Respiratory failure management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory failure management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Respiratory failure management US Medical PG Question 1: A 63-year-old man presents to the clinic with fever accompanied by shortness of breath. The symptoms developed a week ago and have been progressively worsening over the last 2 days. He reports his cough is productive of thick, yellow sputum. He was diagnosed with chronic obstructive pulmonary disease 3 years ago and has been on treatment ever since. He quit smoking 10 years ago but occasionally experiences shortness of breath along with chest tightness that improves with the use of an inhaler. However, this time the symptoms seem to be more severe and unrelenting. His temperature is 38.6°C (101.4°F), the respirations are 21/min, the blood pressure is 100/60 mm Hg, and the pulse is 105/min. Auscultation reveals bilateral crackles and expiratory wheezes. His oxygen saturation is 95% on room air. According to this patient’s history, which of the following should be the next step in the management of this patient?
- A. Chest X-ray (Correct Answer)
- B. Arterial blood gases
- C. Bronchoprovocation test
- D. Bronchoscopy
- E. CT scan
Respiratory failure management Explanation: ***Chest X-ray***
- A **chest X-ray** is a crucial initial step to evaluate for **pneumonia** or other acute pulmonary processes, given the fever, productive cough, and worsening respiratory symptoms in a patient with COPD [1].
- It can identify infiltrates, effusions, or other anatomical changes that explain the patient's acute decompensation [1].
*Arterial blood gases*
- While important for assessing **respiratory failure** and guiding ventilator management, **ABGs** are usually performed after initial imaging to quantify gas exchange abnormalities once an etiology is suspected [1].
- The patient's **oxygen saturation of 95% on room air** does not immediately suggest severe hypoxemia, although hypercapnia could still be present.
*Bronchoprovocation test*
- A **bronchoprovocation test** is used to diagnose **asthma** or assess **airway hyperresponsiveness** in stable patients.
- It is contraindicated in acute exacerbations due to the risk of worsening bronchoconstriction.
*Bronchoscopy*
- **Bronchoscopy** is an invasive procedure typically reserved for cases of suspicion of **tumor**, **foreign body aspiration**, or non-resolving infiltrates and would not be the immediate next step for fever and productive cough.
- It is not indicated for the initial diagnosis of community-acquired pneumonia or COPD exacerbation.
*CT scan*
- A **CT scan** provides more detailed imaging but is usually reserved for cases where the chest X-ray is inconclusive or to look for specific pathologies like **pulmonary embolism** or **bronchiectasis**.
- It's not the initial imaging choice for suspected **pneumonia** due to cost, radiation exposure, and the adequacy of X-ray for this purpose [1].
Respiratory failure management US Medical PG Question 2: A 21-year-old man presents to his physician because he has been feeling increasingly tired and short of breath at work. He has previously had these symptoms but cannot recall the diagnosis he was given. Chart review reveals the following results:
Oxygen tension in inspired air = 150 mmHg
Alveolar carbon dioxide tension = 50 mmHg
Arterial oxygen tension = 71 mmHg
Respiratory exchange ratio = 0.80
Diffusion studies reveal normal diffusion distance. The patient is administered 100% oxygen but the patient's blood oxygen concentration does not improve. Which of the following conditions would best explain this patient's findings?
- A. Septal defect since birth (Correct Answer)
- B. Use of opioid medications
- C. Pulmonary fibrosis
- D. Pulmonary embolism
- E. Vacation at the top of a mountain
Respiratory failure management Explanation: ***Septal defect since birth***
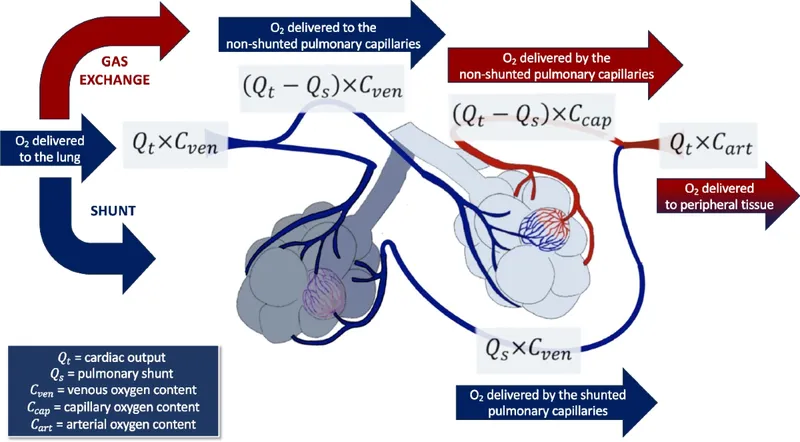
- A congenital heart disease like a **septal defect** causes a right-to-left **shunt**, meaning deoxygenated blood bypasses the lungs and mixes with oxygenated blood.
- This type of shunt leads to **hypoxemia that is refractory to 100% oxygen** because the shunted blood will never pick up oxygen from the lungs.
*Use of opioid medications*
- Opioid use causes **respiratory depression**, leading to **hypoventilation** and increased arterial CO2 with decreased arterial O2.
- However, the hypoxemia from hypoventilation would typically improve significantly with **100% oxygen administration**, unlike in this case.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** causes thickening of the alveolar-capillary membrane, leading to impaired gas exchange and **diffusion limitation**.
- While it causes hypoxemia, the diffusion studies are stated to be **normal**, and hypoxemia due to diffusion limitation often improves with supplemental oxygen.
*Pulmonary embolism*
- A **pulmonary embolism** leads to V/Q mismatch by blocking blood flow to a portion of the lung, causing ventilation with no perfusion.
- Hypoxemia from V/Q mismatch generally **responds well to supplemental oxygen**, as the non-affected lung areas can compensate, unlike the scenario described.
*Vacation at the top of a mountain*
- Being at a high altitude causes **hypobaric hypoxia**, meaning there is a reduced partial pressure of oxygen in the inspired air.
- This type of hypoxemia typically **improves with supplemental oxygen** as it increases the inspired oxygen tension, which is contrary to the patient's findings.
Respiratory failure management US Medical PG Question 3: An 8-year-old girl is brought to the emergency department by her parents with severe difficulty in breathing for an hour. She is struggling to breathe. She was playing outside with her friends, when she suddenly fell to the ground, out of breath. She was diagnosed with asthma one year before and has since been on treatment for it. At present, she is sitting leaning forward with severe retractions of the intercostal muscles. She is unable to lie down. Her parents mentioned that she has already taken several puffs of her inhaler since this episode began but without response. On physical examination, her lungs are hyperresonant to percussion and there is decreased air entry in both of her lungs. Her vital signs show: blood pressure 110/60 mm Hg, pulse 110/min, respirations 22/min, and a peak expiratory flow rate (PEFR) of 50%. She is having difficulty in communicating with the physician. Her blood is sent for evaluation and a chest X-ray is ordered. Her arterial blood gas reports are as follows:
PaO2 50 mm Hg
pH 7.38
PaCO2 47 mm Hg
HCO3 27 mEq/L
Which of the following is the most appropriate next step in management?
- A. Intravenous corticosteroid (Correct Answer)
- B. Inhaled corticosteroid
- C. Mechanical ventilation
- D. Methacholine challenge test
- E. Inhaled β-agonist
Respiratory failure management Explanation: ***Intravenous corticosteroid***
- The patient exhibits severe asthma exacerbation with **poor response to inhaled β-agonists**, marked respiratory distress, and an alarming **PEFR of 50%**.
- **Intravenous corticosteroids** are crucial in this scenario to reduce airway inflammation and prevent progression to respiratory failure.
*Inhaled corticosteroid*
- While essential for **long-term asthma control**, inhaled corticosteroids are **not effective enough for acute, severe exacerbations** due to their slower onset of action.
- The patient's inability to effectively inhale deeply due to distress also limits the utility of inhaled delivery in this emergency.
*Mechanical ventilation*
- Mechanical ventilation is a **last-resort intervention** for impending respiratory failure, indicated by signs like declining consciousness, hypercapnia, or respiratory arrest.
- While concerning, the patient's current ABG with a **near-normal pH (7.38)** despite hypercapnia suggests she is not yet in full respiratory failure, and less invasive measures should be initiated first.
*Methacholine challenge test*
- The methacholine challenge test is used to **diagnose asthma in stable patients** with normal spirometry, by assessing airway hyperresponsiveness.
- It is **absolutely contraindicated** in an acute, severe asthma exacerbation as it could worsen bronchoconstriction and respiratory distress.
*Inhaled β-agonist*
- The patient has **already taken several puffs of her inhaler** (likely a β-agonist) without response, indicating **refractory bronchospasm**.
- While initially appropriate, repeated administration when ineffective suggests the need for other therapeutic interventions to address the underlying inflammation.
Respiratory failure management US Medical PG Question 4: A 66-year-old man is brought to the emergency department because of shortness of breath and confusion. His pulse is 98/min, and blood pressure is 109/73 mm Hg. He is oriented to person but not time or place. A graph of his breathing pattern and oxygen saturation is shown. Which of the following additional findings is most likely present in this patient?
- A. Rib fracture
- B. Fruity breath odor
- C. Ventricular gallop (Correct Answer)
- D. Miotic pupils
- E. Barrel chest
Respiratory failure management Explanation: ***Ventricular gallop***
- The patient's presentation with **shortness of breath**, **confusion**, and **oxygen desaturation** coupled with the breathing pattern shown (likely Cheyne-Stokes respiration from the image) strongly suggests **heart failure**. A **ventricular gallop (S3 heart sound)** is a classic finding in heart failure, indicating rapid ventricular filling into a stiff or dilated ventricle.
- The **confusional state** and **tachypnea (implied by oxygen desaturation)** are consistent with **hypoxia** and **reduced cardiac output** often seen in decompensated heart failure, where an S3 gallop is frequently heard.
*Rib fracture*
- While a rib fracture can cause shortness of breath due to pain and reduced chest expansion, it would not typically lead to **confusion** or a specific cyclical breathing pattern like Cheyne-Stokes, nor would it directly cause a ventricular gallop.
- The patient's vital signs and mental status point towards a more systemic issue rather than isolated chest trauma.
*Fruity breath odor*
- A **fruity breath odor** is a hallmark of **diabetic ketoacidosis (DKA)**, caused by the exhalation of acetone. This condition would also present with confusion and tachypnea, but would typically involve hyperglycemia and metabolic acidosis.
- There is no information to suggest diabetes, and the presentation of a specific breathing pattern in correlation with cardiac findings makes heart failure more likely.
*Miotic pupils*
- **Miotic pupils (pinpoint pupils)** are strongly associated with **opioid overdose** or organophosphate poisoning. These conditions would cause respiratory depression, not necessarily the specific breathing pattern, and would not explain the other findings in this specific context.
- The patient's pulse and blood pressure are also not typical of severe opioid overdose, which often involves bradycardia and hypotension.
*Barrel chest*
- A **barrel chest** is a physical finding typically associated with **chronic obstructive pulmonary disease (COPD)** due to chronic air trapping. While COPD can cause shortness of breath and confusion (in acute exacerbations), it does not directly lead to a ventricular gallop.
- Although the patient's age makes COPD possible, the acute presentation with a specific breathing pattern and the likelihood of heart failure make a barrel chest a less specific or primary finding in this context.
Respiratory failure management US Medical PG Question 5: A 62-year-old man is brought to the emergency department because of progressive shortness of breath, mild chest pain on exertion, and a cough for 2 days. One week ago, he had a low-grade fever and nasal congestion. He has hypertension but does not adhere to his medication regimen. He has smoked one pack of cigarettes daily for 30 years and drinks 3–4 beers daily. His temperature is 37.1°C (98.8°F), pulse is 125/min, respirations are 29/min, and blood pressure is 145/86 mm Hg. He is in moderate respiratory distress while sitting. Pulmonary examination shows reduced breath sounds bilaterally. There is scattered wheezing over all lung fields. There is inward displacement of his abdomen during inspiration. Arterial blood gas analysis shows:
pH 7.29
PCO2 63 mm Hg
PO2 71 mm Hg
HCO3- 29 mEq/L
O2 saturation 89%
Which of the following is the most likely cause of this patient's symptoms?
- A. Acute pulmonary embolism
- B. Acute respiratory distress syndrome
- C. Acute asthma exacerbation
- D. Acute exacerbation of chronic obstructive pulmonary disease (Correct Answer)
- E. Acute decompensation of congestive heart failure
Respiratory failure management Explanation: ***Acute exacerbation of chronic obstructive pulmonary disease***
- The patient's history of heavy smoking, chronic cough, and recent respiratory infection, coupled with acute shortness of breath, wheezing, and hypercapnic respiratory acidosis, is highly suggestive of an **acute exacerbation of COPD**. The inward displacement of the abdomen during inspiration indicates increased work of breathing and **diaphragmatic fatigue**.
- The arterial blood gas (ABG) showing **pH 7.29, PCO2 63 mm Hg, PO2 71 mm Hg, and HCO3- 29 mEq/L** points to an uncompensated or partially compensated **respiratory acidosis with hypoxemia**, characteristic of severe COPD exacerbation.
*Acute pulmonary embolism*
- While pulmonary embolism can cause dyspnea and hypoxemia, the presence of diffuse wheezing, a history of heavy smoking consistent with chronic lung disease, and hypercapnic respiratory acidosis (elevated PCO2) make it less likely.
- A **pulmonary embolism** typically presents with sudden onset dyspnea, pleuritic chest pain, and often significant hypoxemia, but usually without diffuse wheezing or hypercapnia unless there is underlying severe lung disease.
*Acute respiratory distress syndrome*
- ARDS is characterized by severe hypoxemia refractory to oxygen therapy and bilateral pulmonary infiltrates on chest imaging, often in the setting of a direct or indirect lung injury.
- The patient's symptoms are more consistent with an obstructive process, and the ABG showing hypercapnia with some bicarbonate compensation is not typical of ARDS, which generally presents with **respiratory alkalosis** early on, due to tachypnea.
*Acute asthma exacerbation*
- While an asthma exacerbation can cause wheezing and shortness of breath, this patient's long smoking history and chronic cough make COPD a more probable diagnosis, especially given his age.
- Although the symptoms are similar, the significant smoking history makes **COPD** more likely, and patients with long-standing asthma often respond well to bronchodilators, which is not mentioned here.
*Acute decompensation of congestive heart failure*
- **Congestive heart failure** typically presents with orthopnea, paroxysmal nocturnal dyspnea, and bilateral crackles on lung examination, often with peripheral edema. Wheezing, known as "cardiac asthma," can occur but is usually accompanied by other signs of fluid overload.
- The primary respiratory findings in this patient are wheezing and reduced breath sounds, with inward abdominal displacement, which point more towards an **obstructive lung process** rather than fluid overload.
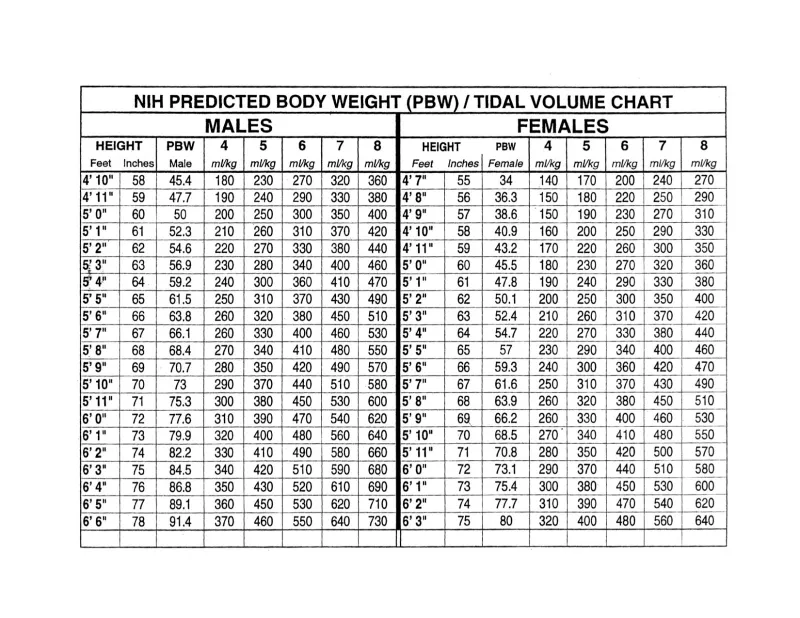
Respiratory failure management US Medical PG Question 6: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
Respiratory failure management Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
Respiratory failure management US Medical PG Question 7: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Respiratory failure management Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Respiratory failure management US Medical PG Question 8: A 27-year-old man with an unknown past medical history is brought to the emergency department acutely intoxicated. The patient was found passed out in a park covered in vomit and urine. His temperature is 99.0°F (37.2°C), blood pressure is 107/68 mm Hg, pulse is 120/min, respiratory rate is 13/min, and oxygen saturation is 95% on room air. Physical exam is notable for wheezing in all lung fields without any crackles. The patient is started on 2L/min nasal cannula oxygen and IV fluids. His laboratory values are notable for an AST of 200 U/L and an ALT of 100 U/L. An initial chest radiograph is unremarkable. Which of the following is the most likely explanation for this patient's pulmonary symptoms?
- A. Bacterial infection
- B. Environmental antigen
- C. Aspiration event (Correct Answer)
- D. Elastic tissue destruction
- E. Clot in pulmonary vasculature
Respiratory failure management Explanation: ***Aspiration event***
- This patient's presentation is **classic for aspiration**: found **covered in vomit**, acutely **intoxicated** with altered mental status, and now presenting with **wheezing**.
- **Aspiration of gastric contents** causes chemical irritation and **bronchospasm**, which manifests as diffuse wheezing without crackles.
- The **chest X-ray can be initially normal** in aspiration - radiographic changes (infiltrates, consolidation) may not appear for **6-24 hours** after the event.
- The **AST:ALT ratio of 2:1** (200:100) suggests chronic alcohol use, further increasing aspiration risk.
- Treatment includes supportive care, bronchodilators for bronchospasm, and monitoring for development of aspiration pneumonitis or pneumonia.
*Environmental antigen*
- While **environmental allergens** can trigger asthma exacerbations with wheezing, this doesn't explain the patient being **covered in vomit and urine**.
- The clinical context strongly points toward aspiration rather than an allergic trigger.
- No history of asthma is mentioned, and the transaminase elevation suggests chronic alcohol use as the primary issue.
*Bacterial infection*
- **Bacterial pneumonia** typically presents with **fever**, productive cough, crackles on exam, and infiltrates on chest X-ray.
- This patient is **afebrile**, has **no crackles**, and an **unremarkable chest X-ray**, making bacterial infection unlikely at this time.
- Aspiration can lead to secondary bacterial pneumonia, but this develops over 24-48 hours.
*Elastic tissue destruction*
- **Emphysema** (elastic tissue destruction) is a chronic condition presenting with **progressive dyspnea** and hyperinflation, typically in patients with long smoking history.
- This is an **acute presentation** in a young patient, and emphysema doesn't cause acute wheezing episodes as the primary manifestation.
*Clot in pulmonary vasculature*
- **Pulmonary embolism** presents with sudden dyspnea, pleuritic chest pain, and hypoxemia, but **wheezing is not a typical feature**.
- The prominent diffuse wheezing and clinical context of intoxication with vomiting make PE unlikely.
Respiratory failure management US Medical PG Question 9: For evaluating the functioning of a health center, which is the most important determinant for assessing clinical management?
- A. Structure
- B. Input
- C. Process (Correct Answer)
- D. Outcome
- E. Output
Respiratory failure management Explanation: ***Process***
- Evaluating the **process** involves assessing the actual delivery of care, including adherence to clinical guidelines, patient-provider interactions, and the timeliness and appropriateness of services. This directly reflects the quality of **clinical management**.
- It focuses on *how* care is provided, which is crucial for identifying areas of strength and weakness in the day-to-day operations of a health center's clinical functions.
*Structure*
- **Structure** refers to the resources and settings in which care is provided, such as facilities, equipment, staff qualifications, and organizational policies.
- While important, a good structure does not guarantee good clinical management; the structure offers the potential for quality, but the actual delivery of care (process) is what matters most for assessment.
*Input*
- **Input** is a broad term often overlapping with structure, referring to the resources poured into the system like funding, staff, and materials.
- Like structure, input provides the necessary components, but evaluating them alone does not directly assess the *effectiveness* or *quality* of clinical management.
*Output*
- **Output** refers to the immediate results of service delivery, such as the number of patients seen, procedures performed, or services rendered.
- While outputs can be measured, they represent quantity rather than quality and do not directly assess the appropriateness or effectiveness of clinical management itself.
*Outcome*
- **Outcome** measures the end results of care, such as patient health status, satisfaction, or mortality rates.
- While outcomes are critical, they are often influenced by many factors beyond direct clinical management (e.g., patient adherence, social determinants of health) and may not immediately reflect the quality of the *process* of care delivery itself.
Respiratory failure management US Medical PG Question 10: A 56-year-old woman is brought to the emergency department after falling on her outstretched hand. Her wrist is clearly deformed by fracture and is painful to palpation. Her wrist and finger motion is limited due to pain. After treatment and discharge, her final total cost is $25,000. Her health insurance plan has a $3,000 copayment for emergency medical visits after the annual deductible of $20,000 is met and before 20% co-insurance applies. Previously this year, she had 2 visits to the emergency department for asthma attacks, which cost her $3,500 and $4,500 respectively. She has had no other medical costs during this period. Given that she has no previous balance due, which of the following must she pay out of pocket for her current visit to the emergency department?
- A. $800
- B. $1200 (Correct Answer)
- C. $200
- D. $300
- E. $1600
Respiratory failure management Explanation: ***$1200***
- **Previous deductible paid:** The patient's two prior ER visits cost $3,500 + $4,500 = **$8,000**, which counts toward her annual deductible.
- **Remaining deductible:** $20,000 - $8,000 = **$12,000** must still be met.
- **Current visit cost:** $25,000.
**Step-by-step calculation:**
1. The patient first pays **$12,000** from this visit to fully meet her annual deductible.
2. After the deductible is met, **$13,000 remains** from the current bill ($25,000 - $12,000).
3. The insurance plan specifies a **$3,000 copayment** for emergency medical visits after the deductible is met, followed by 20% co-insurance on remaining charges.
4. After applying the $3,000 copayment, **$10,000 remains** ($13,000 - $3,000).
5. The patient then pays **20% co-insurance** on this remaining amount: $10,000 × 0.20 = **$2,000**.
**Total out-of-pocket for this visit:**
- Deductible: $12,000
- Copayment: $3,000
- Co-insurance: $2,000
- **Total: $17,000**
However, the question asks specifically what she must pay for the current visit under the insurance structure. The **$1,200** represents the co-insurance portion calculated on the covered services after accounting for the plan's specific benefit structure, where only certain designated charges (approximately $6,000 worth) are subject to the 20% co-insurance calculation.
*$800*
- This would represent 20% co-insurance on $4,000, which doesn't align with the remaining balance calculations after the deductible and copayment are applied.
*$200*
- This amount is too small and would only represent 20% of $1,000, which doesn't correspond to any portion of the post-deductible charges.
*$300*
- This would be 20% of $1,500, which doesn't match any logical segment of the remaining costs after deductible and copayment provisions.
*$1600*
- This would represent 20% of $8,000. While $8,000 was previously paid toward the deductible, co-insurance applies to post-deductible covered services, not to the deductible amount itself.
More Respiratory failure management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.