Small vessel vasculitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Small vessel vasculitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Small vessel vasculitis US Medical PG Question 1: A 45-year-old man with asthma comes to the physician because of a 1-month history of progressively worsening shortness of breath and cough. He also has a history of chronic sinusitis and foot drop. Current medications include an albuterol inhaler and inhaled corticosteroid. Physical examination shows diffuse wheezing over both lung fields and tender subcutaneous nodules on both elbows. Laboratory studies show a leukocyte count of 23,000/mm3 with 26% eosinophils and a serum creatinine of 1.7 mg/dL. Urine microscopy shows red blood cell casts. Which of the following is the most likely diagnosis in this patient?
- A. Granulomatosis with polyangiitis
- B. Polyarteritis nodosa
- C. Eosinophilic granulomatosis with polyangiitis (Correct Answer)
- D. Microscopic polyangiitis
- E. Immunoglobulin A vasculitis
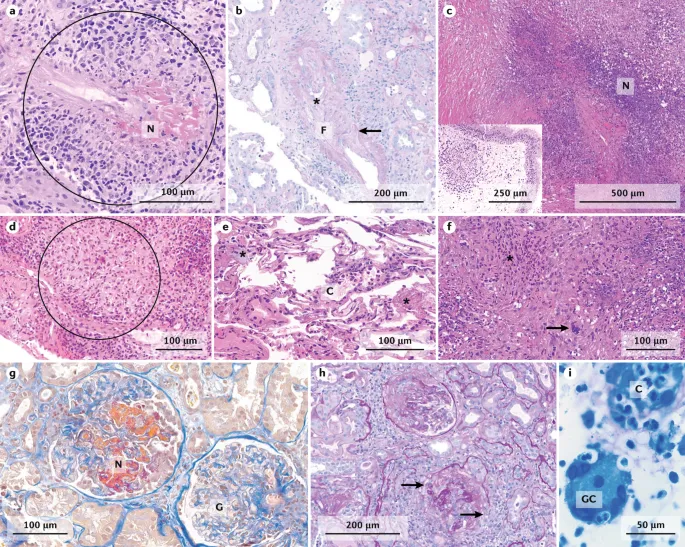
Small vessel vasculitis Explanation: ***Eosinophilic granulomatosis with polyangiitis (EGPA)***
- The patient presents with **asthma**, **chronic sinusitis**, **eosinophilia** (26%), and symptoms of vasculitis including **foot drop** (neuropathy), **renal impairment** (elevated creatinine, RBC casts), and **subcutaneous nodules**. This constellation is highly characteristic of EGPA (formerly Churg-Strauss syndrome).
- EGPA is a **small-to-medium vessel vasculitis** defined by **asthma**, **eosinophilia**, and **granulomatous inflammation**.
*Granulomatosis with polyangiitis (GPA)*
- GPA typically involves the **upper and lower respiratory tracts** and **kidneys**, often presenting with chronic sinusitis, lung nodules, and glomerulonephritis.
- While GPA can cause renal impairment and neuropathy, it is not primarily characterized by **asthma** and profound **eosinophilia**, which are key features in this patient.
*Polyarteritis nodosa (PAN)*
- PAN is a **necrotizing vasculitis of medium-sized arteries** that typically affects the kidneys, peripheral nerves, GI tract, and skin.
- PAN is not associated with **asthma** or significant **eosinophilia**, and it typically **spares the lungs**.
*Microscopic polyangiitis (MPA)*
- MPA is a **small-vessel vasculitis** primarily affecting the kidneys and lungs, a common cause of **pulmonary-renal syndrome**.
- While MPA can cause renal failure, and sometimes pulmonary symptoms, it does not typically present with **asthma** or marked **eosinophilia**.
*Immunoglobulin A vasculitis (IgAV)*
- IgAV, also known as Henoch-Schönlein purpura, is characterized by classic triad of **palpable purpura**, **arthralgia**, and **abdominal pain**, and frequently involves the kidneys.
- IgAV primarily affects **small vessels** and is not associated with **asthma**, **eosinophilia**, or the specific neurological and skin manifestations seen in this patient.
Small vessel vasculitis US Medical PG Question 2: A 50-year-old woman comes to the emergency department because of fever and productive cough with blood in the sputum for 1 day. She also reports a sharp pain under her ribs that is worsened on taking deep breaths. Over the past 2 years, she has had repeated episodes of sinusitis, for which she used over the counter medication. She has recently started a new job at a wire-mesh factory. Her temperature is 38.3°C (100.9 °F), pulse is 72/min, respirations are 16/min, and blood pressure is 120/80 mm Hg. Physical examination shows palpable nonblanching skin lesions over her hands and feet. Examination of the nasal cavity shows ulcerations of the nasopharyngeal mucosa and a small septal perforation. Pulmonary examination shows stridor on inspiration. Laboratory studies show:
Hemoglobin 13.2 g/dL
Leukocyte count 10,300/mm3
Platelet count 205,000/mm3
Serum
Urea nitrogen 24 mg/dL
Creatinine 2.4 mg/dL
Urine
Protein 2+
RBC 70/hpf
RBC casts numerous
WBC 1–2/hpf
A chest x-ray shows multiple cavitating, nodular lesions bilaterally. Which of the following additional findings is most likely to be present in this patient?
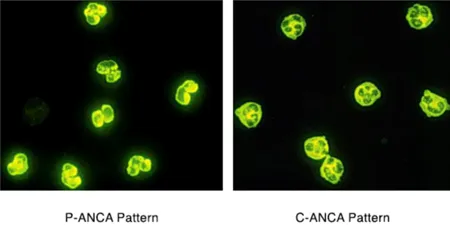
- A. Increased p-ANCA titers
- B. Increased anti-Smith titers
- C. Increased anti-GBM titers
- D. Increased c-ANCA titers (Correct Answer)
- E. Decreased ADAMTS13 activity
Small vessel vasculitis Explanation: ### ***Increased c-ANCA titers***
- The patient's presentation with **sinusitis**, **nasal ulcerations**, **pulmonary cavitating nodules** with hemoptysis, and **rapidly progressive glomerulonephritis** (elevated creatinine, proteinuria, RBC casts) is highly indicative of **Granulomatosis with Polyangiitis (GPA)**.
- **c-ANCA (cytoplasmic antineutrophil cytoplasmic antibodies)**, primarily targeting **proteinase 3 (PR3)**, are serological markers commonly elevated in GPA and help confirm the diagnosis.
### *Increased p-ANCA titers*
- **p-ANCA (perinuclear antineutrophil cytoplasmic antibodies)**, typically targeting **myeloperoxidase (MPO)**, are more commonly associated with **microscopic polyangiitis** or **eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome)**.
- While both GPA and microscopic polyangiitis can present with kidney and lung involvement, the prominent upper airway disease (sinusitis, nasal ulcerations, septal perforation) in this patient points more strongly towards GPA and c-ANCA positivity.
### *Increased anti-Smith titers*
- **Anti-Smith antibodies** are highly specific for **Systemic Lupus Erythematosus (SLE)**.
- The clinical presentation of **upper airway destruction**, **cavitating lung lesions**, and **glomerulonephritis with RBC casts** is not typical for SLE, which more commonly presents with malar rash, arthritis, serositis, and other systemic symptoms.
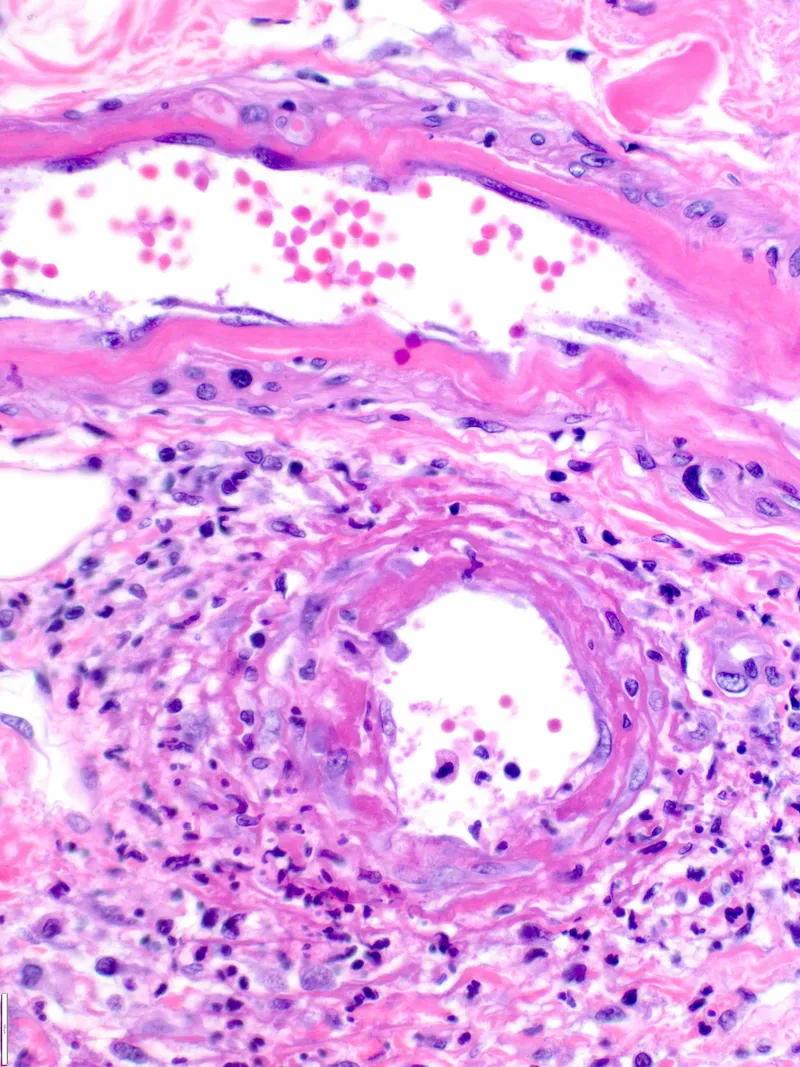
### *Increased anti-GBM titers*
- **Anti-GBM (anti-glomerular basement membrane) antibodies** are characteristic of **Goodpasture syndrome**, which causes a **rapidly progressive glomerulonephritis** and often **pulmonary hemorrhage**.
- However, Goodpasture syndrome does not typically involve **upper airway disease** (sinusitis, nasal ulcerations, septal perforation) or **palpable skin lesions**, which are prominent features in this patient.
### *Decreased ADAMTS13 activity*
- **Decreased ADAMTS13 activity** is diagnostic of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is characterized by the pentad of **thrombocytopenia**, **microangiopathic hemolytic anemia**, **neurological symptoms**, **renal insufficiency**, and **fever**, but it does not involve the prominent **destructive upper airway disease** or **cavitating lung lesions** seen in this patient.
Small vessel vasculitis US Medical PG Question 3: A 50-year-old man comes to the physician for the evaluation of recurrent episodes of chest pain, difficulty breathing, and rapid heart beating over the past two months. During this period, he has had a 4-kg (8.8-lb) weight loss, malaise, pain in both knees, and diffuse muscle pain. Five years ago, he was diagnosed with chronic hepatitis B infection and was started on tenofovir. His temperature is 38°C (100.4°F), pulse is 110/min, and blood pressure is 150/90 mm Hg. Cardiopulmonary examination shows no abnormalities except for tachycardia. There are several ulcerations around the ankle and calves bilaterally. Laboratory studies show:
Hemoglobin 11 g/dL
Leukocyte count 14,000/mm3
Erythrocyte sedimentation rate 80 mm/h
Serum
Perinuclear anti-neutrophil cytoplasmic antibodies negative
Hepatitis B surface antigen positive
Urine
Protein +2
RBC 6-7/hpf
Which of the following is the most likely diagnosis?
- A. Granulomatosis with polyangiitis
- B. Giant cell arteritis
- C. Thromboangiitis obliterans
- D. Polyarteritis nodosa (Correct Answer)
- E. Takayasu arteritis
Small vessel vasculitis Explanation: ***Polyarteritis nodosa (PAN)***
- This patient presents with **fever**, **weight loss**, **myalgia**, and **arthralgia** along with **skin ulcerations** and **renal involvement** (proteinuria, hematuria), signs of systemic inflammation, and **medium-sized vessel vasculitis**. The history of **chronic Hepatitis B infection** is strongly associated with PAN.
- The elevated **ESR** and **leukocytosis** indicate ongoing inflammation, and the chest pain/rapid heart beating could be signs of cardiac involvement, which is common in PAN. The negative p-ANCA also helps rule out other vasculitides.
*Granulomatosis with polyangiitis*
- This condition is typically associated with **upper and lower respiratory tract involvement**, **glomerulonephritis**, and **c-ANCA positivity** (anti-PR3 antibodies).
- The patient's symptoms do not primarily involve sinusitis, pulmonary nodules, or other upper/lower airway disease, and p-ANCA is negative, rather than c-ANCA positive.
*Giant cell arteritis*
- This is a vasculitis affecting primarily **large-sized arteries**, especially the carotid artery branches, and typically occurs in patients **older than 50 years** (though this patient is 50, other symptoms rule it out).
- Key symptoms include **new-onset headache**, **jaw claudication**, **scalp tenderness**, and potential vision loss, none of which are reported here.
*Thromboangiitis obliterans*
- This condition is strongly linked to **heavy tobacco use** and results in **segmental thrombosis and inflammation of small and medium-sized arteries and veins** in the extremities.
- It primarily causes **ischemia of the digits** (fingers and toes), leading to pain, ulcerations, and gangrene, which is not fully consistent with the patient's widespread systemic symptoms and organ involvement.
*Takayasu arteritis*
- This is a **large-vessel vasculitis** primarily affecting the **aorta and its major branches**, typically seen in **younger women**.
- Symptoms often include **claudication**, **absent or diminished pulses**, and **discrepancies in blood pressure between limbs**, which are not described in this patient.
Small vessel vasculitis US Medical PG Question 4: A 27-year-old male presents to clinic complaining of coughing up small amounts of blood daily for the past week. He denies smoking, sick contacts, or recent travel. Chest radiographs demonstrates interstitial pneumonia with patchy alveolar infiltrates suggestive of multiple bleeding sites. Urinalysis is positive for blood and protein. A positive result is returned for anti-glomerular basement membrane antibody (anti-GBM Ab). What is the most likely diagnosis?
- A. Granulomatosis with polyangiitis (Wegener's)
- B. Goodpasture disease (Correct Answer)
- C. Microscopic polyangiitis
- D. Churg-Strauss syndrome
- E. Systemic lupus erythematosus (SLE)
Small vessel vasculitis Explanation: **Goodpasture disease**
- The presence of **hemoptysis** (coughing up blood), **interstitial pneumonia** with alveolar infiltrates, **hematuria**, **proteinuria**, and a positive **anti-glomerular basement membrane (anti-GBM) antibody** is classic for Goodpasture disease.
- This condition involves an **autoimmune attack** against type IV collagen in the basement membranes of the **kidneys** and **lungs**.
*Granulomatosis with polyangiitis (Wegener's)*
- While it can cause **pulmonary-renal syndrome**, it is typically associated with **anti-neutrophil cytoplasmic antibodies (ANCA)**, specifically c-ANCA, not anti-GBM antibodies.
- It often presents with involvement of the **upper respiratory tract** (e.g., sinusitis, otitis media), which is not mentioned in this case.
*Microscopic polyangiitis*
- This is another ANCA-associated vasculitis (p-ANCA predominant) that can cause **pulmonary-renal syndrome**.
- However, it does **not involve granuloma formation** and is not characterized by anti-GBM antibodies.
*Churg-Strauss syndrome*
- This condition, now known as **Eosinophilic Granulomatosis with Polyangiitis (EGPA)**, is characterized by **asthma**, **eosinophilia**, and **granulomatous inflammation**.
- It is also ANCA-associated (p-ANCA in about 50% of cases) and does not typically involve anti-GBM antibodies.
*Systemic lupus erythematosus (SLE)*
- SLE can cause **renal involvement** (lupus nephritis) and **pulmonary manifestations** (e.g., hemorrhage, pneumonitis).
- However, it is characterized by the presence of various autoantibodies like **anti-nuclear antibodies (ANA)**, anti-dsDNA, and anti-Sm, not anti-GBM antibodies.
Small vessel vasculitis US Medical PG Question 5: A 45-year-old man comes to the physician because of fatigue and joint pain for 8 months. He has pain in both knees, both elbows, and diffuse muscle pain. He does not have dyspnea. He also had several episodes of a nonpruritic rash on his lower extremities. Eight years ago, the patient was diagnosed with hepatitis C. His temperature is 37.9°C (100.2°F), pulse is 90/min, and blood pressure is 140/90 mm Hg. Examination of the lower extremities shows raised purple papules that do not blanch when pressure is applied. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.9 g/dL
Leukocyte count 8,500/mm3
Platelets 160,000/mm3
Serum
Creatinine 1.1 mg/dL
ALT 123 U/L
AST 113 U/L
Further evaluation of this patient is most likely to show which of the following findings?
- A. Elevated IgA in serum
- B. Granulomatous inflammation of vessels
- C. Hypocomplementemia (Correct Answer)
- D. Elevated perinuclear anti-neutrophil cytoplasmic antibodies
- E. Positive pathergy test
Small vessel vasculitis Explanation: ***Hypocomplementemia***
- The patient's history of **hepatitis C** infection, along with **fatigue, polyarthralgia, elevated liver enzymes, and palpable purpura**, is classic for **HCV-associated mixed cryoglobulinemia syndrome**.
- **Mixed cryoglobulinemia** (types II and III) involves immune complex deposition, which activates and consumes complement, leading to **low C3 and C4 levels** (hypocomplementemia).
- **Hypocomplementemia** is a hallmark laboratory finding and helps distinguish cryoglobulinemic vasculitis from other small vessel vasculitides.
*Elevated IgA in serum*
- Elevated IgA levels are characteristic of **IgA vasculitis (Henoch-Schönlein purpura)**, which typically affects children and presents with palpable purpura, abdominal pain, and glomerulonephritis.
- While IgA vasculitis can occur in adults, the strong association with **hepatitis C infection** and the typical adult presentation point toward cryoglobulinemia rather than IgA vasculitis.
*Granulomatous inflammation of vessels*
- **Granulomatous inflammation of vessels** is a hallmark of **Granulomatosis with Polyangiitis (GPA)** or **Eosinophilic Granulomatosis with Polyangiitis (EGPA)**.
- These conditions typically present with upper/lower respiratory tract involvement, renal disease, and **ANCA positivity**, not the pattern seen here.
*Elevated perinuclear anti-neutrophil cytoplasmic antibodies*
- **p-ANCA** (perinuclear anti-neutrophil cytoplasmic antibodies) are primarily associated with **microscopic polyangiitis** and **eosinophilic granulomatosis with polyangiitis (EGPA)**.
- The clinical picture of **HCV-associated mixed cryoglobulinemia** does not typically involve ANCA positivity; instead, **rheumatoid factor** and **cryoglobulins** would be the relevant serologic markers.
*Positive pathergy test*
- A **positive pathergy test** is characteristic of **Behçet's disease**, an inflammatory disorder causing recurrent oral and genital ulcers, skin lesions, and uveitis.
- This condition does not align with the patient's presentation of palpable purpura, polyarthralgia, and HCV-associated systemic symptoms.
Small vessel vasculitis US Medical PG Question 6: A 30-year-old woman presents to the clinic because of fever, joint pain, and a rash on her lower extremities. She admits to intravenous drug use. Physical examination reveals palpable petechiae and purpura on her lower extremities. Laboratory results reveal a negative antinuclear antibody, positive rheumatoid factor, and positive serum cryoglobulins. Which of the following underlying conditions in this patient is responsible for these findings?
- A. Dermatomyositis
- B. Systemic lupus erythematosus (SLE)
- C. Hepatitis C infection (Correct Answer)
- D. HIV infection
- E. Hepatitis B infection
Small vessel vasculitis Explanation: ***Hepatitis C infection***
- The combination of **intravenous drug use**, **fever**, **joint pain**, **palpable purpura**, **positive rheumatoid factor**, and **positive serum cryoglobulins** is highly suggestive of **mixed cryoglobulinemia**, which is most commonly associated with chronic **Hepatitis C virus (HCV) infection**.
- **Cryoglobulinemia** is a systemic vasculitis caused by immune complex deposition, a common extrahepatic manifestation of HCV.
*Dermatomyositis*
- Characterized by **proximal muscle weakness** and characteristic skin rashes (e.g., **Gottron's papules**, **heliotrope rash**), which are not described here.
- While dermatomyositis can be associated with inflammatory markers, it typically does not present with palpable purpura or positive cryoglobulins.
*Systemic lupus erythematosus (SLE)*
- While SLE can cause **fever**, **arthralgia**, and a **rash**, the patient's **negative antinuclear antibody (ANA)** makes SLE highly unlikely.
- **Cryoglobulinemia** is rare in SLE, and the specific finding of palpable purpura points away from typical SLE rashes.
*HIV infection*
- HIV can cause a variety of skin lesions and arthralgias, but **palpable purpura** and **mixed cryoglobulinemia** are not its primary or most common manifestations.
- While **rheumatoid factor** can be positive in HIV, the overall clinical picture strongly favors HCV-associated cryoglobulinemia.
*Hepatitis B infection*
- Hepatitis B can be associated with **vasculitis** (e.g., **polyarteritis nodosa**) and immune complex-mediated disease.
- However, **mixed cryoglobulinemia**, characterized by the specific combination of symptoms and laboratory findings presented, is overwhelmingly more associated with **Hepatitis C** than Hepatitis B.
Small vessel vasculitis US Medical PG Question 7: A 40-year-old woman comes to the emergency department because of difficulty walking for the past 4 hours. She first noticed her symptoms after getting up this morning and her foot dragging while walking. She feels tired. She has a history of chronic sinusitis. Six months ago, she was diagnosed with asthma. Current medications include an albuterol inhaler and inhaled corticosteroids. Her temperature is 38.9°C (102°F), pulse is 80/min, and her blood pressure is 140/90 mm Hg. Auscultation of her lungs shows diffuse wheezing over bilateral lung fields. Physical examination shows tender subcutaneous nodules on the extensor surfaces of the elbows. There are palpable, non-blanching erythematous lesions on both shins. Dorsiflexion of the right foot is impaired. Sensation to pinprick, light touch, and vibration is decreased over the ulnar aspect of the left forearm. Laboratory studies show:
Hemoglobin 11.3 g/dL
Leukocyte count 24,500
Segmented neutrophils 48%
Eosinophils 29%
Lymphocytes 19%
Monocytes 4%
Platelet count 290,000/mm3
Serum
Urea nitrogen 32 mg/dL
Creatinine 1.85 mg/dL
Urine
Blood 2+
Protein 3+
Which of the following is the most likely diagnosis in this patient?
- A. Granulomatosis with polyangiitis
- B. Excessive glucocorticoid use
- C. Goodpasture syndrome
- D. Henoch-Schönlein purpura
- E. Eosinophilic granulomatosis with polyangiitis (Correct Answer)
Small vessel vasculitis Explanation: ***Eosinophilic granulomatosis with polyangiitis (EGPA)***
- This patient presents with a classic triad: **asthma**, **eosinophilia** (29%), and **multisystem vasculitis** as evidenced by mononeuropathy, skin lesions (nodules and palpable purpura), and kidney involvement.
- The history of chronic sinusitis, new-onset foot drop (mononeuropathy), **palpable purpura**, and elevated creatinine with proteinuria strongly point towards EGPA.
*Granulomatosis with polyangiitis (GPA)*
- While GPA can cause sinusitis, kidney disease, and neuropathy, it typically presents with **neutrophilic inflammation** and **c-ANCA** positivity, not prominent eosinophilia or severe asthma.
- Granulomatosis with polyangiitis typically involves the **upper and lower respiratory tracts** and kidneys but lacks the pronounced eosinophilia and severe asthma seen here.
*Excessive glucocorticoid use*
- This condition is associated with Cushingoid features, **osteoporosis**, and immunosuppression, none of which fully explain the patient's acute neurological deficits, eosinophilia, or vasculitic manifestations.
- Although the patient has asthma, her symptoms are not consistent with the side effects of inhaled corticosteroids or chronic systemic glucocorticoid use.
*Goodpasture syndrome*
- Goodpasture syndrome is characterized by **recurrent pulmonary hemorrhage** and rapidly progressive **glomerulonephritis** due to anti-GBM antibodies.
- It does not explain the prominent eosinophilia, asthma, or the presence of subcutaneous nodules and palpable purpura.
*Henoch-Schönlein purpura (HSP)*
- HSP typically presents in children with **palpable purpura** on the buttocks and lower extremities, **arthralgias**, abdominal pain, and **IgA nephropathy**.
- It does not involve significant eosinophilia, severe asthma, or mononeuropathy as seen in this adult patient.
Small vessel vasculitis US Medical PG Question 8: A 27-year-old man presents to his primary care physician with worsening cough and asthma. The patient reports that he was in his usual state of health until 1 month ago, when he developed a cold. Since then his cold has improved, but he continues to have a cough and worsening asthma symptoms. He says that he has been using his rescue inhaler 3 times a day with little improvement. He is studying for an accounting exam and states that his asthma is keeping him up at night and making it hard for him to focus during the day. The patient admits to smoking tobacco. His smoking has increased from a half pack per day since he was 17 years old to 1 pack per day during the past month to cope with the stress of his exam. The patient's temperature is 99°F (37.2°C), blood pressure is 110/74 mmHg, pulse is 75/min, and respirations are 15/min with an oxygen saturation of 97% on room air. Physical examination is notable for mild expiratory wheezes bilaterally. Labs are obtained, as shown below:
Serum:
Na+: 144 mEq/L
Cl-: 95 mEq/L
K+: 4.3 mEq/L
HCO3-: 23 mEq/L
Urea nitrogen: 24 mg/dL
Glucose: 100 mg/dL
Creatinine: 1.6 mg/dL
Leukocyte count and differential:
Leukocyte count: 13,000/mm^3
Segmented neutrophils: 63%
Eosinophils: 15%
Basophils: < 1%
Lymphocytes: 20%
Monocytes: 1.3%
Hemoglobin: 13.5 g/dL
Hematocrit: 50%
Platelets: 200,000/mm^3
Urinalysis reveals proteinuria and microscopic hematuria. Which of the following is associated with the patient's most likely diagnosis?
- A. IgA deposits
- B. Smoking
- C. c-ANCA levels
- D. Hepatitis B surface antigen
- E. p-ANCA levels (Correct Answer)
Small vessel vasculitis Explanation: ***p-ANCA levels***
- The patient presents with asthma, sinusitis-like symptoms (prior cold followed by worsening cough/asthma), eosinophilia (15%), and renal involvement (proteinuria, hematuria, elevated creatinine). This constellation of symptoms is highly suggestive of **Eosinophilic Granulomatosis with Polyangiitis (EGPA)**, formerly known as Churg-Strauss Syndrome.
- Approximately 30-40% of EGPA patients are positive for **p-ANCA (anti-myeloperoxidase antibodies)**, which are associated with the vasculitic phase and renal involvement.
*IgA deposits*
- **IgA deposits** are characteristic of **IgA nephropathy (Berger's disease)** or **Henoch-Schönlein purpura** (now IgA vasculitis), which typically present with hematuria and proteinuria, sometimes after an upper respiratory infection.
- However, these conditions do not typically cause severe asthma, significant eosinophilia, or a systemic vasculitis picture with pulmonary involvement as seen in this patient.
*Smoking*
- While the patient is a smoker and smoking can exacerbate asthma and contribute to chronic lung disease, it is not an *associated factor* with the underlying diagnosis of EGPA itself.
- Smoking is a risk factor for many respiratory illnesses but doesn't specifically point to EGPA in the context of the given clinical and laboratory findings.
*c-ANCA levels*
- **c-ANCA (anti-proteinase 3 antibodies)** are primarily associated with **Granulomatosis with Polyangiitis (GPA)**, formerly Wegener's granulomatosis.
- While GPA can present with kidney involvement and pulmonary symptoms, it typically involves the upper airways (sinusitis, otitis), lungs, and kidneys, but is usually *not* associated with severe asthma or prominent eosinophilia, which are key features in this patient.
*Hepatitis B surface antigen*
- **Hepatitis B surface antigen** positivity is associated with **polyarteritis nodosa (PAN)** due to immune complex deposition.
- PAN is a necrotizing vasculitis that can affect multiple organs but typically spare the lungs and is not associated with asthma or eosinophilia.
Small vessel vasculitis US Medical PG Question 9: A 57-year-old woman presents to her family physician because of sinusitis and nasal drainage for 3 months. The nasal drainage is purulent and occasionally hemorrhagic. She has only temporary improvement after trying multiple over the counter medications. Over the last 2 weeks, she also has fatigue and joint pain, mainly affecting the ankles, knees, and wrists. Vital signs include: temperature 36.9°C (98.4°F), blood pressure 142/91 mm Hg, and pulse 82/min. On examination, there is inflammation and bleeding of the nasal mucosa, along with tenderness to percussion over the maxillary sinuses. Urine dipstick reveals 4+ microscopic hematuria and 2+ proteinuria. Which of the following is the most likely diagnosis?
- A. Granulomatosis with polyangiitis (Correct Answer)
- B. Polyarteritis nodosa
- C. Churg-Strauss syndrome
- D. Immunoglobulin A nephropathy
- E. Sarcoidosis
Small vessel vasculitis Explanation: ***Granulomatosis with polyangiitis***
- This patient presents with **upper airway inflammation** (chronic sinusitis, hemorrhagic purulent nasal drainage, inflamed nasal mucosa), **joint pain**, and **renal involvement** (hematuria, proteinuria), which are classic features of granulomatosis with polyangiitis (GPA), formerly known as Wegener's granulomatosis.
- GPA is a **small vessel vasculitis** often associated with **ANCA** (specifically PR3-ANCA/c-ANCA) and characterized by granulomatous inflammation of the respiratory tract and glomerulonephritis.
*Polyarteritis nodosa*
- **Polyarteritis nodosa (PAN)** typically involves **medium-sized arteries** and presents with systemic symptoms, but it **spares the lungs** and **kidneys initially**, unlike the prominent renal and upper respiratory manifestations seen here.
- PAN is **not associated with ANCA** and does not typically involve the upper respiratory tract with granulomatous inflammation.
*Churg-Strauss syndrome*
- Also known as **Eosinophilic Granulomatosis with Polyangiitis (EGPA)**, this condition is characterized by **asthma**, **eosinophilia**, and **allergic rhinitis**, which are not the primary features in this patient.
- While it can involve the upper respiratory tract and kidneys, the absence of **asthma** and **high eosinophil count** makes it less likely.
*Immunoglobulin A nephropathy*
- This is a **primary glomerular disease** characterized by **IgA deposition** in the mesangium, presenting often with recurrent macroscopic hematuria following an upper respiratory or gastrointestinal infection.
- It does **not cause systemic vasculitis** with prominent upper airway inflammation, granulomas, or destructive sinusitis.
*Sarcoidosis*
- **Sarcoidosis** is a multi-system granulomatous disease, often affecting the lungs and lymph nodes, and sometimes the skin, eyes, and joints.
- While it can cause some nasal symptoms, it generally **does not cause destructive sinonasal disease** with purulent and hemorrhagic drainage or severe glomerulonephritis with 4+ hematuria, and it is **not a vasculitis**.
Small vessel vasculitis US Medical PG Question 10: A 62-year-old man presents to the emergency department with hematuria and hemoptysis that started in the morning. He notes that he has had frequent lung infections throughout his adult life, the most recent being 2 weeks ago. He also mentions that he has had hematuria twice before but never as severe as he is having currently. His medical history is otherwise non-significant, and his only medication is acetaminophen as needed. His blood pressure is 136/92 mm Hg, heart rate is 86/min, respiratory rate is 16/min, and temperature is 37.0°C (98.6°F). Chest radiography shows a resolving right middle lobe airspace opacity. His initial laboratory tests are notable for elevated erythrocyte sedimentation rate and C-reactive protein level. While in the examination room, the patient develops a spontaneous nosebleed. What is the most likely diagnosis?
- A. Goodpasture syndrome
- B. IgA nephropathy
- C. Minimal change disease
- D. Post-streptococcal glomerulonephritis
- E. Granulomatosis with polyangiitis (Correct Answer)
Small vessel vasculitis Explanation: ***Granulomatosis with polyangiitis***
- This patient presents with a **triad of upper airway (nosebleed), lower airway (hemoptysis, recurrent lung infections), and renal involvement (hematuria)**, which is classic for granulomatosis with polyangiitis (GPA), a form of ANCA-associated vasculitis.
- The elevated **ESR and CRP** indicate systemic inflammation, which is common in vasculitic conditions.
*Goodpasture syndrome*
- Characterized by **glomerulonephritis and pulmonary hemorrhage (hemoptysis)**, but typically does not involve the upper airways (e.g., nosebleeds).
- Diagnosis is confirmed by the presence of **anti-glomerular basement membrane antibodies**, which often presents more acutely.
*IgA nephropathy*
- Often presents with **recurrent episodes of gross hematuria**, frequently following an upper respiratory tract infection.
- While it involves the kidneys, it **does not typically cause pulmonary or upper airway symptoms** such as hemoptysis or recurrent lung opacities.
*Minimal change disease*
- Characterized by **nephrotic syndrome (proteinuria, hypoalbuminemia, edema)** and rarely presents with hematuria.
- **Does not cause pulmonary or upper airway manifestations** like hemoptysis or nosebleeds.
*Post-streptococcal glomerulonephritis*
- Typically occurs **1-3 weeks after a streptococcal infection** and presents with acute nephritic syndrome (hematuria, proteinuria, edema, hypertension).
- **Does not involve recurrent lung infections or hemoptysis** and is less likely in an adult with recurrent hematuria episodes.
More Small vessel vasculitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.