Systemic sclerosis (scleroderma) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Systemic sclerosis (scleroderma). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Systemic sclerosis (scleroderma) US Medical PG Question 1: A 51-year-old woman is brought to the emergency department after not being able to urinate for the past 12 hours. She also complains of a headache that is sharp in nature, 9/10, without radiation, and associated with nausea and vomiting. She neither smokes cigarettes nor drinks alcohol. She complains that her fingers have become numb and very painful on exposure to cold weather during the last few months. She has also noticed her fingers change color from blue to pale to red on cold exposure. Her face looks shiny with thickened, wrinkle-free skin. She has had joint pain and stiffness for the last 20 years. She takes over-the-counter omeprazole for heartburn, which she says improves her symptoms. She has unintentionally lost 9 kg (20 lb) in the last 6 months. She has no previous history of diabetes, hypertension, chest pain, orthopnea, or paroxysmal nocturnal dyspnea. Her mother has rheumatoid arthritis for which she takes methotrexate, and her father takes medications for hypertension and hypercholesterolemia. Her temperature is 37°C (98.6°F), blood pressure is 210/120 mm Hg, pulse is 102/min, respiratory rate is 18/min, and BMI is 22 kg/m2.
Laboratory test
Complete blood count:
Hemoglobin 9.5 g/dL
Leukocytes 15,500/mm3
Platelets 90,000/mm3
Serum haptoglobin 20 mg/dL (30–200 mg/dL)
Serum creatinine 2.3 mg/dL
Blood urea nitrogen 83.5 mg/dL
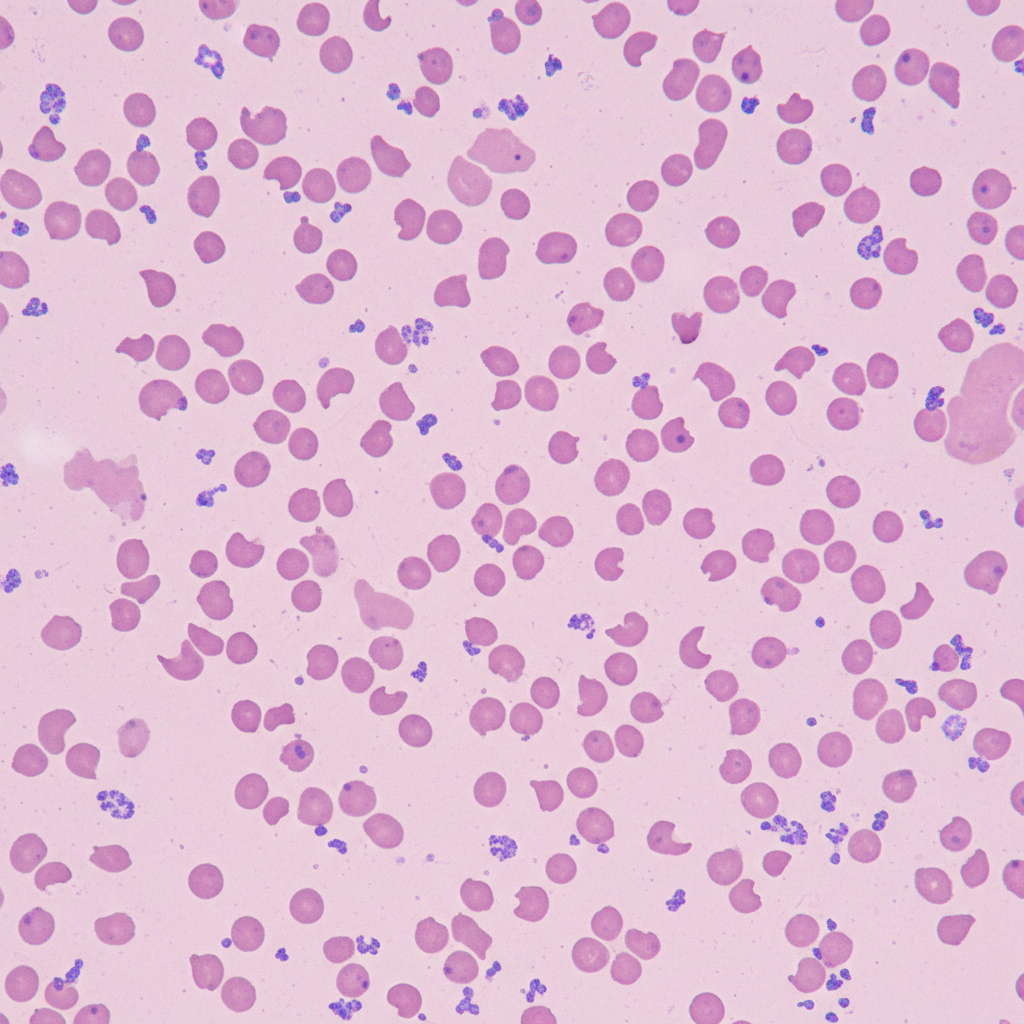
The peripheral blood film of the patient shows the following. Which of the following would be the most appropriate treatment for this patient?
- A. Nitroprusside
- B. Renal transplantation
- C. Ramipril (Correct Answer)
- D. Dialysis
- E. Labetalol
Systemic sclerosis (scleroderma) Explanation: ***Ramipril***
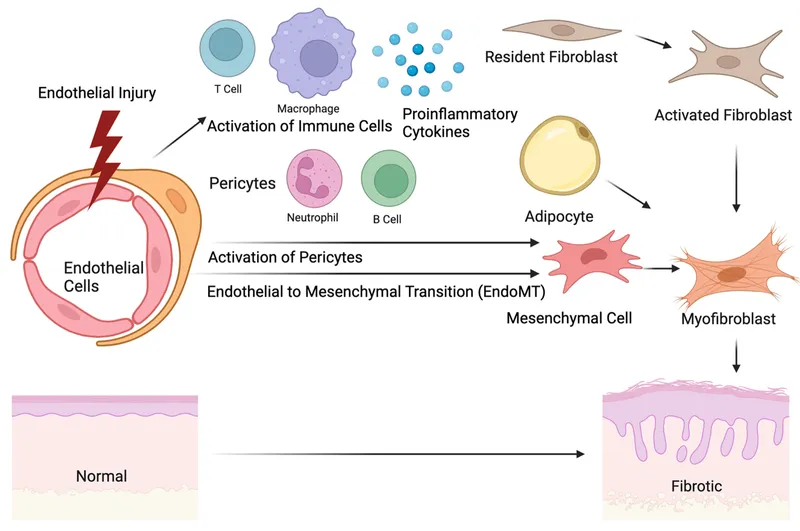
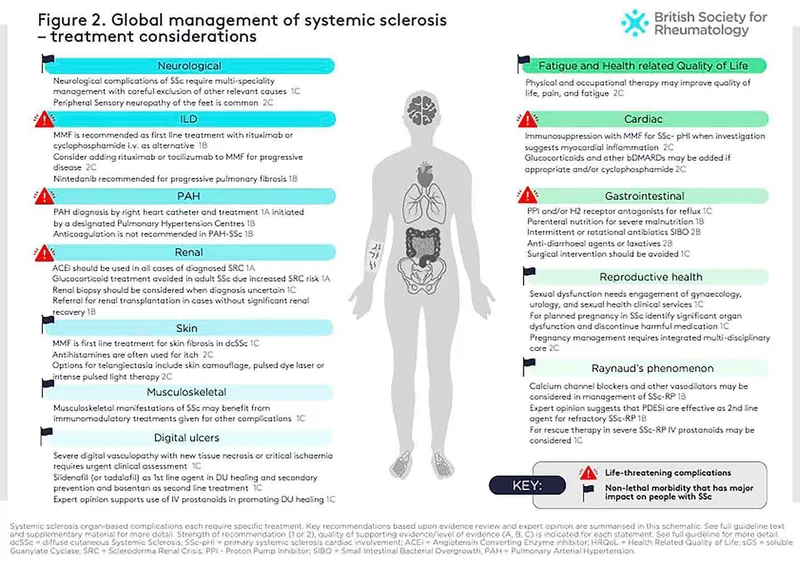
- This patient presents with **scleroderma renal crisis (SRC)**, characterized by new-onset **malignant hypertension**, **acute kidney injury**, and features of **microangiopathic hemolytic anemia**. **ACE inhibitors** like ramipril are the **first-line treatment** for SRC, regardless of the blood pressure, as they can reverse renal ischemia and improve kidney function.
- The patient's presentation with **Raynaud phenomenon**, **thickened skin** (sclerodactyly leading to "wrinkle-free" appearance), **esophageal dysmotility** (heartburn managed with omeprazole), and **unintentional weight loss** over many months are all consistent with systemic sclerosis, which predisposed her to SRC.
*Nitroprusside*
- While nitroprusside is a potent vasodilator used in **hypertensive emergencies**, it is **contraindicated** in scleroderma renal crisis.
- Its rapid reduction in blood pressure can exacerbate renal hypoperfusion and worsen kidney function in SRC.
*Renal transplantation*
- Renal transplantation is a treatment option for **end-stage renal disease**, but it is **not the initial management** for acute kidney injury in the context of scleroderma renal crisis.
- The priority is to stabilize the patient's condition and preserve existing renal function with ACE inhibitors.
*Dialysis*
- Dialysis is indicated for **severe kidney failure** or uremia, which may develop if SRC is not adequately treated or if kidney function rapidly deteriorates.
- However, the primary goal in SRC is to prevent progression to dialysis through prompt and aggressive ACE inhibitor therapy, making it not the most appropriate initial treatment.
*Labetalol*
- Labetalol is a **beta-blocker with alpha-blocking activity** used to treat **hypertensive emergencies**, but it is generally **not the first-line agent for SRC**.
- While it can lower blood pressure, ACE inhibitors are specifically preferred in SRC due to their targeted effect on the **renin-angiotensin-aldosterone system (RAAS)** and ability to reverse renal ischemia.
Systemic sclerosis (scleroderma) US Medical PG Question 2: A 60-year-old African American woman presents to her family physician with shortness of breath on exertion. She also describes shortness of breath when she lies down to go to bed at night, as well as recent swelling in her ankles. Past medical history is significant for long-standing hypertension, for which she takes amlodipine and lisinopril. Her temperature is 36.8°C (98.2°F), the heart rate is 90/min, the respiratory rate is 15/min, and the blood pressure is 135/80 mm Hg. The physical exam is significant for JVD, lower extremity pitting edema, laterally displaced PMI, left ventricular heave, bilateral pulmonary crackles, and an S4 heart sound. Chest X-ray demonstrates pulmonary vascular congestion, Kerley B lines, and cardiomegaly. Echocardiogram demonstrates a preserved ejection fraction. Kidney biopsy would likely demonstrate which of the following?
- A. Thinning of the intima and media
- B. Onion-skinning
- C. Nodular sclerosis
- D. Intimal thickening and medial hypertrophy (Correct Answer)
- E. Fibrinoid necrosis
Systemic sclerosis (scleroderma) Explanation: ***Intimal thickening and medial hypertrophy***
* The patient's presentation of **heart failure with preserved ejection fraction (HFpEF)**, long-standing **hypertension**, and findings like left ventricular heave and S4 heart sound strongly suggest **hypertensive cardiomyopathy**, which in turn causes **hypertensive nephrosclerosis**.
* **Hypertensive nephrosclerosis** is characterized by **intimal thickening** and **medial hypertrophy** of renal arterioles, leading to **ischemia** and atrophy of glomeruli and tubules.
*Thinning of the intima and media*
* This is not a characteristic pathological change seen in hypertensive nephrosclerosis.
* In hypertension, the vessel walls typically undergo thickening due to **hypertrophy** and **hyperplasia** of smooth muscle cells and increased extracellular matrix, not thinning.
*Onion-skinning*
* **"Onion-skinning"** is a hallmark feature of **malignant hypertension**, characterized by concentric laminar thickening of the arteriolar walls.
* The patient's blood pressure (135/80 mmHg) is not consistent with malignant hypertension, which would typically involve much higher blood pressure readings.
*Nodular sclerosis*
* **Nodular sclerosis** (also known as **Kimmelstiel-Wilson lesions**) is characteristic of **diabetic nephropathy**, not primarily hypertensive nephrosclerosis.
* While diabetes and hypertension often co-exist, the prompt in this case points more directly to long-standing hypertension as the primary cause of renal damage.
*Fibrinoid necrosis*
* **Fibrinoid necrosis** of arterioles is also associated with **malignant hypertension** and some forms of vasculitis.
* This patient's blood pressure is controlled (135/80 mmHg) and does not indicate the severe, rapid increase in blood pressure seen in malignant hypertension.
Systemic sclerosis (scleroderma) US Medical PG Question 3: A 47-year-old woman comes to the physician because of a 1-month history of progressive weakness. She has had increased difficulty climbing stairs and standing from a seated position. She takes no medications. Neurologic examination shows weakness of the proximal muscles. Skin examination shows diffuse erythema of the upper back, posterior neck, and shoulders. A photograph of the patient's eye is shown. Antibodies against which of the following are most likely to be present in this patient?
- A. Histones
- B. Mi-2 protein (Correct Answer)
- C. Centromeres
- D. La protein
- E. Scl-70 protein
Systemic sclerosis (scleroderma) Explanation: ***Mi-2 protein***
- The patient's presentation with **progressive proximal muscle weakness** and characteristic skin findings (**heliotrope rash** on the eyes and **Shawl sign** on the upper back/shoulders) is highly indicative of **dermatomyositis**.
- **Anti-Mi-2 antibodies** are highly specific for dermatomyositis, particularly in patients with classic skin findings.
*Histones*
- **Anti-histone antibodies** are most commonly associated with **drug-induced lupus erythematosus**.
- This patient has no history of medication use that would suggest a drug-induced lupus, and her symptoms are more consistent with dermatomyositis.
*Centromeres*
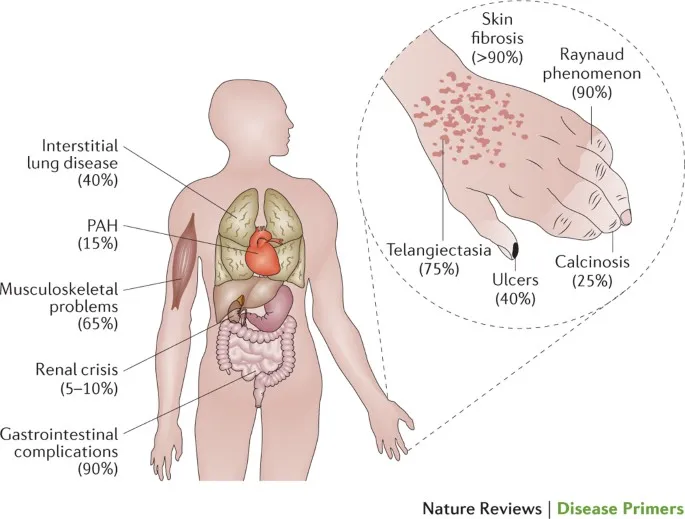
- **Anti-centromere antibodies** are characteristic of the **limited cutaneous systemic sclerosis** (CREST syndrome).
- This condition presents with diverse symptoms like **calcinosis**, **Raynaud's phenomenon**, **esophageal dysmotility**, **sclerodactyly**, and **telangiectasias**, which are not observed in this patient.
*La protein*
- **Anti-La (SS-B) antibodies** are associated with **Sjögren's syndrome**, an autoimmune disorder primarily affecting exocrine glands.
- While Sjögren's can present with fatigue, the prominent **proximal muscle weakness** and **dermatological signs** seen in this case are not typical of Sjögren's.
*Scl-70 protein*
- **Anti-Scl-70 antibodies** (anti-topoisomerase I) are associated with **diffuse cutaneous systemic sclerosis**.
- This condition is characterized by widespread skin thickening, **Raynod's phenomenon**, and significant internal organ involvement (e.g., lung fibrosis, renal crisis), which are not described in this patient.
Systemic sclerosis (scleroderma) US Medical PG Question 4: A 45-year-old woman presents to the clinic with a variety of complaints on different areas of her body, including telangiectasias on both the upper and lower extremities, bluish discoloration of the fingertips when exposed to cold, and burning midsternal chest pain. She is a tobacco smoker and works as a school teacher. After evaluation, an anti-centromere antibody test is ordered, and returns with an elevated titer. Which of the following symptoms are least likely to be seen in this patient's condition?
- A. Gastroesophageal reflux
- B. Spasm of blood vessels in response to cold or stress
- C. Thickening and tightening of the skin on the fingers
- D. Dysphagia
- E. Erythematous periorbital rash (Correct Answer)
Systemic sclerosis (scleroderma) Explanation: ***Erythematous periorbital rash***
- An **erythematous periorbital rash** (**heliotrope rash**) is highly characteristic of **dermatomyositis**, not the patient's condition.
- This symptom, along with **Gottron's papules** and **proximal muscle weakness**, would point away from scleroderma.
*Gastroesophageal reflux*
- **Gastroesophageal reflux** is common in **scleroderma**, particularly the limited cutaneous systemic sclerosis (CREST) variant.
- Esophageal dysmotility and lower esophageal sphincter incompetence lead to reflux and **heartburn**.
*Spasm of blood vessels in response to cold or stress*
- This describes **Raynaud's phenomenon**, a hallmark feature of **limited cutaneous systemic sclerosis (CREST syndrome)**.
- The patient's description of "bluish discoloration of the fingertips when exposed to cold" directly points to this symptom.
*Thickening and tightening of the skin on the fingers*
- **Sclerodactyly**, or thickening and tightening of the skin on the fingers, is a primary manifestation of **scleroderma**.
- This is a key diagnostic criterion for systemic sclerosis, especially in the limited form.
*Dysphagia*
- **Dysphagia**, or difficulty swallowing, is very common in **scleroderma** due to **esophageal hypomotility** and fibrosis.
- The sensation of food sticking or difficulty propelling food down the esophagus is a frequent complaint.
Systemic sclerosis (scleroderma) US Medical PG Question 5: A 52-year-old African-American woman presents to the office complaining of difficulty swallowing for 1 week, and described it as "food getting stuck in her throat". Her discomfort is mainly for solid foods, and she does not have any problem with liquids. She further adds that she has frequent heartburn and lost 5 pounds in the last month because of this discomfort. She sometimes takes antacids to relieve her heartburn. Her past medical history is insignificant. She is an occasional drinker and smokes a half pack of cigarettes a day. On examination, her skin is shiny and taut especially around her lips and fingertips. A barium swallow study is ordered. Which of the following is the most likely diagnosis?
- A. Scleroderma (Correct Answer)
- B. Zenker's diverticulum
- C. Diffuse esophageal spasm
- D. Achalasia
- E. Polymyositis
Systemic sclerosis (scleroderma) Explanation: ***Scleroderma***
- The combination of **dysphagia for solids**, **heartburn**, **weight loss**, and characteristic **skin changes** (shiny, taut skin around lips and fingertips) is highly suggestive of **scleroderma (systemic sclerosis)**.
- Scleroderma can cause **esophageal dysmotility** due to fibrosis and atrophy of the smooth muscle, leading to impaired peristalsis and a weakened lower esophageal sphincter.
*Zenker's diverticulum*
- This condition typically presents with **regurgitation of undigested food**, **halitosis**, and sometimes a **gurgling sound** in the neck, which are not described here.
- It involves a **pouch protruding from the pharyngeal wall** and is less commonly associated with widespread skin changes.
*Diffuse esophageal spasm*
- Characterized by **intermittent dysphagia** for both solids and liquids and **chest pain** that can mimic angina.
- While it causes dysphagia, it typically does not present with the specific dermatological features seen in this patient.
*Achalasia*
- Presents with progressive **dysphagia for both solids and liquids**, often accompanied by **regurgitation of undigested food** and occasional chest pain.
- It is caused by the **failure of the lower esophageal sphincter to relax** and loss of peristalsis in the esophageal body, but lacks the characteristic skin findings of scleroderma.
*Polymyositis*
- This is an **inflammatory myopathy** affecting skeletal muscles, leading to muscle weakness, particularly in the proximal muscles.
- While it can cause **oropharyngeal dysphagia** due to striated muscle involvement, it typically does not cause the esophageal dysmotility or the characteristic skin changes seen in this case.
Systemic sclerosis (scleroderma) US Medical PG Question 6: A 45-year-old woman comes to the physician's office with her 17-year-old daughter. She tells the physician that she developed Sjögren's syndrome when she was her daughter's age, and that she is concerned about her daughter developing the same condition. The girl appears to be in good health, with no signs or symptoms of the disease or pathology. Which of the following antibodies will most likely be positive if the woman's daughter were to develop Sjögren's syndrome?
- A. Anti-dsDNA antibodies
- B. Anti-histone antibodies
- C. Anti-cyclic citrullinated antibodies
- D. Anti-topoisomerase (anti-Scl 70) antibodies
- E. Anti-SS-B (anti-La) antibodies (Correct Answer)
Systemic sclerosis (scleroderma) Explanation: ***Anti-SS-B (anti-La) antibodies***
- **Anti-SS-B (anti-La)** antibodies are highly specific for **Sjögren's syndrome** and are often found in conjunction with anti-SS-A (anti-Ro) antibodies.
- The presence of anti-SS-B antibodies supports a diagnosis of Sjögren's syndrome, particularly in patients with classic symptoms like **dry eyes** and **dry mouth**.
*Anti-dsDNA antibodies*
- **Anti-dsDNA antibodies** are most strongly associated with **systemic lupus erythematosus (SLE)**, particularly with lupus nephritis.
- They are not a primary diagnostic marker for Sjögren's syndrome, although some patients with Sjögren's may have secondary SLE.
*Anti-histone antibodies*
- **Anti-histone antibodies** are characteristic of **drug-induced lupus erythematosus**, though they can be present in other autoimmune diseases.
- They are not a specific marker for Sjögren's syndrome.
*Anti-cyclic citrullinated antibodies*
- **Anti-cyclic citrullinated peptides (anti-CCP) antibodies** are a sensitive and specific marker for **rheumatoid arthritis**.
- While Sjögren's and RA can coexist, anti-CCP antibodies are not indicative of Sjögren's syndrome itself.
*Anti-topoisomerase (anti-Scl 70) antibodies*
- **Anti-topoisomerase I (anti-Scl-70) antibodies** are specific for **systemic sclerosis (scleroderma)**, particularly the diffuse cutaneous form.
- They are not found in Sjögren's syndrome.
Systemic sclerosis (scleroderma) US Medical PG Question 7: A 27-year-old woman presents with a history of repeated episodes of discoloration of the fingers over the last 3 years. She mentions that the episodes are usually triggered by exposure to cold, which leads to a sequential white, blue, and red discoloration of her fingers, followed by resolution of the symptoms. During an episode, she experiences pain and numbness in the affected fingers. The episodes are usually of short duration and do not interfere with her life, so she did not seek medical advice till now. Which of the following additional clinical features in this patient would most likely support the most likely diagnosis?
- A. Generalized pruritus
- B. Telangiectasia over face (Correct Answer)
- C. Calcinosis on the dorsal surface of the forearm
- D. Photosensitive skin rash
- E. Bilateral symmetrical involvement of the extremities
Systemic sclerosis (scleroderma) Explanation: ***Telangiectasia over face***
- The patient's history of **Raynaud phenomenon** (white, blue, red discoloration of fingers triggered by cold) along with associated pain and numbness suggests a secondary form of Raynaud, often seen in **systemic sclerosis (scleroderma)**.
- **Telangiectasias** are a highly specific component of **CREST syndrome** (Calcinosis, Raynaud phenomenon, Esophageal dysmotility, Sclerodactyly, Telangiectasias), which is a limited form of systemic sclerosis.
- Telangiectasias over the face are particularly characteristic and help distinguish systemic sclerosis from other causes of Raynaud phenomenon.
*Generalized pruritus*
- While pruritus can occur in various systemic conditions, it is not a classic or specific feature that would strongly support a diagnosis of autoimmune connective tissue disease like systemic sclerosis.
- It is more commonly associated with conditions like **dermatitis**, **liver disease**, or **renal failure**.
*Calcinosis on the dorsal surface of the forearm*
- **Calcinosis** is indeed a feature of **CREST syndrome**, but it typically presents as hard, subcutaneous nodules over pressure points or fingertips, not primarily on the dorsal forearm.
- While calcinosis is part of CREST, **telangiectasias are more specific and appear earlier** in the disease course, making them a better distinguishing feature.
- Calcinosis tends to develop later and is less commonly the presenting feature.
*Photosensitive skin rash*
- A **photosensitive skin rash** is a hallmark feature of **systemic lupus erythematosus (SLE)**, particularly the malar rash or discoid lupus.
- It is not typically associated with systemic sclerosis or Raynaud phenomenon as a primary distinguishing feature.
*Bilateral symmetrical involvement of the extremities*
- While some autoimmune diseases can cause bilateral symmetrical involvement, this is a very general description and does not specifically point to systemic sclerosis or help differentiate it from other conditions.
- Raynaud phenomenon itself commonly affects both hands, but "symmetrical involvement of extremities" is too broad to be diagnostically specific in this context.
Systemic sclerosis (scleroderma) US Medical PG Question 8: A 35-year-old woman comes to the clinic with complaints of joint pain and stiffness for the past few months. Her hands, lower back, and left knee are involved and associated with morning stiffness that improves throughout the day with activities. She also complains that her fingers change color upon exposure to cold. She has also noticed a tightening of the skin on her face and thinning of her lips. She feels tired throughout the day and has taken over-the-counter multivitamins that do not seem to help her much. The patient does not smoke cigarettes and drinks alcohol socially. She was diagnosed with hypertension 1 year ago and has been taking hydralazine for the past year. She lost her parents in a road traffic accident 3 years ago. Temperature is 36.7°C (98°F), blood pressure is 140/85 mm Hg, pulse is 72/min, respirations are 12/min, and BMI is 25 kg/m2. Her skin appears shiny and slightly thickened, especially her face and hands.
Laboratory investigation:
Complete blood count
Hemoglobin 9.5 g/dl
Leucocytes 5,500/mm3
Platelets 150,000/mm3
ANA positive
Anti-centromere Antibody negative
Anti Scl-70 positive
Anti Jo-1 negative
Anti-histone negative
Anti DsDNA negative
What is the most likely diagnosis in this patient?
- A. Polymyositis
- B. SLE
- C. Limited cutaneous systemic scleroderma
- D. Diffuse cutaneous systemic scleroderma (Correct Answer)
- E. Drug-induced lupus
Systemic sclerosis (scleroderma) Explanation: ***Diffuse cutaneous systemic scleroderma***
- The presence of **anti-Scl-70 (anti-topoisomerase I) antibodies**, along with **widespread skin thickening** involving the hands and face, and **internal organ involvement** (hypertension, joint pain, Raynaud's phenomenon), points to diffuse cutaneous systemic scleroderma.
- This variant is associated with rapid skin thickening, significant internal organ involvement (e.g., lung fibrosis, renal crisis), and a poorer prognosis compared to the limited form.
*Polymyositis*
- Characterized primarily by **proximal muscle weakness** and elevated muscle enzymes (e.g., CK), which are not described as prominent features in this patient's presentation.
- While ANA can be positive, **anti-Jo-1 antibodies** are more specific for polymyositis/dermatomyositis, and they are negative in this case.
*SLE*
- Although the patient presents with **arthralgias**, **fatigue**, and **positive ANA**, several key features of SLE, such as malar rash, discoid rash, serositis, renal involvement (beyond hypertension, which can be seen in scleroderma), are absent.
- The prominent **skin thickening** and **positive anti-Scl-70** are not typical for SLE and make this diagnosis less likely.
*Limited cutaneous systemic scleroderma*
- This variant is characterized by **skin thickening restricted** to areas distal to the elbows and knees, with or without face/neck involvement.
- It is strongly associated with **anti-centromere antibodies**, which are negative in this patient, and typically has a slower progression and is associated with PAH.
*Drug-induced lupus*
- Although the patient is on **hydralazine**, a known cause of drug-induced lupus, the negative **anti-histone antibodies** make this diagnosis less likely.
- The extensive **skin thickening**, **Raynaud's phenomenon**, and **anti-Scl-70 antibodies** are not characteristic features of drug-induced lupus.
Systemic sclerosis (scleroderma) US Medical PG Question 9: A 29-year-old woman presents to the emergency department with joint pain and a notable rash. She has had joint pain for the past 12 months but noticed the rash recently as well as generalized malaise. She states her joint pain is symmetric, in her upper extremities, and is worse in the morning. Her temperature is 97.6°F (36.4°C), blood pressure is 111/74 mmHg, pulse is 83/min, respirations are 14/min, and oxygen saturation is 98% on room air. Laboratory studies are ordered as seen below.
Hemoglobin: 10 g/dL
Hematocrit: 30%
Leukocyte count: 6,800/mm^3 with normal differential
Platelet count: 207,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.9 mEq/L
HCO3-: 21 mEq/L
BUN: 30 mg/dL
Glucose: 120 mg/dL
Creatinine: 1.8 mg/dL
The patient is ultimately admitted to the hospital. Which of the following is the most appropriate test to monitor her disease progression?
- A. Rheumatoid factor
- B. Anti-topoisomerase
- C. Anti-dsDNA (Correct Answer)
- D. Anti-CCP
- E. Anti-nuclear antibody
Systemic sclerosis (scleroderma) Explanation: ***Anti-dsDNA***
- The patient's presentation with **symmetric polyarthritis**, a **rash**, and **renal involvement** (elevated BUN and creatinine) is highly suggestive of **Systemic Lupus Erythematosus (SLE)**.
- **Anti-dsDNA antibodies** correlate well with disease activity, especially **lupus nephritis**, making them an excellent marker for monitoring disease progression and response to therapy in SLE.
*Rheumatoid factor*
- **Rheumatoid factor** is primarily associated with **Rheumatoid Arthritis** and is generally not used for monitoring SLE activity.
- While some SLE patients may test positive for RF, it is not a specific marker for SLE.
*Anti-topoisomerase*
- **Anti-topoisomerase I (Scl-70) antibodies** are characteristic of **systemic sclerosis (scleroderma)**, particularly the diffuse cutaneous form.
- This antibody is not typically seen in SLE and does not help monitor its progression.
*Anti-CCP*
- **Anti-cyclic citrullinated peptide (anti-CCP) antibodies** are highly specific for **Rheumatoid Arthritis**.
- They are useful for diagnosis and prognosis in RA but have no role in monitoring SLE.
*Anti-nuclear antibody*
- **Antinuclear antibodies (ANA)** are present in almost all patients with SLE and are essential for diagnosis, but they do not correlate with disease activity.
- A positive ANA test is a screening tool but cannot be used to monitor disease progression or response to treatment.
Systemic sclerosis (scleroderma) US Medical PG Question 10: A 32-year-old woman presents with a 3-month history of intermittent blurred vision and problems walking. The patient states that she often feels “pins and needles” in her legs that cause her problems when she’s walking. The patient is afebrile, and her vital signs are within normal limits. An autoimmune disorder is suspected. Which of the following findings would most likely be present in this patient?
- A. Damaged myelin sheath and myelin-producing cells (Correct Answer)
- B. Absence of interneurons
- C. Destruction of blood-brain barrier
- D. Degeneration of anterior horn cells
- E. Decreased cerebrospinal fluid due to destruction of cells
Systemic sclerosis (scleroderma) Explanation: ***Damaged myelin sheath and myelin-producing cells***
- The patient's symptoms of intermittent **blurred vision** (optic neuritis), **problems walking** (ataxia, spasticity), and **paresthesias** ("pins and needles") are classical presentations of Multiple Sclerosis (MS).
- MS is characterized by multifocal areas of inflammation and **demyelination** in the central nervous system, where the **myelin sheath** surrounding axons is damaged, and the **oligodendrocytes** (myelin-producing cells) are attacked.
- This demyelination disrupts saltatory conduction, leading to the varied and intermittent neurological symptoms.
*Absence of interneurons*
- The absence of **interneurons** is typically associated with conditions like **spinal muscular atrophy** or certain **neuropathies**, which present with different clinical features (e.g., muscle weakness, atrophy) than those described.
- While interneurons are crucial for neuronal communication, their absence doesn't explain the *intermittent* and multifocal symptoms seen in this case.
*Destruction of blood-brain barrier*
- While **blood-brain barrier (BBB) breakdown** does occur in MS, it is a *consequence* of the inflammatory process rather than the primary *pathological finding* that directly explains the neurological symptoms.
- BBB destruction allows inflammatory cells to enter the CNS, contributing to demyelination, but the core issue remains the myelin damage itself.
*Degeneration of anterior horn cells*
- **Anterior horn cell degeneration** is the hallmark of **amyotrophic lateral sclerosis (ALS)** and **spinal muscular atrophy**, presenting with progressive muscle weakness, atrophy, and fasciculations.
- These conditions lack the sensory symptoms (paresthesias) and visual disturbances seen in this patient, and typically show a progressive rather than intermittent course.
*Decreased cerebrospinal fluid due to destruction of cells*
- **Decreased CSF volume** is not a characteristic feature of MS; in fact, CSF analysis often shows increased protein and **oligoclonal bands**.
- The destruction of cells in MS primarily affects myelin and oligodendrocytes, not cells responsible for CSF production or volume regulation.
More Systemic sclerosis (scleroderma) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.