Acute pain management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute pain management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute pain management US Medical PG Question 1: A 50-year-old male is brought to the dermatologist's office with complaints of a pigmented lesion. The lesion is uniformly dark with clean borders and no asymmetry and has been increasing in size over the past two weeks. He works in construction and spends large portions of his day outside. The dermatologist believes that this mole should be biopsied. To prepare the patient for the biopsy, the dermatologist injects a small amount of lidocaine into the skin around the lesion. Which of the following nerve functions would be the last to be blocked by the lidocaine?
- A. Pain
- B. Touch
- C. Temperature
- D. Sympathetic stimulation
- E. Pressure (Correct Answer)
Acute pain management Explanation: ***Pressure***
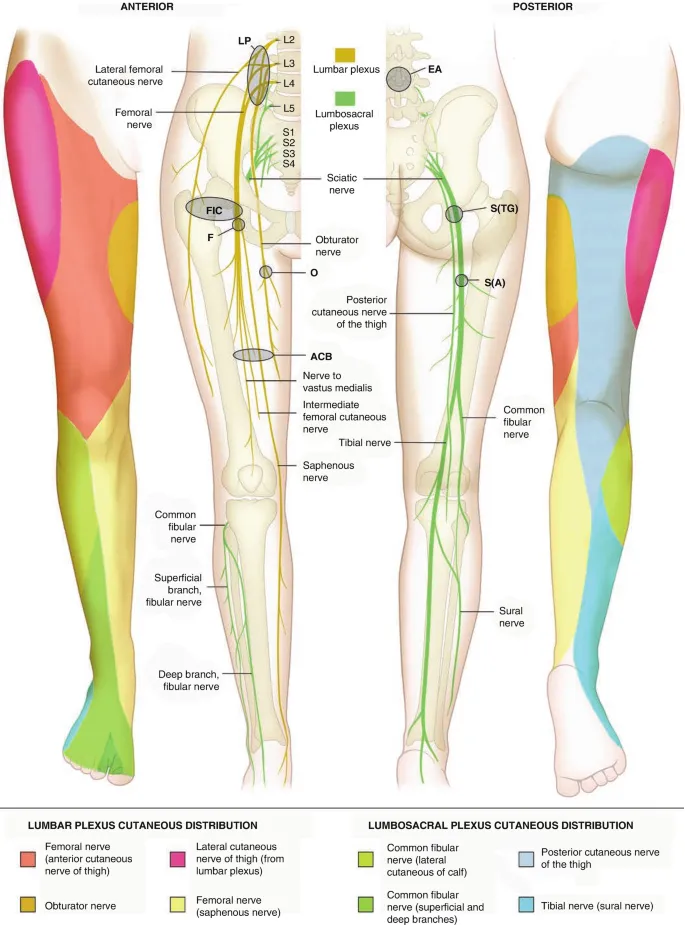
- **Pressure** sensation is mediated by **Aβ fibers**, which are relatively **larger** and **myelinated**, making them more resistant to local anesthetic blockade.
- Nerve fibers are blocked in a specific order, typically starting with smaller, unmyelinated fibers and ending with larger, myelinated fibers.
*Pain*
- **Pain** sensation is primarily carried by **unmyelinated C fibers** and **small myelinated Aδ fibers**, which are among the **first to be blocked** by local anesthetics.
- These fibers have a **high surface-to-volume ratio**, making them more susceptible to the action of lidocaine.
*Touch*
- **Touch** sensation is mediated by a mix of **Aβ and Aδ fibers**; light touch is typically blocked relatively early due to the involvement of smaller fibers.
- However, **crude touch** often persists longer than pain and temperature but is usually blocked before pressure.
*Temperature*
- **Temperature** sensation is primarily carried by **Aδ and C fibers**, making it one of the **earliest sensations to be blocked** by local anesthetic.
- These fibers are generally small and have high sensitivity to local anesthetic agents.
*Sympathetic stimulation*
- **Sympathetic nerve fibers** are typically **small, unmyelinated C fibers** and are generally the **first to be blocked** by local anesthetics.
- This early blockade can lead to **vasodilation** in the area due to the loss of sympathetic tone.
Acute pain management US Medical PG Question 2: A 14-year-old boy is brought to the emergency department because of a 4-hour history of vomiting, lethargy, and confusion. Three days ago, he was treated with an over-the-counter medication for fever and runny nose. He is oriented only to person. His blood pressure is 100/70 mm Hg. Examination shows bilateral optic disc swelling and hepatomegaly. His blood glucose concentration is 65 mg/dL. Toxicology screening for serum acetaminophen is negative. The over-the-counter medication that was most likely used by this patient has which of the following additional effects?
- A. Increased partial thromboplastin time
- B. Decreased uric acid elimination
- C. Decreased expression of glycoprotein IIb/IIIa
- D. Irreversible inhibition of ATP synthase
- E. Irreversible inhibition of cyclooxygenase-1 (Correct Answer)
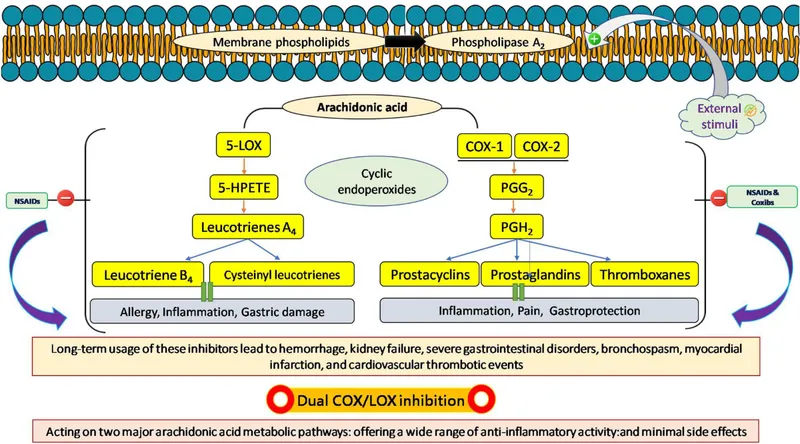
Acute pain management Explanation: ***Irreversible inhibition of cyclooxygenase-1***
- The patient's presentation is classic for **Reye syndrome** (vomiting, lethargy, confusion, cerebral edema with optic disc swelling, hepatomegaly, hypoglycemia) following recent viral illness treated with OTC medication
- **Aspirin** is strongly associated with Reye syndrome in children with viral infections and should be avoided in this population
- The "additional effect" of aspirin is its mechanism of action: **irreversible acetylation and inhibition of COX-1 and COX-2**
- This irreversible COX inhibition also explains aspirin's antiplatelet effects (via inhibition of thromboxane A2 synthesis) and anti-inflammatory properties
*Increased partial thromboplastin time*
- PTT measures the intrinsic and common coagulation pathways and is prolonged by **heparin** or clotting factor deficiencies
- Aspirin affects **platelet function** (prolonging bleeding time), not the coagulation cascade measured by PTT
- While Reye syndrome can cause coagulopathy from liver dysfunction, increased PTT is not a direct pharmacologic effect of aspirin
*Decreased uric acid elimination*
- **Low-dose aspirin** (<2 g/day) can decrease renal uric acid excretion and may precipitate gout
- While this is true, it is not the primary or most clinically relevant "additional effect" in this context
- High-dose aspirin actually increases uric acid excretion (uricosuric effect)
*Decreased expression of glycoprotein IIb/IIIa*
- This is the mechanism of **GP IIb/IIIa inhibitors** (abciximab, eptifibatide, tirofiban), not aspirin
- Aspirin inhibits platelet aggregation by preventing thromboxane A2 synthesis, not by affecting GP IIb/IIIa expression
- These are IV antiplatelet agents used in acute coronary syndromes, not OTC medications
*Irreversible inhibition of ATP synthase*
- This is not a mechanism of aspirin or other common OTC fever/cold medications
- While Reye syndrome involves mitochondrial dysfunction, aspirin does not directly inhibit ATP synthase
- The mitochondrial injury in Reye syndrome is likely multifactorial
Acute pain management US Medical PG Question 3: A 72-year-old woman with metastatic ovarian cancer is brought to the physician by her son because she is in immense pain and cries all the time. On a 10-point scale, she rates the pain as an 8 to 9. One week ago, a decision to shift to palliative care was made after she failed to respond to 2 years of multiple chemotherapy regimens. She is now off chemotherapy drugs and has been in hospice care. Current medications include 2 mg morphine intravenously every 2 hours and 650 mg of acetaminophen every 4 to 6 hours. The son is concerned because he read online that increasing the dose of morphine would endanger her breathing. Which of the following is the most appropriate next step in management?
- A. Counsel patient and continue same opioid dose
- B. Increase dosage of morphine (Correct Answer)
- C. Change morphine to a non-opioid analgesic
- D. Initiate palliative radiotherapy
- E. Initiate cognitive behavioral therapy
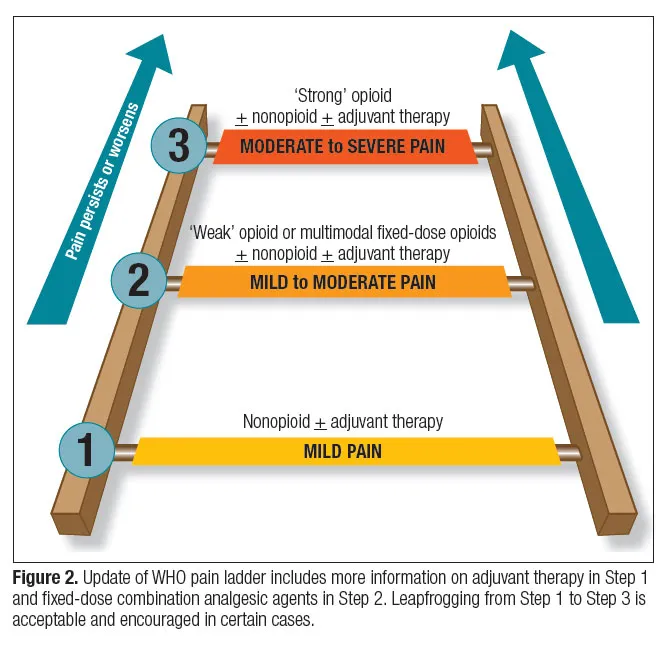
Acute pain management Explanation: ***Increase dosage of morphine***
- The patient is experiencing severe, **uncontrolled pain** (8-9/10), indicating her current morphine dose is inadequate. In palliative care, the goal is to provide maximum comfort, and **opioid dose escalation** is appropriate to achieve this.
- While respiratory depression is a concern with opioids, in patients with chronic pain who are already on opioids, **tolerance to respiratory depressant effects** develops more quickly than tolerance to analgesic effects. Careful titration and monitoring can safely increase pain relief.
*Counsel patient and continue same opioid dose*
- The patient's pain is severe and unmanaged, so simply counseling her without addressing the **inadequate analgesia** would be inappropriate and unethical.
- Continuing the same dose would perpetuate her suffering, as the current regimen is clearly **insufficient for pain control**.
*Change morphine to a non-opioid analgesic*
- For severe cancer pain (8-9/10), **non-opioid analgesics** alone are typically ineffective.
- Switching to a non-opioid would likely lead to even poorer pain control and increased suffering, as opioids are the **cornerstone of severe cancer pain management**.
*Initiate palliative radiotherapy*
- While **radiotherapy** can be effective for localized pain caused by bone metastases, its onset of action is not immediate, and the primary issue here is urgent, **uncontrolled systemic pain**.
- It is not an appropriate initial step for immediate pain relief in a patient already in hospice with widespread metastatic disease and severe current pain.
*Initiate cognitive behavioral therapy*
- **Cognitive behavioral therapy (CBT)** can be a useful adjunct in chronic pain management to help with coping strategies and psychological distress.
- However, it does not directly address the severe, acute physical pain the patient is experiencing and is not a substitute for **pharmacological pain control** in this context.
Acute pain management US Medical PG Question 4: A 68-year-old man presents to his primary care physician with pain that started after he visited his daughter as she moved into her new apartment. The patient states that the pain is likely related to all the traveling he has done and helping his daughter move and set up furniture. The patient has a past medical history of obesity, type II diabetes, multiple concussions while he served in the army, and GERD. He is currently taking metformin, lisinopril, omeprazole, and a multivitamin. On physical exam, pain is elicited upon palpation of the patient's lower back. Flexion of the patient's leg results in pain that travels down the patient's lower extremity. The patient's cardiac, pulmonary, and abdominal exam are within normal limits. Rectal exam reveals normal rectal tone. The patient denies any difficulty caring for himself, defecating, or urinating. Which of the following is the best next step in management?
- A. NSAIDS and activity as tolerated (Correct Answer)
- B. MRI of the spine
- C. Oxycodone and bed rest
- D. Oxycodone and activity as tolerated
- E. NSAIDS and bed rest
Acute pain management Explanation: ***NSAIDS and activity as tolerated***
- The patient presents with classic symptoms of **acute low back pain** with **radicular symptoms** (pain radiating down the leg) following exertion, but without any **red flag symptoms** such as **fever**, **weight loss**, **neurological deficits**, or **cauda equina syndrome**.
- Initial management for uncomplicated acute low back pain, including those with radiculopathy, typically involves **NSAIDs or acetaminophen** for pain relief and **maintaining activity as tolerated** to prevent deconditioning and chronicity.
*MRI of the spine*
- An MRI is generally not indicated as the **initial step** for acute, uncomplicated lower back pain unless **red flag symptoms** or a suspicion of **serious underlying pathology** (e.g., cauda equina syndrome, epidural abscess, malignancy) are present.
- Doing an MRI too early in these cases can lead to identifying incidental findings, thus causing **unnecessary investigations** and interventions.
*Oxycodone and bed rest*
- **Oxycodone** (an opioid) is generally reserved for **severe pain** unresponsive to first-line agents and carries risks of **dependence** and **side effects**; it is not a first-line therapy for this presentation given the lack of severe red flags.
- **Bed rest** is **contraindicated** for most cases of acute low back pain as it can worsen symptoms and lead to deconditioning; **activity as tolerated** is preferred.
*Oxycodone and activity as tolerated*
- While **activity as tolerated** is beneficial, the use of **oxycodone** as a primary treatment for initial, uncomplicated low back pain is generally **inappropriate** due to the risks associated with opioid use.
- The patient's symptoms do not suggest a need for strong opioid analgesia at this stage.
*NSAIDS and bed rest*
- **NSAIDs** are an appropriate initial analgesic, but **bed rest** is **not recommended** for acute low back pain.
- Promoting activity helps to prevent stiffness, muscle weakness, and chronicity of pain.
Acute pain management US Medical PG Question 5: A 49-year-old man being treated for Helicobacter pylori infection presents to his primary care physician complaining of lower back pain. His physician determines that a non-steroidal anti-inflammatory drug (NSAID) would be the most appropriate initial treatment. Which of the following is the most appropriate NSAID for this patient?
- A. Aspirin
- B. Ibuprofen
- C. Celecoxib (Correct Answer)
- D. Naproxen
- E. Diclofenac
Acute pain management Explanation: **Celecoxib**
- This patient is being treated for a *Helicobacter pylori* infection, indicating a potential risk for **gastrointestinal complications** like ulcers. **Celecoxib** is a selective **COX-2 inhibitor**, which has a lower risk of causing GI side effects compared to non-selective NSAIDs.
- Its selective inhibition of COX-2 helps reduce pain and inflammation while largely sparing the **COX-1 enzyme**, which is responsible for maintaining the **gastric mucosal lining**.
*Aspirin*
- **Aspirin** is a non-selective NSAID that inhibits both **COX-1** and **COX-2** enzymes.
- Inhibition of COX-1 can lead to a significant increase in the risk of **gastrointestinal bleeding** and **ulcer formation**, which is particularly concerning for a patient with an *H. pylori* infection.
*Ibuprofen*
- **Ibuprofen** is a non-selective NSAID that can cause **gastrointestinal irritation** and damage by inhibiting **COX-1**.
- Its use would increase the risk of worsening the patient's existing **gastrointestinal vulnerability** due to the *H. pylori* infection.
*Naproxen*
- **Naproxen** is another non-selective NSAID with a relatively long half-life, making its **gastrointestinal side effects** potentially more prolonged and severe than some other non-selective NSAIDs.
- It carries a **higher risk for GI bleeding** and ulcers compared to selective COX-2 inhibitors, especially in patients with pre-existing GI issues.
*Diclofenac*
- **Diclofenac** is a non-selective NSAID that carries a risk of **gastrointestinal adverse events**, although some studies suggest it might have a slightly better GI safety profile than other non-selective NSAIDs at lower doses.
- However, in a patient with *H. pylori*, it still poses a significant risk for **ulcers** and bleeding compared to a COX-2 selective inhibitor.
Acute pain management US Medical PG Question 6: Scientists are developing a new non-steroidal anti-inflammatory drug for osteoarthritis. Their hope is that the new drug will have a higher potency but the same efficacy as ibuprofen in the hope of minimizing gastrointestinal side effects. If ibuprofen is curve C in the figure provided, which of the following would be the curve for the new drug based on the scientists’ specifications? The desired therapeutic effect in patients is represented by the dashed line Y.
- A. Curve B
- B. Curve D
- C. Curve C
- D. Curve E
- E. Curve A (Correct Answer)
Acute pain management Explanation: ***Curve A***
- A drug with **higher potency** will achieve its maximal effect at a lower concentration, shifting the curve to the **left** (from C to A).
- **Same efficacy** means the drug reaches the **same maximal effect** (height on the y-axis) as ibuprofen (curve C), which curve A does.
*Curve B*
- This curve represents a drug with **lower potency** than ibuprofen, as it requires a higher concentration to achieve its maximal effect, shifting the curve to the right.
- While it has the same efficacy, it does not meet the requirement of higher potency.
*Curve D*
- Curve D shows a drug with **higher potency** (shifted left) but **lower efficacy** (lower maximal effect) compared to ibuprofen.
- The scientists are looking for the same efficacy, not lower efficacy.
*Curve E*
- Curve E represents a drug with **lower efficacy** (lower maximal effect) than ibuprofen.
- It also appears to have lower potency as the curve is shifted to the right, failing both criteria.
*Curve C*
- This curve is ibuprofen itself, meaning there is no change in potency or efficacy.
- The new drug needs to have higher potency while maintaining the same efficacy as ibuprofen.
Acute pain management US Medical PG Question 7: 29-year-old construction worker is brought to the emergency department after falling 10 ft (3 m) from the scaffolding at a construction site. He reports that he landed on his outstretched arms, which are now in severe pain (10/10 on a numeric scale). He has a history of opioid use disorder and is currently on methadone maintenance treatment. His pulse is 100/min, respirations are 20/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. He is diaphoretic and in distress. Physical examination shows a hematoma on the patient's right forearm. X-ray of the right arm shows a nondisplaced fracture of the ulna. A CT of the abdomen and pelvis shows no abnormalities. The patient requests pain medication. In addition to managing the patient's injury, which of the following is the most appropriate next step in management?
- A. Administration of buprenorphine
- B. Psychiatric evaluation for drug-seeking behavior
- C. Increase of outpatient methadone regimen
- D. Urine toxicology screening
- E. Scheduled short-acting opioid administration (Correct Answer)
Acute pain management Explanation: ***Scheduled short-acting opioid administration***
- This patient is experiencing significant pain (10/10) from a verified injury (ulna fracture) and has a known history of **opioid use disorder** managed with methadone.
- Providing **scheduled short-acting opioids** is appropriate for acute pain management in this context, addressing both the severe pain and the risk of withdrawal/escalated pain due to his opioid tolerance.
*Administration of buprenorphine*
- Administering buprenorphine in a patient currently on methadone for **opioid use disorder** could precipitate **acute opioid withdrawal** due to buprenorphine's partial agonist and high affinity properties.
- Buprenorphine is typically used for **opioid dependence treatment** rather than acute pain management in someone currently maintained on methadone.
*Psychiatric evaluation for drug-seeking behavior*
- Attributing the patient's request for pain medication solely to "drug-seeking behavior" while he has a confirmed painful injury is **unethical and inappropriate**.
- All patients, regardless of their substance use history, deserve adequate pain management for acute injuries.
*Increase of outpatient methadone regimen*
- Adjusting a stable outpatient methadone regimen for **acute pain management** is complex and typically requires coordination with the patient's opioid treatment program (OTP).
- An isolated increase in methadone might not adequately address acute, incident pain from a fracture and could complicate subsequent long-term management.
*Urine toxicology screening*
- While a urine toxicology screen might be part of a comprehensive assessment in some contexts, it is **not the most appropriate immediate next step** for a patient presenting with severe acute pain from a confirmed injury.
- The patient's pain needs immediate attention, and awaiting toxicology results would delay necessary pain relief.
Acute pain management US Medical PG Question 8: A 36-year-old man is admitted to the hospital for treatment of burn wounds on his upper extremities. Analgesic therapy with an opioid drug is begun. Shortly after, the patient develops chills, diaphoresis, nausea, and abdominal pain. On further questioning, the patient reports that he has been smoking opium at home to help him ""deal with the depression and pain.” This patient was most likely given which of the following opioid drugs?
- A. Butorphanol (Correct Answer)
- B. Oxycodone
- C. Morphine
- D. Fentanyl
- E. Hydrocodone
Acute pain management Explanation: ***Butorphanol***
- **Butorphanol** is a **mixed opioid agonist-antagonist** that acts as a **kappa (κ) receptor agonist** and **mu (μ) receptor antagonist/partial agonist**.
- In opioid-dependent patients who use **mu receptor agonists** (like opium), butorphanol can precipitate **acute opioid withdrawal** by displacing full agonists from mu receptors and blocking their effects.
- The patient's symptoms of chills, diaphoresis, nausea, and abdominal pain are classic signs of **acute opioid withdrawal syndrome**.
*Oxycodone*
- **Oxycodone** is a **full mu opioid receptor agonist** and would not precipitate withdrawal in an opioid-dependent patient.
- Administering oxycodone would provide continued mu receptor stimulation, potentially alleviating withdrawal symptoms or maintaining the patient's opioid dependence.
*Morphine*
- **Morphine** is a **full mu opioid receptor agonist** and would not cause withdrawal in an opioid-dependent individual.
- It would continue to stimulate mu opioid receptors, providing analgesia and preventing withdrawal symptoms.
*Fentanyl*
- **Fentanyl** is a potent **full mu opioid receptor agonist** and would provide continued opioid receptor stimulation.
- Its administration would prevent withdrawal and provide effective analgesia in an opioid-tolerant patient.
*Hydrocodone*
- **Hydrocodone** is a **full mu opioid receptor agonist** and would not induce withdrawal symptoms.
- Like other full agonists, it would continue mu receptor activation, providing analgesia without precipitating withdrawal.
Acute pain management US Medical PG Question 9: A 45-year-old homeless man presents to the emergency department with a 1-week history of an intensely pruritic, red rash on his hands, wrists, and finger webs. The itching is worse at night. Physical examination reveals small, erythematous papules and burrows. A topical drug with which of the following mechanisms of action is most likely to be effective in treating this condition?
- A. Increase in keratinocyte turnover
- B. Inhibition of histamine-1 receptors
- C. Decrease in peptidoglycan synthesis
- D. Inhibition of nuclear factor-κB
- E. Binding to sodium channels (Correct Answer)
Acute pain management Explanation: ***Binding to sodium channels***
- The clinical presentation of **intensely pruritic rash**, especially worse at night, with **burrows** on hands, wrists, and finger webs, is highly suggestive of **scabies**.
- Scabies is caused by the mite *Sarcoptes scabiei*, and treatment often involves **permethrin**, which acts by **binding to sodium channels** in the mite's nervous system, leading to paralysis and death.
*Increase in keratinocyte turnover*
- This mechanism of action is characteristic of drugs used to treat conditions like **psoriasis**, where the goal is to reduce rapid skin cell proliferation.
- It is not relevant for parasitic infestations like scabies, which require an agent to directly kill the mites.
*Inhibition of histamine-1 receptors*
- Antihistamines, which block H1 receptors, are used to alleviate **pruritus** associated with allergic reactions or other inflammatory skin conditions.
- While they can help with the *symptom* of itching, they do not address the underlying *cause* of scabies (the mite infestation itself).
*Decrease in peptidoglycan synthesis*
- This mechanism is characteristic of **antibiotics** like **penicillins** and **cephalosporins**, which target the bacterial cell wall.
- It is effective against bacterial infections but has no utility in treating parasitic infestations like scabies, which are caused by arthropods, not bacteria.
*Inhibition of nuclear factor-κB*
- **NF-κB** is a protein complex that controls **transcription of DNA**, cytokine production, and cell survival, and its inhibition is often targeted in **inflammatory diseases** or cancers.
- This mechanism is not directly involved in the eradication of scabies mites.
Acute pain management US Medical PG Question 10: A 69-year-old man presents to his primary care physician for pain when he walks. He states that the pain is the worst in his left great toe but is also present in his hips and knees. He says that his symptoms are worse with activity and tend to improve with rest. His symptoms have progressively worsened over the past several years. He has a past medical history of obesity, type II diabetes mellitus, smoking, and hypertension. He drinks roughly ten beers per day. His current medications include metformin, insulin, lisinopril, and hydrochlorothiazide. The patient has a recent travel history to Bangkok where he admits to having unprotected sex. On physical exam, examination of the lower extremity results in pain. There is crepitus of the patient's hip when his thigh is flexed and extended. Which of the following is the most likely diagnosis?
- A. Pseudogout
- B. Gout
- C. Rheumatoid arthritis
- D. Infectious arthritis
- E. Osteoarthritis (Correct Answer)
Acute pain management Explanation: ***Osteoarthritis***
- The patient presents with classic features of **osteoarthritis (OA)**: **progressive worsening over several years**, pain that is **worse with activity and improves with rest** (mechanical pain pattern), and **crepitus of the hip** on examination.
- **Crepitus** is a hallmark physical finding in OA, indicating cartilage degradation and bone-on-bone contact.
- The patient has major risk factors including **age (69 years)**, **obesity**, and involvement of **weight-bearing joints** (hips and knees).
- While the great toe is also affected, polyarticular OA commonly involves multiple joints including the first metatarsophalangeal joint.
*Gout*
- Although the patient has risk factors for gout (**alcohol consumption** and **thiazide diuretic use**), gout typically presents with **acute, severe attacks** of monoarticular arthritis, not chronic progressive pain over several years.
- Acute gout would present with sudden onset of severe pain, erythema, warmth, and swelling, which are not described in this case.
- The **mechanical pain pattern** (worse with activity, better with rest) and **crepitus** are inconsistent with gout.
*Pseudogout*
- Pseudogout (calcium pyrophosphate deposition disease) typically causes **acute attacks** affecting larger joints like the knees, similar to gout.
- The **chronic progressive nature** of this patient's symptoms over several years, along with crepitus, is not consistent with pseudogout.
- Pseudogout does not explain the mechanical pain pattern or the hip crepitus.
*Infectious arthritis*
- While the patient's recent travel and unprotected sex raise concern for sexually transmitted infections, **septic arthritis** would present with **acute onset**, severe pain, fever, warmth, erythema, and systemic signs of infection.
- The **chronic progressive course over several years** is completely inconsistent with infectious arthritis.
- Gonococcal arthritis can cause migratory polyarthritis but would be acute, not chronic.
*Rheumatoid arthritis*
- Rheumatoid arthritis typically presents with **symmetric polyarthritis** affecting small joints of the hands and feet, with **prolonged morning stiffness** (>30-60 minutes).
- The pain pattern in RA is **inflammatory** (worse with rest, improves with activity), which is the **opposite** of this patient's presentation.
- **Crepitus** and mechanical pain pattern point to a degenerative process (OA), not an inflammatory arthropathy like RA.
More Acute pain management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.