Seronegative spondyloarthropathies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Seronegative spondyloarthropathies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Seronegative spondyloarthropathies US Medical PG Question 1: A 23-year-old man comes to the physician for frequent and painful urination. He has also had progressive painful swelling of his right knee over the past week. He is sexually active with two female partners and uses condoms inconsistently. His mother has an autoimmune disease that involves a malar rash. Examination shows conjunctivitis bilaterally. The right knee is warm, erythematous, and tender to touch; range of motion is limited. Laboratory studies show an erythrocyte sedimentation rate of 62 mm/h. Urinalysis shows WBCs. Further evaluation of this patient is most likely to reveal which of the following?
- A. Hiking trip two months ago
- B. Recent norovirus gastroenteritis
- C. Chondrocalcinosis of the left knee
- D. Positive anti-dsDNA antibodies
- E. HLA-B27 positive genotype (Correct Answer)
Seronegative spondyloarthropathies Explanation: ***HLA-B27 positive genotype***
- The patient's symptoms (urethritis, conjunctivitis, and arthritis) constitute the classic triad of **Reiter's syndrome**, a form of **reactive arthritis**.
- **Reactive arthritis** is strongly associated with the **HLA-B27 genotype**, which is found in a significant majority of affected individuals.
*Hiking trip two months ago*
- This information is vague and does not directly link to a specific pathogen or trigger for reactive arthritis.
- While some bacterial infections can be acquired through environmental exposure, there is no direct evidence provided in the stem to support a connection.
*Recent norovirus gastroenteritis*
- **Norovirus** typically causes acute, self-limiting gastroenteritis and is not commonly associated with the development of **reactive arthritis**.
- Reactive arthritis is primarily triggered by certain **genitourinary** or **gastrointestinal bacterial infections** (e.g., Chlamydia, Shigella, Salmonella, Campylobacter).
*Chondrocalcinosis of the left knee*
- **Chondrocalcinosis** (calcium pyrophosphate deposition disease or pseudogout) primarily affects older individuals and typically presents with acute, severe arthritis.
- While it can affect the knee, it is not consistently associated with the extra-articular manifestations (urethritis, conjunctivitis) seen in this patient, and its etiology is distinct from reactive arthritis.
*Positive anti-dsDNA antibodies*
- **Positive anti-dsDNA antibodies** are a hallmark of **systemic lupus erythematosus (SLE)**, an autoimmune disease.
- While SLE can cause arthritis and sometimes conjunctivitis, it does not typically cause urethritis in the manner described, nor does it fit the overall clinical picture as well as reactive arthritis.
Seronegative spondyloarthropathies US Medical PG Question 2: A 26-year-old woman presents with sudden-onset pain in her lower back. She says she was exercising in the gym several hours ago when she felt a sharp pain. The pain is radiating down the side of her leg and into her foot. On physical exam, her vital signs are as follows: HR 95, BP 120/70, T 37.2 degrees C. She has extreme pain shooting down her leg with a straight leg raise. Her sensation to light touch and pin-prick is intact throughout. Which of the following is the most likely diagnosis?
- A. Cauda equina syndrome
- B. Ankylosing spondylitis
- C. Osteomyelitis
- D. Spinal stenosis
- E. Disc herniation (Correct Answer)
Seronegative spondyloarthropathies Explanation: ***Disc herniation***
- The sudden onset of **sharp back pain** radiating down the leg (**radiculopathy**) after physical exertion, coupled with a positive **straight leg raise test**, is highly indicative of a disc herniation.
- Radiating pain suggests nerve root compression, and the straight leg raise test stretches the sciatic nerve, aggravating the pain in cases of disc herniation.
*Cauda equina syndrome*
- This is a neurological emergency characterized by **saddle anesthesia**, bowel or bladder dysfunction, and progressive motor weakness in both legs.
- These severe neurological deficits are not present in the patient's presentation; sensation is intact, and no mention of bowel/bladder issues.
*Ankylosing spondylitis*
- Typically presents with **chronic inflammatory back pain** that improves with exercise and worsens with rest, often in younger males.
- It is a systemic inflammatory condition, and the acute, exertion-related onset of pain with radiculopathy described here is not characteristic.
*Osteomyelitis*
- This is an **infection of the bone**, usually accompanied by fever, localized tenderness, and systemic signs of infection.
- The patient's vital signs are stable, and there is no indication of infection, making osteomyelitis less likely.
*Spinal stenosis*
- Characterized by **neurogenic claudication**, where leg pain and numbness worsen with walking and improve with sitting or leaning forward.
- The acute onset of pain after an intense activity and the presence of a positive straight leg raise are not typical features of spinal stenosis.
Seronegative spondyloarthropathies US Medical PG Question 3: A 27-year-old male presents to his primary care physician complaining of pain with urination and eye redness. He reports that he developed these symptoms approximately one week ago. He also has noticed left knee and right heel pain that started a few days ago. He denies any recent trauma. He had an episode of abdominal pain and diarrhea ten days ago that resolved. He has otherwise felt well. On exam, he walks with a limp and his conjunctivae are erythematous. Laboratory findings are notable for an elevated erythrocyte sedimentation rate (ESR) and elevated C-reactive protein (CRP). Which of the following is most likely associated with this patient’s condition?
- A. Anti-centromere antibody
- B. HLA-B27 haplotype (Correct Answer)
- C. Anti-cyclic citrullinated peptide (anti-CCP) antibody
- D. HLA-DR4 haplotype
- E. Rheumatoid factor
Seronegative spondyloarthropathies Explanation: ***HLA-B27 haplotype***
- The patient presents with symptoms of **urethritis** (pain with urination), **conjunctivitis** (eye redness), and **arthritis** (knee and heel pain), which is the classic triad of **Reactive Arthritis**
- **Reactive arthritis** is strongly associated with the presence of the **HLA-B27 haplotype**, especially following gastrointestinal or genitourinary infections.
*Anti-centromere antibody*
- This antibody is associated with **limited cutaneous systemic sclerosis** (CREST syndrome) characterized by calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasias.
- The patient's symptoms do not align with systemic sclerosis.
*Anti-cyclic citrullinated peptide (anti-CCP) antibody*
- **Anti-CCP antibodies** are highly specific for **rheumatoid arthritis**, which primarily affects the small joints of the hands and feet symmetrically and does not typically present with conjunctivitis or urethritis.
- The patient's presentation with an acute, asymmetric arthritis following an infection is not consistent with rheumatoid arthritis.
*HLA-DR4 haplotype*
- The **HLA-DR4 haplotype** is primarily associated with **rheumatoid arthritis**, a chronic inflammatory autoimmune disease that differs significantly in presentation from the patient's acute symptoms.
- This patient's symptoms are more indicative of a seronegative spondyloarthropathy, not rheumatoid arthritis.
*Rheumatoid factor*
- **Rheumatoid factor (RF)** is an autoantibody found in many patients with **rheumatoid arthritis**, but it is also present in other conditions and can be negative in some RA cases.
- While it indicates systemic inflammation, it is not specific to the patient's constellation of symptoms, which point more directly to a reactive process.
Seronegative spondyloarthropathies US Medical PG Question 4: A 22-year-old man comes to the physician for a follow-up evaluation for chronic lower back pain. He has back stiffness that lasts all morning and slowly improves throughout the day. He has tried multiple over-the-counter medications, including ibuprofen, without any improvement in his symptoms. Physical examination shows tenderness over the iliac crest bilaterally and limited range of motion of the lumbar spine with forward flexion. The results of HLA-B27 testing are positive. An x-ray of the lumbar spine shows fusion of the lumbar vertebrae and sacroiliac joints. The physician plans to prescribe a new medication but first orders a tuberculin skin test to assess for the risk of latent tuberculosis reactivation. Inhibition of which of the following is the most likely primary mechanism of action of this drug?
- A. mTOR kinase
- B. Calcineurin
- C. NF-κB
- D. Inosine monophosphate dehydrogenase
- E. TNF-α (Correct Answer)
Seronegative spondyloarthropathies Explanation: **TNF-α**
- The clinical presentation with **chronic lower back pain**, morning stiffness, **limited lumbar spine range of motion**, positive **HLA-B27**, and **fusion of lumbar vertebrae and sacroiliac joints** is highly suggestive of **ankylosing spondylitis**.
- Biologic medications, specifically **TNF-α inhibitors**, are a cornerstone of treatment for ankylosing spondylitis, especially when conventional therapies like NSAIDs fail. The mention of screening for latent tuberculosis reactivation strongly points to the use of a TNF-α inhibitor, as these drugs increase the risk of TB reactivation.
*mTOR kinase*
- **mTOR inhibitors** (e.g., sirolimus, everolimus) are primarily used as **immunosuppressants** in organ transplantation and in some cancers.
- They are not a first-line or common treatment for ankylosing spondylitis or other spondyloarthropathies.
*Calcineurin*
- **Calcineurin inhibitors** (e.g., cyclosporine, tacrolimus) are potent **immunosuppressants** used in transplant rejection prevention and some autoimmune diseases.
- While they can have immunosuppressive effects, they are not the primary target for the treatment of ankylosing spondylitis.
*NF-κB*
- **NF-κB** is a crucial transcription factor involved in inflammation and immune responses. While relevant to inflammatory conditions, directly targeting NF-κB is not the primary mechanism of action for the most effective biologic therapies used in ankylosing spondylitis.
- **Glucocorticoids** can inhibit NF-κB, but they are not the main long-term treatment for ankylosing spondylitis, and the context points to a biologic.
*Inosine monophosphate dehydrogenase*
- **Inosine monophosphate dehydrogenase (IMPDH) inhibitors** (e.g., mycophenolate mofetil) block purine synthesis, thus inhibiting lymphocyte proliferation.
- These drugs are used in **transplantation** and some **autoimmune diseases** (e.g., lupus, vasculitis) but are not typically used for ankylosing spondylitis.
Seronegative spondyloarthropathies US Medical PG Question 5: A 42-year-old man presents to clinic complaining of increasing difficulty climbing stairs and standing up from sitting in his chair. On exam you perceive his strength to be 5/5 distally, but only 3/5 in proximal muscle groups bilaterally. There is a distinctive rash on his upper eyelids and around his eyes. Examination of the fingers is most likely to reveal which of the following?
- A. Enlargement of the PIP
- B. Ulnar deviation of the fingers
- C. Dactylitis
- D. Violaceous papules over the MCP and PIP joints (Correct Answer)
- E. Nail pitting with oil spots
Seronegative spondyloarthropathies Explanation: ***Violaceous papules over the MCP and PIP joints***
- The patient's symptoms of **proximal muscle weakness** and characteristic rash (rash on upper eyelids, i.e., **heliotrope rash**) are highly suggestive of **dermatomyositis**.
- **Gottron's papules**, which are violaceous papules over the **extensor surfaces** of the **metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints**, are a **pathognomonic cutaneous finding** in dermatomyositis.
- These lesions may also appear over the elbows and knees, and occasionally over the distal interphalangeal (DIP) joints, but MCP and PIP involvement is most characteristic.
*Enlargement of the PIP*
- **Enlargement of the proximal interphalangeal (PIP) joints** is more characteristic of **osteoarthritis** (Bouchard's nodes) or **rheumatoid arthritis**, which typically presents with symmetric joint involvement and different cutaneous manifestations.
- This finding does not align with the patient's pattern of proximal muscle weakness and distinctive rash.
*Ulnar deviation of the fingers*
- **Ulnar deviation of the fingers** is a classic deformity seen in advanced **rheumatoid arthritis**, which primarily affects joints symmetrically and is not associated with the proximal muscle weakness and specific facial rash described.
- The patient's symptoms point away from an inflammatory arthropathy like rheumatoid arthritis.
*Dactylitis*
- **Dactylitis** (swelling of an entire digit, giving a **"sausage digit"** appearance) is characteristic of **psoriatic arthritis** or **spondyloarthropathies** (such as reactive arthritis or ankylosing spondylitis).
- It is not a feature of dermatomyositis and does not fit the overall clinical picture of proximal muscle weakness and heliotrope rash.
*Nail pitting with oil spots*
- **Nail pitting** and **oil spots** (yellow-brown discoloration under the nail) are characteristic dermatological manifestations of **psoriasis** and **psoriatic arthritis**.
- These findings are not associated with dermatomyositis, whose dermatological features include Gottron's papules and heliotrope rash.
Seronegative spondyloarthropathies US Medical PG Question 6: A 42-year-old woman comes to the physician because of stiffness and pain in multiple joints. She says that the fingers on both of her hands have become increasingly stiff and difficult to move over the past 8 months. She also complains of nails that break easily and look spotty as well as chronic back pain. She had a urinary tract infection a year ago that was treated with antibiotics. She is sexually active with 2 male partners and uses condoms inconsistently. Her vitals are within normal limits. A photograph of her right hand is shown. There are multiple, well-demarcated red plaques with silvery-white scales over the shins and back. Serum studies show a negative rheumatoid factor and ANA. Which of the following is the most likely diagnosis?
- A. Rheumatoid arthritis
- B. Secondary syphilis
- C. Psoriatic arthritis (Correct Answer)
- D. Systemic lupus erythematosus
- E. Ankylosing spondylitis
Seronegative spondyloarthropathies Explanation: ***Psoriatic arthritis***
- The patient presents with **polyarticular joint pain and stiffness**, particularly in the hands, along with characteristic **nail changes** (onycholysis, pitting) and **psoriasis** (red plaques with silvery scales on shins and back).
- The **negative rheumatoid factor (RF)** and **ANA** help rule out rheumatoid arthritis and systemic lupus erythematosus, respectively, making psoriatic arthritis the most likely diagnosis given the constellation of skin, nail, and joint findings.
*Rheumatoid arthritis*
- While it causes polyarticular joint pain and stiffness, **rheumatoid arthritis typically presents with symmetric synovitis**, often spares the distal interphalangeal joints, and is frequently associated with a **positive rheumatoid factor** or anti-CCP antibodies.
- The presence of **psoriatic skin lesions** and nail changes, and a **negative RF**, make this diagnosis less likely.
*Secondary syphilis*
- Secondary syphilis can present with various skin manifestations and arthralgia, but it rarely causes the **erosive arthritis of the small joints** or the specific **nail changes** seen in psoriatic arthritis.
- The patient's history of inconsistent condom use is a risk factor, however, the specific clinical findings point away from syphilis.
*Systemic lupus erythematosus*
- This condition can cause **polyarthralgia/arthritis** and **skin rashes**, but the characteristic scaly plaques on the shins and back, and the **specific nail involvement** (onycholysis, pitting), are not typical features.
- A **negative ANA** also makes systemic lupus erythematosus an unlikely diagnosis.
*Ankylosing spondylitis*
- While **ankylosing spondylitis** can cause chronic back pain and stiffness, it primarily affects the **axial skeleton** (spine and sacroiliac joints) and typically presents with inflammatory back pain that improves with activity.
- It does not usually involve peripheral joints with the mentioned **nail changes** or **psoriatic skin lesions**.
Seronegative spondyloarthropathies US Medical PG Question 7: A 22-year-old woman presents to the emergency department with a 3-day history of fever and abdominal pain. She says that the pain is located in the left lower quadrant of the abdomen and feels crampy in nature. The pain has been associated with bloody diarrhea and joint tenderness. She has no past medical history but says that she returned 2 weeks ago from vacation in Asia where she tried many new foods. Her family history is significant for multiple cancers in close relatives. Physical exam reveals swollen ulcers on her legs, and colonoscopy reveals contiguous ulcerations from the rectum through the descending colon. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Noncaseating granulomas
- B. Severe aortic stenosis
- C. Gram-negative rod
- D. HLA-DQ2 positivity
- E. Perinuclear anti-neutrophil cytoplasmic antibodies (Correct Answer)
Seronegative spondyloarthropathies Explanation: ***Perinuclear anti-neutrophil cytoplasmic antibodies***
- The patient's presentation with **bloody diarrhea**, low-grade fever, **crampy abdominal pain**, joint tenderness, and contiguous ulcerations in the colon is highly suggestive of **ulcerative colitis**.
- **Perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA)** are found in 50-70% of patients with ulcerative colitis and are associated with a more extensive disease.
*Noncaseating granulomas*
- **Noncaseating granulomas** are a characteristic histological finding in **Crohn's disease**, not ulcerative colitis.
- Crohn's disease typically presents with **skip lesions**, **transmural inflammation**, and affects any part of the GI tract, often with perianal disease.
*Severe aortic stenosis*
- **Severe aortic stenosis** is a condition of the heart valves that can lead to symptoms like chest pain, syncope, and heart failure, and is not directly associated with the patient's gastrointestinal and systemic symptoms.
- While inflammatory conditions can rarely have cardiac manifestations, there's no direct link between aortic stenosis and inflammatory bowel disease in this context.
*Gram-negative rod*
- While infections, especially from **Gram-negative rods** like *Shigella* or *Salmonella*, can cause acute bloody diarrhea, the 3-day history with joint tenderness and contiguous ulcers on colonoscopy points more towards an inflammatory bowel disease.
- The chronicity and systemic involvement are less typical for an acute bacterial enteritis, although such infections might trigger IBD.
*HLA-DQ2 positivity*
- **HLA-DQ2 positivity** is strongly associated with **celiac disease**, an immune-mediated enteropathy triggered by gluten.
- Celiac disease typically presents with malabsorption symptoms like fatty stools, weight loss, and iron deficiency, rather than bloody diarrhea and contiguous colonic ulcerations.
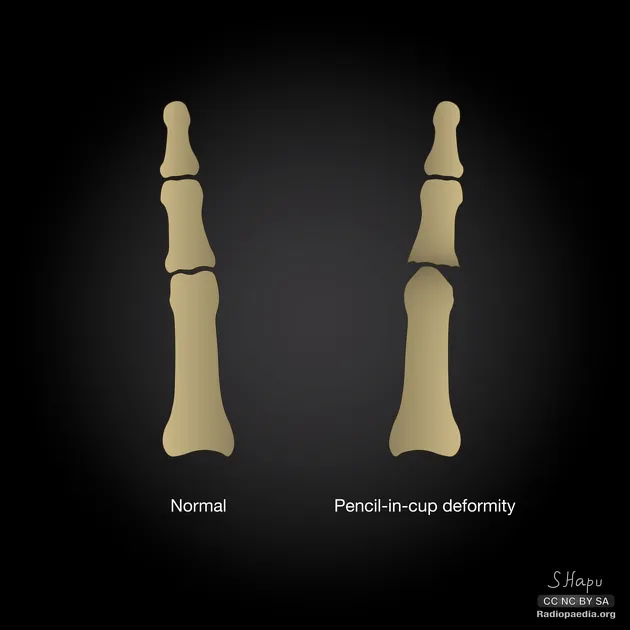
Seronegative spondyloarthropathies US Medical PG Question 8: A 47-year-old man presents to his primary care physician complaining of pain and stiffness in his right index finger and left knee. The past medical history is remarkable for severe dandruff and an episode of apparent gout in the left 1st toe 6 months ago, which never resolved. The physical examination confirms dactylitis of the right index finger and several toes, as well as synovitis of the left knee. He is also noted to have pitting of his fingernails. Plain X-rays of his hand reveal erosions in the distal interphalangeal (DIP) joint and periarticular new bone formation. Which of the following is most consistent with these findings?
- A. Psoriatic arthritis (Correct Answer)
- B. Pseudogout
- C. Osteoarthritis
- D. Reactive arthritis
- E. Rheumatoid arthritis
Seronegative spondyloarthropathies Explanation: ***Psoriatic arthritis***
- The constellation of **dactylitis**, **nail pitting**, involvement of both **DIP joints** with erosions, and a history of **psoriasis** (severe dandruff) is highly characteristic of psoriatic arthritis.
- The previous episode resembling gout and synovitis of the knee are also consistent, as psoriatic arthritis can mimic other arthropathies and affect various joints.
*Pseudogout*
- This condition is caused by **calcium pyrophosphate dihydrate crystal deposition** and typically presents as acute, severe joint pain, often in larger joints like the knee or wrist, but without dermatological or nail changes.
- While it can cause synovitis, it does not typically involve dactylitis, DIP erosions, nail pitting, or a history of psoriasis.
*Osteoarthritis*
- Characterized by **cartilage degeneration** and **new bone formation** (osteophytes), often in weight-bearing joints or DIP/PIP joints, but typically without the marked inflammatory signs like dactylitis or nail changes.
- While X-rays can show new bone formation, the presence of dactylitis, nail pitting, and psoriasis history rule out uncomplicated osteoarthritis.
*Reactive arthritis*
- This is an **acute, inflammatory arthropathy** that typically develops after a genitourinary or gastrointestinal infection.
- While it can present with dactylitis and oligoarthritis, it does not involve nail pitting or a history of psoriasis, and the initial trigger infection is usually identifiable.
*Rheumatoid arthritis*
- This is a **chronic autoimmune disease** primarily affecting smaller joints symmetrically, particularly the MCP and PIP joints, but typically sparing the DIP joints.
- It is not associated with psoriasis, nail pitting, and usually presents with periarticular osteopenia rather than significant new bone formation on X-ray.
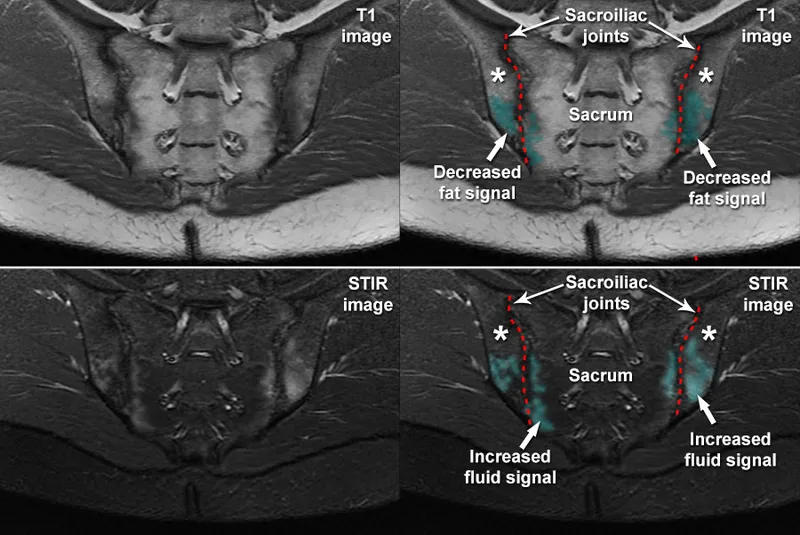
Seronegative spondyloarthropathies US Medical PG Question 9: A 32-year-old woman comes to her physician because of increasing back pain for the past 10 months. The pain is worse in the morning when she wakes up and improves with activity. She used to practice yoga, but stopped 5 months ago as bending forward became increasingly difficult. She has also had bilateral hip pain for the past 4 months. She has not had any change in urination. She has celiac disease and eats a gluten-free diet. Her temperature is 37.1°C (98.8°F), pulse is 65/min, respirations are 13/min, and blood pressure is 116/72 mmHg. Examination shows the range of spinal flexion is limited. Flexion, abduction, and external rotation of bilateral hips produces pain. An x-ray of her pelvis is shown. Further evaluation of this patient is likely to show which of the following?
- A. High levels of creatine phosphokinase
- B. High levels of rheumatoid factor
- C. HLA-B27 positive genotype (Correct Answer)
- D. Presence of anti-dsDNA antibodies
- E. Presence of anti-Ro and anti-La antibodies
Seronegative spondyloarthropathies Explanation: ***HLA-B27 positive genotype***
- The patient's symptoms of **inflammatory back pain** (worse in the morning, improves with activity, limited spinal flexion, bilateral hip pain) are classic for **spondyloarthritis**, particularly **ankylosing spondylitis**.
- **HLA-B27** is strongly associated with ankylosing spondylitis and other spondyloarthropathies, making its presence highly likely in this clinical scenario.
*High levels of creatine phosphokinase*
- Elevated **creatine phosphokinase (CPK)** levels typically indicate **muscle damage** or inflammation, as seen in conditions like myositis.
- While back pain can have a muscular component, her symptoms are more indicative of inflammatory arthritis of the spine and hips, not primary muscle inflammation.
*High levels of rheumatoid factor*
- **Rheumatoid factor (RF)** is a key marker for **rheumatoid arthritis**, which primarily affects peripheral joints in a symmetrical pattern, not typically the axial skeleton in this manner.
- The patient's presentation with **inflammatory back pain** and hip involvement is inconsistent with typical rheumatoid arthritis.
*Presence of anti-dsDNA antibodies*
- **Anti-dsDNA antibodies** are highly specific for **systemic lupus erythematosus (SLE)**, a systemic autoimmune disease with diverse manifestations.
- While SLE can cause arthralgia or arthritis, her specific pattern of inflammatory back pain and hip involvement is not characteristic of SLE.
*Presence of anti-Ro and anti-La antibodies*
- **Anti-Ro (SSA)** and **anti-La (SSB) antibodies** are primarily associated with **Sjögren's syndrome**, an autoimmune disease causing dry eyes and mouth.
- They can also be present in SLE, but again, the patient's presentation is more specific for a spondyloarthropathy than for Sjögren's or SLE.
Seronegative spondyloarthropathies US Medical PG Question 10: A 32-year-old man presents to his physician with a complaint of pain with urination that has developed and persisted over the past 8 days. Upon awakening today, he also noted a clear discharge from his urethra. The patient states he is otherwise healthy. Social history is notable for the patient working at a local farm with livestock. Review of systems is notable for left knee and ankle pain for the past week and worsening of his seasonal allergies with red and itchy eyes. His temperature is 97.7°F (36.5°C), blood pressure is 122/83 mmHg, pulse is 89/min, respirations are 14/min, and oxygen saturation is 98% on room air. Which of the following is likely to be positive in this patient?
- A. p-ANCA
- B. HLA-B27 (Correct Answer)
- C. Anti-dsDNA
- D. Anti-CCP
- E. HLA-DR4
Seronegative spondyloarthropathies Explanation: ***HLA-B27***
- The patient presents with a classic triad of symptoms: **urethritis** (painful urination, clear discharge), **arthritis** (left knee and ankle pain), and **conjunctivitis** (red and itchy eyes), which is highly suggestive of **reactive arthritis**.
- **Reactive arthritis** is strongly associated with the presence of the **HLA-B27** allele, found in 30-50% to up to 80% of patients depending on the population.
*p-ANCA*
- **p-ANCA (perinuclear anti-neutrophil cytoplasmic antibodies)** are typically associated with certain **vasculitides** like microscopic polyangiitis or eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome).
- Symptoms of **vasculitis** such as constitutional symptoms, organ damage, or purpuric rash are not described in this patient's presentation.
*Anti-dsDNA*
- **Anti-double-stranded DNA (anti-dsDNA) antibodies** are a highly specific marker for **systemic lupus erythematosus (SLE)**.
- The patient's symptoms (urethritis, arthritis, conjunctivitis) are not typical for a primary presentation of SLE, which often involves skin rashes, serositis, and renal or hematological manifestations.
*Anti-CCP*
- **Anti-cyclic citrullinated peptide (anti-CCP) antibodies** are a specific and sensitive marker for **rheumatoid arthritis (RA)**.
- While the patient has arthritis, the accompanying conjunctivitis and urethritis are not characteristic features of RA, and RA typically presents with symmetrical polyarthritis.
*HLA-DR4*
- **HLA-DR4** is a genetic marker strongly associated with **rheumatoid arthritis (RA)**, particularly in certain ethnic groups.
- As with anti-CCP antibodies, the overall clinical picture, including urethritis and conjunctivitis, makes RA an unlikely primary diagnosis.
More Seronegative spondyloarthropathies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.