Biomarker interpretation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Biomarker interpretation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Biomarker interpretation US Medical PG Question 1: A woman with coronary artery disease is starting to go for a walk. As she begins, her heart rate accelerates from a resting pulse of 60 bpm until it reaches a rate of 120 bpm, at which point she begins to feel a tightening in her chest. She stops walking to rest and the tightening resolves. This has been happening to her consistently for the last 6 months. Which of the following is a true statement?
- A. This patient's chest pain is indicative of transmural ischemia
- B. Perfusion of the myocardium takes place equally throughout the cardiac cycle
- C. Increasing the heart rate increases the amount of time spent during each cardiac cycle
- D. Increasing the heart rate decreases the relative amount of time spent during diastole (Correct Answer)
- E. Perfusion of the myocardium takes place primarily during systole
Biomarker interpretation Explanation: ***Increasing the heart rate decreases the relative amount of time spent during diastole***
- With increasing heart rate, the **duration of the cardiac cycle decreases**, but this reduction is disproportionately greater in **diastole (filling phase)** compared to systole (ejection phase), which becomes critical in patients with coronary artery disease as myocardial perfusion occurs during diastole.
- Reduced diastolic time means less time for **coronary artery filling** and **myocardial perfusion**, exacerbating ischemia in the presence of fixed coronary stenosis.
*This patient's chest pain is indicative of transmural ischemia*
- The patient's symptoms are consistent with **stable angina**, characterized by chest pain with exertion that resolves with rest, suggesting **subendocardial ischemia** rather than transmural.
- **Transmural ischemia** typically indicates a more severe, often prolonged, and extensive reduction in blood flow, such as in a **ST-elevation myocardial infarction (STEMI)**.
*Perfusion of the myocardium takes place equally throughout the cardiac cycle*
- Myocardial perfusion is **not equal throughout the cardiac cycle**; it primarily occurs during **diastole** when the heart muscle is relaxed and coronary arteries are less compressed.
- During **systole**, the contracting myocardium compresses the coronary arteries, restricting blood flow, especially to the **subendocardial layers**.
*Increasing the heart rate increases the amount of time spent during each cardiac cycle*
- **Increasing heart rate** by definition **decreases the total duration of each cardiac cycle** (e.g., if heart rate is 60 bpm, cycle duration is 1 second; if 120 bpm, cycle duration is 0.5 seconds).
- While both systole and diastole shorten, the **diastolic phase shortens more significantly**, which is problematic for myocardial perfusion.
*Perfusion of the myocardium takes place primarily during systole*
- **Myocardial perfusion primarily occurs during diastole**, not systole, because the **intramyocardial pressure is lower** and the coronary arteries are less compressed, allowing for better blood flow.
- During **systole**, the high intramyocardial pressure, especially in the left ventricular wall, compresses the coronary vessels, significantly reducing blood flow to the myocardium.
Biomarker interpretation US Medical PG Question 2: A 66-year-old man comes to the emergency department because of a 1-day history of chest pain, palpitations, and dyspnea on exertion. He had a similar episode 3 days ago and was diagnosed with an inferior wall myocardial infarction. He was admitted and a percutaneous transluminal coronary angioplasty was successfully done that day. A fractional flow reserve test during the procedure showed complete resolution of the stenosis. Laboratory tests including serum glucose, lipids, and blood count were within normal limits. He was discharged the day after the procedure on a drug regimen of aspirin, simvastatin, and isosorbide dinitrate. At the time of discharge, he had no chest pain or dyspnea. Presently, his vitals are normal and ECG at rest shows new T-wave inversion. Which of the following is the most reliable test for rapidly establishing the diagnosis in this patient?
- A. Creatine kinase MB
- B. Lactate dehydrogenase
- C. Copeptin
- D. Aspartate aminotransferase
- E. Cardiac troponin T (Correct Answer)
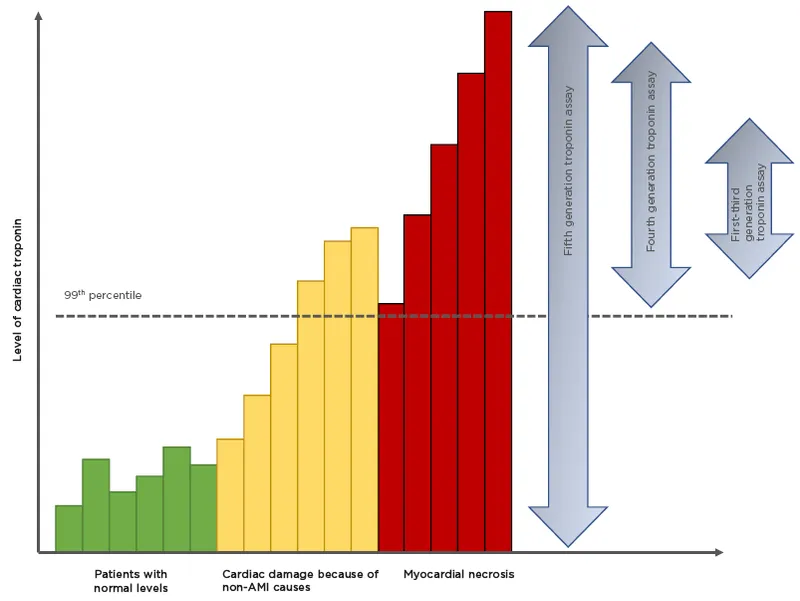
Biomarker interpretation Explanation: ***Cardiac troponin T***
- **Cardiac troponin T** is a highly sensitive and specific biomarker for **myocardial injury**, making it the most reliable test for rapidly diagnosing acute coronary syndrome or re-infarction.
- Its elevation indicates ongoing **myocardial necrosis**, even after a recent MI, and is crucial for guiding immediate management.
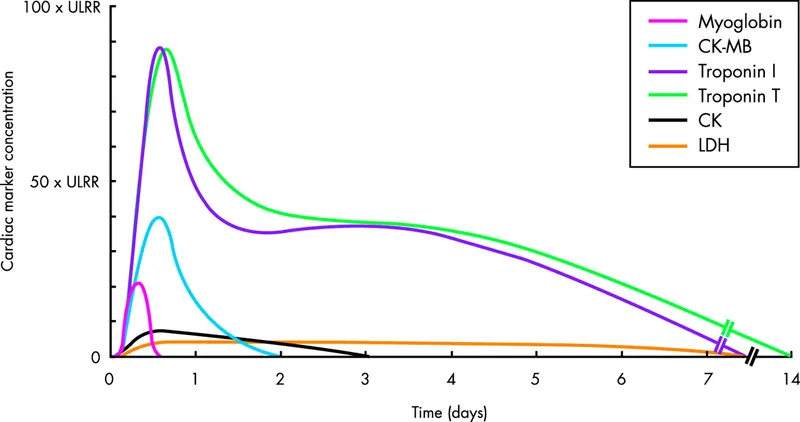
*Creatine kinase MB*
- While CK-MB is used for diagnosing myocardial infarction, its levels can also be elevated in cases of **skeletal muscle injury** or **after cardiac procedures**, reducing its specificity in this context.
- CK-MB also has a **shorter window of elevation** compared to troponins, potentially missing later presentations of myocardial injury.
*Lactate dehydrogenase*
- **LDH** is a relatively **nonspecific marker** that can elevate due to various conditions affecting different organs (e.g., liver disease, hemolysis, renal injury).
- Its elevation onset is **slower** and its diagnostic window is longer, making it less suitable for rapid diagnosis of acute myocardial injury.
*Copeptin*
- **Copeptin** is a marker of **endogenous stress** and is often used in conjunction with troponins to rule out NSTEMI, especially at early presentation.
- However, it is not a direct marker of myocardial necrosis itself and is **not as specific** as troponin for diagnosing a re-infarction.
*Aspartate aminotransferase*
- **AST** is a **nonspecific enzyme** found in various tissues, including the liver, skeletal muscle, and heart.
- Elevated AST levels are frequently seen in **liver damage** and are not a primary biomarker for diagnosing acute myocardial infarction or re-infarction.
Biomarker interpretation US Medical PG Question 3: A 32-year-old man comes to the emergency department because of sharp chest pain for 3 days. The pain is retrosternal, 8 out of 10 in intensity, increases with respiration, and decreases while sitting upright and leaning forward. He has nausea and myalgia. He has not had fever or a cough. He has asthma and was treated for bronchitis 6 months ago with azithromycin. His mother has hypertension. He uses an over-the-counter inhaler. His temperature is 37.3°C (99.1°F), pulse is 110/min, and blood pressure is 130/84 mm Hg. Breath sounds are normal. Cardiac examination shows a high-pitched grating sound between S1 and S2. The remainder of the examination shows no abnormalities. Serum studies show:
Urea nitrogen 16 mg/dl
Glucose 103 mg/dL
Creatinine 0.7 mg/dL
Troponin I 0.230 ng/mL (N < 0.1 ng/mL)
An ECG shows diffuse ST elevations in all leads. The patient is at increased risk for which of the following conditions?
- A. Cardiac tamponade (Correct Answer)
- B. Papillary muscle rupture
- C. Pulmonary infarction
- D. Ventricular aneurysm
- E. Mediastinitis
Biomarker interpretation Explanation: ***Cardiac tamponade***
- The patient's symptoms (sharp chest pain relieving with sitting upright and leaning forward, pericardial friction rub on exam, diffuse ST elevations on ECG, and elevated troponin) are highly suggestive of **acute pericarditis**.
- **Cardiac tamponade** is a serious complication of pericarditis, occurring when excessive fluid accumulation in the pericardial sac compresses the heart, impairing its filling and leading to hemodynamic compromise.
*Papillary muscle rupture*
- **Papillary muscle rupture** is typically a complication of acute myocardial infarction, leading to severe **mitral regurgitation** and acute heart failure.
- The patient's ECG shows diffuse ST elevations, not localized changes indicative of transmural infarction, and there is no mention of a new murmur or signs of heart failure.
*Pulmonary infarction*
- **Pulmonary infarction** usually presents with pleuritic chest pain, dyspnea, and hemoptysis, often in the context of a **pulmonary embolism**.
- The patient's current presentation, including the characteristic pain relief with leaning forward and the ECG findings, is not consistent with pulmonary infarction.
*Ventricular aneurysm*
- A **ventricular aneurysm** is a late complication of a transmural myocardial infarction, typically manifesting weeks to months after the event with persistent ST elevation on ECG in the affected leads.
- While there are diffuse ST elevations, the acute onset of symptoms and pericardial rub point away from a chronic complication like a ventricular aneurysm.
*Mediastinitis*
- **Mediastinitis** is a severe infection of the mediastinum, often presenting with fever, severe chest pain (usually constant), and systemic signs of infection.
- The patient is afebrile, and his chest pain characteristics, physical exam (pericardial rub), and ECG findings are not typical for mediastinitis.
Biomarker interpretation US Medical PG Question 4: A 43-year-old man comes to the emergency room complaining of chest discomfort. He describes the feeling as "tightness," and also reports weakness and palpitations for the past hour. He denies shortness of breath, diaphoresis, or lightheadedness. He has no significant past medical history, and does not smoke, drink, or use illicit drugs. His father had a myocardial infarction at age 72. He is afebrile, heart rate is 125 bpm, and his blood pressure is 120/76. He is alert and oriented to person, place, and time. His electrocardiogram is shown below. Which of the following tests should be ordered in the initial work-up of this patient's condition?
- A. Chest x-ray
- B. Blood alcohol level
- C. Urine free cortisol level
- D. Urine metanephrines
- E. Thyroid stimulating hormone level (TSH) (Correct Answer)
Biomarker interpretation Explanation: ***Thyroid stimulating hormone level (TSH)***
- The patient presents with **palpitations**, **tachycardia (HR 125 bpm)**, and chest tightness, with an ECG showing a **regular narrow-complex tachycardia** consistent with **supraventricular tachycardia (SVT)**.
- **Hyperthyroidism** is a critical secondary cause of SVT and atrial arrhythmias that must be ruled out in the initial workup.
- **TSH testing** is essential to identify **thyroid dysfunction** as a reversible and treatable cause of the tachyarrhythmia.
- Treating the underlying hyperthyroidism can resolve the arrhythmia and prevent recurrence.
*Incorrect: Urine metanephrines*
- While **pheochromocytoma** can cause palpitations and tachycardia, it typically presents with **paroxysmal hypertension**, **headaches**, and **diaphoresis** (the classic triad).
- This patient has **normal blood pressure** and denies diaphoresis, making pheochromocytoma less likely.
- TSH is a more appropriate first-line test given the clinical presentation.
*Incorrect: Chest x-ray*
- A chest X-ray may help evaluate for **structural cardiac or pulmonary abnormalities**, but it does not identify the **underlying cause** of SVT.
- It is not specific for diagnosing **metabolic or endocrine triggers** of tachyarrhythmias.
*Incorrect: Blood alcohol level*
- The patient **denies alcohol use**, making this test unnecessary in the initial evaluation.
- Alcohol withdrawal can cause tachycardia, but there is no clinical history suggesting this.
*Incorrect: Urine free cortisol level*
- **Cushing's syndrome** does not typically present with acute palpitations or SVT as the primary manifestation.
- This test is not relevant to the immediate evaluation of **tachyarrhythmia**.
Biomarker interpretation US Medical PG Question 5: A cardiologist is studying how a new virus that infects the heart affects the electrical conduction system of the cardiac myocytes. He decides to obtain electrocardiograms on patients with this disease in order to see how the wave patterns and durations change over time. While studying these records, he asks a medical student who is working with him to interpret the traces. Specifically, he asks her to identify the part that represents initial ventricular depolarization. Which of the following characteristics is most consistent with this feature of the electrocardiogram?
- A. Elevated in patients with full thickness ischemic injury of the heart
- B. Becomes peaked in states of hyperkalemia
- C. Becomes prominent in states of hypokalemia
- D. Normal duration defined as less than 120 milliseconds (Correct Answer)
- E. Normal duration defined as less than 200 milliseconds
Biomarker interpretation Explanation: ***Normal duration defined as less than 120 milliseconds***
- The question asks for the representation of **initial ventricular depolarization**, which corresponds to the **QRS complex** on an ECG.
- The normal duration of the **QRS complex** is typically less than **0.12 seconds (120 milliseconds)**, reflecting efficient ventricular depolarization.
*Elevated in patients with full thickness ischemic injury of the heart*
- This description refers to the **ST segment elevation** seen in **ST-segment elevation myocardial infarction (STEMI)**, which represents myocardial injury, not initial ventricular depolarization.
- While related to cardiac electrical activity, **ST segment elevation** is a consequence of injury and refers to repolarization abnormalities, not the QRS complex itself.
*Becomes peaked in states of hyperkalemia*
- **Peaked T waves** are characteristic of **hyperkalemia**, indicating altered ventricular repolarization, not ventricular depolarization.
- The T wave represents ventricular repolarization, and its morphology changes significantly with potassium imbalances.
*Becomes prominent in states of hypokalemia*
- A **prominent U wave** is sometimes observed in **hypokalemia**, which follows the T wave and is thought to represent repolarization of Purkinje fibers.
- The U wave is distinct from the QRS complex and does not represent initial ventricular depolarization.
*Normal duration defined as less than 200 milliseconds*
- A duration of less than 200 milliseconds (0.20 seconds) typically refers to the normal duration of the **PR interval**, which represents atrial depolarization and conduction through the AV node.
- The **QRS complex** (initial ventricular depolarization) has a shorter normal duration, typically less than 120 milliseconds.
Biomarker interpretation US Medical PG Question 6: A 71-year-old man presents to the emergency department for shortness of breath. The patient was returning from a business trip to China, when he suddenly felt short of breath during the taxi ride home from the airport. The patient has a past medical history of poorly controlled diabetes mellitus and a 50 pack-year smoking history. The patient is non-compliant with his medications and is currently only taking ibuprofen. An initial ECG demonstrates sinus tachycardia. A chest radiograph is within normal limits. Laboratory values are notable for a creatinine of 2.4 mg/dL and a BUN of 32 mg/dL as compared to his baseline creatinine of 0.9 mg/dL. His temperature is 98.8°F (37.1°C), pulse is 122/min, blood pressure is 145/90 mmHg, respirations are 19/min, and oxygen saturation is 93% on room air. On physical exam, you note an older gentleman in distress. Cardiac exam is notable only for tachycardia. Pulmonary exam is notable for expiratory wheezes. Which of the following is the best confirmatory test for this patient?
- A. Ventilation perfusion scan
- B. Lower extremity ultrasound with Doppler
- C. CT angiogram (Correct Answer)
- D. Arterial blood gas
- E. D-dimer
Biomarker interpretation Explanation: ***CT angiogram***
- This patient presents with multiple risk factors for **pulmonary embolism (PE)**, including a recent long-haul flight and acute onset of dyspnea with tachycardia and hypoxemia. CT pulmonary angiography (CTPA) is the **gold standard confirmatory test** for PE, directly visualizing thrombi in the pulmonary arteries with high sensitivity (>90%) and specificity.
- While this patient has **acute kidney injury** (creatinine elevated from 0.9 to 2.4 mg/dL), raising concerns about contrast-induced nephropathy, the **high clinical probability of PE** (recent long flight, acute dyspnea, tachycardia, hypoxemia) makes urgent diagnosis critical. In hemodynamically stable patients with intermediate-to-high PE probability and renal insufficiency, CTPA with appropriate precautions (IV hydration, minimizing contrast dose, avoiding nephrotoxic agents) is still preferred as it provides the most definitive diagnosis.
- The patient's hemodynamic stability (BP 145/90) allows time for renal protective measures before contrast administration.
*Ventilation perfusion scan*
- A V/Q scan is an important **alternative** for diagnosing PE, particularly valuable in patients with severe renal insufficiency (CKD Stage 4-5) or contrast allergy where CTPA is truly contraindicated.
- However, in this patient with **expiratory wheezes** suggesting possible underlying obstructive lung disease (50 pack-year smoking history), a V/Q scan has higher likelihood of **indeterminate results** (intermediate probability), which would not confirm or exclude PE and might necessitate additional testing anyway.
- V/Q scans also have lower sensitivity than CTPA and require the patient to cooperate with breathing maneuvers, which may be difficult in an acutely dyspneic patient.
*Lower extremity ultrasound with Doppler*
- This test diagnoses **deep vein thrombosis (DVT)**, the most common source of PE. While a positive DVT in a patient with suspected PE would support treatment, a **negative study does not rule out PE** since the thrombus may have already completely embolized.
- This is a supportive test, not a confirmatory test for PE itself. The patient's symptoms require direct assessment of the pulmonary vasculature.
*Arterial blood gas*
- An ABG typically shows **hypoxemia and respiratory alkalosis** in PE due to V/Q mismatch and hyperventilation, but these findings are **non-specific** and occur in many cardiopulmonary conditions (pneumonia, asthma, COPD exacerbation, heart failure).
- ABG is a supportive tool that may guide oxygen therapy but does not confirm PE diagnosis.
*D-dimer*
- D-dimer has excellent **negative predictive value** and is useful to exclude PE in patients with **low clinical probability** (Wells score <2 or PERC rule negative).
- In this patient with **high clinical probability** of PE (recent long flight, acute symptoms, risk factors), D-dimer would almost certainly be elevated and thus **not helpful for confirmation**. Elevated D-dimer occurs in many conditions including infection, inflammation, malignancy, recent surgery, and advanced age, making it non-specific in this context.
Biomarker interpretation US Medical PG Question 7: A 70-year-old man with diabetes, hypertension, and chronic kidney disease (eGFR 35 mL/min/1.73m²) presents with NSTEMI. Troponin is elevated at 8.5 ng/mL. ECG shows 2mm ST depression in V2-V5. GRACE score is 165 (high risk). He is hemodynamically stable. Cardiologist recommends early invasive strategy within 24 hours. Nephrologist is concerned about contrast-induced nephropathy potentially requiring dialysis. Patient is on metformin. Evaluate the management strategy integrating multiple specialist perspectives and evidence.
- A. Proceed with angiography within 24 hours using iso-osmolar contrast and intravenous hydration, hold metformin (Correct Answer)
- B. Perform coronary CT angiography as alternative to invasive angiography
- C. Delay catheterization for 72 hours to optimize renal function with hydration
- D. Prophylactic hemodialysis before and after catheterization to remove contrast
- E. Medical management only with dual antiplatelet therapy, avoid catheterization
Biomarker interpretation Explanation: ***Proceed with angiography within 24 hours using iso-osmolar contrast and intravenous hydration, hold metformin***
- High-risk NSTEMI patients with a **GRACE score >140** benefit from an **early invasive strategy** within 24 hours to reduce ischemic events and mortality.
- Renal protection is maximized through **pre-procedural hydration** and **iso-osmolar contrast**, while **metformin** must be held to avoid the risk of lactic acidosis if acute kidney injury occurs.
*Perform coronary CT angiography as alternative to invasive angiography*
- **Coronary CTA** is primarily used for ruling out coronary artery disease in low-to-intermediate risk stable patients, not for high-risk **NSTEMI**.
- This modality still requires **iodinated contrast** and does not provide the therapeutic benefit of percutaneous coronary intervention (**PCI**).
*Delay catheterization for 72 hours to optimize renal function with hydration*
- Delaying the procedure in a high-risk patient increases the risk of **re-infarction** and **cardiovascular death**, outweighing the minor benefits of prolonged hydration.
- Evidence suggests that optimization of renal status should happen concurrently with the preparation for **early intervention** in high-risk ACS.
*Prophylactic hemodialysis before and after catheterization to remove contrast*
- **Prophylactic hemodialysis** has not been proven to prevent contrast-induced nephropathy and may actually increase the risk of adverse events.
- High-volume **intravenous hydration** with isotonic saline remains the gold standard for preventing renal injury in patients with **CKD**.
*Medical management only with dual antiplatelet therapy, avoid catheterization*
- While **dual antiplatelet therapy** is essential, medical management alone is inferior to an invasive strategy in patients with **high GRACE scores**.
- Avoiding catheterization based solely on **renal impairment** results in "renalism," where patients are undertreated for their life-threatening cardiac condition.
Biomarker interpretation US Medical PG Question 8: A 58-year-old woman with anterior STEMI underwent primary PCI with drug-eluting stent placement. Post-procedure echocardiogram shows left ventricular ejection fraction of 30% with apical akinesis. She is started on aspirin, ticagrelor, high-intensity statin, and ACE inhibitor. On hospital day 3, she develops atrial fibrillation with rapid ventricular response. CHA2DS2-VASc score is 4. Creatinine is normal. Evaluate the optimal antithrombotic strategy balancing ischemic and bleeding risk.
- A. Triple therapy with aspirin, ticagrelor, and apixaban indefinitely
- B. Triple therapy for 6 months, then aspirin and apixaban indefinitely
- C. Aspirin and ticagrelor only, hold anticoagulation due to bleeding risk
- D. Warfarin with INR 2-3 plus aspirin, discontinue ticagrelor
- E. Triple therapy for 1 month, then apixaban and clopidogrel for 11 months, then apixaban alone (Correct Answer)
Biomarker interpretation Explanation: ***Triple therapy for 1 month, then apixaban and clopidogrel for 11 months, then apixaban alone***
- In patients with **Atrial Fibrillation** (CHA2DS2-VASc ≥2) undergoing **PCI**, current guidelines recommend minimizing the duration of **triple therapy** (aspirin, P2Y12 inhibitor, and anticoagulant) to 1 week to 1 month to reduce **bleeding risk**.
- Transitioning to **dual therapy** with a **NOAC** (like apixaban) and a P2Y12 inhibitor (preferably **clopidogrel**) for up to 12 months, followed by NOAC monotherapy, provides an optimal balance between preventing **stent thrombosis** and systemic **thromboembolism**.
*Triple therapy with aspirin, ticagrelor, and apixaban indefinitely*
- Indefinite **triple therapy** carries a prohibitively high risk of life-threatening **major bleeding** without added benefit for stroke prevention.
- **Ticagrelor** is generally avoided in triple therapy regimens due to a significantly higher bleeding profile compared to **clopidogrel**.
*Triple therapy for 6 months, then aspirin and apixaban indefinitely*
- **Triple therapy** for 6 months is rarely indicated and significantly increases the risk of **gastrointestinal and intracranial hemorrhage** compared to the 1-month strategy.
- Aspirin is usually discontinued after the first year in favor of **anticoagulant monotherapy**, as the latter is sufficient for both AF and stable CAD protection.
*Aspirin and ticagrelor only, hold anticoagulation due to bleeding risk*
- This approach leaves the patient with a high **CHA2DS2-VASc score of 4** unprotected against **cardioembolic stroke**, which carries high morbidity and mortality.
- Dual antiplatelet therapy (DAPT) alone is significantly less effective than **oral anticoagulants** for stroke prevention in the setting of atrial fibrillation.
*Warfarin with INR 2-3 plus aspirin, discontinue ticagrelor*
- **NOACs** (like apixaban) are now preferred over **Warfarin** for non-valvular AF due to a superior safety profile, including a lower risk of **intracranial hemorrhage**.
- Discontinuing the P2Y12 inhibitor (ticagrelor) immediately post-PCI in favor of aspirin and warfarin significantly increases the risk of **stent thrombosis**.
Biomarker interpretation US Medical PG Question 9: A 60-year-old man with inferoposterior STEMI presents to a rural hospital. The nearest PCI-capable facility is 3 hours away. He arrives 90 minutes after symptom onset. Blood pressure is 130/85 mmHg, heart rate 88/min, oxygen saturation 96% on room air. He has no contraindications to fibrinolysis. The transfer team can arrive in 30 minutes. Evaluate the evidence-based approach considering time metrics and available resources.
- A. Immediate fibrinolytic therapy followed by transfer (Correct Answer)
- B. Helicopter transfer to reduce transfer time, then primary PCI
- C. Administer half-dose fibrinolytic and transfer for immediate PCI
- D. Fibrinolytic therapy at rural hospital, transfer only if fails
- E. Wait for transfer team and proceed directly to PCI facility
Biomarker interpretation Explanation: ***Immediate fibrinolytic therapy followed by transfer***
- In a STEMI patient where the expected **door-to-balloon time** exceeds **120 minutes**, and the patient is seen within **12 hours** of symptom onset, **fibrinolytic therapy** is the preferred reperfusion strategy.
- Following fibrinolysis, a **pharmacoinvasive strategy** is recommended, involving a routine transfer to a PCI-capable center for angiography within **3 to 24 hours**.
*Helicopter transfer to reduce transfer time, then primary PCI*
- Even with expedited transport, the distance and total time likely still exceed the recommended **120-minute window** for primary PCI superiority over fibrinolysis.
- Choosing transfer over immediate thrombolysis in a rural setting when delays are significant increases the risk of **myocardial necrosis**.
*Administer half-dose fibrinolytic and transfer for immediate PCI*
- **Half-dose fibrinolytics** are generally only considered in specific subsets like elderly patients (over 75) to reduce **intracranial hemorrhage** risk, which does not apply here.
- Combining half-dose thrombolysis with immediate PCI (facilitated PCI) has not shown superior outcomes and may increase **bleeding complications**.
*Fibrinolytic therapy at rural hospital, transfer only if fails*
- Modern guidelines recommend a **pharmacoinvasive approach**, meaning all patients should be transferred for **coronary angiography** regardless of clinical success of fibrinolysis.
- Waiting only for "failure" (rescue PCI) ignores the benefit of definitive **revascularization** and stabilization provided by routine post-thrombolysis PCI.
*Wait for transfer team and proceed directly to PCI facility*
- Delaying reperfusion for a 3-hour transport window violates the "**time is muscle**" principle, as the patient is currently in the highly time-sensitive **early window** (under 3 hours).
- Failure to administer fibrinolytics when the **PCI-related delay** is over 90-120 minutes is a deviation from standard **STEMI management protocols**.
Biomarker interpretation US Medical PG Question 10: A 65-year-old man with extensive anterior STEMI underwent PCI 6 hours after symptom onset due to delayed presentation. Peak troponin was significantly elevated. Three days later, he develops progressive dyspnea. Examination reveals a new holosystolic murmur at the apex radiating to the axilla. Echocardiogram shows severe mitral regurgitation with flail posterior leaflet and hyperdynamic left ventricle. Pulmonary capillary wedge pressure tracing shows prominent v waves. He is euvolemic on examination. Analyze this complication to determine timing of intervention.
- A. Immediate surgical mitral valve repair or replacement
- B. Aggressive diuresis and ACE inhibitor, reassess in 2 weeks
- C. Intra-aortic balloon pump with surgery within 24-48 hours (Correct Answer)
- D. Percutaneous mitral valve repair with MitraClip
- E. Medical management with afterload reduction for 6 weeks, then surgery
Biomarker interpretation Explanation: ***Intra-aortic balloon pump with surgery within 24-48 hours***
- **Acute papillary muscle rupture** leads to severe mitral regurgitation and hemodynamic instability; an **IABP** provides essential **afterload reduction** and increases forward flow while reducing the regurgitant fraction.
- Providing a brief period of stabilization for 24-48 hours allows for therapeutic optimization before **urgent surgical intervention**, balancing the high risk of immediate surgery with the extreme mortality of medical delay.
*Immediate surgical mitral valve repair or replacement*
- Performing surgery immediately upon diagnosis carries an exceptionally high mortality rate due to the **friable, necrotic myocardial tissue** that is difficult to suture.
- While definitive, Proceeding without initial **hemodynamic stabilization** (like IABP) increases the risk of intraoperative cardiovascular collapse.
*Aggressive diuresis and ACE inhibitor, reassess in 2 weeks*
- This patient has a mechanical complication (flail leaflet); medical management alone for **acute MR** has a mortality rate exceeding 90%.
- **ACE inhibitors** may be poorly tolerated in the acute setting of a large MI if the patient becomes hypotensive, and waiting 2 weeks is far too long for a **mechanical emergency**.
*Percutaneous mitral valve repair with MitraClip*
- **MitraClip** is primarily indicated for chronic secondary MR or in patients with prohibitive surgical risk, rather than as first-line treatment for **acute post-MI papillary muscle rupture**.
- The necrotic and distorted nature of the **subvalvular apparatus** in an acute rupture makes it a poor substrate for percutaneous repair techniques.
*Medical management with afterload reduction for 6 weeks, then surgery*
- Delaying surgery for 6 weeks for "tissue healing" is inappropriate for **papillary muscle rupture** as the patient will likely suffer from progressive **pulmonary edema** or cardiogenic shock.
- While chronic MR can be managed medically, **acute structural failure** requires urgent mechanical correction once stable, not prolonged medical therapy.
More Biomarker interpretation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.