MI

On this page
🔥 The Cardiac Catastrophe: When Hearts Attack
When a coronary artery suddenly closes, you have minutes to recognize the crisis, decode the electrical chaos on the ECG, choose between competing reperfusion strategies, and prevent lethal arrhythmias that can strike without warning. This lesson takes you from the first chest pain through the diagnostic decision tree, the time-critical treatment battlefield, and into the reconstruction phase where you'll learn to prevent remodeling and recurrent events. You'll build the pattern recognition and clinical judgment that separates competent management from mastery when seconds determine whether muscle survives or dies.

The Ischemic Cascade: Cellular Warfare
The transition from stable angina to acute MI follows a predictable sequence of cellular events, each with specific timeframes and clinical correlations:
-
Plaque Rupture Phase (0-15 minutes)
- Vulnerable plaque with thin fibrous cap (<65 μm thickness)
- Inflammatory cell infiltration increases matrix metalloproteinase activity by 400%
- Sudden cap rupture exposes highly thrombogenic lipid core
- Tissue factor concentration: >1000-fold higher than normal vessel wall
- Platelet adhesion occurs within seconds of exposure
- Thrombin generation increases >50-fold at rupture site
-
Thrombotic Occlusion (15-60 minutes)
- Primary platelet plug formation via GPIIb/IIIa receptor activation
- Secondary hemostasis through fibrin mesh stabilization
- Complete vessel occlusion in >90% of STEMI cases
- Partial occlusion (<70% stenosis) in 60-70% of NSTEMI
- Collateral flow preservation in 15-20% of chronic cases
📌 Remember: PLAQUE - Platelet adhesion, Lipid core exposure, Acute thrombosis, Quick occlusion, Unstable angina progression, Emergent intervention needed. Vulnerable plaques have >40% lipid content and <65 μm fibrous caps.
Cellular Death Timeline: The Point of No Return
Understanding the temporal progression of myocardial necrosis guides all reperfusion strategies and explains the "golden hour" concept:
| Time Post-Occlusion | Cellular Changes | Reversibility | Clinical Markers | Intervention Window |
|---|---|---|---|---|
| 0-20 minutes | ATP depletion, anaerobic metabolism | 100% reversible | No biomarker elevation | Optimal reperfusion |
| 20-60 minutes | Membrane dysfunction, calcium influx | 80-90% salvageable | Minimal troponin rise | Critical window |
| 1-3 hours | Mitochondrial swelling, protein denaturation | 60-70% salvageable | Troponin elevation begins | Standard PCI window |
| 3-6 hours | Nuclear chromatin clumping, cell death | 30-40% salvageable | Peak CK-MB elevation | Extended window |
| >6 hours | Coagulation necrosis, neutrophil infiltration | <20% salvageable | Peak troponin levels | Salvage attempts |
Coronary Territory Mapping: Predicting the Damage
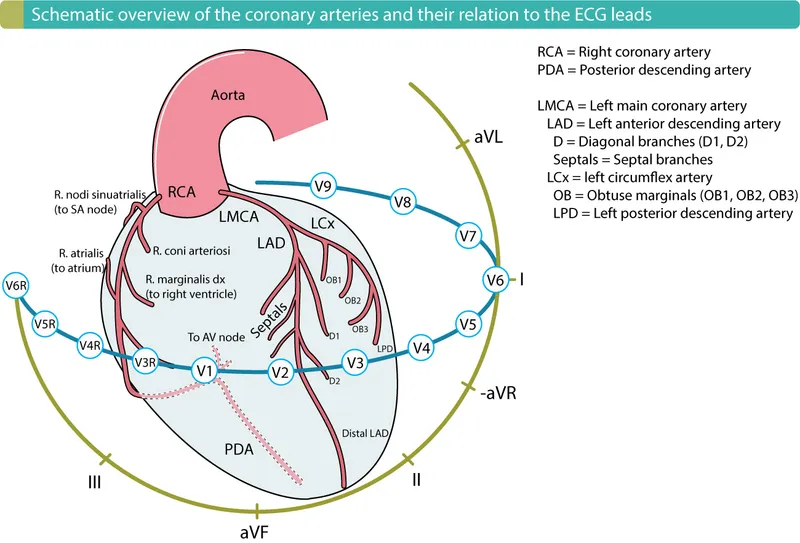
Each coronary vessel supplies specific myocardial territories, creating predictable patterns of infarction and ECG changes:
-
Left Anterior Descending (LAD) - "Widow Maker"
- Territory: Anterior wall, anterior septum, apex
- ECG leads: V1-V6, I, aVL
- Complications: Anterior STEMI (40% of all MIs)
- Cardiogenic shock risk: 15-20% (highest of all territories)
- Complete heart block in 5-10% (septal branch involvement)
- Left ventricular aneurysm in 10-15% of cases
-
Right Coronary Artery (RCA) - "The Rhythm Keeper"
- Territory: Inferior wall, posterior wall, right ventricle
- ECG leads: II, III, aVF (inferior); V7-V9 (posterior)
- Complications: Inferior STEMI (30% of all MIs)
- Bradyarrhythmias in 40-50% (AV node supply)
- Right heart failure when RV involved (30% of inferior MIs)
- Mechanical complications in 5-8% (papillary muscle rupture)
💡 Master This: RCA dominance occurs in 85% of population, supplying PDA and posterolateral branches. In left-dominant systems (8%), LCX supplies inferior wall. Co-dominant patterns (7%) share inferior supply. This anatomy determines collateral flow patterns and infarct size - RCA occlusion in dominant systems causes larger inferior MIs with higher complication rates.
📌 Remember: INFERIOR complications - Increased bradycardia, Nausea/vomiting (vagal), Fluid retention (RV failure), Electrical blocks (AV node), Right heart involvement, Ischemic MR (posterior papillary), Occlusion patterns (RCA dominant), Rhythm disturbances. 40-50% develop bradyarrhythmias requiring atropine or pacing.
The foundation of MI pathophysiology reveals how plaque vulnerability, thrombotic occlusion, and territorial anatomy determine clinical presentation and outcomes. This cellular understanding transforms into pattern recognition frameworks that guide rapid diagnosis and optimal reperfusion strategies.
🔥 The Cardiac Catastrophe: When Hearts Attack
⚡ The Electrical Storm: When Rhythms Turn Deadly

Electrophysiological Chaos: The Arrhythmic Cascade
Myocardial ischemia disrupts normal electrical conduction through multiple mechanisms, each creating specific arrhythmic patterns with predictable timing:
-
Phase 1: Hyperacute (0-30 minutes)
- Potassium efflux increases extracellular K+ to 8-12 mEq/L (normal: 3.5-5.0)
- Conduction velocity decreases by 40-60% in ischemic zones
- Ventricular ectopy appears in >90% of patients
- R-on-T phenomenon triggers VF in 15-20%
- Accelerated idioventricular rhythm (60-100 bpm) in 25%
- Ventricular tachycardia (>100 bpm) in 10-15%
-
Phase 2: Acute (30 minutes-12 hours)
- Calcium overload creates delayed afterdepolarizations
- Conduction blocks develop in border zones
- Reentrant circuits form around infarct periphery
- Sustained VT risk peaks at 6-12 hours
- Complete AV block in 15% of inferior MIs
- Bundle branch blocks in 20% of anterior MIs
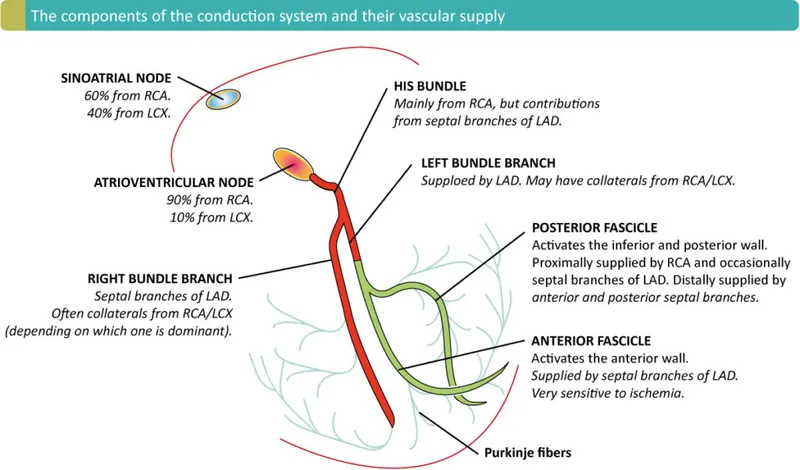
Territory-Specific Conduction Defects
The location of coronary occlusion determines specific conduction abnormalities based on the blood supply to specialized conduction tissues:
| Infarct Location | Conduction System Affected | Blood Supply | Incidence | Clinical Significance |
|---|---|---|---|---|
| Inferior MI | AV node, Bundle of His | RCA (90%) | 40-50% | Transient, reversible |
| Anterior MI | Bundle branches, Fascicles | LAD septal | 20-25% | Permanent, poor prognosis |
| Posterior MI | AV node (if RCA dominant) | PDA | 15-20% | Variable duration |
| Right ventricular | SA node, AV node | RCA proximal | 30-40% | Bradycardia, hypotension |
| Lateral MI | Left fascicles | LCX/OM | 10-15% | Hemiblocks |
📌 Remember: BLOCKS in MI - Bradycardia (inferior), Left bundle (anterior), Occasional pacing needs, Complete heart block, Keep atropine ready, Septal artery involvement. Anterior MI conduction blocks carry 3-fold higher mortality than inferior blocks due to extensive septal necrosis.
Ventricular Arrhythmia Risk Stratification
Early identification of high-risk patients for sudden cardiac death guides monitoring intensity and prophylactic interventions:
-
Highest Risk (VF/VT incidence >25%)
- Anterior STEMI with ejection fraction <40%
- Cardiogenic shock (VF risk 40-50%)
- Mechanical complications (VSD, acute MR)
- Frequent PVCs (>10/hour) increase VF risk 3-fold
- R-on-T PVCs mandate immediate lidocaine (1-1.5 mg/kg IV)
- Sustained VT requires cardioversion if hemodynamically unstable
-
Moderate Risk (VF/VT incidence 10-25%)
- Inferior STEMI with RV involvement
- NSTEMI with troponin >50x upper limit
- Reperfusion arrhythmias (paradoxically good sign)
- Accelerated idioventricular rhythm during successful reperfusion
- Transient VT bursts lasting <30 seconds
- Bradycardia followed by accelerated rhythms
💡 Master This: Reperfusion arrhythmias occur in 75-90% of successful thrombolysis and 60-80% of primary PCI. AIVR (rate 60-100 bpm) is benign and indicates restored flow. Sustained VT/VF during reperfusion (5-10% incidence) requires immediate defibrillation but doesn't predict future events - it's acute electrical instability, not chronic substrate.
The electrical consequences of MI create a temporal pattern of risk, where hyperacute arrhythmias threaten immediate survival while chronic conduction defects determine long-term prognosis. This understanding guides monitoring protocols and intervention thresholds throughout the acute phase.
⚡ The Electrical Storm: When Rhythms Turn Deadly
🎯 The Diagnostic Arsenal: Decoding Cardiac Catastrophe
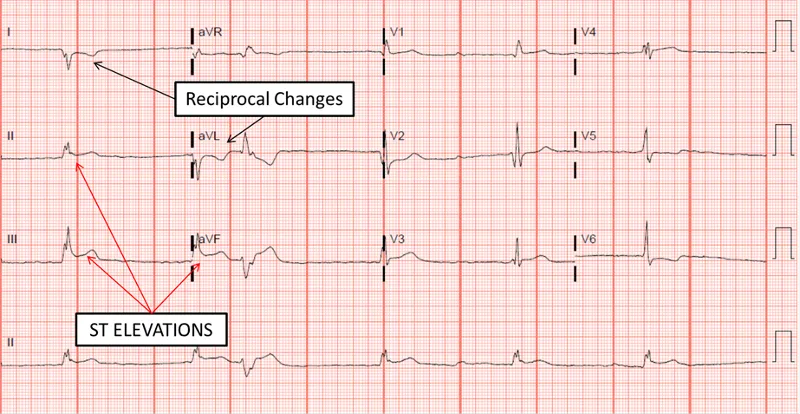
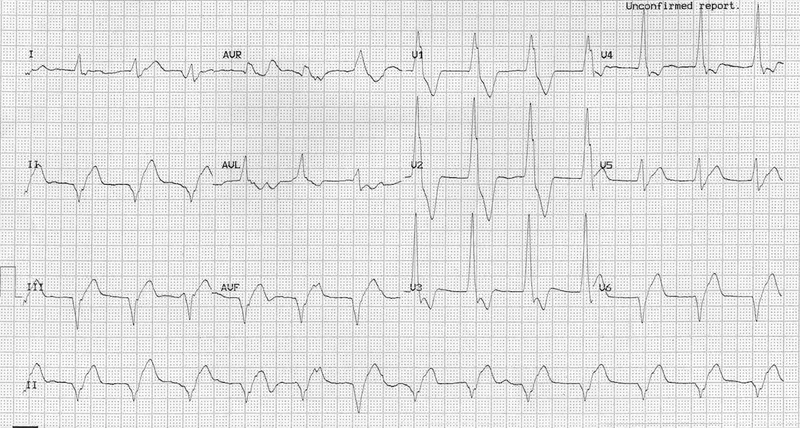
ECG Pattern Recognition: Reading the Electrical Fingerprint
The ECG provides real-time evidence of myocardial injury, with specific patterns that localize culprit vessels and predict complications within seconds of acquisition:
-
STEMI Criteria (Immediate Cath Lab Activation)
- ≥2 mm ST elevation in ≥2 contiguous leads (V1-V6)
- ≥1 mm ST elevation in ≥2 contiguous limb leads (I, II, III, aVL, aVF)
- New LBBB with clinical presentation consistent with ACS
- Posterior STEMI: ≥0.5 mm ST depression in V1-V3 with tall R waves
- Right ventricular STEMI: ≥1 mm ST elevation in V4R (check in all inferior STEMIs)
- Hyperacute T waves may precede ST elevation by 15-30 minutes
-
STEMI Equivalents (Treat as STEMI)
- De Winter pattern: Upsloping ST depression in V1-V5 with tall T waves in aVR
- Wellens syndrome: Biphasic or deeply inverted T waves in V2-V3
- Sgarbossa criteria in LBBB: ≥1 mm concordant ST elevation (specificity >95%)
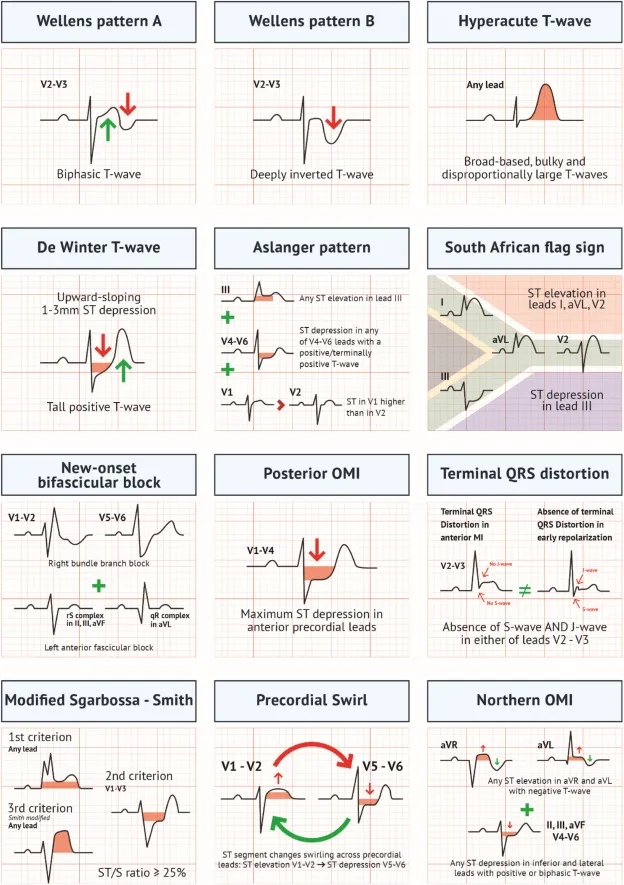
📌 Remember: ELEVATION criteria - Early recognition saves muscle, Limb leads need 1mm, V-leads need 2mm, Adjacent leads required, Time is muscle, Immediate cath lab, Occluded artery likely, New LBBB counts. False positive rate <5% when strict criteria applied with appropriate clinical context.
Biomarker Kinetics: The Chemical Timeline
Cardiac biomarkers provide quantitative evidence of myocardial necrosis, with specific kinetics that guide diagnosis, prognosis, and treatment decisions:
| Biomarker | Rise Time | Peak Time | Duration | Sensitivity | Specificity | Clinical Use |
|---|---|---|---|---|---|---|
| Troponin I/T | 3-6 hours | 12-24 hours | 7-14 days | >95% | >95% | Gold standard |
| CK-MB | 4-8 hours | 12-24 hours | 2-3 days | 85-90% | 80-85% | Re-infarction |
| Myoglobin | 1-3 hours | 6-12 hours | 24 hours | >95% | <70% | Early exclusion |
| CK-Total | 6-12 hours | 18-36 hours | 3-5 days | 70-80% | <60% | Infarct sizing |
| LDH | 12-24 hours | 2-5 days | 7-14 days | 80-85% | <70% | Late diagnosis |
Diagnostic Algorithm Integration
Successful MI diagnosis requires systematic integration of clinical presentation, ECG findings, and biomarker results within evidence-based algorithms:
-
STEMI Recognition (Target: <10 minutes)
- Primary survey: Chest pain >20 minutes, diaphoresis, nausea
- ECG acquisition: Within 10 minutes of arrival
- Cath lab activation: Single physician decision if STEMI criteria met
- Door-to-balloon goal: ≤90 minutes for primary PCI
- Door-to-needle goal: ≤30 minutes for fibrinolysis
- False activation rate: <20% acceptable for optimal outcomes
-
NSTEMI Risk Stratification (TIMI/GRACE Scores)
- TIMI Risk Score: Age ≥65 (+1), ≥3 CAD risk factors (+1), known CAD (+1)
- GRACE Score: More complex but better discrimination for 6-month mortality
- High-risk features: Troponin >50x ULN, dynamic ST changes, hemodynamic instability
💡 Master This: Type 1 MI (plaque rupture) versus Type 2 MI (supply-demand mismatch) distinction is crucial for treatment decisions. Type 2 MI shows troponin elevation but no acute plaque rupture - caused by tachycardia, hypotension, anemia, or hypoxemia. Treatment focuses on underlying cause, not antiplatelet therapy or invasive procedures.
📌 Remember: NSTEMI high-risk features - New ST depression, Sustained chest pain, Troponin markedly elevated, Elevated BNP/NT-proBNP, Mitral regurgitation murmur, Instability (hemodynamic). Early invasive strategy (<24 hours) reduces death/MI by 25% in high-risk patients.
The diagnostic framework transforms clinical uncertainty into evidence-based action, where pattern recognition and algorithmic thinking enable rapid triage and optimal resource allocation. This systematic approach ensures no STEMI goes unrecognized while avoiding unnecessary interventions in low-risk presentations.
🎯 The Diagnostic Arsenal: Decoding Cardiac Catastrophe
⚔️ The Treatment Battlefield: Reperfusion Wars
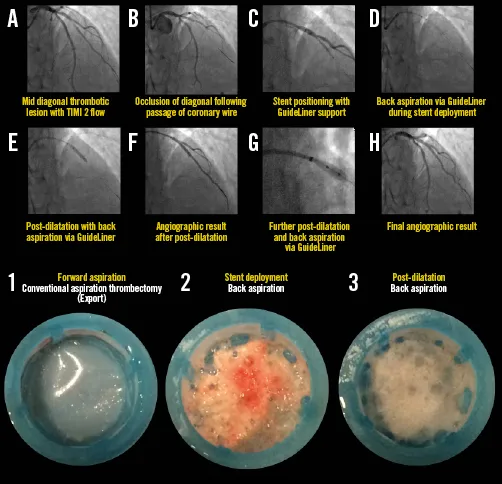
Primary PCI: The Mechanical Solution
Primary percutaneous coronary intervention represents the gold standard for STEMI reperfusion, offering superior outcomes compared to fibrinolysis when performed within evidence-based timeframes:
-
Primary PCI Advantages (Class I Recommendation)
- TIMI 3 flow achieved in >95% of cases (vs 60-70% with fibrinolysis)
- 30-day mortality reduction: 2-3% absolute decrease (NNT = 33-50)
- Reinfarction rate: <3% (vs 6-8% with fibrinolysis)
- Intracranial hemorrhage risk: <0.1% (vs 0.5-1.0% with fibrinolysis)
- Major bleeding complications: 4-6% (vs 8-12% with fibrinolysis)
- Complete revascularization possible in multivessel disease
-
Time-Dependent Efficacy (Critical Windows)
- Door-to-balloon ≤90 minutes: Optimal outcomes with maximum myocardial salvage
- 90-120 minutes: Acceptable if no fibrinolysis contraindications
- >120 minutes: Consider fibrinolysis if PCI-related delay >60 minutes
- Symptom onset <3 hours: PCI preferred even with longer delays
- Cardiogenic shock: PCI preferred regardless of time delays
- Contraindications to fibrinolysis: PCI only option
Fibrinolytic Therapy: Chemical Reperfusion
When primary PCI is unavailable or significantly delayed, fibrinolytic therapy provides effective reperfusion with specific protocols and careful patient selection:
| Agent | Dose | Administration | TIMI 3 Flow | ICH Risk | Cost |
|---|---|---|---|---|---|
| Alteplase (tPA) | 15 mg bolus + 0.75 mg/kg + 0.5 mg/kg | 90 minutes | 60-65% | 0.6-0.9% | High |
| Reteplase (rPA) | 10 U + 10 U | 30 minutes apart | 55-60% | 0.4-0.7% | Moderate |
| Tenecteplase (TNK) | Weight-based bolus | Single injection | 65-70% | 0.3-0.6% | Moderate |
| Streptokinase | 1.5 million units | 60 minutes | 45-50% | 0.3-0.5% | Low |
📌 Remember: FIBRINOLYSIS contraindications - Facial trauma/surgery, Intracranial pathology, Bleeding disorders, Recent surgery (<2 weeks), Internal bleeding, Neoplasm (CNS), Old stroke (<3 months), Labile BP (>180/110), Young age (<18), Severe liver disease, Infective endocarditis, Suspected aortic dissection.
Adjunctive Pharmacotherapy: The Supporting Cast
Optimal reperfusion requires coordinated antiplatelet, anticoagulant, and supportive therapies with evidence-based dosing and monitoring protocols:
-
Antiplatelet Therapy (Dual Therapy Standard)
- Aspirin: 325 mg loading, then 81 mg daily (indefinite)
- P2Y12 inhibitors: Choice based on bleeding risk and ischemic risk
- Clopidogrel: 600 mg loading, 75 mg daily (standard option)
- Prasugrel: 60 mg loading, 10 mg daily (more potent, higher bleeding)
- Ticagrelor: 180 mg loading, 90 mg BID (reversible, dyspnea risk)
-
Anticoagulation Strategy (Procedure-Dependent)
- Primary PCI: Bivalirudin preferred (reduces bleeding by 40%)
- Fibrinolysis: Enoxaparin or UFH based on age and renal function
- Duration: 48 hours minimum, longer if high thrombotic risk
💡 Master This: Prasugrel is contraindicated in patients with prior stroke/TIA and age >75 years (unless weight >60 kg and no other bleeding risks). Ticagrelor causes reversible dyspnea in 15-20% of patients due to adenosine reuptake inhibition - not dangerous but affects compliance. Genetic testing for CYP2C19 can guide clopidogrel effectiveness but results take 24-48 hours.
The reperfusion strategy selection depends on institutional capabilities, patient factors, and time constraints, where systematic protocols ensure optimal outcomes regardless of treatment modality. Success requires coordinated team effort with clear communication and evidence-based decision-making.
⚔️ The Treatment Battlefield: Reperfusion Wars
🏗️ The Reconstruction Phase: Building Cardiac Resilience
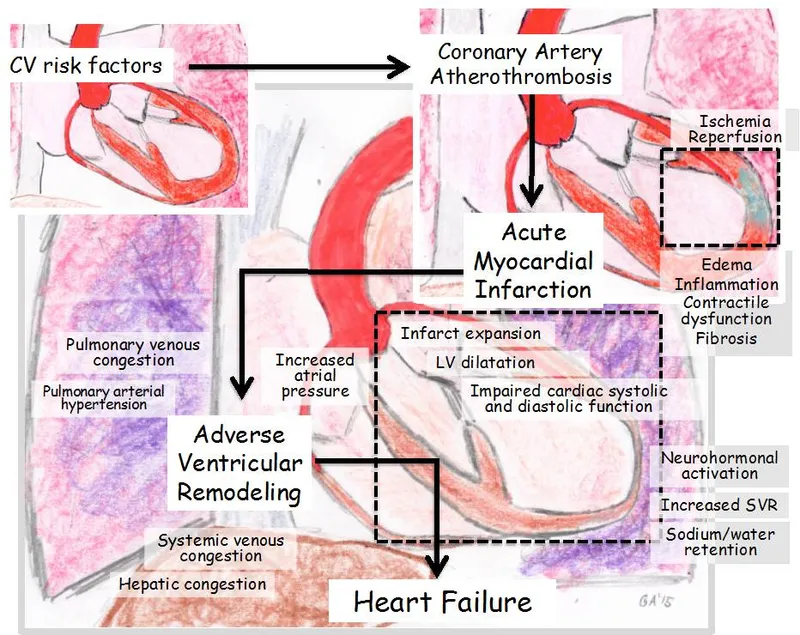
The Remodeling Cascade: Cellular Architecture Changes
Post-MI ventricular remodeling follows predictable phases with specific therapeutic windows for intervention and prevention of adverse outcomes:
-
Acute Phase (0-72 hours)
- Inflammatory response: Neutrophil infiltration peaks at 24-48 hours
- Matrix metalloproteinase activation increases collagen degradation by 300-500%
- Infarct expansion: Wall thinning and chamber dilation begin
- Early ACE inhibition reduces expansion by 30-40%
- Beta-blocker therapy decreases wall stress and oxygen demand
- Aldosterone antagonists reduce fibrosis and sudden death by 15-30%
-
Healing Phase (3 days-8 weeks)
- Macrophage infiltration and debris clearance
- Angiogenesis and collateral formation
- Scar tissue formation with collagen deposition
- Optimal medical therapy preserves remote myocardium
- Exercise rehabilitation improves collateral flow by 20-30%
- Statin therapy stabilizes non-culprit plaques and reduces recurrent events
Evidence-Based Medical Therapy: The Protective Quartet
Guideline-directed medical therapy forms the cornerstone of secondary prevention, with specific medications providing additive benefits for mortality reduction and event prevention:
| Medication Class | Primary Agent | Target Dose | Mortality Benefit | Key Monitoring | Contraindications |
|---|---|---|---|---|---|
| ACE Inhibitors | Lisinopril | 10-20 mg daily | 20-25% reduction | Creatinine, K+ | Bilateral RAS |
| Beta-Blockers | Metoprolol XL | 200 mg daily | 15-20% reduction | Heart rate, BP | Decompensated HF |
| Statins | Atorvastatin | 80 mg daily | 25-30% reduction | LDL, LFTs | Active hepatitis |
| Antiplatelet | Aspirin + P2Y12 | 81 mg + varies | 20-25% reduction | Bleeding signs | Active bleeding |
Advanced Therapeutic Strategies: Beyond Standard Care
High-risk post-MI patients benefit from additional interventions that address specific pathophysiological mechanisms and residual cardiovascular risk:
-
Heart Failure Prevention (EF ≤40%)
- Aldosterone antagonists: Spironolactone 25-50 mg or eplerenone 50 mg
- SGLT2 inhibitors: Empagliflozin 10 mg reduces HF hospitalization by 30%
- Device therapy: ICD for primary prevention if EF ≤35% after 3 months optimal therapy
- CRT-D if QRS ≥150 ms and LBBB morphology
- Wearable defibrillator for bridge therapy during optimization period
-
Residual Risk Management (Recurrent Events)
- Extended DAPT: Beyond 12 months in high ischemic risk, low bleeding risk
- Vorapaxar: PAR-1 antagonist for additional 13% event reduction
- Rivaroxaban: Low-dose anticoagulation (2.5 mg BID) with aspirin
💡 Master This: Cardiac rehabilitation participation reduces cardiovascular mortality by 13-20% and improves quality of life significantly. Core components include supervised exercise (3x/week for 12 weeks), nutritional counseling, smoking cessation, and psychosocial support. Participation rates remain <30% despite Class I recommendation - physician referral is the strongest predictor of enrollment.
📌 Remember: REHABILITATION benefits - Reduced mortality (15-20%), Exercise capacity improved, Heart rate recovery enhanced, Anxiety/depression decreased, Blood pressure lowered, Insulin sensitivity improved, Lipid profile optimized, Inflammation reduced, Thrombotic risk decreased, Adherence to medications increased, Tobacco cessation supported, Improved quality of life, Optimal weight management, Nutritional education provided.
The post-MI reconstruction phase requires systematic implementation of evidence-based therapies with regular monitoring and adjustment based on patient response and emerging evidence. This comprehensive approach transforms MI survivors from high-risk patients into well-managed individuals with excellent long-term prognosis.
🏗️ The Reconstruction Phase: Building Cardiac Resilience
🎖️ The Master Clinician's Arsenal: MI Command Center
Rapid Response Protocol Matrix
Time-critical MI management requires standardized protocols that eliminate decision delays and ensure optimal care delivery regardless of clinical complexity or institutional resources:
| Time Frame | STEMI Actions | NSTEMI Actions | Quality Metrics | Decision Points |
|---|---|---|---|---|
| 0-10 min | ECG + IV access | ECG + troponin | Door-to-ECG <10 min | STEMI vs NSTEMI |
| 10-30 min | Cath lab activation | Risk stratification | Door-to-balloon <90 min | Primary PCI vs lysis |
| 30-60 min | Arterial access | Medical optimization | Door-to-needle <30 min | Invasive vs conservative |
| 1-6 hours | Post-PCI care | Serial biomarkers | TIMI 3 flow achieved | Complications present |
| 6-24 hours | Monitoring + meds | Cath timing decision | Guideline meds initiated | Discharge planning |
Essential Clinical Calculations
Quantitative assessment tools provide objective data for risk stratification, treatment selection, and prognosis determination:
-
TIMI Risk Score (STEMI)
- Age ≥75 (+3), Age 65-74 (+2)
- Diabetes/HTN/Angina (+1)
- Systolic BP <100 (+3)
- Heart rate >100 (+2)
- Killip class II-IV (+2)
- Weight <67 kg (+1)
- Anterior STEMI or LBBB (+1)
- Time to treatment >4 hours (+1)
-
GRACE Score (NSTEMI) - More Complex but Superior
- Age, heart rate, systolic BP, creatinine
- Killip class, cardiac arrest, ST deviation, troponin elevation
- Score >140: High risk (>3% in-hospital mortality)
- Score <109: Low risk (<1% in-hospital mortality)
📌 Remember: GRACE score components - Greater age increases risk, Rate (heart) elevation dangerous, Arrest (cardiac) worst prognostic sign, Creatinine elevation (renal dysfunction), Elevated troponin confirms diagnosis. Online calculators provide precise risk estimates and treatment recommendations based on individual patient factors.
Complication Recognition Framework
Early identification of MI complications enables prompt intervention and improved outcomes through systematic surveillance and pattern recognition:
-
Mechanical Complications (2-7 days post-MI)
- Papillary muscle rupture: Acute severe MR with pulmonary edema
- Ventricular septal defect: New harsh murmur with step-up in O2 saturation
- Free wall rupture: Sudden hemodynamic collapse with pericardial tamponade
- Incidence: <1% with primary PCI, 2-3% with fibrinolysis
- Mortality: >90% without immediate surgical repair
- Risk factors: Age >70, female sex, first MI, anterior location
-
Electrical Complications (First 48 hours)
- Ventricular arrhythmias: VT/VF in 15-20% of STEMI patients
- Conduction blocks: Complete AV block in 15% of inferior MI
- Atrial fibrillation: New onset in 10-15%, increases stroke risk
💡 Master This: Cardiogenic shock develops in 5-10% of STEMI patients with >40% mortality despite optimal therapy. Early recognition requires systematic assessment: SBP <90 mmHg, CI <2.2 L/min/m², PCWP >15 mmHg. Mechanical circulatory support (IABP, Impella, ECMO) provides bridge to recovery or definitive therapy but doesn't improve mortality unless combined with revascularization.
The MI command center approach transforms complex clinical scenarios into manageable protocols where systematic thinking, evidence-based medicine, and quality improvement converge to deliver optimal patient outcomes consistently across diverse clinical settings.
🎖️ The Master Clinician's Arsenal: MI Command Center
Practice Questions: MI
Test your understanding with these related questions
A 53-year-old man with a past medical history significant for hyperlipidemia, hypertension, and hyperhomocysteinemia presents to the emergency department complaining of 10/10 crushing, left-sided chest pain radiating down his left arm and up his neck into the left side of his jaw. His ECG shows ST-segment elevation in leads V2-V4. He is taken to the cardiac catheterization laboratory for successful balloon angioplasty and stenting of a complete blockage in his left anterior descending coronary artery. Echocardiogram the following day shows decreased left ventricular function and regional wall motion abnormalities. A follow-up echocardiogram 14 days later shows a normal ejection fraction and no regional wall motion abnormalities. This post-infarct course illustrates which of the following concepts?












