Acute Care

On this page
🚨 Emergency Medicine Fundamentals: The Critical Care Command Center
Acute care is where medicine moves fastest and stakes run highest-you'll learn to recognize life-threatening patterns within seconds, understand how cellular crises cascade into organ failure, and deploy evidence-based interventions that reverse shock, respiratory collapse, and metabolic catastrophe. This lesson builds your command of emergency pathophysiology, sharpens your diagnostic discrimination across multi-system failures, and equips you with treatment algorithms that translate split-second decisions into survival. You'll integrate physiology, pattern recognition, and therapeutic precision into a unified framework for managing patients when every moment counts.

📌 Remember: ABCDE - Airway, Breathing, Circulation, Disability, Exposure - The universal primary survey sequence that guides every acute care encounter
The foundation of acute care excellence rests on understanding that 85% of emergency diagnoses can be made through systematic history and physical examination, while the remaining 15% require targeted diagnostic testing. This principle drives efficient resource utilization and prevents diagnostic anchoring.
- Primary Assessment Categories
- Airway patency (complete vs partial vs absent)
- Breathing adequacy (rate 12-20/min, SpO₂ >94%)
- Respiratory distress signs: accessory muscle use, tripod positioning
- Oxygen delivery methods: nasal cannula (1-6L/min), non-rebreather (10-15L/min)
- Circulatory status (BP, pulse, perfusion)
- Shock index: HR/SBP (normal <0.9, concerning >1.0)
- Capillary refill (normal <2 seconds)
⭐ Clinical Pearl: Shock index >1.3 indicates severe hemorrhage with >30% blood volume loss, requiring immediate massive transfusion protocol activation
| Assessment Component | Normal Range | Mild Concern | Severe Concern | Immediate Action |
|---|---|---|---|---|
| Respiratory Rate | 12-20/min | 21-24/min | >25/min | Ventilatory support |
| Oxygen Saturation | >94% | 90-94% | <90% | High-flow oxygen |
| Systolic BP | 90-140 mmHg | 80-89 mmHg | <80 mmHg | Vasopressor support |
| Heart Rate | 60-100 bpm | 101-120 bpm | >120 bpm | Fluid/blood products |
| Glasgow Coma Scale | 15 | 13-14 | <13 | Airway protection |
Understanding triage principles enables rapid patient prioritization. The Emergency Severity Index (ESI) stratifies patients into 5 levels based on acuity and resource needs, with Level 1 requiring immediate life-saving intervention and Level 5 representing minor complaints requiring minimal resources.
Connect these foundational assessment principles through systematic diagnostic approaches to understand how pattern recognition transforms emergency medicine practice.
🚨 Emergency Medicine Fundamentals: The Critical Care Command Center
🔄 Pathophysiological Cascade Mastery: The Cellular Crisis Response
📌 Remember: SHOCK - Systolic <90, Heart rate >100, Oxygen sat <90, Cool extremities, Kidney dysfunction - Five cardinal signs of inadequate perfusion
The oxygen delivery equation (DO₂ = CO × Hgb × 1.34 × SaO₂) reveals why different shock types require targeted interventions. Normal oxygen delivery averages 1000 mL/min, with critical threshold at 400 mL/min below which cellular dysfunction occurs.
- Shock Classification by Mechanism
- Hypovolemic: decreased preload (CVP <8 mmHg)
- Hemorrhagic: blood loss >20% circulating volume
- Non-hemorrhagic: dehydration, third-spacing
- Cardiogenic: pump failure (EF <40%, CI <2.2 L/min/m²)
- Acute MI, cardiomyopathy, mechanical complications
- Pulmonary edema with PCWP >18 mmHg
- Distributive: vasodilation (SVR <800 dynes·sec/cm⁵)
- Septic: SIRS + infection + organ dysfunction
- Anaphylactic: IgE-mediated massive histamine release
- Neurogenic: spinal cord injury above T6 level
- Hypovolemic: decreased preload (CVP <8 mmHg)
⭐ Clinical Pearl: Lactate >4 mmol/L indicates tissue hypoperfusion regardless of blood pressure, with lactate clearance >10% in 6 hours predicting 75% survival improvement
| Shock Type | CVP | PCWP | Cardiac Index | SVR | Mixed SvO₂ |
|---|---|---|---|---|---|
| Hypovolemic | ↓ (<8) | ↓ (<12) | ↓ (<2.2) | ↑ (>1200) | ↓ (<65%) |
| Cardiogenic | ↑ (>12) | ↑ (>18) | ↓ (<2.2) | ↑ (>1200) | ↓ (<65%) |
| Distributive | ↓ (<8) | ↓ (<12) | ↑ (>4.0) | ↓ (<800) | ↑ (>75%) |
| Obstructive | ↑ (>12) | Variable | ↓ (<2.2) | ↑ (>1200) | ↓ (<65%) |
| Mixed | Variable | Variable | ↓ (<2.2) | Variable | ↓ (<65%) |
💡 Master This: qSOFA score ≥2 (altered mental status, SBP ≤100 mmHg, RR ≥22/min) identifies sepsis patients with 10-fold increased mortality risk, triggering immediate "Sepsis-3" protocols
Understanding these pathophysiological principles through pattern recognition frameworks enables rapid clinical decision-making in complex emergency presentations.
🔄 Pathophysiological Cascade Mastery: The Cellular Crisis Response
🎯 Clinical Pattern Recognition Arsenal: The Diagnostic Decision Matrix
The ABCDE approach provides systematic pattern recognition for any acute presentation, but specific clinical syndromes require targeted recognition frameworks that bypass lengthy differential diagnosis processes.
- Chest Pain Pattern Recognition
- ACS Pattern: substernal pressure, radiation to arm/jaw, diaphoresis
- HEART Score >3: History, ECG, Age, Risk factors, Troponin
- TIMI Risk Score: predicts 30-day cardiac events
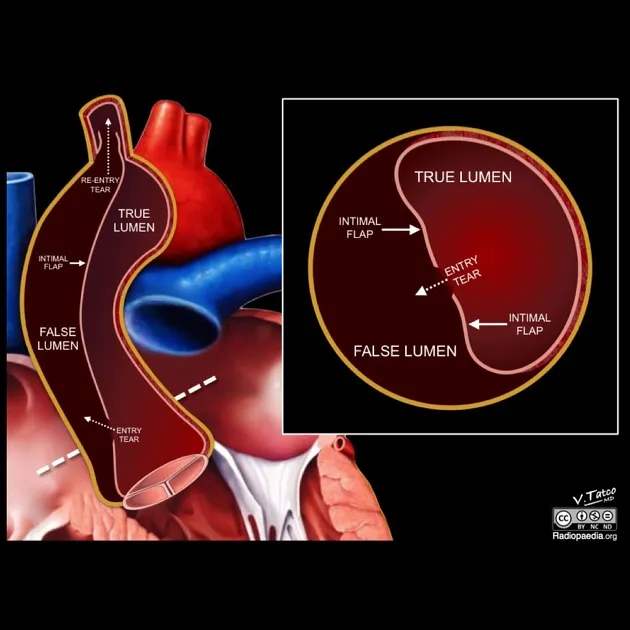
- Aortic Dissection: tearing pain, pulse differential >20 mmHg
- D-dimer >500 ng/mL has 95% sensitivity
- CT angiography gold standard (98% sensitivity)
- Pulmonary Embolism: pleuritic pain, dyspnea, tachycardia
- Wells Score >4: high probability (>40% pre-test)
- PERC Rule: rules out PE if 8 criteria negative
- ACS Pattern: substernal pressure, radiation to arm/jaw, diaphoresis

📌 Remember: MONA - Morphine, Oxygen, Nitroglycerin, Aspirin - Classic ACS treatment (though oxygen only if SpO₂ <90%)
| Clinical Syndrome | Key Pattern | Time-Sensitive Threshold | Diagnostic Test | Treatment Window |
|---|---|---|---|---|
| STEMI | ST elevation >1mm | <90 min door-to-balloon | 12-lead ECG | Primary PCI |
| Stroke | FAST positive | <4.5 hours symptom onset | CT head, CTA | tPA/thrombectomy |
| Sepsis | qSOFA ≥2 | <1 hour recognition | Lactate, cultures | Antibiotics |
| Anaphylaxis | Rapid onset, 2+ systems | <15 minutes | Clinical diagnosis | Epinephrine |
| Aortic Dissection | Tearing pain, pulse deficit | <6 hours | CT angiography | Surgical repair |
The "Rule of 3s" provides rapid assessment frameworks across multiple systems:
- Respiratory: RR >30, SpO₂ <90%, PaO₂ <60 mmHg indicate severe dysfunction
- Cardiovascular: HR >120, SBP <90, MAP <65 mmHg suggest shock
- Neurological: GCS <13, pupils >3mm difference, focal deficits indicate serious pathology
- Dyspnea Pattern Recognition Framework
- Cardiac: orthopnea, PND, bilateral rales, elevated BNP >400 pg/mL
- Framingham criteria: 2 major or 1 major + 2 minor = CHF
- NYHA Class IV: symptoms at rest, EF <30%
- Pulmonary: unilateral findings, pleuritic pain, D-dimer elevation
- COPD exacerbation: pH <7.35, PCO₂ >50 mmHg
- Asthma: PEFR <50% predicted, accessory muscle use
- Mixed: bilateral infiltrates, PaO₂/FiO₂ <300, no cardiac cause
- ARDS criteria: acute onset, bilateral opacities, PCWP <18 mmHg
- Cardiac: orthopnea, PND, bilateral rales, elevated BNP >400 pg/mL
💡 Master This: BNP >400 pg/mL or NT-proBNP >1800 pg/mL indicates heart failure with 95% sensitivity, while levels <100 and <300 respectively rule out acute CHF
Connect these pattern recognition skills through systematic differential diagnosis approaches to understand how clinical reasoning transforms emergency presentations into targeted treatment plans.
🎯 Clinical Pattern Recognition Arsenal: The Diagnostic Decision Matrix
⚖️ Differential Diagnosis Mastery: The Clinical Discrimination Engine
Understanding likelihood ratios transforms clinical findings into diagnostic probability modifiers. A positive likelihood ratio >10 or negative likelihood ratio <0.1 provides strong diagnostic evidence, while ratios between 0.5-2.0 provide minimal diagnostic value.
- Chest Pain Differential Discrimination
- Acute Coronary Syndrome vs Aortic Dissection
- ACS: gradual onset, responds to nitroglycerin, troponin positive
- Dissection: sudden onset, pulse differential >20 mmHg, D-dimer >500
- Pulmonary Embolism vs Pneumonia
- PE: acute dyspnea, Wells Score >4, normal WBC
- Pneumonia: productive cough, fever >38.3°C, infiltrate on CXR
- Pericarditis vs Myocarditis
- Pericarditis: positional pain, friction rub, PR depression
- Myocarditis: CHF symptoms, elevated troponin, wall motion abnormalities
- Acute Coronary Syndrome vs Aortic Dissection
📌 Remember: VINDICATE - Vascular, Infectious, Neoplastic, Degenerative, Intoxication, Congenital, Autoimmune, Traumatic, Endocrine - Systematic differential diagnosis framework
| Diagnostic Feature | ACS | Aortic Dissection | Pulmonary Embolism | Pneumothorax | Pericarditis |
|---|---|---|---|---|---|
| Pain Character | Pressure/squeezing | Tearing/ripping | Pleuritic/sharp | Sharp/stabbing | Sharp/positional |
| Onset | Gradual (minutes) | Sudden (seconds) | Acute (minutes) | Sudden (seconds) | Gradual (hours) |
| Radiation | Arm/jaw/back | Back/abdomen | None | Ipsilateral shoulder | None |
| Physical Findings | Diaphoresis | Pulse deficit | Tachycardia | Decreased breath sounds | Friction rub |
| ECG Changes | ST changes | Usually normal | S1Q3T3 pattern | Usually normal | PR depression |
The Bayesian approach to diagnosis combines pre-test probability with test characteristics to generate post-test probability. Understanding disease prevalence in your patient population prevents over-testing low-probability conditions and under-investigating high-risk presentations.
- Abdominal Pain Discrimination Matrix
- Appendicitis vs Ovarian Pathology (reproductive-age females)
- Appendicitis: Alvarado Score >7, RLQ tenderness, leukocytosis >10,000
- Ovarian torsion: sudden onset, adnexal mass, absent flow on Doppler
- Cholangitis vs Cholecystitis
- Cholangitis: Charcot's triad (fever, jaundice, RUQ pain), bilirubin >4 mg/dL
- Cholecystitis: Murphy's sign, wall thickening >4mm, pericholecystic fluid
- Bowel Obstruction vs Ileus
- Obstruction: cramping pain, high-pitched bowel sounds, air-fluid levels
- Ileus: constant pain, absent bowel sounds, diffuse gas pattern
- Appendicitis vs Ovarian Pathology (reproductive-age females)
💡 Master This: Lactate >4 mmol/L in abdominal pain suggests bowel ischemia, sepsis, or shock - requiring immediate surgical consultation regardless of other findings

Understanding these discrimination principles through evidence-based treatment algorithms enables rapid therapeutic decision-making in complex clinical scenarios.
⚖️ Differential Diagnosis Mastery: The Clinical Discrimination Engine
🚀 Evidence-Based Treatment Algorithms: The Therapeutic Command Protocol
Sepsis-3 protocols demonstrate how systematic treatment algorithms improve survival. The "Hour-1 Bundle" achieves 15-20% mortality reduction through standardized interventions: lactate measurement, blood cultures, broad-spectrum antibiotics, and 30 mL/kg crystalloid resuscitation.
📌 Remember: SEPSIS - Systemic infection, Elevated lactate, Persistent hypotension, Shock index >1, Inadequate perfusion, Source control - Six-point treatment checklist
| Treatment Algorithm | Time Target | Key Interventions | Success Metric | Mortality Benefit |
|---|---|---|---|---|
| Sepsis Hour-1 Bundle | <60 minutes | Cultures, antibiotics, fluids | Lactate clearance >10% | 15-20% reduction |
| STEMI Primary PCI | <90 minutes | Dual antiplatelet, heparin, PCI | TIMI 3 flow | 50% reduction |
| Stroke tPA Protocol | <4.5 hours | CT head, tPA 0.9mg/kg | NIHSS improvement | 30% better outcomes |
| Trauma Resuscitation | <15 minutes | ABCDE, blood products | Hemodynamic stability | 25% reduction |
| Anaphylaxis Treatment | <15 minutes | Epinephrine, H1/H2 blockers | Symptom resolution | 90% response rate |
The massive transfusion protocol (MTP) exemplifies how systematic approaches manage complex resuscitations. Activation criteria include systolic BP <90 mmHg with evidence of ongoing bleeding, triggering 1:1:1 ratio of packed RBCs, fresh frozen plasma, and platelets.
- Advanced Cardiac Life Support (ACLS) Algorithm Mastery
- Ventricular Fibrillation/Pulseless VT
- Immediate defibrillation at 200J (biphasic)
- Epinephrine 1mg IV every 3-5 minutes
- Amiodarone 300mg IV after 3rd shock
- Pulseless Electrical Activity (PEA)
- High-quality CPR with rate 100-120/min
- Epinephrine 1mg IV every 3-5 minutes
- Treat reversible causes: 5 H's and 5 T's
- Asystole Management
- Confirm in 2 leads, high-quality CPR
- Epinephrine 1mg IV every 3-5 minutes
- Consider transcutaneous pacing
- Ventricular Fibrillation/Pulseless VT
💡 Master This: Return of spontaneous circulation (ROSC) occurs in 25% of in-hospital arrests and 10% of out-of-hospital arrests, with neurologically intact survival rates of 15% and 5% respectively
Understanding these evidence-based protocols through multi-system integration approaches reveals how standardized care pathways optimize outcomes across diverse emergency presentations.
🚀 Evidence-Based Treatment Algorithms: The Therapeutic Command Protocol
🌐 Multi-System Integration Nexus: The Physiological Network Architecture
Advanced hemodynamic monitoring reveals the complex interplay between preload, afterload, and contractility. The Frank-Starling mechanism explains how venous return affects cardiac output, while baroreceptor reflexes modulate heart rate and vascular tone in response to pressure changes.
- Cardiovascular-Pulmonary Integration
- Right heart failure → systemic venous congestion → hepatic dysfunction
- CVP >12 mmHg indicates volume overload
- Hepatojugular reflux demonstrates RV dysfunction
- Left heart failure → pulmonary edema → hypoxemia → RV strain
- PCWP >18 mmHg causes pulmonary capillary leak
- PaO₂/FiO₂ <200 indicates ARDS development
- Pulmonary embolism → RV dysfunction → decreased LV filling
- RV/LV ratio >1.0 on echo indicates massive PE
- Troponin elevation suggests RV strain
- Right heart failure → systemic venous congestion → hepatic dysfunction
📌 Remember: SHOCK-MODS - Shock leads to Multiple Organ Dysfunction Syndrome through hypoperfusion, inflammation, and cellular dysfunction
| System Integration | Primary Dysfunction | Secondary Effects | Tertiary Complications | Monitoring Parameter |
|---|---|---|---|---|
| Cardio-Renal | Heart failure | Decreased GFR | Fluid overload | BUN/Cr ratio >20:1 |
| Hepato-Renal | Liver failure | Decreased albumin | Ascites, edema | Albumin <2.5 g/dL |
| Cardio-Pulmonary | Pulmonary edema | Hypoxemia | RV dysfunction | BNP >400 pg/mL |
| Neuro-Cardiac | Increased ICP | Hypertension | Cushing's triad | CPP <60 mmHg |
| Renal-Metabolic | Kidney dysfunction | Acidosis | Hyperkalemia | Anion gap >12 |
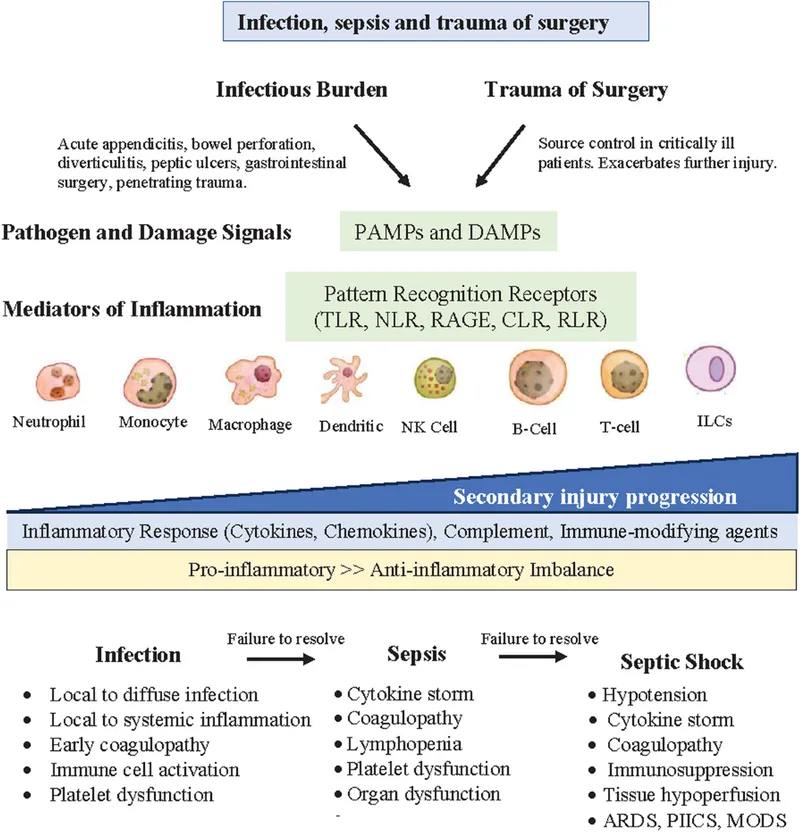
The systemic inflammatory response syndrome (SIRS) illustrates how local tissue injury triggers systemic dysfunction through cytokine release, endothelial activation, and coagulation cascade activation. Understanding this pathway explains why sepsis can cause multi-organ failure even with source control.
- Neuro-Endocrine-Immune Integration
- Hypothalamic-pituitary-adrenal axis activation during stress
- Cortisol release provides anti-inflammatory effects
- Adrenal insufficiency in septic shock requires hydrocortisone
- Sympathetic nervous system activation in shock states
- Norepinephrine release maintains vascular tone
- Beta-blocker use in sepsis may worsen hypotension
- Immune system dysfunction in critical illness
- Immunoparalysis increases secondary infection risk
- Lymphocyte count <1000 predicts poor outcomes
- Hypothalamic-pituitary-adrenal axis activation during stress
💡 Master This: Relative adrenal insufficiency occurs in 60% of septic shock patients, where random cortisol <25 μg/dL or poor response to cosyntropin indicates need for hydrocortisone 200mg/day
Understanding these integration principles through rapid mastery frameworks enables synthesis of complex clinical presentations into actionable treatment strategies.
🌐 Multi-System Integration Nexus: The Physiological Network Architecture
🎯 Clinical Mastery Arsenal: The Emergency Medicine Rapid Reference
📌 Remember: CRASH-CART - Cardiac arrest, Respiratory failure, Anaphylaxis, Shock, Hemorrhage, Coma, Arrhythmia, Respiratory distress, Trauma - Nine presentations requiring immediate resuscitation
| Emergency Syndrome | Recognition Threshold | First-Line Treatment | Time Target | Success Metric |
|---|---|---|---|---|
| Cardiac Arrest | No pulse | CPR + defibrillation | <2 minutes | ROSC |
| Anaphylaxis | 2+ system involvement | Epinephrine 0.3mg IM | <5 minutes | Symptom resolution |
| Status Epilepticus | Seizure >5 minutes | Lorazepam 4mg IV | <10 minutes | Seizure termination |
| Septic Shock | qSOFA ≥2 + hypotension | Fluid + antibiotics | <60 minutes | MAP >65 mmHg |
| STEMI | ST elevation >1mm | Dual antiplatelet + PCI | <90 minutes | Reperfusion |
The Emergency Drug Dosing Arsenal provides weight-based calculations for critical medications:
- Resuscitation Medication Quick Reference
- Epinephrine: 0.01 mg/kg IV (cardiac arrest), 0.3-0.5mg IM (anaphylaxis)
- Atropine: 0.02 mg/kg IV (minimum 0.1mg, maximum 3mg)
- Amiodarone: 5 mg/kg IV loading dose, then 10-15 mg/kg/day
- Dopamine: 5-20 μg/kg/min (inotrope), >20 μg/kg/min (vasopressor)
- Norepinephrine: 0.1-3 μg/kg/min (first-line vasopressor in shock)
💡 Master This: Push-dose pressors provide immediate hemodynamic support - phenylephrine 50-200 μg IV or epinephrine 5-20 μg IV - while preparing continuous infusions
The Clinical Decision Rules Compendium enables rapid risk stratification:
- High-Yield Scoring Systems
- HEART Score (chest pain): 0-3 low risk, 4-6 moderate, 7-10 high
- Wells Score (PE): <2 unlikely, 2-6 moderate, >6 high probability
- CHADS₂-VASc (stroke risk): 0-1 low, 2-3 moderate, >4 high
- APACHE II (ICU mortality): <10 low, 10-20 moderate, >20 high
- SOFA Score (organ dysfunction): 1-2 mild, 3-4 moderate, >4 severe
⚠️ Warning: High-sensitivity troponin can be elevated in renal failure, sepsis, and pulmonary embolism - always correlate with clinical presentation and ECG changes
This comprehensive emergency medicine foundation provides the systematic approach and evidence-based tools necessary for excellence in acute care practice, where rapid recognition, systematic assessment, and timely intervention determine patient outcomes.
🎯 Clinical Mastery Arsenal: The Emergency Medicine Rapid Reference
Practice Questions: Acute Care
Test your understanding with these related questions
A scientist in Chicago is studying a new blood test to detect Ab to EBV with increased sensitivity and specificity. So far, her best attempt at creating such an exam reached 82% sensitivity and 88% specificity. She is hoping to increase these numbers by at least 2 percent for each value. After several years of work, she believes that she has actually managed to reach a sensitivity and specificity much greater than what she had originally hoped for. She travels to China to begin testing her newest blood test. She finds 2,000 patients who are willing to participate in her study. Of the 2,000 patients, 1,200 of them are known to be infected with EBV. The scientist tests these 1,200 patients' blood and finds that only 120 of them tested negative with her new exam. Of the patients who are known to be EBV-free, only 20 of them tested positive. Given these results, which of the following correlates with the exam's specificity?












