Cardiogenic shock management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiogenic shock management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
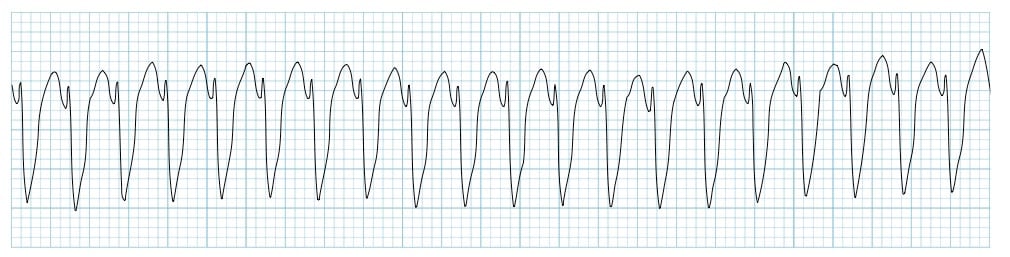
Cardiogenic shock management US Medical PG Question 1: Two days after admission for myocardial infarction and subsequent coronary angioplasty, a 65-year-old man becomes distressed and diaphoretic in the cardiac intensive care unit. Suddenly he is no longer responsive. Pulse oximetry does not show a tracing. He has a history of hypertension and depression. Prior to his admission, his medication included ramipril and aripiprazole. Examination shows no carotid pulse. An ECG is shown. After beginning chest compressions, which of the following is the most appropriate step in management of the patient?
- A. Intravenous procainamide
- B. Cardiac catheterization
- C. Intravenous amiodarone
- D. Intravenous magnesium sulfate
- E. Defibrillation (Correct Answer)
Cardiogenic shock management Explanation: ***Defibrillation***
- The ECG shows a **wide complex tachycardia** consistent with either **ventricular fibrillation (VF)** or **pulseless ventricular tachycardia (VT)**.
- In a patient who is **unresponsive and pulseless**, both VF and pulseless VT are treated identically with **immediate unsynchronized defibrillation** after initiating CPR, according to **ACLS guidelines**.
- **Defibrillation** is the definitive treatment to restore a perfusing rhythm and is the priority intervention after chest compressions have begun.
*Intravenous procainamide*
- **Procainamide** is an antiarrhythmic drug used for certain types of **stable ventricular tachycardia** or wide-complex tachycardia of uncertain type when the patient has a pulse.
- It is **contraindicated** in pulseless arrhythmias like VF or pulseless VT, where electrical therapy (defibrillation) is paramount.
- Administration would cause dangerous delay in definitive treatment.
*Cardiac catheterization*
- **Cardiac catheterization** is an invasive diagnostic and interventional procedure typically performed to evaluate and treat coronary artery disease.
- It is **not an immediate life-saving intervention** for a patient in **cardiac arrest**, which requires immediate electrical therapy.
- Catheterization may be considered after return of spontaneous circulation (ROSC) to address underlying ischemia.
*Intravenous amiodarone*
- **Amiodarone** is an antiarrhythmic agent used in **VF/pulseless VT that is refractory to initial defibrillation attempts** and after epinephrine administration.
- It is administered **after initial defibrillation attempts have failed**, not as the primary or first-line treatment.
- The ACLS algorithm recommends amiodarone after the third shock if VF/pulseless VT persists.
*Intravenous magnesium sulfate*
- **Magnesium sulfate** is the treatment of choice for **Torsades de Pointes**, a polymorphic ventricular tachycardia often associated with **prolonged QT interval**.
- The clinical presentation and ECG do not suggest Torsades de Pointes, and magnesium is not indicated as the initial treatment for VF or monomorphic VT.
- Magnesium may also be considered for refractory VF/VT with suspected hypomagnesemia.
Cardiogenic shock management US Medical PG Question 2: A 40-year-old Caucasian male presents to the emergency room after being shot in the arm in a hunting accident. His shirt is soaked through with blood. He has a blood pressure of 65/40, a heart rate of 122, and his skin is pale, cool to the touch, and moist. This patient is most likely experiencing all of the following EXCEPT:
- A. Decreased sarcomere length in the myocardium
- B. Increased stroke volume (Correct Answer)
- C. Confusion and irritability
- D. Decreased preload
- E. Increased thromboxane A2
Cardiogenic shock management Explanation: ***Increased stroke volume***
- The patient is experiencing **hypovolemic shock** due to significant blood loss, meaning their **cardiac output** is severely compromised.
- In shock, the heart attempts to compensate by increasing **heart rate**, but **stroke volume** is typically decreased due to reduced **preload**.
*Decreased sarcomere length in the myocardium*
- In situations of significant blood loss and **decreased preload**, there is less venous return to the heart, leading to reduced end-diastolic volume.
- According to the **Frank-Starling law**, reduced end-diastolic volume results in shorter initial sarcomere length, which reduces the force of contraction and thus, **stroke volume**.
*Confusion and irritability*
- **Hypovolemic shock** leads to widespread **tissue hypoperfusion**, especially to vital organs like the brain.
- Reduced cerebral blood flow results in impaired brain function, manifesting as **confusion, irritability**, and altered mental status.
*Decreased preload*
- Significant blood loss leads to a reduction in the **total circulating blood volume**.
- This reduction directly decreases the venous return to the heart, thus lowering the **end-diastolic volume** and subsequently, the **preload**.
*Increased thromboxane A2*
- In response to **vascular injury and bleeding**, the body initiates hemostasis, a critical component of which is platelet aggregation.
- **Thromboxane A2** is a potent vasoconstrictor and platelet aggregator released by activated platelets to form a **platelet plug** and help stop bleeding.
Cardiogenic shock management US Medical PG Question 3: A 27-year-old man is brought to the emergency department 30 minutes after being shot in the abdomen during a violent altercation. His temperature is 36.5°C (97.7°F), pulse is 118/min and regular, and blood pressure is 88/65 mm Hg. Examination shows cool extremities. Abdominal examination shows a 2.5-cm entrance wound in the left upper quadrant at the midclavicular line, below the left costal margin. Focused ultrasound shows free fluid in the left upper quadrant. Which of the following sets of hemodynamic changes is most likely in this patient?
Cardiac output (CO) | Pulmonary capillary wedge pressure (PCWP) | Systemic vascular resistance (SVR) | Central venous pressure (CVP)
- A. ↑ ↓ ↓ ↓
- B. ↓ ↓ ↑ ↑
- C. ↓ ↓ ↓ ↓
- D. ↓ ↓ ↑ ↓ (Correct Answer)
- E. ↓ ↑ ↑ ↑
Cardiogenic shock management Explanation: ***↓ ↓ ↑ ↓***
- This patient is in **hypovolemic shock** due to hemorrhage, leading to decreased **cardiac output (CO)** and **pulmonary capillary wedge pressure (PCWP)** due to reduced preload.
- The body compensates for hypovolemia by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, while **central venous pressure (CVP)** decreases due to the depleted blood volume.
*↑ ↓ ↓ ↓*
- An increased **cardiac output** is inconsistent with hypovolemic shock, where the heart's ability to pump blood is compromised by a lack of circulating volume.
- While **PCWP**, **SVR**, and **CVP** decreasing could be seen in some forms of shock, the elevated CO rules out hypovolemic shock.
*↓ ↓ ↑ ↑*
- An elevated **central venous pressure (CVP)** is inconsistent with hypovolemic shock, as CVP reflects right atrial pressure and would be low due to decreased blood volume.
- While other parameters such as **CO** and **PCWP** decreasing and **SVR** increasing can be seen in hypovolemic shock, the increased CVP suggests a different hemodynamic state, like cardiogenic shock.
*↓ ↓ ↓ ↓*
- A decrease in **systemic vascular resistance (SVR)** is characteristic of **distributive shock** (e.g., septic or neurogenic shock), not hypovolemic shock, where compensatory vasoconstriction would lead to increased SVR.
- While **CO**, **PCWP**, and **CVP** would decrease due to overall poor perfusion, the SVR response differentiates it from hypovolemic shock.
*↓ ↑ ↑ ↑*
- An elevated **pulmonary capillary wedge pressure (PCWP)** and **central venous pressure (CVP)** indicate increased fluid volume or cardiac dysfunction, which is contrary to the reduced preload seen in hypovolemic shock.
- While **cardiac output (CO)** may decrease in cardiogenic shock, the other elevated pressures point away from a primary hypovolemic cause.
Cardiogenic shock management US Medical PG Question 4: A 72-year-old man is taken to the emergency room after losing consciousness. According to his wife, he suddenly complained of fluttering in his chest, lightheadedness, and profuse sweating while walking to the grocery store. He then turned gray, lost consciousness, and collapsed onto the ground. His medical history is significant for a prior anterior wall myocardial infarction 2 years ago that was complicated by severe left ventricular systolic dysfunction. His blood pressure is 80/50 mm Hg, the temperature is 36.7°C (98.0°F), and the carotid pulse is not palpable. An ECG was obtained and the results are shown in the picture. Cardiopulmonary resuscitation is initiated and the patient is cardioverted to sinus rhythm with an external defibrillator. The patient regains consciousness and states there was no antecedent chest discomfort. Cardiac enzymes are negative and serum electrolytes are normal. Which of the following is the best next step for this patient?
- A. Intravenous magnesium sulphate
- B. Intravenous adenosine
- C. Implantable cardioverter-defibrillator (Correct Answer)
- D. Intravenous metoprolol
- E. Temporary or permanent cardiac pacing
Cardiogenic shock management Explanation: ***Implantable cardioverter-defibrillator***
- The patient experienced **sudden cardiac arrest (SCA)** due to a **lethal ventricular arrhythmia (ventricular tachycardia progressing to ventricular fibrillation)**, suggested by the syncopal episode, unrecordable pulse, and successful defibrillation.
- Given the history of severe **left ventricular systolic dysfunction** (LVEF <35-40%) post-MI, he is at high risk for recurrence, making an **ICD** the most appropriate intervention for secondary prevention of SCA.
*Intravenous magnesium sulphate*
- **Magnesium sulfate** is primarily used for the treatment of **Torsades de Pointes**, a polymorphic VT often associated with a prolonged QT interval.
- The provided ECG (though not visible here, the clinical context implies a monomorphic VT or VF) and history do not specifically suggest Torsades de Pointes.
*Intravenous adenosine*
- **Adenosine** is the drug of choice for terminating **supraventricular tachycardias (SVTs)** by transiently blocking the AV node.
- It is **contraindicated** in wide-complex tachycardias of uncertain origin, especially in patients with structural heart disease, as it can worsen ventricular arrhythmias.
*Intravenous metoprolol*
- **Beta-blockers** like metoprolol are used to slow heart rate, reduce myocardial oxygen demand, and can be helpful in some forms of VT, but they are not the definitive treatment for **hemodynamically unstable** VT or for preventing future SCA in a patient with severe LV dysfunction.
- Administering a beta-blocker during an acute, unstable event could worsen hypotension.
*Temporary or permanent cardiac pacing*
- **Cardiac pacing** is indicated for **bradyarrhythmias** or some forms of **tachycardia** (e.g., overdrive pacing for recurrent VT), but it is not the primary treatment for preventing SCA from ventricular fibrillation in a patient with severe LV dysfunction like this.
- The patient's presentation was due to a fast, lethal arrhythmia, not a slow rhythm.
Cardiogenic shock management US Medical PG Question 5: A 68-year-old woman is brought to the emergency department by ambulance after she was found down by her daughter. She lives alone in her apartment so it is unclear when she began to develop symptoms. Her medical history is significant for cardiac arrhythmias, diabetes, pericarditis, and a stroke 2 years ago. On presentation her temperature is 98.1°F (36.7°C), blood pressure is 88/51 mmHg, pulse is 137/min, and respirations are 18/min. On physical exam her skin is cold and clammy. If special tests were obtained, they would reveal dramatically decreased pulmonary capillary wedge pressure, increased systemic vascular resistance, and mildly decreased cardiac output. Which of the following treatments would most directly target the cause of this patient's low blood pressure?
- A. Vasopressors
- B. Intravenous fluids (Correct Answer)
- C. Antibiotic administration
- D. Relieve obstruction
- E. Intravenous inotropes
Cardiogenic shock management Explanation: ***Intravenous fluids***
- The patient exhibits signs of **hypovolemic shock**, including **hypotension** (BP 88/51 mmHg), **tachycardia** (pulse 137/min), and **cold, clammy skin**. The dramatically decreased **pulmonary capillary wedge pressure (PCWP)** indicates low preload, which is characteristic of hypovolemia.
- Administration of intravenous fluids directly addresses the underlying cause of this patient's low blood pressure by increasing intravascular volume, thereby improving **cardiac preload** and ultimately **cardiac output** and blood pressure.
*Vasopressors*
- While vasopressors can temporarily increase blood pressure by causing **vasoconstriction**, they do not address the root cause of hypovolemic shock, which is insufficient circulating blood volume.
- Using vasopressors without adequate fluid resuscitation in hypovolemic shock can lead to further **organ hypoperfusion** due to increased afterload on an already compromised heart.
*Antibiotic administration*
- Although the patient's presentation with hypotension and tachycardia could raise suspicion for **sepsis**, there is no explicit evidence of infection presented (e.g., fever, focal source).
- The **decreased PCWP** points more strongly towards hypovolemic shock rather than septic shock, where PCWP can be variable or even normal/elevated.
*Relieve obstruction*
- Obstruction, such as in **cardiac tamponade** or **pulmonary embolism**, can cause obstructive shock, which presents with hypotension.
- However, the dramatically **decreased PCWP** is not typically seen in obstructive shock, where PCWP would likely be normal or elevated due to impedance to cardiac filling or outflow.
*Intravenous inotropes*
- **Inotropes** like dobutamine increase myocardial contractility and are primarily indicated in **cardiogenic shock** or severe heart failure with reduced ejection fraction to improve cardiac output.
- While cardiac output is mildly decreased, the primary issue is reduced preload as indicated by the very low PCWP, making fluid resuscitation a more appropriate initial step than directly increasing contractility.
Cardiogenic shock management US Medical PG Question 6: A 71-year-old woman with a past medical history of type 2 diabetes, hypercholesterolemia, and hypertension was admitted to the hospital 8 hours ago with substernal chest pain for management of acute non-ST-elevated myocardial infarction (NSTEMI). The ECG findings noted by ST-depressions and T-wave inversions on anterolateral leads, which is also accompanied by elevated cardiac enzymes. Upon diagnosis, management with inhaled oxygen therapy, beta-blockers and aspirin, and low-molecular-weight heparin therapy were initiated, and she was placed on bed rest with continuous electrocardiographic monitoring. Since admission, she required 2 doses of sublingual nitroglycerin for recurrent angina, and the repeat troponin levels continued to rise. Given her risk factors, plans were made for early coronary angiography. The telemetry nurse calls the on-call physician because of her concern with the patient's mild confusion and increasing need for supplemental oxygen. At bedside evaluation, The vital signs include: heart rate 122/min, blood pressure 89/40 mm Hg, and the pulse oximetry is 91% on 6L of oxygen by nasal cannula. The telemetry and a repeat ECG show sinus tachycardia. She is breathing rapidly, appears confused, and complains of shortness of breath. On physical exam, the skin is cool and clammy and appears pale and dull. She has diffuse bilateral pulmonary crackles, and an S3 gallop is noted on chest auscultation with no new murmurs. She has jugular venous distention to the jaw-line, rapid and faint radial pulses, and 1+ dependent edema. She is immediately transferred to the intensive care unit for respiratory support and precautions for airway security. The bedside sonography shows abnormal hypodynamic anterior wall movement and an ejection fraction of 20%, but no evidence of mitral regurgitation or ventricular shunt. The chest X-ray demonstrates cephalization of pulmonary veins and pulmonary edema. What is the most appropriate next step in the stabilization of this patient?
- A. Obtain blood cultures and start preliminary broad-spectrum antibiotics
- B. Start intravenous fluids and epinephrine therapy
- C. Intubate the patient and perform an emergency cardiocentesis
- D. Initiate dopamine therapy and diuresis (Correct Answer)
- E. Insert two large-bore intravenous catheters and start rapid fluid resuscitation
Cardiogenic shock management Explanation: ***Initiate dopamine therapy and diuresis***
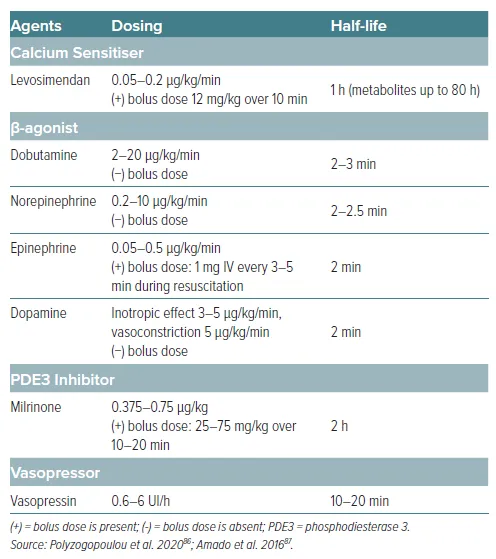
- This patient is presenting with **cardiogenic shock** secondary to extensive NSTEMI, characterized by **hypotension**, signs of **end-organ hypoperfusion** (confusion, cool clammy skin), **pulmonary edema** (crackles, dyspnea, elevated jugular venous pressure), and **severely reduced ejection fraction**. Dopamine is a vasopressor that can increase cardiac output and blood pressure.
- **Diuresis** with loop diuretics such as furosemide is crucial to reduce the fluid overload contributing to the pulmonary edema and jugular venous distention.
*Obtain blood cultures and start preliminary broad-spectrum antibiotics*
- While infection is a concern in critically ill patients, there are **no signs of infection** in this clinical presentation. The patient's symptoms are clearly attributable to acute cardiac decompensation.
- A delay in treating cardiogenic shock to investigate for infection would be detrimental and potentially fatal.
*Start intravenous fluids and epinephrine therapy*
- Intravenous fluids would **worsen the existing pulmonary edema and fluid overload** in a patient with an ejection fraction of 20% and clinical signs of volume overload (crackles, JVD, S3 gallop).
- Epinephrine is a potent vasopressor but is generally reserved for more severe shock refractory to other inotropes, or in cases of **cardiac arrest**, not typically first-line for cardiogenic shock with significant pulmonary congestion.
*Intubate the patient and perform an emergency cardiocentesis*
- While the patient is confused and has respiratory distress, **intubation** should be considered after hemodynamic stabilization, if respiratory failure persists or worsens.
- **Cardiocentesis** is indicated for **cardiac tamponade**, which is not supported by the absence of an effusion on bedside sonography and the finding of hypodynamic anterior wall movement, which points to pump failure.
*Insert two large-bore intravenous catheters and start rapid fluid resuscitation*
- This patient is in **cardiogenic shock with clear evidence of fluid overload**, including pulmonary edema and elevated jugular venous pressure.
- **Rapid fluid resuscitation would exacerbate heart failure** and worsen respiratory compromise due to increased preload.
Cardiogenic shock management US Medical PG Question 7: A 70-year-old man with diabetes, hypertension, and chronic kidney disease (eGFR 35 mL/min/1.73m²) presents with NSTEMI. Troponin is elevated at 8.5 ng/mL. ECG shows 2mm ST depression in V2-V5. GRACE score is 165 (high risk). He is hemodynamically stable. Cardiologist recommends early invasive strategy within 24 hours. Nephrologist is concerned about contrast-induced nephropathy potentially requiring dialysis. Patient is on metformin. Evaluate the management strategy integrating multiple specialist perspectives and evidence.
- A. Proceed with angiography within 24 hours using iso-osmolar contrast and intravenous hydration, hold metformin (Correct Answer)
- B. Perform coronary CT angiography as alternative to invasive angiography
- C. Delay catheterization for 72 hours to optimize renal function with hydration
- D. Prophylactic hemodialysis before and after catheterization to remove contrast
- E. Medical management only with dual antiplatelet therapy, avoid catheterization
Cardiogenic shock management Explanation: ***Proceed with angiography within 24 hours using iso-osmolar contrast and intravenous hydration, hold metformin***
- High-risk NSTEMI patients with a **GRACE score >140** benefit from an **early invasive strategy** within 24 hours to reduce ischemic events and mortality.
- Renal protection is maximized through **pre-procedural hydration** and **iso-osmolar contrast**, while **metformin** must be held to avoid the risk of lactic acidosis if acute kidney injury occurs.
*Perform coronary CT angiography as alternative to invasive angiography*
- **Coronary CTA** is primarily used for ruling out coronary artery disease in low-to-intermediate risk stable patients, not for high-risk **NSTEMI**.
- This modality still requires **iodinated contrast** and does not provide the therapeutic benefit of percutaneous coronary intervention (**PCI**).
*Delay catheterization for 72 hours to optimize renal function with hydration*
- Delaying the procedure in a high-risk patient increases the risk of **re-infarction** and **cardiovascular death**, outweighing the minor benefits of prolonged hydration.
- Evidence suggests that optimization of renal status should happen concurrently with the preparation for **early intervention** in high-risk ACS.
*Prophylactic hemodialysis before and after catheterization to remove contrast*
- **Prophylactic hemodialysis** has not been proven to prevent contrast-induced nephropathy and may actually increase the risk of adverse events.
- High-volume **intravenous hydration** with isotonic saline remains the gold standard for preventing renal injury in patients with **CKD**.
*Medical management only with dual antiplatelet therapy, avoid catheterization*
- While **dual antiplatelet therapy** is essential, medical management alone is inferior to an invasive strategy in patients with **high GRACE scores**.
- Avoiding catheterization based solely on **renal impairment** results in "renalism," where patients are undertreated for their life-threatening cardiac condition.
Cardiogenic shock management US Medical PG Question 8: A 58-year-old woman with anterior STEMI underwent primary PCI with drug-eluting stent placement. Post-procedure echocardiogram shows left ventricular ejection fraction of 30% with apical akinesis. She is started on aspirin, ticagrelor, high-intensity statin, and ACE inhibitor. On hospital day 3, she develops atrial fibrillation with rapid ventricular response. CHA2DS2-VASc score is 4. Creatinine is normal. Evaluate the optimal antithrombotic strategy balancing ischemic and bleeding risk.
- A. Triple therapy with aspirin, ticagrelor, and apixaban indefinitely
- B. Triple therapy for 6 months, then aspirin and apixaban indefinitely
- C. Aspirin and ticagrelor only, hold anticoagulation due to bleeding risk
- D. Warfarin with INR 2-3 plus aspirin, discontinue ticagrelor
- E. Triple therapy for 1 month, then apixaban and clopidogrel for 11 months, then apixaban alone (Correct Answer)
Cardiogenic shock management Explanation: ***Triple therapy for 1 month, then apixaban and clopidogrel for 11 months, then apixaban alone***
- In patients with **Atrial Fibrillation** (CHA2DS2-VASc ≥2) undergoing **PCI**, current guidelines recommend minimizing the duration of **triple therapy** (aspirin, P2Y12 inhibitor, and anticoagulant) to 1 week to 1 month to reduce **bleeding risk**.
- Transitioning to **dual therapy** with a **NOAC** (like apixaban) and a P2Y12 inhibitor (preferably **clopidogrel**) for up to 12 months, followed by NOAC monotherapy, provides an optimal balance between preventing **stent thrombosis** and systemic **thromboembolism**.
*Triple therapy with aspirin, ticagrelor, and apixaban indefinitely*
- Indefinite **triple therapy** carries a prohibitively high risk of life-threatening **major bleeding** without added benefit for stroke prevention.
- **Ticagrelor** is generally avoided in triple therapy regimens due to a significantly higher bleeding profile compared to **clopidogrel**.
*Triple therapy for 6 months, then aspirin and apixaban indefinitely*
- **Triple therapy** for 6 months is rarely indicated and significantly increases the risk of **gastrointestinal and intracranial hemorrhage** compared to the 1-month strategy.
- Aspirin is usually discontinued after the first year in favor of **anticoagulant monotherapy**, as the latter is sufficient for both AF and stable CAD protection.
*Aspirin and ticagrelor only, hold anticoagulation due to bleeding risk*
- This approach leaves the patient with a high **CHA2DS2-VASc score of 4** unprotected against **cardioembolic stroke**, which carries high morbidity and mortality.
- Dual antiplatelet therapy (DAPT) alone is significantly less effective than **oral anticoagulants** for stroke prevention in the setting of atrial fibrillation.
*Warfarin with INR 2-3 plus aspirin, discontinue ticagrelor*
- **NOACs** (like apixaban) are now preferred over **Warfarin** for non-valvular AF due to a superior safety profile, including a lower risk of **intracranial hemorrhage**.
- Discontinuing the P2Y12 inhibitor (ticagrelor) immediately post-PCI in favor of aspirin and warfarin significantly increases the risk of **stent thrombosis**.
Cardiogenic shock management US Medical PG Question 9: A 60-year-old man with inferoposterior STEMI presents to a rural hospital. The nearest PCI-capable facility is 3 hours away. He arrives 90 minutes after symptom onset. Blood pressure is 130/85 mmHg, heart rate 88/min, oxygen saturation 96% on room air. He has no contraindications to fibrinolysis. The transfer team can arrive in 30 minutes. Evaluate the evidence-based approach considering time metrics and available resources.
- A. Immediate fibrinolytic therapy followed by transfer (Correct Answer)
- B. Helicopter transfer to reduce transfer time, then primary PCI
- C. Administer half-dose fibrinolytic and transfer for immediate PCI
- D. Fibrinolytic therapy at rural hospital, transfer only if fails
- E. Wait for transfer team and proceed directly to PCI facility
Cardiogenic shock management Explanation: ***Immediate fibrinolytic therapy followed by transfer***
- In a STEMI patient where the expected **door-to-balloon time** exceeds **120 minutes**, and the patient is seen within **12 hours** of symptom onset, **fibrinolytic therapy** is the preferred reperfusion strategy.
- Following fibrinolysis, a **pharmacoinvasive strategy** is recommended, involving a routine transfer to a PCI-capable center for angiography within **3 to 24 hours**.
*Helicopter transfer to reduce transfer time, then primary PCI*
- Even with expedited transport, the distance and total time likely still exceed the recommended **120-minute window** for primary PCI superiority over fibrinolysis.
- Choosing transfer over immediate thrombolysis in a rural setting when delays are significant increases the risk of **myocardial necrosis**.
*Administer half-dose fibrinolytic and transfer for immediate PCI*
- **Half-dose fibrinolytics** are generally only considered in specific subsets like elderly patients (over 75) to reduce **intracranial hemorrhage** risk, which does not apply here.
- Combining half-dose thrombolysis with immediate PCI (facilitated PCI) has not shown superior outcomes and may increase **bleeding complications**.
*Fibrinolytic therapy at rural hospital, transfer only if fails*
- Modern guidelines recommend a **pharmacoinvasive approach**, meaning all patients should be transferred for **coronary angiography** regardless of clinical success of fibrinolysis.
- Waiting only for "failure" (rescue PCI) ignores the benefit of definitive **revascularization** and stabilization provided by routine post-thrombolysis PCI.
*Wait for transfer team and proceed directly to PCI facility*
- Delaying reperfusion for a 3-hour transport window violates the "**time is muscle**" principle, as the patient is currently in the highly time-sensitive **early window** (under 3 hours).
- Failure to administer fibrinolytics when the **PCI-related delay** is over 90-120 minutes is a deviation from standard **STEMI management protocols**.
Cardiogenic shock management US Medical PG Question 10: A 65-year-old man with extensive anterior STEMI underwent PCI 6 hours after symptom onset due to delayed presentation. Peak troponin was significantly elevated. Three days later, he develops progressive dyspnea. Examination reveals a new holosystolic murmur at the apex radiating to the axilla. Echocardiogram shows severe mitral regurgitation with flail posterior leaflet and hyperdynamic left ventricle. Pulmonary capillary wedge pressure tracing shows prominent v waves. He is euvolemic on examination. Analyze this complication to determine timing of intervention.
- A. Immediate surgical mitral valve repair or replacement
- B. Aggressive diuresis and ACE inhibitor, reassess in 2 weeks
- C. Intra-aortic balloon pump with surgery within 24-48 hours (Correct Answer)
- D. Percutaneous mitral valve repair with MitraClip
- E. Medical management with afterload reduction for 6 weeks, then surgery
Cardiogenic shock management Explanation: ***Intra-aortic balloon pump with surgery within 24-48 hours***
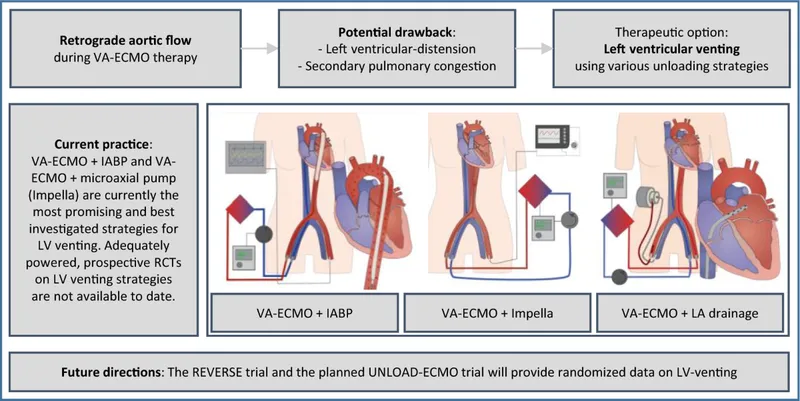
- **Acute papillary muscle rupture** leads to severe mitral regurgitation and hemodynamic instability; an **IABP** provides essential **afterload reduction** and increases forward flow while reducing the regurgitant fraction.
- Providing a brief period of stabilization for 24-48 hours allows for therapeutic optimization before **urgent surgical intervention**, balancing the high risk of immediate surgery with the extreme mortality of medical delay.
*Immediate surgical mitral valve repair or replacement*
- Performing surgery immediately upon diagnosis carries an exceptionally high mortality rate due to the **friable, necrotic myocardial tissue** that is difficult to suture.
- While definitive, Proceeding without initial **hemodynamic stabilization** (like IABP) increases the risk of intraoperative cardiovascular collapse.
*Aggressive diuresis and ACE inhibitor, reassess in 2 weeks*
- This patient has a mechanical complication (flail leaflet); medical management alone for **acute MR** has a mortality rate exceeding 90%.
- **ACE inhibitors** may be poorly tolerated in the acute setting of a large MI if the patient becomes hypotensive, and waiting 2 weeks is far too long for a **mechanical emergency**.
*Percutaneous mitral valve repair with MitraClip*
- **MitraClip** is primarily indicated for chronic secondary MR or in patients with prohibitive surgical risk, rather than as first-line treatment for **acute post-MI papillary muscle rupture**.
- The necrotic and distorted nature of the **subvalvular apparatus** in an acute rupture makes it a poor substrate for percutaneous repair techniques.
*Medical management with afterload reduction for 6 weeks, then surgery*
- Delaying surgery for 6 weeks for "tissue healing" is inappropriate for **papillary muscle rupture** as the patient will likely suffer from progressive **pulmonary edema** or cardiogenic shock.
- While chronic MR can be managed medically, **acute structural failure** requires urgent mechanical correction once stable, not prolonged medical therapy.
More Cardiogenic shock management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.