Systemic lupus erythematosus US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Systemic lupus erythematosus. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Systemic lupus erythematosus US Medical PG Question 1: A 29-year-old woman, gravida 1, para 0, at 33 weeks' gestation comes to her doctor for a routine visit. Her pregnancy has been uncomplicated. She has systemic lupus erythematosus and has had no flares during her pregnancy. She does not smoke cigarettes, drink alcohol, or use illicit drugs. Current medications include iron, vitamin supplements, and hydroxychloroquine. Her temperature is 37.2°C (98.9°F), pulse is 70/min, respirations are 17/min, and blood pressure is 134/70 mm Hg. She appears well. Physical examination shows no abnormalities. Ultrasound demonstrates fetal rhythmic breathing for > 30 seconds, amniotic fluid with deepest vertical pocket of 1 cm, one distinct fetal body movement over 30 minutes, and no episodes of extremity extension over 30 minutes. Nonstress test is reactive and reassuring. Which of the following is the next best step in management?
- A. Administer corticosteroids and continue close monitoring (Correct Answer)
- B. Perform cesarean delivery
- C. Discontinue hydroxychloroquine and continue close monitoring
- D. Induction of labor
- E. Reassurance with expectant management
Systemic lupus erythematosus Explanation: ***Administer corticosteroids and continue close monitoring***
- The combination of a **nonreactive nonstress test (NST)** and an **amniotic fluid index (AFI) < 5 cm** (deepest vertical pocket of 1 cm) indicates **oligohydramnios** and potential fetal compromise, necessitating corticosteroid administration for lung maturity and close monitoring.
- While the NST is reassuring, the oligohydramnios is a significant concern that warrants intervention to optimize fetal outcomes and prepare for potential preterm delivery.
*Perform cesarean delivery*
- This step is **overly aggressive** given the reactive nonstress test and stable maternal condition.
- There are no immediate signs of **acute fetal distress** that would necessitate emergent delivery.
*Discontinue hydroxychloroquine and continue close monitoring*
- **Hydroxychloroquine** is safe and often continued during pregnancy for patients with systemic lupus erythematosus, as it helps prevent flares and is not associated with adverse fetal outcomes.
- Discontinuing it without a clear indication could lead to a **maternal SLE flare**, which could be detrimental to both mother and fetus.
*Induction of labor*
- Induction of labor is not indicated at this gestational age (33 weeks) unless there is clear evidence of **significant fetal distress** or maternal complications.
- While there is oligohydramnios, the **reactive NST** suggests sufficient fetal reserve to allow for corticosteroid administration to promote lung maturity first.
*Reassurance with expectant management*
- The finding of **oligohydramnios** (deepest vertical pocket of 1 cm) is a significant concern, as it is associated with increased risks of **cord compression**, fetal growth restriction, and adverse perinatal outcomes.
- Therefore, expectant management without intervention would be **inappropriate** given this finding.
Systemic lupus erythematosus US Medical PG Question 2: A 40-year-old man presents to a clinic in Michigan in December complaining of painful blue fingers and toes. He also complains of numbness and tingling. The patient’s vital signs are within normal limits, and his symptoms typically disappear when he comes back into a warm room. The patient also notes that he recently moved to the area from Arizona and had recently recovered from a viral infection in which he had a low-grade fever and severe lymphadenopathy. Which of the following tests would most likely be positive in this patient?
- A. Direct Coomb’s test with anti-C3 reagent (Correct Answer)
- B. Anti-centromere antibody
- C. Anti-Ro antibody
- D. Indirect Coomb’s test
- E. Direct Coomb’s test with anti-IgG reagent
Systemic lupus erythematosus Explanation: ***Direct Coombs test with anti-C3 reagent***
- The patient presents with classic symptoms of **cold agglutinin disease**, characterized by painful blue fingers and toes (acrocyanosis) triggered by cold exposure that resolves with warming.
- The recent **viral infection with severe lymphadenopathy** suggests infections such as **Mycoplasma pneumoniae, EBV, or CMV**, which are well-known triggers for cold agglutinin disease.
- Cold agglutinins are **IgM antibodies** that bind to red blood cells at cold temperatures, causing **complement activation** (C3d deposition) and **extravascular hemolysis**.
- The **direct Coombs test with anti-C3 reagent** detects complement (C3) bound to RBC surfaces and is the diagnostic test of choice for cold agglutinin disease.
- The recent move from Arizona to Michigan in December provides the cold exposure trigger needed to manifest symptoms.
*Direct Coombs test with anti-IgG reagent*
- This test detects **IgG antibodies bound to red blood cells** and is positive in **warm autoimmune hemolytic anemia**, not cold agglutinin disease.
- Cold agglutinin disease is mediated by **IgM antibodies and complement (C3)**, not IgG, so this test would be negative.
*Indirect Coombs test*
- The **indirect Coombs test** detects **free antibodies in serum** against RBCs and is used primarily for blood typing and cross-matching.
- While it may detect cold agglutinins in serum, the **direct Coombs with anti-C3** is the more specific and diagnostic test for cold agglutinin disease.
*Anti-centromere antibody*
- **Anti-centromere antibodies** are highly specific for **limited cutaneous systemic sclerosis (CREST syndrome)**, which can present with Raynaud's phenomenon.
- However, the **acute onset** following a viral illness, the **severe lymphadenopathy**, and the **cold-triggered acrocyanosis** are more consistent with cold agglutinin disease rather than a chronic autoimmune connective tissue disease.
- Systemic sclerosis typically has a more insidious onset and is not triggered by viral infections.
*Anti-Ro antibody*
- **Anti-Ro antibodies** are associated with **Sjögren's syndrome** and **systemic lupus erythematosus (SLE)**.
- While Raynaud's can occur in these conditions, the clinical presentation with recent viral infection, severe lymphadenopathy, and cold-triggered symptoms points to cold agglutinin disease rather than SLE or Sjögren's syndrome.
Systemic lupus erythematosus US Medical PG Question 3: A 29-year-old woman presents to the emergency department with joint pain and a notable rash. She has had joint pain for the past 12 months but noticed the rash recently as well as generalized malaise. She states her joint pain is symmetric, in her upper extremities, and is worse in the morning. Her temperature is 97.6°F (36.4°C), blood pressure is 111/74 mmHg, pulse is 83/min, respirations are 14/min, and oxygen saturation is 98% on room air. Laboratory studies are ordered as seen below.
Hemoglobin: 10 g/dL
Hematocrit: 30%
Leukocyte count: 6,800/mm^3 with normal differential
Platelet count: 207,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.9 mEq/L
HCO3-: 21 mEq/L
BUN: 30 mg/dL
Glucose: 120 mg/dL
Creatinine: 1.8 mg/dL
The patient is ultimately admitted to the hospital. Which of the following is the most appropriate test to monitor her disease progression?
- A. Rheumatoid factor
- B. Anti-topoisomerase
- C. Anti-dsDNA (Correct Answer)
- D. Anti-CCP
- E. Anti-nuclear antibody
Systemic lupus erythematosus Explanation: ***Anti-dsDNA***
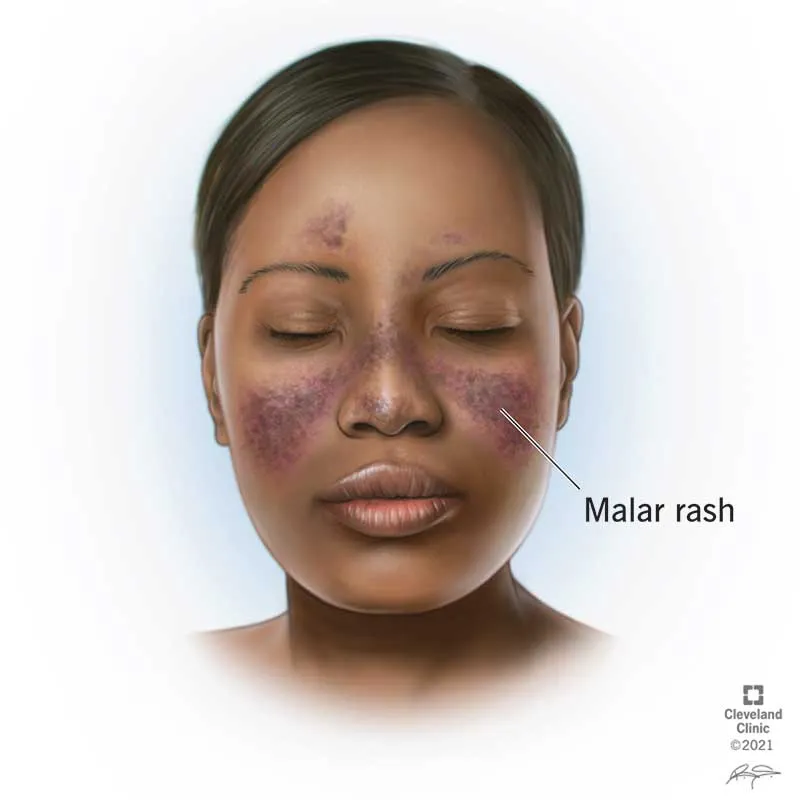
- The patient's presentation with **symmetric polyarthritis**, a **rash**, and **renal involvement** (elevated BUN and creatinine) is highly suggestive of **Systemic Lupus Erythematosus (SLE)**.
- **Anti-dsDNA antibodies** correlate well with disease activity, especially **lupus nephritis**, making them an excellent marker for monitoring disease progression and response to therapy in SLE.
*Rheumatoid factor*
- **Rheumatoid factor** is primarily associated with **Rheumatoid Arthritis** and is generally not used for monitoring SLE activity.
- While some SLE patients may test positive for RF, it is not a specific marker for SLE.
*Anti-topoisomerase*
- **Anti-topoisomerase I (Scl-70) antibodies** are characteristic of **systemic sclerosis (scleroderma)**, particularly the diffuse cutaneous form.
- This antibody is not typically seen in SLE and does not help monitor its progression.
*Anti-CCP*
- **Anti-cyclic citrullinated peptide (anti-CCP) antibodies** are highly specific for **Rheumatoid Arthritis**.
- They are useful for diagnosis and prognosis in RA but have no role in monitoring SLE.
*Anti-nuclear antibody*
- **Antinuclear antibodies (ANA)** are present in almost all patients with SLE and are essential for diagnosis, but they do not correlate with disease activity.
- A positive ANA test is a screening tool but cannot be used to monitor disease progression or response to treatment.
Systemic lupus erythematosus US Medical PG Question 4: A 27-year-old Asian woman presents to her primary care physician with joint pain and a headache. She has had intermittent joint and muscle pain for the past several months in the setting of a chronic headache. She states that the pain seems to migrate from joint to joint, and her muscles typically ache making it hard for her to sleep. The patient's past medical history is non-contributory, and she is currently taking ibuprofen for joint pain. Physical exam is notable for an asymmetrical pulse in the upper extremities. The patient has lost 10 pounds since her previous visit 2 months ago. Laboratory values are notable for an elevated C-reactive protein and erythrocyte sedimentation rate. Which of the following is the best next step in management?
- A. Methotrexate
- B. Recommend exercise and optimize the patient's sleep regimen
- C. Prednisone (Correct Answer)
- D. Temporal artery biopsy
- E. Anti-dsDNA level
Systemic lupus erythematosus Explanation: ***Prednisone***
- The patient's presentation with **migratory joint pain**, headache, **asymmetrical pulses**, and elevated inflammatory markers (CRP, ESR) in a young Asian woman suggests **Takayasu arteritis**.
- **Corticosteroids** like prednisone are the cornerstone of initial treatment for active Takayasu arteritis to suppress inflammation and prevent further vascular damage.
*Methotrexate*
- **Methotrexate** is an immunosuppressant often used in conjunction with corticosteroids or as a steroid-sparing agent in rheumatic conditions.
- However, it's not the initial monotherapy of choice for active, severe vasculitis requiring rapid inflammation control.
*Recommend exercise and optimize the patient's sleep regimen*
- While exercise and sleep are important for overall well-being, they do not address the underlying **severe inflammatory vasculitis** and are not an appropriate primary intervention for Takayasu arteritis.
- Delaying proper medical treatment can lead to irreversible vascular damage.
*Temporal artery biopsy*
- A **temporal artery biopsy** is the diagnostic gold standard for **Giant Cell Arteritis (GCA)**, which typically affects older individuals (>50 years).
- The patient's age (27 years) and other clinical features are more consistent with Takayasu arteritis, which affects larger arteries and often presents at a younger age.
*Anti-dsDNA level*
- An **anti-dsDNA level** is a specific marker for **Systemic Lupus Erythematosus (SLE)**.
- While SLE can cause joint pain and headaches, the presence of **asymmetrical pulses** and the demographic (young Asian woman) are more indicative of Takayasu arteritis, not SLE.
Systemic lupus erythematosus US Medical PG Question 5: A 32-year-old woman comes to the physician because of a 4-day history of low-grade fever, joint pain, and muscle aches. The day before the onset of her symptoms, she was severely sunburned on her face and arms during a hike with friends. She also reports being unusually fatigued over the past 3 months. Her only medication is a combined oral contraceptive pill. Her temperature is 37.9°C (100.2°F). Examination shows bilateral swelling and tenderness of the wrists and metacarpophalangeal joints. There are multiple nontender superficial ulcers on the oral mucosa. The detection of antibodies directed against which of the following is most specific for this patient's condition?
- A. Nuclear Sm proteins (Correct Answer)
- B. Fc region of IgG
- C. Single-stranded DNA
- D. Cell nucleus
- E. Histones
Systemic lupus erythematosus Explanation: ***Nuclear Sm proteins***
- Antibodies to **Sm proteins** (anti-Sm antibodies) are highly specific for **Systemic Lupus Erythematosus (SLE)**, although present in only a minority of patients.
- The patient's symptoms, including **photosensitivity (exacerbation by sunburn)**, **arthritis**, **oral ulcers**, and **fatigue**, are classic manifestations of SLE.
*Fc region of IgG*
- Antibodies directed against the **Fc region of IgG** are known as **rheumatoid factor (RF)**.
- While RF can be positive in a small percentage of SLE patients, it is most characteristic of **rheumatoid arthritis** and is not specific for SLE.
*Single-stranded DNA*
- Antibodies to **single-stranded DNA (anti-ssDNA antibodies)** are found in various autoimmune diseases, including SLE, but are **less specific** than anti-dsDNA or anti-Sm antibodies for SLE diagnosis.
- These antibodies can also be seen in drug-induced lupus and other conditions, making them a less definitive marker.
*Cell nucleus*
- Antibodies directed against the **cell nucleus** (antinuclear antibodies or **ANA**) are present in nearly all patients with SLE and are highly sensitive for the disease.
- However, ANA can also be positive in many other autoimmune conditions, infections, and even healthy individuals, making it **not specific** enough for a definitive diagnosis without other criteria.
*Histones*
- Antibodies to **histones** are most commonly associated with **drug-induced lupus erythematosus**.
- While they can be present in some cases of SLE, the patient's presentation does not strongly suggest drug-induced lupus, and anti-histone antibodies are not the most specific marker for typical SLE.
Systemic lupus erythematosus US Medical PG Question 6: A previously healthy 13-year-old girl is brought to the physician for evaluation of a 2-month history of fatigue. She reports recurrent episodes of pain in her right wrist and left knee. During this period, she has had a 4-kg (8.8-lb) weight loss. Her mother has rheumatoid arthritis. Her temperature is 38°C (100.4°F). Examination shows diffuse lymphadenopathy. Oral examination shows several painless oral ulcers. The right wrist and the left knee are swollen and tender. Laboratory studies show a hemoglobin concentration of 9.8 g/dL, a leukocyte count of 2,000/mm3, and a platelet count of 75,000/mm3. Urinalysis shows excessive protein. This patient's condition is associated with which of the following laboratory findings?
- A. Anti-citrullinated peptide antibodies
- B. Anti-dsDNA antibodies (Correct Answer)
- C. Leukocytoclastic vasculitis with IgA and C3 immune complex deposition
- D. Positive HLA-B27 test
- E. Excessive lymphoblasts
Systemic lupus erythematosus Explanation: ***Anti-dsDNA antibodies***
- The patient presents with **fatigue, fever, weight loss, lymphadenopathy, oral ulcers**, **arthralgia/arthritis**, and **proteinuria**, along with **anemia, leukopenia, and thrombocytopenia**. This constellation of symptoms is highly suggestive of **Systemic Lupus Erythematosus (SLE)**.
- **Anti-dsDNA antibodies** are highly specific for SLE and are often associated with active disease, particularly **lupus nephritis**, which is indicated by the proteinuria.
*Anti-citrullinated peptide antibodies*
- These antibodies are highly specific for **rheumatoid arthritis (RA)**, a disease primarily affecting joints in a symmetrical pattern.
- While the patient's mother has RA, the patient's systemic symptoms (fever, weight loss, anemia, leukopenia, thrombocytopenia, proteinuria) and oral ulcers are not typical features of RA, especially in a 13-year-old.
*Leukocytoclastic vasculitis with IgA and C3 immune complex deposition*
- This finding is characteristic of **IgA vasculitis (Henoch-Schönlein Purpura)**, which typically presents with a palpable purpuric rash, arthritis, abdominal pain, and renal involvement (hematuria/proteinuria).
- The patient's presentation lacks the characteristic rash and GI symptoms, making this diagnosis less likely.
*Positive HLA-B27 test*
- A positive **HLA-B27** is associated with **spondyloarthropathies** such as ankylosing spondylitis, psoriatic arthritis, and reactive arthritis.
- These conditions primarily affect the spine and sacroiliac joints, often with enthesitis, and do not typically present with the multi-systemic features like cytopenias, oral ulcers, and significant proteinuria observed in this patient.
*Excessive lymphoblasts*
- The presence of **excessive lymphoblasts** in the bone marrow or blood is indicative of **acute lymphoblastic leukemia (ALL)**.
- Although ALL can present with fatigue, fever, weight loss, anemia, and thrombocytopenia, it is less commonly associated with oral ulcers, arthritis, and significant proteinuria. Additionally, while the patient has leukopenia (2,000/mm3), the presence of circulating lymphoblasts would be a key distinguishing feature of ALL that is not mentioned in this case.
Systemic lupus erythematosus US Medical PG Question 7: A 31-year-old woman presents to her primary care provider to discuss the results from a previous urine analysis. She has no new complaints and feels well. Past medical history is significant for systemic lupus erythematosus. She was diagnosed 5 years ago and takes hydroxychloroquine every day and prednisone when her condition flares. Her previous urine analysis shows elevated protein levels (4+) and blood (3+). The urine sediment contained red blood cells (6 RBCs/high-power field). The treating physician would like to perform a renal biopsy to rule out lupus nephritis. What type of hypersensitivity is suggestive of lupus nephritis?
- A. Type IV, mediated by IgG and IgM antibodies
- B. Type IV, mediated by CD4+ T cells
- C. Type III, mediated by IgG antibodies (Correct Answer)
- D. Type I, mediated by IgE antibodies
- E. Type II, mediated by IgG and IgM antibodies
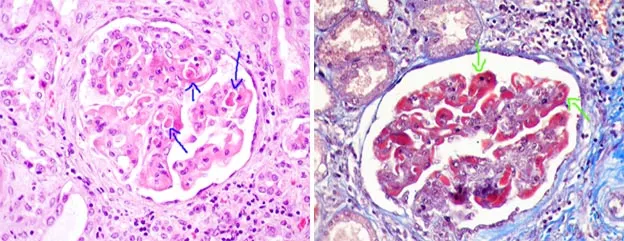
Systemic lupus erythematosus Explanation: ***Type III, mediated by IgG antibodies***
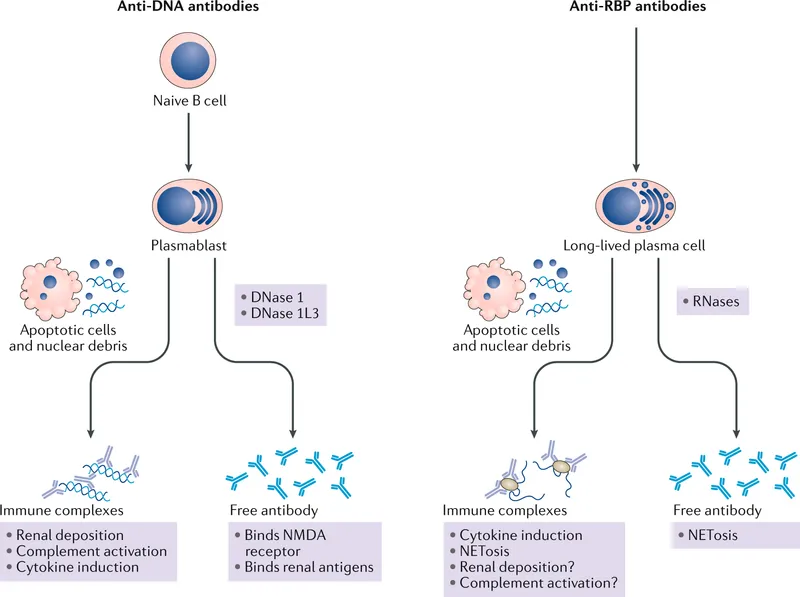
- Lupus nephritis is a classic example of a **Type III hypersensitivity reaction**, characterized by the formation of **immune complexes** (combinations of antibodies and antigens) in the circulation.
- These circulating **autoantibody-antigen complexes** deposit in the glomeruli of the kidneys, activating complement and initiating an inflammatory response that damages renal tissue.
*Type IV, mediated by IgG and IgM antibodies*
- **Type IV hypersensitivity** is a **delayed-type reaction** mediated by T cells, not antibodies.
- IgG and IgM antibodies are involved in Type II and Type III hypersensitivity, not Type IV.
*Type IV, mediated by CD4+ T cells*
- While **Type IV hypersensitivity** is indeed mediated by **CD4+ T cells** (and CD8+ T cells), lupus nephritis is primarily an **immune complex-mediated (Type III)** disease.
- T cells do play a role in the pathogenesis of SLE, but the direct kidney damage in lupus nephritis is driven by antibody-antigen complex deposition.
*Type I, mediated by IgE antibodies*
- **Type I hypersensitivity** is an **immediate allergic reaction** mediated by **IgE antibodies** binding to mast cells and basophils, leading to histamine release.
- This type of reaction is responsible for conditions like asthma, allergies, and anaphylaxis, and is not involved in lupus nephritis.
*Type II, mediated by IgG and IgM antibodies*
- **Type II hypersensitivity** involves **antibodies directly targeting antigens on cell surfaces or extracellular matrix components**, leading to cell lysis or dysfunction.
- While IgG and IgM are involved, the defining feature is direct binding to fixed tissue antigens rather than deposition of circulating immune complexes as seen in lupus nephritis.
Systemic lupus erythematosus US Medical PG Question 8: A 26-year-old woman presents with episodes of intermittent fever, arthralgias, constant fatigue, weight loss, and plaque-like rash on sun-exposed areas, which have been gradually increasing over the last 6 months. On presentation, her vital signs include: blood pressure is 110/80 mm Hg, heart rate is 87/min, respiratory rate is 14/min, and temperature is 37.5°C (99.5°F). Physical examination reveals an erythematous scaling rash on the patient’s face distributed in a ‘butterfly-like’ fashion, erythematous keratinized patches on the sun-exposed areas, and mild lower leg edema. During the workup, the patient is found to be positive for anti-Sm (anti-Smith) antibodies. Which process is altered in this patient?
- A. Protein folding
- B. Base-excision repair
- C. DNA transcription
- D. Ineffective clearance of cellular debris (Correct Answer)
- E. Mismatch repair
Systemic lupus erythematosus Explanation: ***Ineffective clearance of cellular debris***
- The patient's symptoms (fever, arthralgias, fatigue, weight loss, malar rash, photosensitive rash) along with a positive **anti-Sm antibody** are highly indicative of **Systemic Lupus Erythematosus (SLE)**.
- SLE is characterized by a defect in the **clearance of apoptotic cellular debris**, often due to complement deficiencies (particularly C1q, C2, C4) or defects in phagocytic clearance mechanisms.
- This ineffective clearance leads to prolonged exposure of intracellular nuclear antigens (including Smith antigen), which triggers autoantibody formation and immune complex deposition, causing the multisystem manifestations seen in SLE.
*Protein folding*
- **Protein folding disorders** involve the misfolding of proteins, which can lead to conditions like cystic fibrosis or Alzheimer's disease.
- This process is not directly implicated in the pathogenesis of SLE or the symptoms presented.
*Base-excision repair*
- **Base-excision repair** is a DNA repair pathway that primarily fixes damaged bases in DNA.
- While DNA damage can contribute to disease, defects in this specific repair mechanism are not a hallmark of SLE.
*DNA transcription*
- **DNA transcription** is the process by which genetic information from DNA is "transcribed" into RNA.
- While various autoimmune diseases can affect gene expression, a primary defect in the basic process of transcription itself is not characteristic of SLE.
*Mismatch repair*
- **Mismatch repair** is a DNA repair system that corrects errors, such as mispaired bases, that occur during DNA replication.
- Defects in mismatch repair are associated with conditions like Lynch syndrome, not the autoimmune manifestations seen in SLE.
Systemic lupus erythematosus US Medical PG Question 9: A 39-year-old woman comes to the physician because of a 5-day history of pain and stiffness in her hands and wrists and a nonpruritic generalized rash. The stiffness is worst in the morning and improves after 15–20 minutes of activity. She had fever and a runny nose 10 days ago that resolved without treatment. She is sexually active with a male partner and uses condoms inconsistently. She works as an elementary school teacher. Her temperature is 37.3°C (99.1°F), pulse is 78/min, and blood pressure is 120/70 mm Hg. Examination shows swelling, tenderness, and decreased range of motion of the wrists as well as the metacarpophalangeal and proximal interphalangeal joints. There is a lacy macular rash over the trunk and extremities. Laboratory studies, including erythrocyte sedimentation rate and anti-nuclear antibody and anti-dsDNA serology, show no abnormalities. Which of the following is the most likely cause of this patient's symptoms?
- A. Disseminated gonococcal disease
- B. Rheumatoid arthritis
- C. Systemic lupus erythematosus
- D. Parvovirus arthritis (Correct Answer)
- E. Psoriatic arthritis
Systemic lupus erythematosus Explanation: ***Parvovirus arthritis***
- This patient's symptoms, including **polyarthralgia** and a **lacy macular rash**, following a prodromal illness (fever, runny nose), are highly characteristic of parvovirus B19 infection. The joint involvement often resembles **rheumatoid arthritis** but is typically self-limiting.
- The patient's profession as an **elementary school teacher** increases her risk of exposure to parvovirus B19, which is common in children.
*Disseminated gonococcal disease*
- While it can cause **migratory polyarthralgia** and a rash, the rash is typically **pustular or vesicular** on an erythematous base, often with hemorrhagic lesions, which differs from the described lacy macular rash.
- The rash in DGI also tends to be sparse, unlike the generalized lacy rash described.
*Rheumatoid arthritis*
- Although it causes **symmetrical polyarthritis** with morning stiffness, the rash is not typical for RA, and symptoms usually persist for longer than 6 weeks to meet diagnostic criteria.
- Furthermore, **anti-nuclear antibody** (ANA) and **ESR** would likely be elevated in active RA, but are normal here.
*Systemic lupus erythematosus*
- SLE can present with **arthralgia** and various rashes, but the classic rash associated with SLE is a **malar (butterfly) rash** or **discoid rash**. A lacy macular rash is not typical.
- **ANA** and **anti-dsDNA** serologies are usually positive in SLE, but are normal in this patient.
*Psoriatic arthritis*
- Psoriatic arthritis is associated with **psoriasis skin lesions**, which are typically erythematous, scaly plaques, not a lacy macular rash.
- While it can affect the hands and wrists, the rash and preceding viral-like illness do not fit the typical presentation of psoriatic arthritis.
Systemic lupus erythematosus US Medical PG Question 10: A 52-year-old woman complains of intermittent diffuse abdominal pain that becomes worse after eating meals and several episodes of diarrhea, the last of which was bloody. These symptoms have been present for the previous 6 months but have worsened recently. She has had significant weight loss since the onset of symptoms. Her past medical history includes systemic lupus erythematosus (SLE), which has been difficult to manage medically. Vital signs include a blood pressure of 100/70 mm Hg, temperature of 37.1°C (98.8 °F), and pulse of 95/min. On physical examination, the patient appears to be in severe pain, and there is mild diffuse abdominal tenderness. Which of the following is the most likely diagnosis?
- A. Ischemic bowel disease (Correct Answer)
- B. Small bowel obstruction
- C. Acute pancreatitis
- D. Gastroenteritis
- E. Ulcerative colitis
Systemic lupus erythematosus Explanation: ***Ischemic bowel disease***
- The patient's history of **diffuse abdominal pain worsening after meals** (postprandial pain or "abdominal angina"), **bloody diarrhea**, and **significant weight loss** is highly suggestive of **chronic mesenteric ischemia**.
- Her history of **systemic lupus erythematosus (SLE)**, which can cause **vasculitis** and **hypercoagulability**, increases the risk of mesenteric artery thrombosis or emboli, leading to bowel ischemia.
*Small bowel obstruction*
- This typically presents with **colicky abdominal pain**, **vomiting**, and **abdominal distension**, often with obstipation.
- While it can cause pain, it does not typically lead to **bloody diarrhea** or chronic postprandial worsening of symptoms.
*Acute pancreatitis*
- Characterized by **severe epigastric pain** radiating to the back, often associated with nausea and vomiting, and elevated lipase/amylase.
- It does not typically present with **bloody diarrhea** or a chronic history of symptoms worsening after eating.
*Gastroenteritis*
- Usually presents with **acute onset** of nausea, vomiting, diarrhea, and fever, often resolving within a few days to a week.
- The **chronic nature** (6 months) of symptoms, significant weight loss, and the specific pattern of postprandial pain make gastroenteritis unlikely.
*Ulcerative colitis*
- While it causes **bloody diarrhea** and abdominal pain, it typically involves the colon and rectum, and pain is less commonly described as diffuse and worsening specifically after meals due to ischemia.
- The primary symptoms are usually **tenesmus**, frequent bowel movements, and rectal bleeding, and it does not typically present with the specific "abdominal angina" associated with mesenteric ischemia.
More Systemic lupus erythematosus US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.