Severe electrolyte disturbances US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Severe electrolyte disturbances. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Severe electrolyte disturbances US Medical PG Question 1: A 70-year-old man presents to his primary care physician for a general checkup. He states that he has been doing well and taking his medications as prescribed. He recently started a new diet and supplement to improve his health and has started exercising. The patient has a past medical history of diabetes, a myocardial infarction, and hypertension. He denies any shortness of breath at rest or with exertion. An ECG is performed and is within normal limits. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 6.7 mEq/L
HCO3-: 25 mEq/L
Glucose: 133 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most likely cause of this patient's presentation?
- A. Medication (Correct Answer)
- B. Acute renal failure
- C. Hemolysis
- D. Dietary changes
- E. Rhabdomyolysis
Severe electrolyte disturbances Explanation: ***Medication***
- The patient's **hyperkalemia** (K+ 6.7 mEq/L) despite feeling well, suggests a common side effect of medications, particularly those used for his pre-existing conditions like **hypertension** (**ACE inhibitors**, **ARBs**, **spironolactone**) and **diabetes**.
- Medications are a frequent cause of asymptomatic electrolyte abnormalities, and given his complex medical history and the absence of acute symptoms, this is the most likely culprit.
*Acute renal failure*
- While acute renal failure can cause **hyperkalemia**, it typically presents with other symptoms such as **oliguria**, **fluid retention**, or other signs of organ dysfunction, which are not described.
- The patient is reported to be "doing well" without **shortness of breath** or other acute complaints, making acute renal failure less likely as the primary cause of isolated hyperkalemia.
*Hemolysis*
- **Hemolysis** can release intracellular potassium, leading to **pseudohyperkalemia**, but it would typically be suspected in cases of **blood draw errors** or conditions causing red blood cell breakdown, none of which are indicated.
- The patient's presentation does not include any signs or symptoms suggestive of red cell destruction.
*Dietary changes*
- While an extremely **high-potassium diet** or certain **supplements** could contribute to hyperkalemia, it is less common for dietary changes alone to cause such a significant elevation in a patient with normal organ function.
- Given his medical history, medication-induced hyperkalemia is a more direct and common explanation.
*Rhabdomyolysis*
- **Rhabdomyolysis** involves the breakdown of muscle tissue, releasing potassium and other intracellular contents, but it is usually associated with significant **muscle pain**, **weakness**, and elevated **creatine kinase**.
- The patient denies these symptoms and has no other indicators pointing towards severe muscle injury.
Severe electrolyte disturbances US Medical PG Question 2: A 45-year-old man presents to the emergency department with complaint of dizziness and nausea for the past hour. He says that he can feel his heartbeat racing. He also reports of generalized weakness that began in the morning. He was diagnosed with end-stage renal disease 2 years ago and currently on dialysis, but he missed his last dialysis session. He has also been diabetic for the past 15 years and managed with insulin, and was also diagnosed with celiac disease 8 years ago. He does not smoke or drink alcohol. The family history is insignificant. The temperature is 36.7°C (98.0°F), blood pressure is 145/90 mm Hg, pulse is 87/min, and respiratory rate is 14/min. On physical examination, the patient looks fatigued and exhausted. The muscle strength in the lower limbs is 4/5 bilaterally. An ECG is ordered which shows peaked and narrow T waves and prolongation of PR interval. The lab test results are as follows:
Serum Sodium 132 mEq/L
Serum Potassium 8 mEq/L
Serum Creatinine 5 mg/dL
Blood urea nitrogen (BUN) 25 mg/dL
What is the mechanism of action of the most likely initial treatment for the patient's condition?
- A. Prevents platelet aggregation
- B. Blocks beta adrenergic receptors
- C. Antagonizes the membrane action of hyperkalemia (Correct Answer)
- D. Increase potassium loss from the gastrointestinal tract
- E. Blocks Na+/K+ ATPase
Severe electrolyte disturbances Explanation: ***Antagonizes the membrane action of hyperkalemia***
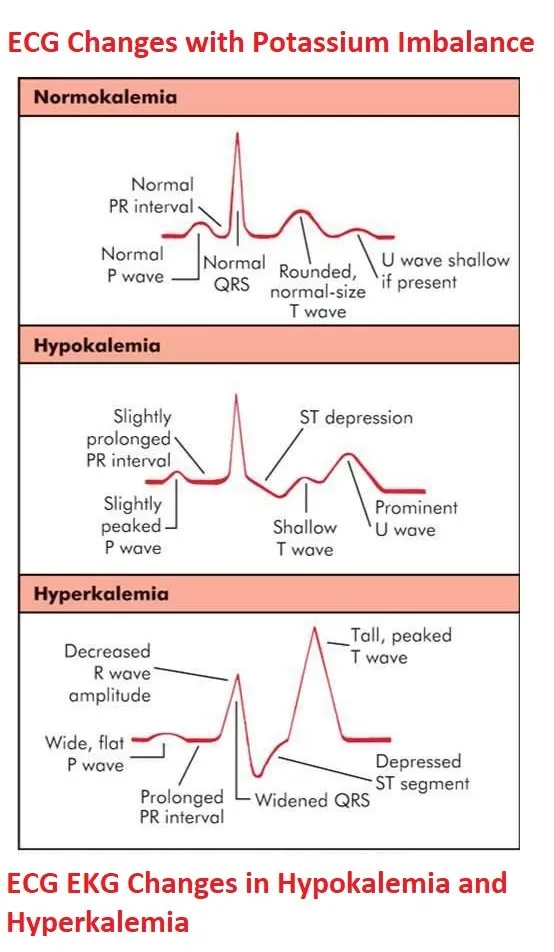
- The patient's presentation with **dizziness**, **nausea**, **racing heartbeat**, **generalized weakness**, **missed dialysis**, and ECG findings of **peaked T waves** and **prolonged PR interval** are classic for **severe hyperkalemia** (potassium 8 mEq/L).
- The most immediate and life-saving initial treatment for hyperkalemia with ECG changes is **intravenous calcium (e.g., calcium gluconate or calcium chloride)**, which **stabilizes the cardiac myocyte membrane** by antagonizing the direct membrane effects of elevated potassium, without lowering serum potassium levels.
*Prevents platelet aggregation*
- This is the mechanism of action for **antiplatelet drugs** like aspirin or clopidogrel, which are used to prevent thrombus formation in conditions like myocardial infarction or stroke.
- Platelet aggregation is not the primary issue in acute hyperkalemia.
*Blocks beta adrenergic receptors*
- This is the mechanism of action of **beta-blockers**, used to treat conditions like hypertension, angina, and certain arrhythmias.
- Beta-blockers are not indicated for the immediate treatment of hyperkalemia.
*Increase potassium loss from the gastrointestinal tract*
- This is the mechanism of action of **potassium binders** such as sodium polystyrene sulfonate (Kayexalate) or patiromer.
- While these can lower potassium, their action is much slower and not the initial life-saving intervention needed in severe hyperkalemia with ECG changes.
*Blocks Na+/K+ ATPase*
- This is the mechanism of action of **cardiac glycosides** like **digoxin**, which increase intracellular calcium and myocardial contractility.
- Blocking the Na+/K+ ATPase can worsen hyperkalemia (as Na+/K+ ATPase normally pumps K+ into cells) and is not a treatment for hyperkalemia.
Severe electrolyte disturbances US Medical PG Question 3: A 32-year-old man with a history of chronic alcoholism presents to the emergency department with vomiting and diarrhea for 1 week. He states he feels weak and has had poor oral intake during this time. The patient is a current smoker and has presented many times to the emergency department for alcohol intoxication. His temperature is 97.5°F (36.4°C), blood pressure is 102/62 mmHg, pulse is 135/min, respirations are 25/min, and oxygen saturation is 99% on room air. On physical exam, he is found to have orthostatic hypotension and dry mucus membranes. Laboratory studies are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 3.9 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 9.8 mg/dL
The patient is given normal saline, oral potassium, dextrose, thiamine, and folic acid. The following day, the patient seems confused and complains of diffuse weakness and muscle/bone pain. An ECG and head CT are performed and are unremarkable. Which of the following is the most likely explanation for this patient's new symptoms?
- A. Hypomagnesemia
- B. Hyponatremia
- C. Hypoglycemia
- D. Hypophosphatemia (Correct Answer)
- E. Hypocalcemia
Severe electrolyte disturbances Explanation: **Hypophosphatemia**
- **Hypophosphatemia** is common in **alcoholics**, often exacerbated by refeeding (administration of glucose and fluids). The patient's initial symptoms of weakness and muscle/bone pain after treatment suggest this condition.
- Symptoms such as **confusion**, **diffuse weakness**, and **muscle/bone pain** are classic manifestations of severe hypophosphatemia as phosphorus is vital for muscle and nerve function, and bone health.
*Hypomagnesemia*
- While common in alcoholics and capable of causing weakness, **hypomagnesemia** typically presents with symptoms like **tremors**, **seizures**, and **cardiac arrhythmias**.
- The patient's primary symptoms of confusion and diffuse muscle/bone pain are less characteristic of magnesium deficiency compared to phosphorus deficiency.
*Hyponatremia*
- The patient's initial sodium level was 139 mEq/L, which is within the normal range, making **hyponatremia** unlikely to be the cause of new symptoms.
- While severe hyponatremia can cause confusion, it typically presents with other neurological symptoms like **headache** and **seizures**, which are not reported here.
*Hypoglycemia*
- The initial glucose level of 99 mg/dL was normal, and the patient received dextrose, making **hypoglycemia** an unlikely cause of the new symptoms.
- Symptoms of hypoglycemia usually include **sweating**, **tremors**, and **palpitations**, in addition to confusion.
*Hypocalcemia*
- The patient's initial calcium level was 9.8 mg/dL, which is within the normal range, making **hypocalcemia** an unlikely cause of the new symptoms.
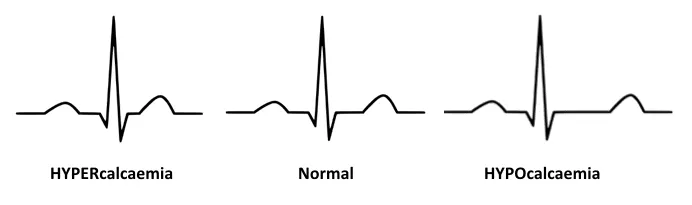
- Symptoms of hypocalcemia typically include **tetany**, **paresthesias**, and a **prolonged QT interval** on EKG, none of which are described.
Severe electrolyte disturbances US Medical PG Question 4: A 39-year-old man comes to the physician because of frequent urination for the past 2 months. He has been urinating 10–12 times during the day and 3–4 times during the night. He says he is drinking a lot of water to compensate for any dehydration. He has no history of serious illness and takes no medications. Vital signs are within normal limits. Physical examination shows no abnormalities. He is concerned he may have diabetes mellitus like his parents. Laboratory studies show:
Hemoglobin 14.3 g/dL
Serum
Na+ 149 mEq/L
K+ 3.9 mEq/L
Cl- 102 mEq/L
Glucose 90 mg/dL
Osmolality 306 mOsmol/kg H2O
Urine
Osmolality 210 mOsmol/kg H2O
A water deprivation test is conducted. After 2 hours of fluid restriction, his plasma osmolality is 315 mOsmol/kg H2O and his urine osmolality is 210 mOsmol/kg H2O. One hour after an ADH analog injection, his plasma osmolality is 276 mOsmol/kg H2O and his urine osmolality is 425 mOsmol/kg H2O. Which of the following is the most appropriate next step in management?
- A. Hydrochlorothiazide therapy
- B. Fluid restriction
- C. Desmopressin therapy (Correct Answer)
- D. Tolvaptan therapy
- E. Amiloride therapy
Severe electrolyte disturbances Explanation: ***Desmopressin therapy***
- The patient's urine osmolality significantly increased after exogenous **ADH analog (desmopressin)** administration during the water deprivation test, indicating a renal response to ADH.
- This response points to **central diabetes insipidus**, where the body does not produce enough ADH, making desmopressin (an ADH analog) the appropriate replacement therapy.
*Hydrochlorothiazide therapy*
- **Thiazide diuretics** are sometimes used in **nephrogenic diabetes insipidus** (where kidneys don't respond to ADH) to induce a mild volume depletion, increasing proximal tubule reabsorption of water, but they are not the primary treatment for central DI.
- The patient's response to exogenous ADH rules out nephrogenic DI as the primary problem.
*Fluid restriction*
- This patient is already experiencing **polyuria** and **polydipsia**, and fluid restriction would worsen his **hypernatremia** and dehydration without addressing the underlying ADH deficiency.
- Fluid restriction is part of the diagnostic **water deprivation test**, not a therapeutic management for diabetes insipidus.
*Tolvaptan therapy*
- **Tolvaptan** is an **ADH receptor antagonist** used in conditions like **hyponatremia** due to SIADH to promote water excretion, which would be counterproductive in a patient with diabetes insipidus.
- It would worsen the patient's condition by further impairing water reabsorption and increasing urine output.
*Amiloride therapy*
- **Amiloride**, a **potassium-sparing diuretic**, is primarily used for hypertension, heart failure, and to counteract potassium loss from other diuretics.
- It has no role in the direct treatment of diabetes insipidus and would not address the ADH deficiency or renal unresponsiveness to ADH.
Severe electrolyte disturbances US Medical PG Question 5: A 39-year-old female presents with confusion. Her husband reports that she doesn't know where she is and cannot remember the date. She was recently diagnosed with small cell lung cancer. Vital signs are T 37C, HR 80, BP 120/80 mmHg, RR 14, and O2 sat 99% on room air. She is not orthostatic. Physical examination reveals moist mucous membranes and normal capillary refill. A basic metabolic profile reveals that serum sodium is 129. Regarding this patient's illness, which of the following is true?
- A. Urinary osmolarity will be < 100, and another potential cause of this disorder is excessive water drinking
- B. Urinary sodium will be > 20 and another potential cause of this disorder is renal failure
- C. Urinary sodium will be > 20 and fractional excretion of sodium will be >1%
- D. Urinary osmolarity will be > 100, and this illness will not correct with normal saline infusion (Correct Answer)
- E. Urinary sodium will be < 10, and fractional excretion of sodium will be <1%
Severe electrolyte disturbances Explanation: ***Urinary osmolarity will be > 100, and this illness will not correct with normal saline infusion***
- The patient's **hyponatremia** in the context of **small cell lung cancer** (a known cause of SIADH), euvolemia (normal vital signs, moist mucous membranes, normal capillary refill), suggests **SIADH**. In SIADH, **ADH** is inappropriately elevated, leading to water retention, dilute serum, and concentrated urine, so **urinary osmolarity will be > 100 mOsm/kg** (typically > 300 mOsm/kg).
- Since SIADH involves excess free water retention due to inappropriate ADH secretion and not volume depletion, administering **normal saline (0.9%)** can actually worsen the hyponatremia by providing additional free water without addressing the underlying ADH excess. The appropriate treatment for symptomatic SIADH is **hypertonic saline (3%)**, fluid restriction, and addressing the underlying cause.
*Urinary osmolarity will be < 100, and another potential cause of this disorder is excessive water drinking*
- In SIADH, the presence of inappropriately high ADH leads to increased water reabsorption in the collecting ducts, resulting in **concentrated urine**; therefore, **urinary osmolarity will be > 100 mOsm/kg**, not < 100.
- **Urinary osmolarity < 100 mOsm/kg** with hyponatremia suggests **primary polydipsia** (excessive water drinking), where ADH is appropriately suppressed and the kidneys produce maximally dilute urine. While polydipsia can cause hyponatremia, it is not consistent with the clinical picture of SIADH, where ADH is elevated and urine is concentrated.
*Urinary sodium will be > 20 and another potential cause of this disorder is renal failure*
- In SIADH, the kidneys continue to excrete sodium due to the expanded extracellular fluid volume even in the setting of hyponatremia, leading to a **urinary sodium concentration > 20 mEq/L** ✓.
- While **renal failure** can cause hyponatremia due to impaired free water excretion, it typically presents with volume overload, elevated BUN/creatinine, and other findings not seen in this euvolemic patient with SIADH. Renal failure is not a typical "other cause" when discussing SIADH specifically.
*Urinary sodium will be > 20 and fractional excretion of sodium will be >1%*
- In SIADH, the body experiences perceived volume expansion, causing natriuresis despite low serum sodium, resulting in **urinary sodium > 20 mEq/L** ✓.
- The **fractional excretion of sodium (FENa)** is typically **>1%** (usually 1-2%) in SIADH because the kidneys appropriately excrete sodium in response to the perceived volume expansion ✓. While this option is medically accurate for SIADH, it doesn't address the critical clinical point about treatment (that normal saline is contraindicated) and the urinary osmolarity, which are more defining diagnostic and therapeutic characteristics.
*Urinary sodium will be < 10, and fractional excretion of sodium will be <1%*
- **Urinary sodium < 10 mEq/L** and **FENa < 1%** typically indicate **hypovolemic hyponatremia** with effective arterial blood volume depletion (e.g., dehydration, heart failure, cirrhosis), where the kidneys are avidly conserving sodium and water.
- This is **not consistent with SIADH**, which presents as **euvolemic hyponatremia** where the urine is concentrated (not maximally dilute) and sodium continues to be excreted, making these values incompatible with the diagnosis.
Severe electrolyte disturbances US Medical PG Question 6: An 80-year-old male with known metastatic prostate cancer presents to your office with vague complaints of "achy bones." Strangely, he refers to you using the name of another physician. On physical exam, he is afebrile, but mildly tachycardic at 100 beats/min. Mucous membranes are dry. Cardiac exam shows regular rhythm and no murmurs. The patient has diffuse, nonfocal abdominal pain. He cannot articulate the correct date. You check the patient's serum calcium level, which is found to be 15.3 mg/dL. What is the best next step in management?
- A. Calcitonin
- B. Intravenous normal saline (Correct Answer)
- C. Furosemide
- D. Pamidronate
- E. Hemodialysis
Severe electrolyte disturbances Explanation: ***Intravenous normal saline***
- The patient exhibits classic symptoms of **hypercalcemia** (vague bone aches, confusion, dry mucous membranes, tachycardia, diffuse nonfocal abdominal pain) in the context of metastatic prostate cancer and a severely elevated serum calcium level of 15.3 mg/dL.
- **Volume expansion with intravenous normal saline** is the initial and most crucial step in managing severe hypercalcemia, as it helps to restore hydration and promote renal calcium excretion.
*Calcitonin*
- **Calcitonin** can rapidly lower serum calcium by inhibiting osteoclastic bone resorption and increasing renal calcium excretion, but its effect is typically transient and less potent than initial hydration.
- It is often used as an adjunct to saline and bisphosphonates, especially in cases where a rapid but temporary decrease in calcium is needed.
*Furosemide*
- **Furosemide** (a loop diuretic) should only be considered *after* adequate volume repletion has been achieved, as it can worsen dehydration and electrolyte abnormalities if given prematurely.
- It works by inhibiting calcium reabsorption in the loop of Henle, but **dehydration must be corrected first** to ensure effective GFR and avoid electrolyte imbalance.
*Pamidronate*
- **Pamidronate** (a bisphosphonate) is a potent inhibitor of osteoclast-mediated bone resorption and is effective in long-term management of hypercalcemia of malignancy.
- However, its onset of action is slow (2-4 days) and therefore it is not the best *initial step* for acutely symptomatic and severely hypercalcemic patients.
*Hemodialysis*
- **Hemodialysis** is reserved for severe, refractory hypercalcemia, particularly in patients with **renal failure** who cannot handle large fluid loads or excrete calcium effectively.
- While effective, it is an invasive procedure and not typically the first-line treatment for hypercalcemia of malignancy in a patient with presumably intact renal function capable of responding to hydration.
Severe electrolyte disturbances US Medical PG Question 7: A 32-year-old woman is hospitalized after developing an allergic reaction to the contrast medium used for a cerebral angiography. The study was initially ordered as part of the diagnostic approach of a suspected case of pseudotumor cerebri. Her medical history is unremarkable. On physical examination she has stable vital signs, a diffuse maculopapular rash over her neck and chest, and a mild fever. She is started on hydrocortisone and monitored for the next 8 hours. After the monitoring period, a laboratory test shows significant azotemia. The patient complains of generalized weakness and palpitations. Tall-peaked T waves are observed on ECG. Which of the following explains this clinical manifestation?
- A. Anemia
- B. Platelet dysfunction
- C. Uremic pericarditis
- D. Metabolic acidosis
- E. Hyperkalemia (Correct Answer)
Severe electrolyte disturbances Explanation: ***Hyperkalemia***
- The combination of **significant azotemia** (indicating acute kidney injury), **generalized weakness**, and **peaked T waves on ECG** are classic signs of hyperkalemia.
- The allergic reaction and subsequent treatment may have exacerbated kidney dysfunction, leading to impaired potassium excretion and subsequent elevated serum potassium levels.
*Anemia*
- While anemia can cause weakness and palpitations, it does not typically manifest with **peaked T waves** on ECG or directly explain the presence of **azotemia**.
- Anemia is common in chronic kidney disease but is not the primary cause of acute symptoms and ECG changes described here.
*Platelet dysfunction*
- Uremia can lead to **platelet dysfunction**, causing bleeding tendencies, but it does not account for the **generalized weakness**, **azotemia**, or the characteristic **peaked T waves** on ECG.
- Platelet dysfunction is typically associated with bruising or prolonged bleeding, not the cardiovascular and neurological symptoms observed.
*Uremic pericarditis*
- **Uremic pericarditis** can cause chest pain, a friction rub, and sometimes palpitations, but it does not directly explain the **peaked T waves** or generalized weakness in the context of acute azotemia.
- The primary symptoms of pericarditis are often related to inflammation of the pericardium rather than electrolyte imbalances.
*Metabolic acidosis*
- **Metabolic acidosis** is common in acute kidney injury and can contribute to weakness and dyspnea, but it does not directly cause **peaked T waves** on ECG.
- While clinically important, acidosis itself doesn't explain the specific ECG findings, which are more indicative of hyperkalemia.
Severe electrolyte disturbances US Medical PG Question 8: A 25-year-old woman is brought to the emergency department 12 hours after ingesting 30 tablets of an unknown drug in a suicide attempt. The tablets belonged to her father, who has a chronic heart condition. She has had nausea and vomiting. She also reports blurring and yellowing of her vision. Her temperature is 36.7°C (98°F), pulse is 51/min, and blood pressure is 108/71 mm Hg. Abdominal examination shows diffuse tenderness with no guarding or rebound. Bowel sounds are normal. An ECG shows prolonged PR-intervals and flattened T-waves. Further evaluation is most likely to show which of the following electrolyte abnormalities?
- A. Increased serum K+ (Correct Answer)
- B. Decreased serum K+
- C. Decreased serum Na+
- D. Increased serum Na+
- E. Increased serum Ca2+
Severe electrolyte disturbances Explanation: ***Increased serum K+***
- The patient presents with classic symptoms of **digoxin toxicity**, including **nausea, vomiting, blurry and yellow vision, bradycardia**, and ECG changes like **prolonged PR interval** and **flattened T-waves**.
- **Digoxin inhibits the Na+/K+-ATPase pump**, leading to an increase in extracellular potassium as potassium cannot enter the cells.
*Decreased serum K+*
- While hypokalemia can exacerbate digoxin toxicity by increasing digoxin binding to the Na+/K+-ATPase, digoxin overdose itself typically causes **hyperkalemia** due to its direct effect on the pump.
- ECG changes like **flattened T-waves** can be seen in hypokalemia, but the overall clinical picture, especially the history of overdose and bradycardia, points more strongly to digoxin toxicity with hyperkalemia.
*Decreased serum Na+*
- **Hyponatremia** is not a characteristic feature of acute digoxin overdose.
- Digoxin primarily affects potassium and calcium channels, with less direct impact on sodium levels, unless related to fluid status changes which are not indicated here.
*Increased serum Na+*
- **Hypernatremia** is not typically associated with digoxin toxicity.
- Digoxin's mechanism of action does not directly lead to increased serum sodium; rather, it primarily inhibits the Na+/K+-ATPase.
*Increased serum Ca2+*
- Digoxin **increases intracellular calcium** by inhibiting the Na+/K+-ATPase, which indirectly leads to increased Na+/Ca2+ exchanger activity.
- However, this primarily affects intracellular levels and **does not typically result in increased serum calcium**.
Severe electrolyte disturbances US Medical PG Question 9: A 62-year-old man comes to the emergency department for severe, acute right leg pain. The patient's symptoms began suddenly 4 hours ago, while he was reading the newspaper. He has poorly-controlled hypertension and osteoarthritis. He has smoked one pack of cigarettes daily for 31 years. Current medications include lisinopril, metoprolol succinate, and ibuprofen. He appears to be in severe pain and is clutching his right leg. His temperature is 37.4°C (99.3°F), pulse is 102/min and irregularly irregular, respirations are 19/min, and blood pressure is 152/94 mm Hg. The right leg is cool to the touch, with decreased femoral, popliteal, posterior tibial, and dorsalis pedis pulses. There is moderate weakness and decreased sensation in the right leg. An ECG shows absent P waves and a variable R-R interval. Right leg Doppler study shows inaudible arterial signal and audible venous signal. Angiography shows 90% occlusion of the right common femoral artery. In addition to initiating heparin therapy, which of the following is the most appropriate next step in management?
- A. Surgical bypass of the affected vessel
- B. Percutaneous transluminal angioplasty
- C. Amputation of the affected limb
- D. Open embolectomy
- E. Balloon catheter embolectomy (Correct Answer)
Severe electrolyte disturbances Explanation: **Balloon catheter embolectomy**
- The patient presents with **acute limb ischemia** characterized by sudden onset of severe pain, cool extremity, absent pulses, motor weakness, and sensory deficits. The **irregularly irregular pulse** and **absent P waves on ECG** are highly suggestive of **atrial fibrillation**, a common source of arterial emboli.
- Given the acute nature, the presence of a probable embolic source, and the Doppler findings of an **inaudible arterial signal**, **balloon catheter embolectomy** (e.g., using a Fogarty catheter) is the most appropriate and rapid intervention to restore blood flow and salvage the limb. This procedure directly retrieves the embolus.
*Surgical bypass of the affected vessel*
- **Surgical bypass** is typically indicated for **chronic limb ischemia** or extensive, complex occlusions that are not amenable to less invasive techniques.
- It is a more extensive procedure with a longer recovery time and is not the first-line treatment for acute embolic occlusion.
*Percutaneous transluminal angioplasty*
- **Percutaneous transluminal angioplasty** (PTA) is generally used for **atherosclerotic stenoses** or occlusions rather than acute arterial emboli.
- While it can be performed in some cases of acute limb ischemia, it is less effective than embolectomy for removing a fresh, mobile clot, especially in large vessels.
*Amputation of the affected limb*
- **Amputation** is considered only when the limb is **irreversibly ischemic** and non-viable, or when revascularization attempts have failed.
- In this case, the patient has moderate weakness and decreased sensation, indicating that the limb is still viable and potentially salvageable.
*Open embolectomy*
- **Open embolectomy** is a surgical procedure to remove an embolus, similar in goal to balloon catheter embolectomy but often performed with a larger incision.
- While effective, **balloon catheter embolectomy** is generally preferred due to its less invasive nature and ability to be performed rapidly, especially in emergent situations.
Severe electrolyte disturbances US Medical PG Question 10: For evaluating the functioning of a health center, which is the most important determinant for assessing clinical management?
- A. Structure
- B. Input
- C. Process (Correct Answer)
- D. Outcome
- E. Output
Severe electrolyte disturbances Explanation: ***Process***
- Evaluating the **process** involves assessing the actual delivery of care, including adherence to clinical guidelines, patient-provider interactions, and the timeliness and appropriateness of services. This directly reflects the quality of **clinical management**.
- It focuses on *how* care is provided, which is crucial for identifying areas of strength and weakness in the day-to-day operations of a health center's clinical functions.
*Structure*
- **Structure** refers to the resources and settings in which care is provided, such as facilities, equipment, staff qualifications, and organizational policies.
- While important, a good structure does not guarantee good clinical management; the structure offers the potential for quality, but the actual delivery of care (process) is what matters most for assessment.
*Input*
- **Input** is a broad term often overlapping with structure, referring to the resources poured into the system like funding, staff, and materials.
- Like structure, input provides the necessary components, but evaluating them alone does not directly assess the *effectiveness* or *quality* of clinical management.
*Output*
- **Output** refers to the immediate results of service delivery, such as the number of patients seen, procedures performed, or services rendered.
- While outputs can be measured, they represent quantity rather than quality and do not directly assess the appropriateness or effectiveness of clinical management itself.
*Outcome*
- **Outcome** measures the end results of care, such as patient health status, satisfaction, or mortality rates.
- While outcomes are critical, they are often influenced by many factors beyond direct clinical management (e.g., patient adherence, social determinants of health) and may not immediately reflect the quality of the *process* of care delivery itself.
More Severe electrolyte disturbances US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.