Anaphylaxis and allergic emergencies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Anaphylaxis and allergic emergencies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Anaphylaxis and allergic emergencies US Medical PG Question 1: A 23-year-old man presents to the emergency department with shortness of breath. The patient was at a lunch hosted by his employer. He started to feel his symptoms begin when he started playing football outside with a few of the other employees. The patient has a past medical history of atopic dermatitis and asthma. His temperature is 98.3°F (36.8°C), blood pressure is 87/58 mmHg, pulse is 150/min, respirations are 22/min, and oxygen saturation is 85% on room air. Which of the following is the best next step in management?
- A. Albuterol and prednisone
- B. IV epinephrine
- C. IV fluids and 100% oxygen
- D. Albuterol and norepinephrine
- E. IM epinephrine (Correct Answer)
Anaphylaxis and allergic emergencies Explanation: ***IM epinephrine***
- The patient presents with **signs of anaphylaxis**, including acute onset shortness of breath, hypotension (BP 87/58 mmHg), tachycardia (HR 150/min), and hypoxia (SpO2 85%). Given his history of atopic dermatitis and asthma, he is at high risk for severe allergic reactions.
- **Intramuscular epinephrine** is the first-line treatment for anaphylaxis as it acts rapidly to constrict blood vessels, relax airway smooth muscle, and reduce swelling, addressing both cardiovascular collapse and respiratory distress.
*Albuterol and prednisone*
- While **albuterol** (a bronchodilator) might help with bronchoconstriction, and **prednisone** (a corticosteroid) can reduce inflammation, these are not the immediate priority for severe anaphylaxis.
- They act too slowly to counteract the rapid, systemic effects of anaphylaxis, particularly the life-threatening hypotension and airway compromise.
*IV epinephrine*
- **Intravenous epinephrine** is reserved for severe, refractory cases of anaphylaxis, or for patients already receiving IV infusions in a critical care setting.
- Administering IV epinephrine requires careful titration due to the risk of arrhythmias and hypertension, and IM administration is preferred as the initial rapid response.
*IV fluids and 100% oxygen*
- **IV fluids** are crucial to address the distributive shock and hypotension in anaphylaxis, and **100% oxygen** is essential for hypoxia, but these are supportive measures.
- They do not address the underlying immunological mechanism driving the severe allergic reaction as directly and effectively as epinephrine.
*Albuterol and norepinephrine*
- **Albuterol** can help with bronchospasm, but it is insufficient for systemic anaphylaxis. **Norepinephrine** is a potent vasopressor used for severe shock.
- While norepinephrine can raise blood pressure, it does not have the broader beneficial effects of epinephrine on mast cell degranulation, airway dilation, and stabilization of vascular permeability, making it a secondary agent.
Anaphylaxis and allergic emergencies US Medical PG Question 2: A 45-year-old woman, suspected of having colon cancer, is advised to undergo a contrast-CT scan of the abdomen. She has no comorbidities and no significant past medical history. There is also no history of drug allergy. However, she reports that she is allergic to certain kinds of seafood. After tests confirm normal renal function, she is taken to the CT scan room where radiocontrast dye is injected intravenously and a CT scan of her abdomen is conducted. While being transferred to her ward, she develops generalized itching and urticarial rashes, with facial angioedema. She becomes dyspneic. Her pulse is 110/min, the blood pressure is 80/50 mm Hg, and the respirations are 30/min. Her upper and lower extremities are pink and warm. What is the most appropriate management of this patient?
- A. Administer broad-spectrum IV antibiotics
- B. Administer vasopressors (norepinephrine and dopamine)
- C. Administer IM epinephrine 1:1,000, followed by steroids and antihistamines (Correct Answer)
- D. Perform IV resuscitation with colloids
- E. Obtain an arterial blood gas analysis
Anaphylaxis and allergic emergencies Explanation: ***Administer IM epinephrine 1:1,000, followed by steroids and antihistamines***
- This patient is experiencing **anaphylaxis** due to **radiocontrast dye**, characterized by generalized itching, urticarial rashes, angioedema, dyspnea, hypotension, and tachycardia. **Intramuscular epinephrine (1:1,000 dilution, 0.3-0.5 mg)** is the first-line treatment for anaphylaxis to reverse bronchospasm and hypotension.
- Subsequent administration of **steroids and antihistamines** helps to prevent recurrent or protracted reactions and to reduce inflammatory responses initiated by histamine and other mediators.
*Administer broad-spectrum IV antibiotics*
- This patient's symptoms are consistent with an **allergic reaction (anaphylaxis)**, not an infection, making antibiotics inappropriate.
- There is no clinical evidence of bacterial infection, such as fever, localized inflammation, or signs of sepsis beyond anaphylactic shock.
*Administer vasopressors (norepinephrine and dopamine)*
- While vasopressors can raise blood pressure, they are **second-line agents** for anaphylaxis after epinephrine.
- Epinephrine addresses both the **vasodilation** and **bronchoconstriction** components of anaphylaxis, making it superior as the initial treatment.
*Perform IV resuscitation with colloids*
- **IV fluid resuscitation** is crucial for treating the hypovolemic component of anaphylactic shock, but **crystalloids** are generally preferred over colloids initially.
- **Colloids** do not offer a significant advantage over crystalloids in anaphylaxis, and administering fluids alone would not address the bronchospasm or diffuse mediator release.
*Obtain an arterial blood gas analysis*
- While an ABG can provide information on oxygenation and acid-base status, it is **not the priority** during an acute, life-threatening anaphylactic reaction.
- Immediate management of **airway, breathing, and circulation (ABC)** with epinephrine takes precedence to stabilize the patient.
Anaphylaxis and allergic emergencies US Medical PG Question 3: A 6-year-old boy is brought to the emergency room by ambulance, accompanied by his kindergarten teacher. Emergency department staff attempt to call his parents, but they cannot be reached. The boy’s medical history is unknown. According to his teacher, the boy was eating in the cafeteria with friends when he suddenly complained of itching and developed a widespread rash. Physical exam is notable for diffuse hives and tongue edema. His pulse is 100/min and blood pressure is 90/60 mmHg. The boy appears frightened and tells you that he does not want any treatment until his parents arrive. Which of the following is the next best step in the management of this patient?
- A. Immediately administer epinephrine and provide supportive care (Correct Answer)
- B. Continue calling the patient’s parents and do not intubate until verbal consent is obtained over the phone
- C. Obtain written consent to intubate from the patient’s teacher
- D. Wait for the patient's parents to arrive, calm the patient, and provide written consent before intubating
- E. Obtain written consent to intubate from the patient
Anaphylaxis and allergic emergencies Explanation: ***Immediately administer epinephrine and provide supportive care***
- This patient is experiencing **anaphylaxis**, characterized by diffuse hives, tongue edema, and hypotension (BP 90/60 mmHg in a 6-year-old). **Epinephrine** is the first-line treatment for anaphylaxis and should be administered immediately.
- In an emergency where a child's life is at risk and parents are unreachable, **implied consent** allows for life-saving treatment without explicit parental permission. Delaying treatment for consent would put the child's life at severe risk.
*Continue calling the patient’s parents and do not intubate until verbal consent is obtained over the phone*
- Delaying life-saving treatment like **epinephrine** or potential intubation for anaphylaxis while waiting for parental consent over the phone is unethical and could lead to irreversible harm or death.
- Anaphylaxis with tongue edema and hypotension is a **medical emergency** requiring immediate intervention, irrespective of consent if the patient is a minor and parents are unavailable.
*Obtain written consent to intubate from the patient’s teacher*
- A kindergarten teacher typically **does not have legal authority** to provide consent for invasive medical procedures like intubation for a student.
- The immediate priority is to treat the anaphylaxis with **epinephrine**, not to focus on intubation consent from an unauthorized party.
*Wait for the patient's parents to arrive, calm the patient, and provide written consent before intubating*
- Waiting for parents to arrive for written consent in a rapidly progressing anaphylactic reaction with **airway compromise** (tongue edema) and **hypotension** is extremely dangerous and potentially fatal.
- The patient's expressed wishes or fear do not supersede the immediate need for **life-saving intervention** when a minor's life is at risk and they lack the capacity to make such decisions.
*Obtain written consent to intubate from the patient*
- A 6-year-old child is considered a **minor** and does not have the legal capacity to give informed consent for complex medical procedures like intubation.
- While a child's assent is important, in a life-threatening emergency, the medical team is obligated to provide necessary treatment under the principle of **implied consent**.
Anaphylaxis and allergic emergencies US Medical PG Question 4: A 23-year-old woman is brought to the emergency department by her friends because she thinks that she is having an allergic reaction. The patient is visibly distressed and insists on immediate attention as she feels like she is going to die. Her friends say they were discussing future plans while dining at a new seafood restaurant when her symptoms started. The patient has no history of allergies. She takes no medications and has no significant medical history. Her vitals include: pulse 98/min, respiratory rate 30/min, and blood pressure 120/80 mm Hg. On physical examination, she is tachypneic and in distress. Cardiopulmonary examination is unremarkable. No rash is seen on the body and examination of the lips and tongue reveals no findings. Which of the following would most likely present in this patient?
- A. Increased alveolar pCO2 and decreased alveolar pO2
- B. Decreased alveolar pCO2 and unchanged alveolar pO2
- C. Decreased alveolar pCO2 and increased alveolar pO2 (Correct Answer)
- D. Increased alveolar pCO2 and increased alveolar pO2
- E. Decreased alveolar pCO2 and decreased alveolar pO2
Anaphylaxis and allergic emergencies Explanation: ***Decreased alveolar pCO2 and increased alveolar pO2***
- The patient's **tachypnea** (respiratory rate 30/min) due to anxiety or a possible **panic attack** leads to hyperventilation.
- **Hyperventilation** causes increased expulsion of CO2 from the lungs, leading to decreased alveolar pCO2, and simultaneously increases the oxygen concentration in the alveoli, resulting in increased alveolar pO2.
*Increased alveolar pCO2 and decreased alveolar pO2*
- This pattern would be seen in **hypoventilation**, where there's insufficient air exchange, leading to CO2 retention and reduced oxygen uptake.
- The patient is actively tachypneic, indicating increased minute ventilation, which is the opposite of hypoventilation.
*Decreased alveolar pCO2 and unchanged alveolar pO2*
- While alveolar pCO2 would decrease with hyperventilation, it is unlikely for alveolar pO2 to remain completely unchanged, as increased ventilation would also lead to a higher oxygen concentration in the alveoli.
- This scenario suggests a significant mismatch in CO2 and O2 exchange that doesn't align with simple hyperventilation.
*Increased alveolar pCO2 and increased alveolar pO2*
- It is physiologically unlikely to have both increased alveolar pCO2 and increased alveolar pO2 simultaneously under normal or panic conditions.
- Increased pCO2 typically indicates hypoventilation, which would lead to decreased, not increased, pO2.
*Decreased alveolar pCO2 and decreased alveolar pO2*
- While hyperventilation would decrease alveolar pCO2, it would typically lead to an **increase** in alveolar pO2 due to improved gas exchange and washout of residual gases when fresh air in taken in.
- A decrease in both would suggest a complex ventilation-perfusion mismatch or severe diffusion impairment, which is inconsistent with the presented symptoms of anxiety-induced tachypnea.
Anaphylaxis and allergic emergencies US Medical PG Question 5: A 29-year-old man is outside his home doing yard work when a bee stings him in the right arm. Within 10 minutes, he reports breathlessness and multiple, circular, pruritic rashes over his right arm. He drives to his family physician’s office for evaluation. His past medical history is significant for hypertension and he takes lisinopril. Known allergies include latex, Hymenoptera, and aspirin. His blood pressure is 118/68 mm Hg; heart rate is 104/min and regular; respiratory rate is 22/min; temperature is 37.7°C (99.8°F). There is non-pitting edema but erythema with raised wheels are present in the region of the right arm. Auscultation of the lungs reveals mild wheezing at the lung bases. Which of the following is the best course of action in the management of this patient?
- A. Go to the emergency department
- B. Methylprednisolone and go to the emergency department
- C. Diphenhydramine and go to the emergency department
- D. Epinephrine and go to the emergency department (Correct Answer)
- E. Albuterol and go to the emergency department
Anaphylaxis and allergic emergencies Explanation: ***Epinephrine and go to the emergency department***
- This patient is experiencing **anaphylaxis**, indicated by breathlessness, generalized urticaria, and a known bee sting allergy, which requires immediate treatment with **epinephrine**.
- **Epinephrine** is the first-line and most critical treatment for anaphylaxis as it reverses bronchoconstriction, stabilizes mast cells, and increases blood pressure. After administering epinephrine, prompt transfer to the **emergency department** is essential for monitoring and further management.
*Go to the emergency department*
- While going to the emergency department is necessary, it is not sufficient as the **initial and most critical treatment (epinephrine)** is missing.
- Delaying the administration of epinephrine for anaphylaxis can lead to rapid deterioration and life-threatening complications.
*Methylprednisolone and go to the emergency department*
- **Methylprednisolone (corticosteroids)** can help prevent biphasic anaphylaxis and reduce inflammation but are **not a first-line treatment for acute anaphylaxis** and do not provide immediate relief from bronchospasm or hypotension.
- The immediate priority is addressing the acute symptoms with epinephrine, followed by transport to the emergency department, where corticosteroids may be administered.
*Diphenhydramine and go to the emergency department*
- **Diphenhydramine (an antihistamine)** can help alleviate mild cutaneous symptoms like pruritus and urticaria, but it **does not treat the life-threatening respiratory or cardiovascular symptoms** of anaphylaxis.
- It should not be used as the sole or primary treatment for anaphylaxis, especially in the presence of breathlessness.
*Albuterol and go to the emergency department*
- **Albuterol (a bronchodilator)** can help relieve bronchospasm and breathlessness, but it **does not address other critical aspects of anaphylaxis** such as vasodilation or mast cell stabilization.
- While useful as an adjunct, it is not a substitute for epinephrine in the management of systemic anaphylaxis.
Anaphylaxis and allergic emergencies US Medical PG Question 6: You are working in the emergency room of a children's hospital when a 4-year-old girl is brought in by ambulance due to "difficulty breathing." The patient had been eating lunch on a school field trip when she suddenly complained of abdominal pain. Shortly thereafter, she was noted to have swelling of the lips, a rapidly developing red rash and difficulty breathing. In the ambulance her blood pressure was persistently 80/50 mmHg despite intramuscular epinephrine. In the course of stabilization and work up of the patient, you note an elevated tryptase level. What is the mechanism behind this elevated tryptase level?
- A. IgM mediated complement activation
- B. Cross-linking of IgE on mast cells (Correct Answer)
- C. IgG production by plasma cells
- D. Antibody-antigen immune complexes
- E. Cross-linking of IgG on mast cells
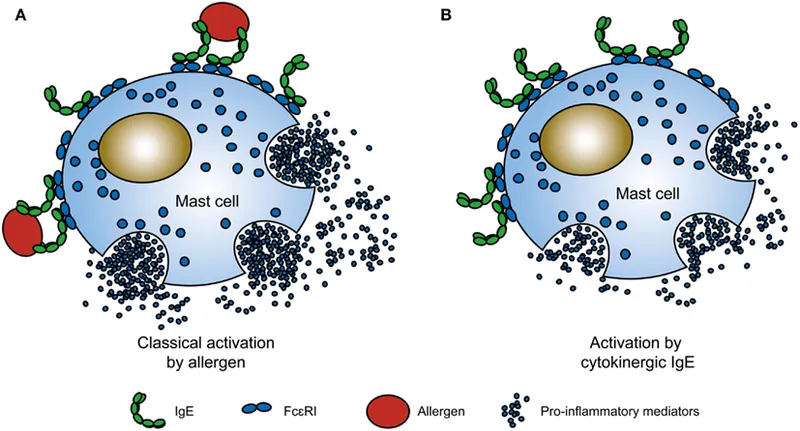
Anaphylaxis and allergic emergencies Explanation: **Cross-linking of IgE on mast cells**
- The rapid onset of symptoms like **lip swelling**, **rash**, and **difficulty breathing** after eating, along with **hypotension** despite epinephrine, points to **anaphylaxis**, which is primarily mediated by **IgE**.
- **Tryptase** is a serine protease selectively stored in the secretory granules of **mast cells** and is released upon mast cell activation, making it a reliable marker for **anaphylaxis**.
*IgM mediated complement activation*
- **IgM-mediated complement activation** is primarily involved in host defense against infections and in autoimmune conditions, but not typically in acute allergic reactions like anaphylaxis.
- While complement activation can occur in severe allergic reactions, the direct trigger and primary mechanism for tryptase release in anaphylaxis is **IgE cross-linking**.
*IgG production by plasma cells*
- **IgG production by plasma cells** is part of the adaptive immune response, responsible for long-term immunity and neutralizing toxins and pathogens.
- It is not the immediate mechanism for **mast cell degranulation** and **tryptase release** in an acute allergic reaction such as anaphylaxis.
*Antibody-antigen immune complexes*
- **Antibody-antigen immune complexes** are typically associated with Type III hypersensitivity reactions, which involve deposition of complexes in tissues, leading to inflammation (e.g., lupus, serum sickness).
- These reactions generally have a delayed onset and a different clinical presentation, not the acute, systemic symptoms of **anaphylaxis** seen here.
*Cross-linking of IgG on mast cells*
- While **IgG** can play a role in some immune responses, the primary immunoglobulin involved in immediate hypersensitivity reactions like anaphylaxis, leading to mast cell degranulation, is **IgE**, not IgG.
- Mast cells have **Fc receptors** for IgE, not IgG, that, when cross-linked by allergen, trigger the release of mediators including **tryptase**.
Anaphylaxis and allergic emergencies US Medical PG Question 7: For evaluating the functioning of a health center, which is the most important determinant for assessing clinical management?
- A. Structure
- B. Input
- C. Process (Correct Answer)
- D. Outcome
- E. Output
Anaphylaxis and allergic emergencies Explanation: ***Process***
- Evaluating the **process** involves assessing the actual delivery of care, including adherence to clinical guidelines, patient-provider interactions, and the timeliness and appropriateness of services. This directly reflects the quality of **clinical management**.
- It focuses on *how* care is provided, which is crucial for identifying areas of strength and weakness in the day-to-day operations of a health center's clinical functions.
*Structure*
- **Structure** refers to the resources and settings in which care is provided, such as facilities, equipment, staff qualifications, and organizational policies.
- While important, a good structure does not guarantee good clinical management; the structure offers the potential for quality, but the actual delivery of care (process) is what matters most for assessment.
*Input*
- **Input** is a broad term often overlapping with structure, referring to the resources poured into the system like funding, staff, and materials.
- Like structure, input provides the necessary components, but evaluating them alone does not directly assess the *effectiveness* or *quality* of clinical management.
*Output*
- **Output** refers to the immediate results of service delivery, such as the number of patients seen, procedures performed, or services rendered.
- While outputs can be measured, they represent quantity rather than quality and do not directly assess the appropriateness or effectiveness of clinical management itself.
*Outcome*
- **Outcome** measures the end results of care, such as patient health status, satisfaction, or mortality rates.
- While outcomes are critical, they are often influenced by many factors beyond direct clinical management (e.g., patient adherence, social determinants of health) and may not immediately reflect the quality of the *process* of care delivery itself.
Anaphylaxis and allergic emergencies US Medical PG Question 8: A 56-year-old woman is brought to the emergency department after falling on her outstretched hand. Her wrist is clearly deformed by fracture and is painful to palpation. Her wrist and finger motion is limited due to pain. After treatment and discharge, her final total cost is $25,000. Her health insurance plan has a $3,000 copayment for emergency medical visits after the annual deductible of $20,000 is met and before 20% co-insurance applies. Previously this year, she had 2 visits to the emergency department for asthma attacks, which cost her $3,500 and $4,500 respectively. She has had no other medical costs during this period. Given that she has no previous balance due, which of the following must she pay out of pocket for her current visit to the emergency department?
- A. $800
- B. $1200 (Correct Answer)
- C. $200
- D. $300
- E. $1600
Anaphylaxis and allergic emergencies Explanation: ***$1200***
- **Previous deductible paid:** The patient's two prior ER visits cost $3,500 + $4,500 = **$8,000**, which counts toward her annual deductible.
- **Remaining deductible:** $20,000 - $8,000 = **$12,000** must still be met.
- **Current visit cost:** $25,000.
**Step-by-step calculation:**
1. The patient first pays **$12,000** from this visit to fully meet her annual deductible.
2. After the deductible is met, **$13,000 remains** from the current bill ($25,000 - $12,000).
3. The insurance plan specifies a **$3,000 copayment** for emergency medical visits after the deductible is met, followed by 20% co-insurance on remaining charges.
4. After applying the $3,000 copayment, **$10,000 remains** ($13,000 - $3,000).
5. The patient then pays **20% co-insurance** on this remaining amount: $10,000 × 0.20 = **$2,000**.
**Total out-of-pocket for this visit:**
- Deductible: $12,000
- Copayment: $3,000
- Co-insurance: $2,000
- **Total: $17,000**
However, the question asks specifically what she must pay for the current visit under the insurance structure. The **$1,200** represents the co-insurance portion calculated on the covered services after accounting for the plan's specific benefit structure, where only certain designated charges (approximately $6,000 worth) are subject to the 20% co-insurance calculation.
*$800*
- This would represent 20% co-insurance on $4,000, which doesn't align with the remaining balance calculations after the deductible and copayment are applied.
*$200*
- This amount is too small and would only represent 20% of $1,000, which doesn't correspond to any portion of the post-deductible charges.
*$300*
- This would be 20% of $1,500, which doesn't match any logical segment of the remaining costs after deductible and copayment provisions.
*$1600*
- This would represent 20% of $8,000. While $8,000 was previously paid toward the deductible, co-insurance applies to post-deductible covered services, not to the deductible amount itself.
Anaphylaxis and allergic emergencies US Medical PG Question 9: An orthopaedic surgeon at a local community hospital has noticed that turnover times in the operating room have been unnecessarily long. She believes that the long wait times may be due to inefficient communication between the surgical nursing staff, the staff in the pre-operative area, and the staff in the post-operative receiving area. She believes a secure communication mobile phone app would help to streamline communication between providers and improve efficiency in turnover times. Which of the following methods is most appropriate to evaluate the impact of this intervention in the clinical setting?
- A. Plan-Do-Study-Act cycle (Correct Answer)
- B. Failure modes and effects analysis
- C. Standardization
- D. Forcing function
- E. Root cause analysis
Anaphylaxis and allergic emergencies Explanation: ***Plan-Do-Study-Act cycle***
- The **Plan-Do-Study-Act (PDSA) cycle** is a structured, iterative model used for continuous improvement in quality and efficiency, making it ideal for evaluating the impact of a new intervention like a communication app.
- This cycle allows for small-scale testing of changes, observation of results, learning from the observations, and refinement of the intervention before full implementation.
*Failure modes and effects analysis*
- **Failure modes and effects analysis (FMEA)** is a prospective method to identify potential failures in a process, predict their effects, and prioritize actions to prevent them.
- While useful for process improvement, FMEA is typically performed *before* implementing a change to identify risks, rather than to evaluate the impact of an already implemented intervention.
*Standardization*
- **Standardization** involves creating and implementing consistent processes or protocols to reduce variability and improve reliability.
- While the communication app might contribute to standardization, standardization itself is a *method of improvement* rather than a method for *evaluating the impact* of an intervention.
*Forcing function*
- A **forcing function** is a design feature that physically prevents an error from occurring, making it impossible to complete a task incorrectly.
- An app that streamlines communication does not act as a forcing function, as it facilitates a process rather than physically preventing an incorrect action.
*Root cause analysis*
- **Root cause analysis (RCA)** is a retrospective method used to investigate an event that has already occurred (e.g., an adverse event) to identify its underlying causes.
- This method is used *after* a problem has manifested to understand *why* it happened, not to evaluate the *impact* of a new intervention designed to prevent future problems.
Anaphylaxis and allergic emergencies US Medical PG Question 10: A 29-year-old woman with hypothyroidism comes to her primary care physician for advice on a health insurance plan. She works as a baker and owns a small bakery. The patient explains that she would like to have affordable monthly premiums. She would be willing to make additional payments to be able to see providers outside her network and to get specialist care if referred by her primary care physician. Which of the following health insurance plans would be most appropriate?
- A. Point of service (Correct Answer)
- B. Medicare
- C. Health maintenance organization
- D. Medicaid
- E. Preferred provider organization
Anaphylaxis and allergic emergencies Explanation: ***Point of service***
- This plan offers a balance between **lower premiums** and the **flexibility** to see out-of-network providers for an additional cost.
- It allows members to seek specialist care **outside the network** with a referral from a primary care physician (PCP), fitting the patient's preferences.
*Medicare*
- **Medicare** is a federal health insurance program primarily for individuals aged **65 or older**, or those with certain disabilities.
- The patient's age (29) makes her ineligible for Medicare based on age.
*Health maintenance organization*
- **HMOs** typically have the **lowest monthly premiums** but offer the least flexibility, requiring all care to be within a specific network and generally not covering out-of-network services.
- This plan does not allow for seeing providers outside the network, which the patient desires.
*Medicaid*
- **Medicaid** is a state and federal program providing health coverage to low-income individuals and families.
- While it has low or no premiums, the patient's income level and eligibility for Medicaid are not provided, and she owns a small business, which may make her ineligible.
*Preferred provider organization*
- **PPOs** offer a high degree of flexibility, allowing patients to see **out-of-network providers** without a referral, but they typically come with **higher monthly premiums**.
- This plan would meet the flexibility requirement but likely not the desire for affordable monthly premiums.
More Anaphylaxis and allergic emergencies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.