** and prolonged illness points more strongly to NBTE.
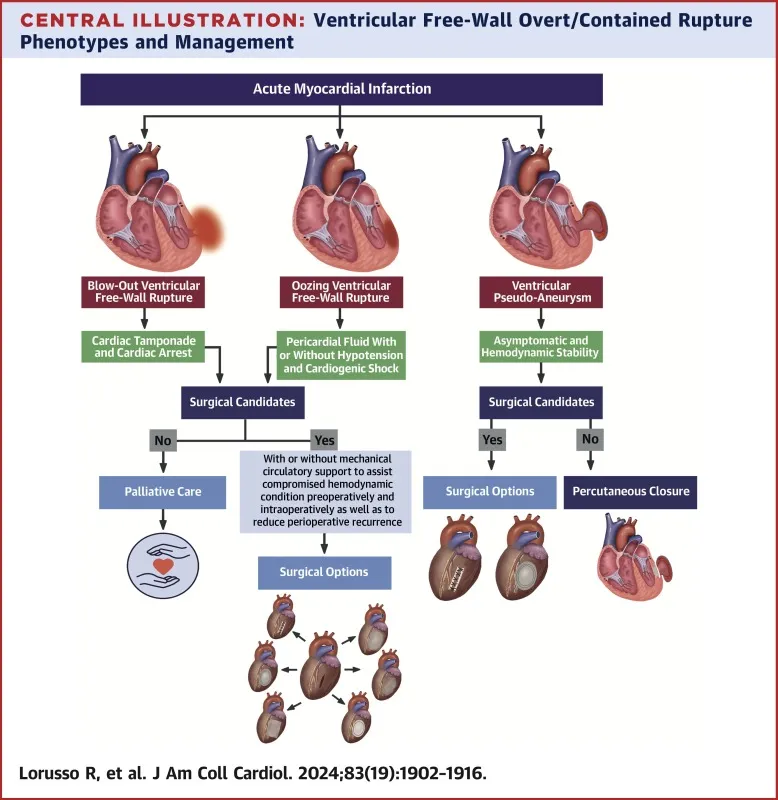
Mechanical complications management US Medical PG Question 6: A 66-year-old female with hypertension and a recent history of acute ST-elevation myocardial infarction (STEMI) 6 days previous, treated with percutaneous transluminal angioplasty (PTA), presents with sudden onset chest pain, shortness of breath, diaphoresis, and syncope. Vitals are temperature 37°C (98.6°F), blood pressure 80/50 mm Hg, pulse 125/min, respirations 12/min, and oxygen saturation 92% on room air. On physical examination, the patient is pale and unresponsive. Cardiac exam reveals tachycardia and a pronounced holosystolic murmur loudest at the apex and radiates to the back. Lungs are clear to auscultation. Chest X-ray shows cardiomegaly with clear lung fields. ECG is significant for ST elevations in the precordial leads (V2-V4) and low-voltage QRS complexes. Emergency transthoracic echocardiography shows a left ventricular wall motion abnormality along with a significant pericardial effusion. The patient is intubated, and aggressive fluid resuscitation is initiated. What is the next best step in management?
- A. Immediate cardiac catheterization
- B. Immediate transfer to the operating room (Correct Answer)
- C. Emergency pericardiocentesis
- D. Intra-aortic balloon counterpulsation
- E. Administer dobutamine 5-10 mcg/kg/min IV
Mechanical complications management Explanation: ***Immediate transfer to the operating room***
- The patient's presentation with sudden onset chest pain, shortness of breath, profound cardiogenic shock, and a new **holosystolic murmur at the apex radiating to the back** in the context of a recent **STEMI**, strongly suggests **acute papillary muscle rupture** causing severe mitral regurgitation. This is a surgical emergency requiring immediate intervention.
- The holosystolic murmur at the apex is pathognomonic for acute mitral regurgitation, distinguishing this from ventricular free wall rupture (which would present with tamponade physiology without a murmur).
- The patient requires urgent surgical repair (mitral valve replacement or repair) to address this mechanical complication of **myocardial infarction (MI)**, which is causing severe hemodynamic compromise.
*Immediate cardiac catheterization*
- While cardiac catheterization is essential for diagnosing coronary artery disease and revascularization, in this emergent situation with profound shock and a mechanical complication (papillary muscle rupture), the primary issue is structural cardiac damage requiring surgical repair, not ongoing ischemia alone.
- Delaying surgical intervention for catheterization in this hemodynamically unstable patient would be detrimental and potentially fatal.
*Emergency pericardiocentesis*
- Although there is a **pericardial effusion** on echocardiography, the patient's presentation with a new holosystolic murmur and profound shock after STEMI indicates **papillary muscle rupture with acute mitral regurgitation**, not cardiac tamponade.
- The presence of a loud murmur excludes ventricular free wall rupture as the primary cause. The effusion is likely reactive or incidental.
- Pericardiocentesis would not address the underlying mitral valve pathology causing the hemodynamic collapse.
*Intra-aortic balloon counterpulsation*
- **Intra-aortic balloon pump (IABP)** can improve cardiac output and reduce afterload, which may provide temporary hemodynamic support in cardiogenic shock.
- However, in cases of **papillary muscle rupture** with severe acute mitral regurgitation, IABP provides only temporary support and does not fix the underlying structural problem.
- It could be considered as a bridge to surgery, but the definitive treatment is surgical repair, which should be expedited without delay.
*Administer dobutamine 5-10 mcg/kg/min IV*
- **Dobutamine** is an inotrope that increases cardiac contractility. While it might improve cardiac output in some forms of cardiogenic shock, in the setting of **acute severe mitral regurgitation from papillary muscle rupture**, it cannot resolve the structural valvular incompetence.
- Increasing contractility may paradoxically worsen the regurgitant fraction and further compromise forward cardiac output.
- Medical management alone cannot resolve this mechanical complication, necessitating urgent surgical intervention.
Mechanical complications management US Medical PG Question 7: Two days after being admitted for acute myocardial infarction, a 61-year-old man has sharp, substernal chest pain that worsens with inspiration and improves when leaning forward. Cardiac examination shows a scratchy sound best heard over the left sternal border. Histopathological examination of the infarcted myocardial tissue is most likely to show which of the following findings?
- A. Neutrophilic infiltration
- B. Collagenous scar tissue
- C. Normal myocardium
- D. Coagulative necrosis (Correct Answer)
- E. Granulation tissue with macrophages
Mechanical complications management Explanation: ***Coagulative necrosis***
- The patient's clinical presentation (sharp, substernal chest pain, worsening with inspiration, improving while leaning forward, and a scratchy pericardial friction rub) indicates **post-MI fibrinous pericarditis**, a common complication occurring 2-4 days after myocardial infarction.
- At **day 2 post-MI**, the infarcted myocardium demonstrates **coagulative necrosis** as the primary and most characteristic histopathological finding, representing irreversible ischemic cell death with preserved tissue architecture.
- While neutrophilic infiltration is also present at this timepoint, coagulative necrosis of the cardiomyocytes themselves is the defining pathological feature that distinguishes irreversible myocardial injury.
*Neutrophilic infiltration*
- **Neutrophilic infiltration** is indeed present at day 2 post-MI (peaks at days 1-3) as part of the acute inflammatory response to clear necrotic debris.
- However, neutrophils represent the **reactive inflammatory response** rather than the primary pathological change in the infarcted cardiomyocytes themselves.
- The question asks about the most characteristic histopathological finding, which is the **coagulative necrosis** of the myocardial cells, not the secondary inflammatory infiltrate.
*Collagenous scar tissue*
- **Collagenous scar tissue** forms much later during the remodeling phase, typically **7 weeks or more** after MI, representing the final stage of healing.
- At day 2, the tissue is still in the acute phase of coagulative necrosis and early inflammation, far too early for mature fibrous scar formation.
*Normal myocardium*
- The patient has sustained an **acute myocardial infarction** with irreversible injury to cardiac tissue.
- Histopathological examination of the infarcted region would show clear abnormalities, not **normal myocardium**.
*Granulation tissue with macrophages*
- **Granulation tissue** with fibroblasts, new capillaries, and macrophages begins forming during the proliferative phase, typically starting around **days 5-7** post-MI.
- At day 2, it is too early for granulation tissue formation; the tissue is still dominated by coagulative necrosis and acute neutrophilic inflammation.
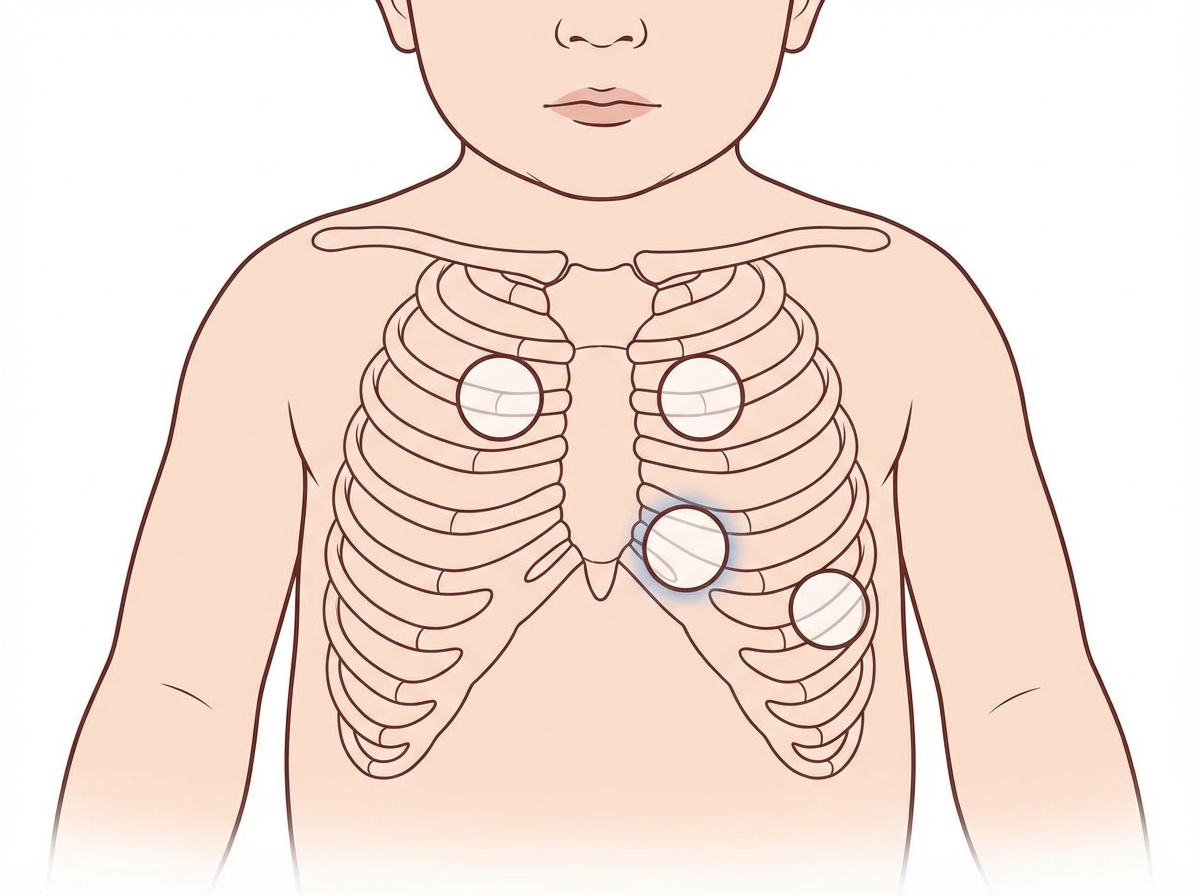
Mechanical complications management US Medical PG Question 8: A 7-year-old boy is brought to the pediatrician by his parents for a routine checkup. The parents note that the patient recently joined a baseball team and has had trouble keeping up with his teammates and gets short of breath with exertion. The patient has otherwise been healthy and has no known history of asthma or allergic reaction. Today, the patient’s temperature is 98.2°F (36.8°C), blood pressure is 112/72 mmHg, pulse is 70/min, and respirations are 12/min. The physical exam is notable for a heart murmur that decreases when the patient bears down. Additionally, the hand grip and rapid squatting maneuvers increase the severity of the murmur. Which of the following is likely heard on auscultation?
- A. Continuous murmur inferior to the left clavicle
- B. Holosystolic murmur at the apex radiating to the axilla
- C. Crescendo-decrescendo systolic murmur radiating to carotids
- D. Late systolic murmur with a midsystolic click
- E. Holosystolic murmur at the lower left sternal border (Correct Answer)
Mechanical complications management Explanation: ***Holosystolic murmur at the lower left sternal border***
- This presentation is classic for a **ventricular septal defect (VSD)**, which is the most common congenital heart defect. The murmur is **holosystolic** and best heard at the **lower left sternal border**.
- The key physiological findings support VSD: the murmur **decreases with Valsalva** (decreased venous return → decreased left-to-right shunt) and **increases with handgrip and squatting** (increased systemic vascular resistance → increased left-to-right shunt across the defect).
- **Exertional dyspnea** in a previously healthy child can occur with moderate-sized VSDs due to increased pulmonary blood flow. Small VSDs may be asymptomatic until increased activity demands reveal the limitation.
*Continuous murmur inferior to the left clavicle*
- This describes a **patent ductus arteriosus (PDA)**, which produces a continuous **"machinery-like" murmur** heard best in the infraclavicular area and under the left clavicle.
- While PDA can cause exertional symptoms, the murmur characteristics don't match the holosystolic pattern described, and the dynamic maneuver responses differ from this case.
*Holosystolic murmur at the apex radiating to the axilla*
- This is the classic presentation of **mitral regurgitation**. The murmur would **increase with squatting** (increased preload), but the location (apex radiating to axilla) doesn't match the lower left sternal border location described.
- Mitral regurgitation is uncommon in otherwise healthy children without rheumatic disease or structural abnormalities.
*Crescendo-decrescendo systolic murmur radiating to carotids*
- This describes **aortic stenosis**, which produces an **ejection systolic murmur** that radiates to the carotids.
- Aortic stenosis has a crescendo-decrescendo (ejection) pattern, not holosystolic, and the location and radiation pattern don't match this patient's findings.
*Late systolic murmur with a midsystolic click*
- This is pathognomonic for **mitral valve prolapse (MVP)**. In MVP, the click and murmur **move earlier and become louder with Valsalva** (decreased ventricular volume allows earlier prolapse), which is opposite to this patient's findings.
- MVP is the opposite response: louder with Valsalva, softer with squatting.
Mechanical complications management US Medical PG Question 9: A 50-year-old man presents the emergency department for intense chest pain, profuse sweating, and shortness of breath. The onset of these symptoms was 3 hours ago. The chest pain began after a heated discussion with a colleague at the community college where he is employed. Upon arrival, he is found conscious and responsive; the vital signs include a blood pressure of 130/80 mm Hg, a heart rate at 90/min, a respiratory rate at 20/min, and a body temperature of 36.4°C (97.5°F). His medical history is significant for hypertension diagnosed 7 years ago, which is well-controlled with a calcium channel blocker. The initial electrocardiogram (ECG) shows ST-segment depression in multiple consecutive leads, an elevated cardiac troponin T level, and normal kidney function. Which of the following would you expect to find in this patient?
- A. Subendocardial necrosis (Correct Answer)
- B. Transmural necrosis
- C. Incomplete occlusion of a coronary artery
- D. Coronary artery spasm
- E. Ventricular pseudoaneurysm
Mechanical complications management Explanation: ***Subendocardial necrosis***
- This patient's presentation with **ST-segment depression** and **elevated troponin T** indicates a **Non-ST-segment Elevation Myocardial Infarction (NSTEMI)**, which typically results from subendocardial ischemia and necrosis.
- Subendocardial tissue is most vulnerable to ischemia due to its high oxygen demand and distal location from the coronary arteries, making it the first region to suffer damage when oxygen supply is compromised.
*Transmural necrosis*
- **Transmural necrosis** is characteristic of a **ST-segment Elevation Myocardial Infarction (STEMI)**, which presents with persistent **ST-segment elevation** on ECG.
- This patient's ECG shows **ST-segment depression**, ruling out transmural involvement at the time of presentation.
*Incomplete occlusion of a coronary artery*
- While an NSTEMI usually involves an **incomplete occlusion** or **critical stenosis** of a coronary artery, the question asks what would be *found* in the patient's heart tissue, not the mechanism.
- The direct tissue consequence of incomplete occlusion leading to NSTEMI is **subendocardial necrosis**, which is a more specific answer about the pathological finding.
*Coronary artery spasm*
- Although **coronary artery spasm (Prinzmetal angina)** can cause chest pain and ECG changes, it typically presents with **transient ST-segment elevation** (not depression) and often resolves spontaneously.
- The elevated troponin T indicates myocardial necrosis, which is not typically a feature of uncomplicated coronary artery spasm, and the duration of symptoms (3 hours) suggests a more sustained event than a transient spasm.
*Ventricular pseudoaneurysm*
- A **ventricular pseudoaneurysm** is a **late complication of myocardial infarction**, typically occurring weeks to months after the acute event, due to rupture of the ventricular free wall contained by pericardium.
- Given the 3-hour symptom onset, it is highly unlikely to be present in the acute phase of myocardial infarction.
Mechanical complications management US Medical PG Question 10: An 80-year-old man presents to the emergency department because of gnawing substernal chest pain that started an hour ago and radiates to his neck and left jaw. A 12-lead ECG is obtained and shows ST-segment elevation with newly developing Q waves. He is admitted for treatment. 4 days after hospitalization he suddenly develops altered mental status, and his blood pressure falls from 115/75 mm Hg to 80/40 mm Hg. Physical examination shows jugular venous distention, pulsus paradoxus, and distant heart sounds. What is the most likely cause of this patient's condition?
- A. Pericardial inflammation
- B. Compression of heart chambers by blood in the pericardial space (Correct Answer)
- C. Arrhythmia caused by ventricular fibrillation
- D. Rupture of papillary muscle
- E. Acute pulmonary edema from left heart failure
Mechanical complications management Explanation: ***Compression of heart chambers by blood in the pericardial space***
- The patient's initial presentation with ST-elevation myocardial infarction (STEMI) and subsequent development of **hypotension**, **jugular venous distention**, **pulsus paradoxus**, and **distant heart sounds** (Beck's triad) is highly indicative of **cardiac tamponade.**
- In the context of a recent MI, this constellation of symptoms strongly suggests a **cardiac free wall rupture**, leading to blood accumulation in the pericardial sac and compression of the heart.
- Free wall rupture typically occurs **3-7 days post-MI** and is a life-threatening mechanical complication.
*Pericardial inflammation*
- While pericardial inflammation (pericarditis) can occur post-MI, it typically manifests with **pleuritic chest pain** that is relieved by leaning forward and is often associated with a **pericardial friction rub.**
- It does not typically lead to acute, severe hypotension, pulsus paradoxus, or sudden circulatory collapse in this manner without significant effusion and tamponade physiology.
*Arrhythmia caused by ventricular fibrillation*
- **Ventricular fibrillation** would cause immediate cardiac arrest and loss of consciousness, not a gradual development of hypotension, JVD, and pulsus paradoxus.
- While arrhythmias are common post-MI, the specific physical findings point away from isolated VFib as the primary cause of hemodynamic collapse.
*Acute pulmonary edema from left heart failure*
- **Acute pulmonary edema** is a manifestation of **left heart failure**, characterized by severe dyspnea, orthopnea, and crackles on lung auscultation.
- While left heart failure can cause hypotension in cardiogenic shock, it would not typically present with the classic signs of cardiac tamponade such as pulsus paradoxus, distant heart sounds, and prominent JVD without pulmonary congestion findings.
*Rupture of papillary muscle*
- **Papillary muscle rupture** leads to severe **acute mitral regurgitation**, causing acute pulmonary edema, a new holosystolic murmur, and often cardiogenic shock.
- While it can lead to hypotension, it doesn't typically present with the classic signs of cardiac tamponade such as pulsus paradoxus and distant heart sounds; instead, a loud murmur would be prominent.
More Mechanical complications management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.