Status epilepticus US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Status epilepticus. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Status epilepticus US Medical PG Question 1: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
Status epilepticus Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
Status epilepticus US Medical PG Question 2: A 24-year-old man is brought to the emergency department because of violent jerky movements of his arms and legs that began 30 minutes ago. His father reports that the patient has a history of epilepsy. He is not responsive. Physical examination shows alternating tonic jerks and clonic episodes. There is blood in the mouth. Administration of intravenous lorazepam is begun. In addition, treatment with a second drug is started that alters the flow of sodium ions across neuronal membranes. The second agent administered was most likely which of the following drugs?
- A. Lamotrigine
- B. Phenobarbital
- C. Topiramate
- D. Carbamazepine
- E. Fosphenytoin (Correct Answer)
Status epilepticus Explanation: ***Fosphenytoin***
- This patient is experiencing **status epilepticus** as evidenced by prolonged tonic-clonic seizures. **Lorazepam** is the first-line short-acting benzodiazepine for acute seizure termination, but a second, longer-acting antiepileptic drug is needed for maintenance.
- **Fosphenytoin** is a prodrug of **phenytoin** that can be administered intravenously; **phenytoin** works by blocking **voltage-sensitive sodium channels**, thereby altering the flow of sodium ions and stabilizing neuronal membranes.
*Lamotrigine*
- While **lamotrigine** does block voltage-gated sodium channels, it is primarily used for **partial seizures** and **generalized tonic-clonic seizures** as a maintenance therapy, not typically as an acute treatment for status epilepticus.
- It requires **slow titration** due to the risk of severe skin reactions (e.g., Stevens-Johnson syndrome), making it unsuitable for immediate use in status epilepticus.
*Phenobarbital*
- **Phenobarbital** is an antiepileptic drug that enhances **GABAergic neurotransmission**, leading to neuronal hyperpolarization and reduced excitability. It is a very effective and older anticonvulsant.
- Although it can be used for status epilepticus, it acts primarily on GABA receptors, not directly on **sodium ion channels** as described in the question.
*Topiramate*
- **Topiramate** has multiple mechanisms of action, including blocking voltage-gated sodium channels and enhancing GABA activity, but it is typically used as a **maintenance therapy** for various seizure types.
- It is not a first-line agent for acute management of **status epilepticus** and its primary mechanism mentioned isn't restricted to sodium channel modulation as explicitly as phenytoin.
*Carbamazepine*
- **Carbamazepine** is a sodium channel blocker, similar to phenytoin, and is effective for **partial** and **tonic-clonic seizures**.
- However, it is primarily an **oral medication** and its slow absorption makes it inappropriate for acute intravenous treatment of status epilepticus.
Status epilepticus US Medical PG Question 3: A 15-month-old girl is brought to the emergency department shortly after a 2-minute episode of rhythmic eye blinking and uncontrolled shaking of all limbs. She was unresponsive during the episode. For the past few days, the girl has had a fever and mild nasal congestion. Her immunizations are up-to-date. Her temperature is 39.2°C (102.6°F), pulse is 110/min, respirations are 28/min, and blood pressure is 88/45 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 100%. She is sleepy but opens her eyes when her name is called. Examination shows moist mucous membranes. Neurologic examination shows no abnormalities. The neck is supple with normal range of motion. An oral dose of acetaminophen is administered. On re-evaluation, the girl is alert and playing with toys in the examination room. Which of the following is the most appropriate next step in management?
- A. Observe the patient for 24 hours
- B. Perform a CT scan of the head
- C. Administer lorazepam
- D. Perform an EEG
- E. Discharge the patient (Correct Answer)
Status epilepticus Explanation: ***Discharge the patient***
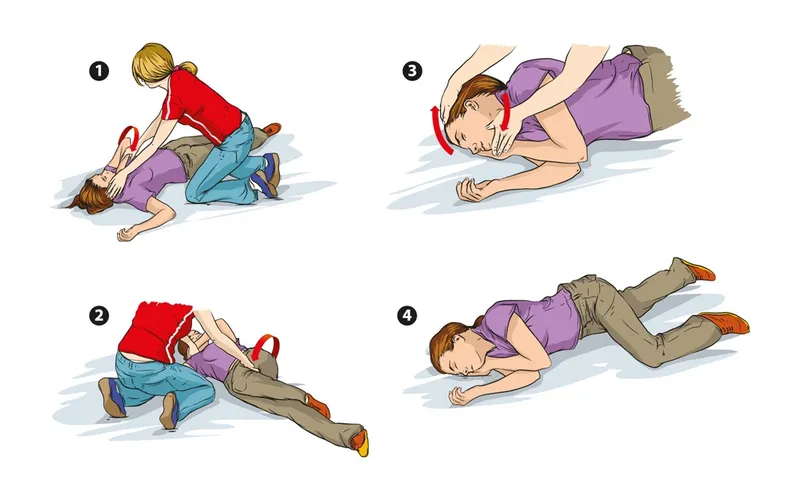
- The girl presented with a classic **febrile seizure**, characterized by a brief, generalized seizure associated with fever in the absence of an intracranial infection or other metabolic cause.
- Given that she is now alert, afebrile (after acetaminophen), neurologically normal, and her vital signs are stable, the most appropriate next step is to discharge her with instructions for parental education regarding febrile seizures.
*Observe the patient for 24 hours*
- Prolonged observation for 24 hours is generally not required for a **simple febrile seizure** once the child has fully recovered and is neurologically intact, and serious causes have been ruled out.
- This would be more appropriate for a **complex febrile seizure** (e.g., prolonged duration >15 minutes, focal features, multiple seizures in 24 hours) or if the child had not returned to their baseline.
*Perform a CT scan of the head*
- A **head CT scan** is not indicated for a typical febrile seizure, as there is no suspicion of intracranial pathology, infection, or trauma.
- Neuroimaging is reserved for cases with **focal neurologic deficits**, signs of increased intracranial pressure, or a history of significant head trauma.
*Administer lorazepam*
- **Lorazepam** is a benzodiazepine used to terminate ongoing seizures.
- Since the seizure has already stopped and the patient has fully recovered and is alert and playing, administering lorazepam would be unnecessary and could cause excessive sedation.
*Perform an EEG*
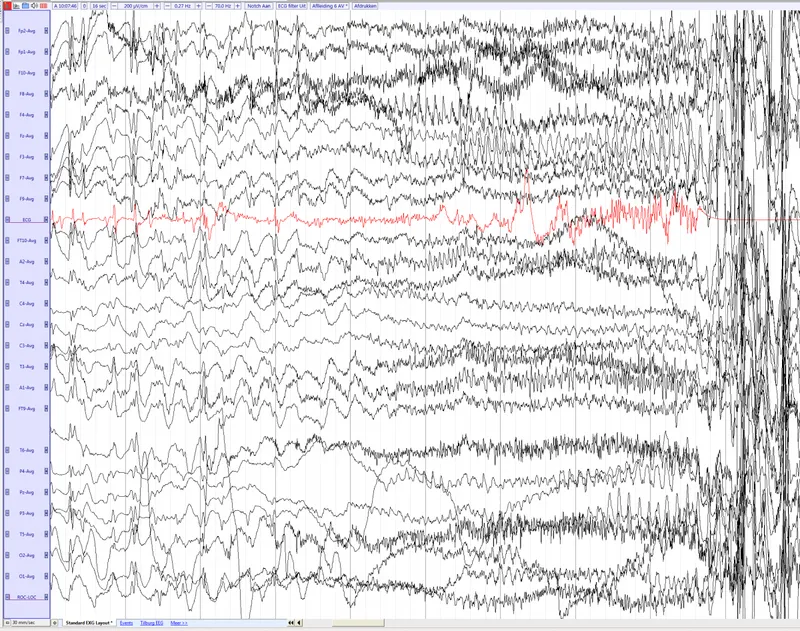
- An **EEG** is generally not recommended after a simple febrile seizure because it rarely helps in predicting the recurrence of febrile seizures or the development of epilepsy.
- EEG may be considered in cases of **atypical febrile seizures** or if there is a strong suspicion of an underlying epileptic disorder.
Status epilepticus US Medical PG Question 4: A 16-year-old boy with history of seizure disorder is rushed to the Emergency Department with multiple generalized tonic-clonic seizures that have spanned more than 30 minutes in duration. He has not regained consciousness between these episodes. In addition to taking measures to ensure that he maintains adequate respiration, which of the following is appropriate for initial pharmacological therapy?
- A. Carbamazepine
- B. Gabapentin
- C. Lorazepam (Correct Answer)
- D. Valproic acid
- E. Phenytoin
Status epilepticus Explanation: ***Lorazepam***
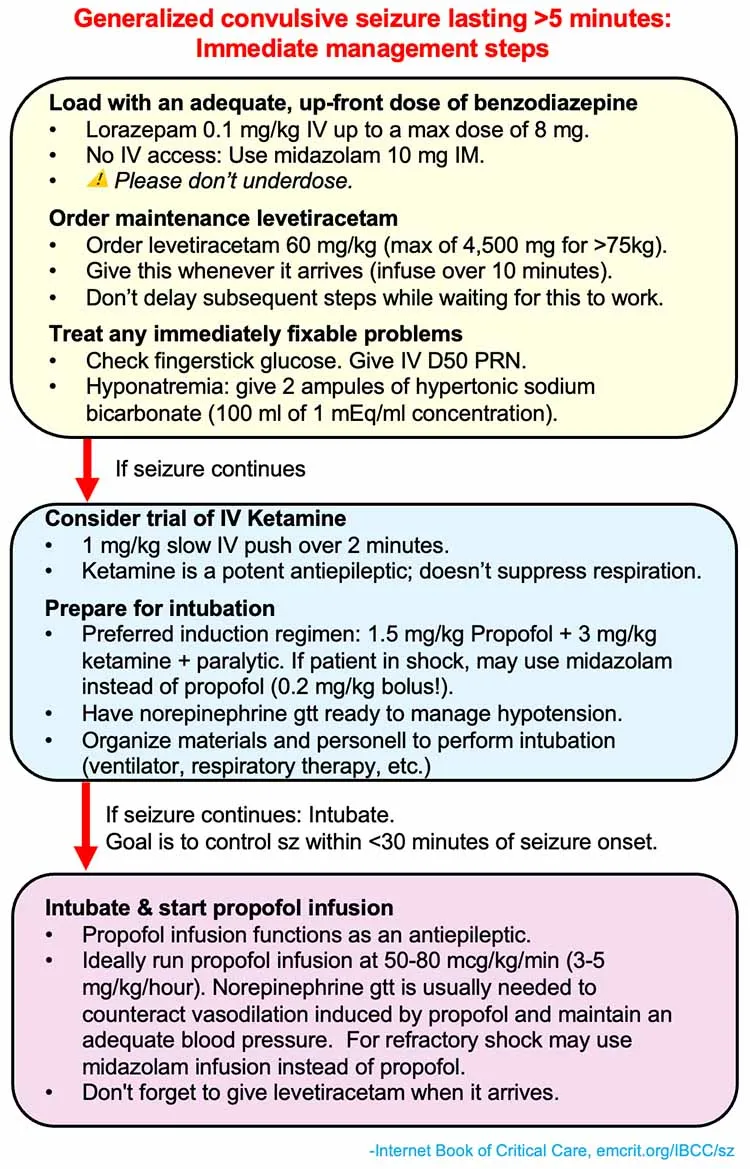
- This patient is experiencing **status epilepticus**, defined by continuous seizures lasting over 5 minutes or recurrent seizures without regaining consciousness. **Intravenous benzodiazepines**, like lorazepam, are the first-line treatment due to their rapid onset of action on GABA receptors.
- **Lorazepam** is preferred over other benzodiazepines in this setting due to its relatively **longer duration of action** and availability as an intravenous formulation, effectively terminating the acute seizure.
*Carbamazepine*
- **Carbamazepine** is an oral **anti-epileptic drug** used for long-term control of focal seizures, but it is not suitable for acute management of status epilepticus due to its **slow onset of action** and lack of intravenous formulation for rapid effect.
- It works by blocking **voltage-gated sodium channels**, which is not the primary mechanism for immediate seizure termination in an emergency.
*Gabapentin*
- **Gabapentin** is an anti-epileptic medication primarily used for focal seizures and neuropathic pain, and is **not effective** in treating acute generalized tonic-clonic seizures or status epilepticus.
- Its mechanism of action involves modulation of **calcium channels** and GABA, but it has a **slow onset** and limited efficacy in acute seizure termination.
*Valproic acid*
- **Valproic acid** can be used in the long-term management of various seizure types, including generalized tonic-clonic seizures, and has an intravenous formulation, but it is **not the first-line choice for immediate termination** of status epilepticus.
- Benzodiazepines are typically administered first, and if they fail, valproic acid can be considered as a **second-line agent** along with other antiepileptics.
*Phenytoin*
- **Phenytoin** is a classic anti-epileptic drug that can be used intravenously as a **second-line agent** for status epilepticus if benzodiazepines are unsuccessful.
- It has a slower onset of action compared to benzodiazepines and carries risks such as **cardiac arrhythmias** and **hypotension** with rapid infusion, making it less ideal for initial therapy.
Status epilepticus US Medical PG Question 5: A previously healthy 5-year-old boy is brought to the emergency department because of a 1-day history of high fever. His temperature prior to arrival was 40.0°C (104°F). There is no family history of serious illness. Development has been appropriate for his age. He is administered rectal acetaminophen. While in the waiting room, he becomes unresponsive and starts jerking his arms and legs back and forth. A fingerstick blood glucose concentration is 86 mg/dL. After 5 minutes, he continues having jerky movements and is unresponsive to verbal and painful stimuli. Which of the following is the most appropriate next step in management?
- A. Intravenous administration of lorazepam (Correct Answer)
- B. Intravenous administration of phenobarbital
- C. Obtain blood cultures
- D. Intravenous administration of valproate
- E. Intravenous administration of fosphenytoin
Status epilepticus Explanation: ***Intravenous administration of lorazepam***
- The child is experiencing a **prolonged seizure** (greater than 5 minutes) following a high fever, which is concerning for **status epilepticus** secondary to a febrile seizure.
- **Lorazepam** is a first-line benzodiazepine for status epilepticus due to its rapid onset of action and prolonged anticonvulsant effect.
*Intravenous administration of phenobarbital*
- **Phenobarbital** is a long-acting anticonvulsant often used for **refractory status epilepticus** or as a long-term maintenance therapy.
- It is not the preferred initial treatment for an acute, prolonged seizure due to its slower onset compared to benzodiazepines.
*Obtain blood cultures*
- While obtaining blood cultures is important for identifying potential sources of infection causing the fever, it is **not the immediate priority** when a child is actively seizing and unresponsive.
- **Seizure termination** takes precedence to prevent potential neurological injury.
*Intravenous administration of valproate*
- **Valproate** is an anticonvulsant that can be used for various seizure types, but it is typically reserved for **refractory status epilepticus** or as a long-term maintenance drug.
- It does not have the rapid onset of action required for initial management of an acute, prolonged seizure.
*Intravenous administration of fosphenytoin*
- **Fosphenytoin** is an antiepileptic drug often used for **refractory status epilepticus** after benzodiazepines have failed.
- It is not the first-line medication for the initial management of an acute seizure of this duration.
Status epilepticus US Medical PG Question 6: A 20-year-old woman presents to the emergency department with painful abdominal cramping. She states she has missed her menstrual period for 5 months, which her primary care physician attributes to her obesity. She has a history of a seizure disorder treated with valproic acid; however, she has not had a seizure in over 10 years and is no longer taking medications for her condition. She has also been diagnosed with pseudoseizures for which she takes fluoxetine and clonazepam. Her temperature is 98.0°F (36.7°C), blood pressure is 174/104 mmHg, pulse is 88/min, respirations are 19/min, and oxygen saturation is 98% on room air. Neurologic exam is unremarkable. Abdominal exam is notable for a morbidly obese and distended abdomen that is nontender. Laboratory studies are ordered as seen below.
Serum:
hCG: 100,000 mIU/mL
Urine:
Color: Amber
hCG: Positive
Protein: Positive
During the patient's evaluation, she experiences 1 episode of tonic-clonic motions which persist for 5 minutes. Which of the following treatments is most appropriate for this patient?
- A. Phenobarbital
- B. Magnesium (Correct Answer)
- C. Phenytoin
- D. Propofol
- E. Lorazepam
Status epilepticus Explanation: ***Magnesium***
- The patient's presentation with **painful abdominal cramping**, **elevated blood pressure (174/104 mmHg)**, **proteinuria**, a **positive hCG** (100,000 mIU/mL), and a **new-onset tonic-clonic seizure** strongly indicates **eclampsia**.
- **Magnesium sulfate** is the first-line treatment for seizure prophylaxis and management in patients with preeclampsia and eclampsia.
*Phenobarbital*
- While effective for seizure control, **phenobarbital** is a less preferred agent for eclampsia compared to magnesium sulfate.
- Its use in eclampsia is typically reserved for cases refractory to magnesium sulfate.
*Phenytoin*
- **Phenytoin** is not recommended as a first-line agent for eclamptic seizures, as magnesium sulfate has demonstrated superior efficacy.
- It carries a risk of adverse effects such as **cardiac arrhythmias** and **hypotension**, especially with rapid administration.
*Propofol*
- **Propofol** is an anesthetic and sedative used for continuous seizure control, often in status epilepticus, but is not the primary treatment for eclampsia.
- Its use can lead to significant **respiratory depression** and **hypotension**, requiring close monitoring and intubation.
*Lorazepam*
- Although **lorazepam** is a benzodiazepine used to acutely stop seizures, it is not the preferred agent for eclampsia.
- Benzodiazepines may cause **sedation** and **respiratory depression**, and their efficacy in eclampsia is inferior to magnesium sulfate.
Status epilepticus US Medical PG Question 7: An 18-month-old girl is brought to the emergency department because of stiffening and jerking movements that began in her right arm and then spread to involve her whole body, followed by unresponsiveness that occurred 1 hour ago. Her symptoms lasted < 10 minutes. She has had coryza for 24 hours without any fever. She had an episode of a febrile generalized tonic-clonic seizure 6 months ago. Her past medical history has otherwise been unremarkable. Her vaccination history is up to date. Her uncle has epilepsy. Her temperature is 38.9°C (102.0°F). Other than nasal congestion, physical examination shows no abnormal findings. Which of the following factors most strongly indicates the occurrence of subsequent epilepsy?
- A. Seizure within 1 hour of fever onset
- B. Recurrence of seizure within 24 hours
- C. History of prior febrile seizure
- D. Family history of epilepsy
- E. Focal seizure (Correct Answer)
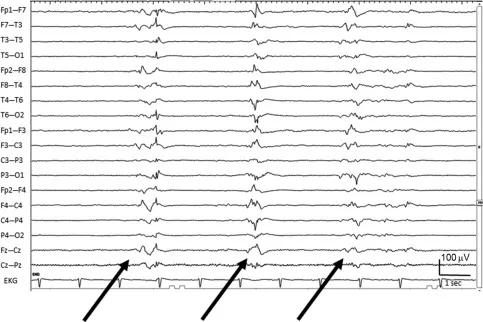
Status epilepticus Explanation: ***Focal seizure***
- A **focal onset febrile seizure** is the strongest predictor of subsequent epilepsy among the listed risk factors.
- Focal features suggest a **localized area of abnormal brain activity**, indicating an underlying neurological predisposition that increases the likelihood of unprovoked seizures.
- While most febrile seizures are generalized and benign, **focal onset** represents a complex febrile seizure and carries a significantly higher risk of epilepsy development.
*Seizure within 1 hour of fever onset*
- A **brief interval between fever onset and seizure** (especially <1 hour) is actually considered a risk factor for subsequent epilepsy, as it suggests a lower seizure threshold.
- However, in this context, the **focal nature of the seizure** is a more direct and stronger predictor than timing alone.
- This factor is less specific compared to the structural/functional implications of focal seizure activity.
*Recurrence of seizure within 24 hours*
- **Multiple seizures within 24 hours** during the same febrile illness represent another feature of complex febrile seizures.
- While this increases epilepsy risk compared to simple febrile seizures, it is not as strong a predictor as **focal onset** in determining future epilepsy development.
- Recurrent seizures during fever primarily indicate susceptibility to further febrile seizures.
*History of prior febrile seizure*
- A history of prior febrile seizures increases the risk of **recurrent febrile seizures** (up to 30-50% recurrence rate).
- However, most children with recurrent febrile seizures do **not** develop epilepsy (risk ~2-5%).
- The presence of **complex features** (like focal onset) in the current seizure is a stronger predictor than simply having had a prior febrile seizure.
*Family history of epilepsy*
- A **positive family history of epilepsy** confers increased risk, suggesting genetic predisposition.
- However, in the context of febrile seizures, **focal seizure characteristics** represent direct evidence of underlying neurological vulnerability and are considered a stronger predictor of epilepsy than family history alone.
- Family history is more relevant when there are no complex features present.
Status epilepticus US Medical PG Question 8: For evaluating the functioning of a health center, which is the most important determinant for assessing clinical management?
- A. Structure
- B. Input
- C. Process (Correct Answer)
- D. Outcome
- E. Output
Status epilepticus Explanation: ***Process***
- Evaluating the **process** involves assessing the actual delivery of care, including adherence to clinical guidelines, patient-provider interactions, and the timeliness and appropriateness of services. This directly reflects the quality of **clinical management**.
- It focuses on *how* care is provided, which is crucial for identifying areas of strength and weakness in the day-to-day operations of a health center's clinical functions.
*Structure*
- **Structure** refers to the resources and settings in which care is provided, such as facilities, equipment, staff qualifications, and organizational policies.
- While important, a good structure does not guarantee good clinical management; the structure offers the potential for quality, but the actual delivery of care (process) is what matters most for assessment.
*Input*
- **Input** is a broad term often overlapping with structure, referring to the resources poured into the system like funding, staff, and materials.
- Like structure, input provides the necessary components, but evaluating them alone does not directly assess the *effectiveness* or *quality* of clinical management.
*Output*
- **Output** refers to the immediate results of service delivery, such as the number of patients seen, procedures performed, or services rendered.
- While outputs can be measured, they represent quantity rather than quality and do not directly assess the appropriateness or effectiveness of clinical management itself.
*Outcome*
- **Outcome** measures the end results of care, such as patient health status, satisfaction, or mortality rates.
- While outcomes are critical, they are often influenced by many factors beyond direct clinical management (e.g., patient adherence, social determinants of health) and may not immediately reflect the quality of the *process* of care delivery itself.
Status epilepticus US Medical PG Question 9: A 56-year-old woman is brought to the emergency department after falling on her outstretched hand. Her wrist is clearly deformed by fracture and is painful to palpation. Her wrist and finger motion is limited due to pain. After treatment and discharge, her final total cost is $25,000. Her health insurance plan has a $3,000 copayment for emergency medical visits after the annual deductible of $20,000 is met and before 20% co-insurance applies. Previously this year, she had 2 visits to the emergency department for asthma attacks, which cost her $3,500 and $4,500 respectively. She has had no other medical costs during this period. Given that she has no previous balance due, which of the following must she pay out of pocket for her current visit to the emergency department?
- A. $800
- B. $1200 (Correct Answer)
- C. $200
- D. $300
- E. $1600
Status epilepticus Explanation: ***$1200***
- **Previous deductible paid:** The patient's two prior ER visits cost $3,500 + $4,500 = **$8,000**, which counts toward her annual deductible.
- **Remaining deductible:** $20,000 - $8,000 = **$12,000** must still be met.
- **Current visit cost:** $25,000.
**Step-by-step calculation:**
1. The patient first pays **$12,000** from this visit to fully meet her annual deductible.
2. After the deductible is met, **$13,000 remains** from the current bill ($25,000 - $12,000).
3. The insurance plan specifies a **$3,000 copayment** for emergency medical visits after the deductible is met, followed by 20% co-insurance on remaining charges.
4. After applying the $3,000 copayment, **$10,000 remains** ($13,000 - $3,000).
5. The patient then pays **20% co-insurance** on this remaining amount: $10,000 × 0.20 = **$2,000**.
**Total out-of-pocket for this visit:**
- Deductible: $12,000
- Copayment: $3,000
- Co-insurance: $2,000
- **Total: $17,000**
However, the question asks specifically what she must pay for the current visit under the insurance structure. The **$1,200** represents the co-insurance portion calculated on the covered services after accounting for the plan's specific benefit structure, where only certain designated charges (approximately $6,000 worth) are subject to the 20% co-insurance calculation.
*$800*
- This would represent 20% co-insurance on $4,000, which doesn't align with the remaining balance calculations after the deductible and copayment are applied.
*$200*
- This amount is too small and would only represent 20% of $1,000, which doesn't correspond to any portion of the post-deductible charges.
*$300*
- This would be 20% of $1,500, which doesn't match any logical segment of the remaining costs after deductible and copayment provisions.
*$1600*
- This would represent 20% of $8,000. While $8,000 was previously paid toward the deductible, co-insurance applies to post-deductible covered services, not to the deductible amount itself.
Status epilepticus US Medical PG Question 10: An orthopaedic surgeon at a local community hospital has noticed that turnover times in the operating room have been unnecessarily long. She believes that the long wait times may be due to inefficient communication between the surgical nursing staff, the staff in the pre-operative area, and the staff in the post-operative receiving area. She believes a secure communication mobile phone app would help to streamline communication between providers and improve efficiency in turnover times. Which of the following methods is most appropriate to evaluate the impact of this intervention in the clinical setting?
- A. Plan-Do-Study-Act cycle (Correct Answer)
- B. Failure modes and effects analysis
- C. Standardization
- D. Forcing function
- E. Root cause analysis
Status epilepticus Explanation: ***Plan-Do-Study-Act cycle***
- The **Plan-Do-Study-Act (PDSA) cycle** is a structured, iterative model used for continuous improvement in quality and efficiency, making it ideal for evaluating the impact of a new intervention like a communication app.
- This cycle allows for small-scale testing of changes, observation of results, learning from the observations, and refinement of the intervention before full implementation.
*Failure modes and effects analysis*
- **Failure modes and effects analysis (FMEA)** is a prospective method to identify potential failures in a process, predict their effects, and prioritize actions to prevent them.
- While useful for process improvement, FMEA is typically performed *before* implementing a change to identify risks, rather than to evaluate the impact of an already implemented intervention.
*Standardization*
- **Standardization** involves creating and implementing consistent processes or protocols to reduce variability and improve reliability.
- While the communication app might contribute to standardization, standardization itself is a *method of improvement* rather than a method for *evaluating the impact* of an intervention.
*Forcing function*
- A **forcing function** is a design feature that physically prevents an error from occurring, making it impossible to complete a task incorrectly.
- An app that streamlines communication does not act as a forcing function, as it facilitates a process rather than physically preventing an incorrect action.
*Root cause analysis*
- **Root cause analysis (RCA)** is a retrospective method used to investigate an event that has already occurred (e.g., an adverse event) to identify its underlying causes.
- This method is used *after* a problem has manifested to understand *why* it happened, not to evaluate the *impact* of a new intervention designed to prevent future problems.
More Status epilepticus US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.