Rheumatoid arthritis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Rheumatoid arthritis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Rheumatoid arthritis US Medical PG Question 1: A 23-year-old man complains of lower back pain that began approximately 6 months ago. He is unsure why he is experiencing this pain and notices that this pain is worse in the morning after waking up and improves with physical activity. Ibuprofen provides significant relief. He denies bowel and bladder incontinence or erectile dysfunction. Physical exam is notable for decreased chest expansion, decreased spinal range of motion, 5/5 strength in both lower extremities, 2+ patellar reflexes bilaterally, and an absence of saddle anesthesia. Which of the following is the most appropriate next test for this patient?
- A. HLA-B27
- B. Slit-lamp examination
- C. MRI sacroiliac joint
- D. Radiograph sacroiliac joint (Correct Answer)
- E. ESR
Rheumatoid arthritis Explanation: **Radiograph sacroiliac joint**
- Plain **radiographs of the sacroiliac (SI) joints** are typically the **initial imaging modality** for suspected **ankylosing spondylitis** due to affordability and diagnostic value.
- They can reveal characteristic changes such as **sacroiliitis (joint erosion, sclerosis, fusion)**, which are common in early-stage disease.
*HLA-B27*
- While a **positive HLA-B27** is associated with ankylosing spondylitis, it is **not diagnostic** on its own, as many HLA-B27 positive individuals never develop the disease.
- Its use is more in **confirming suspicion** or in cases where imaging is equivocal, but it's not the primary diagnostic test.
*Slit-lamp examination*
- A slit-lamp examination is used to detect **uveitis**, which can be an **extra-articular manifestation** of ankylosing spondylitis.
- However, it is not a primary diagnostic test for the condition itself, and its utility arises once the diagnosis is strongly considered or established.
*MRI sacroiliac joint*
- **MRI of the sacroiliac (SI) joints** is more sensitive than radiographs for detecting **early inflammatory changes** (e.g., bone marrow edema) that may not be visible on plain films.
- However, given the duration of symptoms (6 months) and the characteristic inflammatory back pain, **radiographs are typically the first-line imaging** due to cost-effectiveness, reserving MRI for cases with normal radiographs but high clinical suspicion.
*ESR*
- **Erythrocyte sedimentation rate (ESR)** is a **non-specific marker of inflammation** and can be elevated in various inflammatory conditions, including ankylosing spondylitis.
- It is not diagnostic for ankylosing spondylitis and cannot differentiate it from other inflammatory or infectious conditions.
Rheumatoid arthritis US Medical PG Question 2: A 46-year-old woman comes to the physician with a 4-month history of lethargy. She has had joint pain for the past 15 years and does not have a primary care physician. Her temperature is 37.4°C (99.3°F), pulse is 97/min, and blood pressure is 132/86 mm Hg. Physical examination shows pallor of the oral mucosa and nontender subcutaneous nodules on both elbows. The distal interphalangeal joints of both hands are flexed and the proximal interphalangeal joints appear hyperextended. Range of motion in the fingers is restricted. The liver span is 6 cm and the spleen tip is palpated 4 cm below the left costal margin. Laboratory studies show:
Hematocrit 33%
Leukocyte count 1,800/mm3
Segmented neutrophils 35%
Lymphocytes 60%
Platelet count 130,000/mm3
Increased serum titers of which of the following is most specific for this patient's condition?
- A. Anti-U1-RNP antibody
- B. Rheumatoid factor
- C. Antinuclear antibody
- D. Anti-CCP antibody (Correct Answer)
- E. Anti-Sm antibody
Rheumatoid arthritis Explanation: ***Anti-CCP antibody***
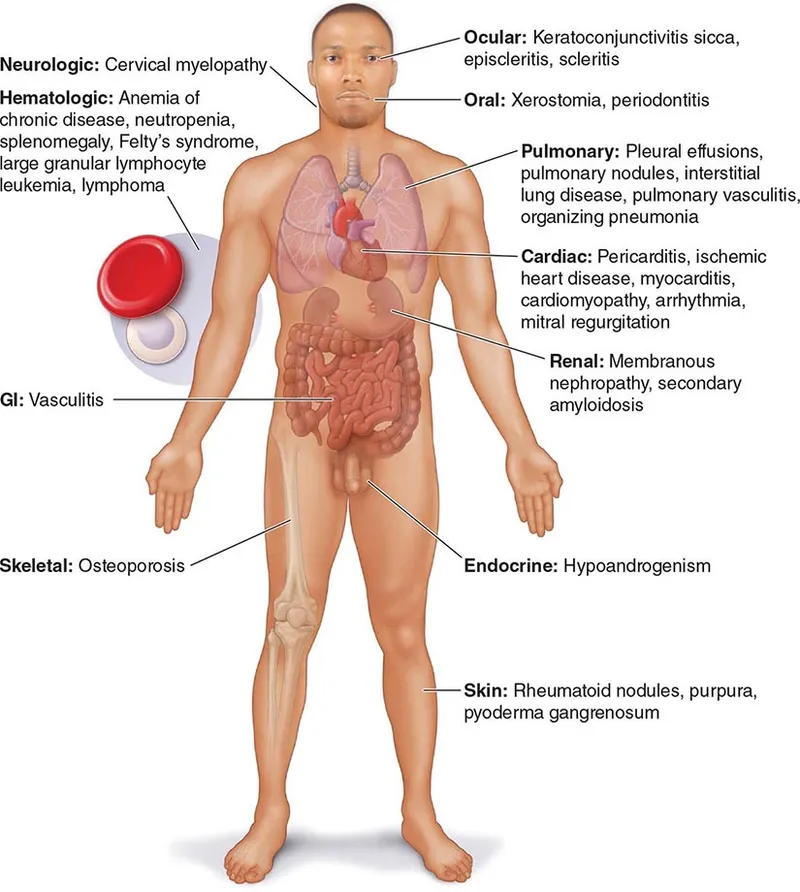
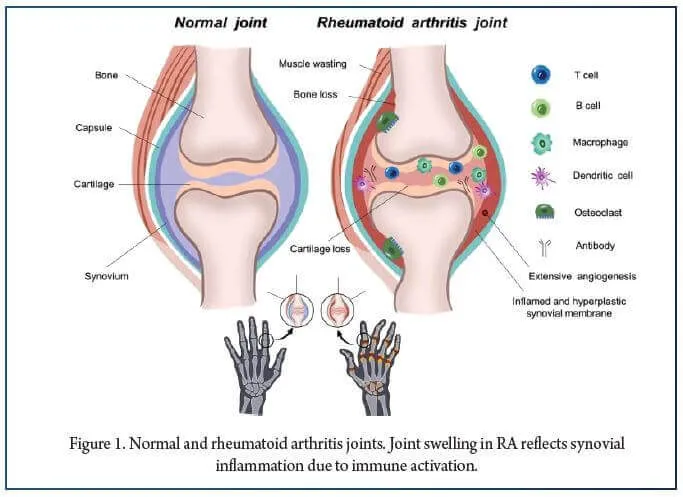
- The patient's presentation with **long-standing joint pain**, **nodules**, specific finger deformities (**swan neck deformity** - PIP hyperextension with DIP flexion), **splenomegaly**, and **pancytopenia** (WBC 1,800/mm³, platelets 130,000/mm³, hematocrit 33%) is highly suggestive of **Felty's syndrome**, a severe complication of **rheumatoid arthritis (RA)**.
- **Anti-CCP antibodies** are highly specific for RA (over 95% specificity) and can be present years before symptoms develop, making them the most specific marker for this condition.
*Anti-U1-RNP antibody*
- This antibody is characteristic of **mixed connective tissue disease (MCTD)**, which presents with overlapping features of SLE, systemic sclerosis, and polymyositis.
- While joint pain can occur in MCTD, the classic deformities, nodule presence, and specific hematologic findings (leukopenia, thrombocytopenia, anemia) better align with Felty's syndrome due to rheumatoid arthritis.
*Rheumatoid factor*
- **Rheumatoid factor (RF)** is positive in about 80% of RA patients, but it is less specific than anti-CCP antibodies as it can be elevated in other autoimmune diseases, chronic infections, and even in healthy individuals.
- While likely positive in this patient, its lower specificity means it's not the *most* specific marker compared to anti-CCP antibodies.
*Antinuclear antibody*
- **Antinuclear antibody (ANA)** is a screening test for various autoimmune diseases, particularly **systemic lupus erythematosus (SLE)**, and is positive in many systemic autoimmune conditions.
- Its high sensitivity but low specificity (positive in other conditions and even in 5-10% of the healthy population) means it is not the most specific marker for this patient's condition.
*Anti-Sm antibody*
- **Anti-Smith (Sm) antibody** is highly specific for **systemic lupus erythematosus (SLE)**.
- The patient's clinical picture, particularly the long history of joint pain with specific deformities and subcutaneous nodules, is not typical for SLE, making anti-Sm antibody an unlikely specific finding.
Rheumatoid arthritis US Medical PG Question 3: A 53-year-old woman presents to her primary care physician with complaints of pain and swelling in her hands and fingers. She states that she has had these symptoms since she was in her 20s, but they have recently become more severe. She states that her wedding ring no longer fits, due to increased swelling of her fingers. She is a 30-pack-year smoker with a body mass index (BMI) of 31 kg/m2. The vital signs include: blood pressure 122/78 mm Hg, heart rate 72/min, and respiratory rate 15/min. On physical exam, a mild systolic murmur is heard over the apex, and her lungs are clear bilaterally. There is swelling of all the digits bilaterally, and a yellow-white plaque is noted beneath 3 of her nail beds. When asked about the plaques, she states that she was given itraconazole for them about 3 weeks ago; however, the plaques did not resolve. When asked further about joint pain, she notes that she has had shoulder and knee pain for the last several years, although she has not sought medical care for this. Which of the following is the best initial step in this patient’s therapeutic management?
- A. Administer methotrexate
- B. Administer indomethacin
- C. Administer indomethacin and methotrexate (Correct Answer)
- D. Administer sulfasalazine
- E. Administer indomethacin and sulfasalazine
Rheumatoid arthritis Explanation: ***Administer indomethacin and methotrexate***
- This patient presents with symptoms highly suggestive of **psoriatic arthritis**, including typical joint pain distribution (hands, fingers, shoulders, knees), **dactylitis** (swelling of all digits causing the wedding ring to no longer fit), and **nail lesions** (yellow-white plaques unresponsive to antifungals).
- Given the patient's severe and chronic symptoms, a **combination of a non-steroidal anti-inflammatory drug (NSAID) like indomethacin for symptomatic relief and a disease-modifying anti-rheumatic drug (DMARD) like methotrexate** is the most appropriate initial therapy to control inflammation and prevent joint damage.
*Administer methotrexate*
- While **methotrexate** is a cornerstone DMARD for psoriatic arthritis, it takes several weeks to exert its full therapeutic effects.
- Administering methotrexate alone would not provide immediate relief for the patient's significant pain and swelling.
*Administer indomethacin*
- **Indomethacin**, an NSAID, would provide symptomatic relief from pain and inflammation.
- However, NSAIDs alone do not modify the disease course or prevent joint damage in psoriatic arthritis; therefore, it is an insufficient long-term monotherapy.
*Administer sulfasalazine*
- **Sulfasalazine** is an alternative DMARD used in psoriatic arthritis, often considered for patients who cannot tolerate methotrexate or for milder forms, especially with peripheral arthritis.
- However, for a patient with severe, chronic, and potentially erosive disease suggested by long-standing symptoms and diffuse dactylitis, **methotrexate is generally preferred due to its stronger efficacy profile** as an initial DMARD for psoriatic arthritis if no contraindications exist.
*Administer indomethacin and sulfasalazine*
- This combination provides short-term symptomatic relief (indomethacin) and long-term disease modification (sulfasalazine).
- While a valid option, **methotrexate is generally considered the first-line DMARD for psoriatic arthritis**, especially in severe cases, due to its greater efficacy in controlling both skin and joint manifestations compared to sulfasalazine.
Rheumatoid arthritis US Medical PG Question 4: A 29-year-old woman presents to the emergency department with joint pain and a notable rash. She has had joint pain for the past 12 months but noticed the rash recently as well as generalized malaise. She states her joint pain is symmetric, in her upper extremities, and is worse in the morning. Her temperature is 97.6°F (36.4°C), blood pressure is 111/74 mmHg, pulse is 83/min, respirations are 14/min, and oxygen saturation is 98% on room air. Laboratory studies are ordered as seen below.
Hemoglobin: 10 g/dL
Hematocrit: 30%
Leukocyte count: 6,800/mm^3 with normal differential
Platelet count: 207,000/mm^3
Serum:
Na+: 140 mEq/L
Cl-: 101 mEq/L
K+: 4.9 mEq/L
HCO3-: 21 mEq/L
BUN: 30 mg/dL
Glucose: 120 mg/dL
Creatinine: 1.8 mg/dL
The patient is ultimately admitted to the hospital. Which of the following is the most appropriate test to monitor her disease progression?
- A. Rheumatoid factor
- B. Anti-topoisomerase
- C. Anti-dsDNA (Correct Answer)
- D. Anti-CCP
- E. Anti-nuclear antibody
Rheumatoid arthritis Explanation: ***Anti-dsDNA***
- The patient's presentation with **symmetric polyarthritis**, a **rash**, and **renal involvement** (elevated BUN and creatinine) is highly suggestive of **Systemic Lupus Erythematosus (SLE)**.
- **Anti-dsDNA antibodies** correlate well with disease activity, especially **lupus nephritis**, making them an excellent marker for monitoring disease progression and response to therapy in SLE.
*Rheumatoid factor*
- **Rheumatoid factor** is primarily associated with **Rheumatoid Arthritis** and is generally not used for monitoring SLE activity.
- While some SLE patients may test positive for RF, it is not a specific marker for SLE.
*Anti-topoisomerase*
- **Anti-topoisomerase I (Scl-70) antibodies** are characteristic of **systemic sclerosis (scleroderma)**, particularly the diffuse cutaneous form.
- This antibody is not typically seen in SLE and does not help monitor its progression.
*Anti-CCP*
- **Anti-cyclic citrullinated peptide (anti-CCP) antibodies** are highly specific for **Rheumatoid Arthritis**.
- They are useful for diagnosis and prognosis in RA but have no role in monitoring SLE.
*Anti-nuclear antibody*
- **Antinuclear antibodies (ANA)** are present in almost all patients with SLE and are essential for diagnosis, but they do not correlate with disease activity.
- A positive ANA test is a screening tool but cannot be used to monitor disease progression or response to treatment.
Rheumatoid arthritis US Medical PG Question 5: A 59-year-old woman comes to the physician because of a 1-year history of pain and stiffness in her fingers and knees. The stiffness lasts for about 10 minutes after she wakes up in the morning. She also reports that her knee pain is worse in the evening. She drinks one glass of wine daily. Her only medication is acetaminophen. She is 175 cm (5 ft 9 in) tall and weighs 102 kg (225 lb); BMI is 33 kg/m2. Physical examination shows firm nodules on the distal interphalangeal joints of the index, ring, and little fingers of both hands. Which of the following is the most likely diagnosis?
- A. Septic arthritis
- B. Pseudogout
- C. Gout
- D. Rheumatoid arthritis
- E. Osteoarthritis (Correct Answer)
Rheumatoid arthritis Explanation: ***Osteoarthritis***
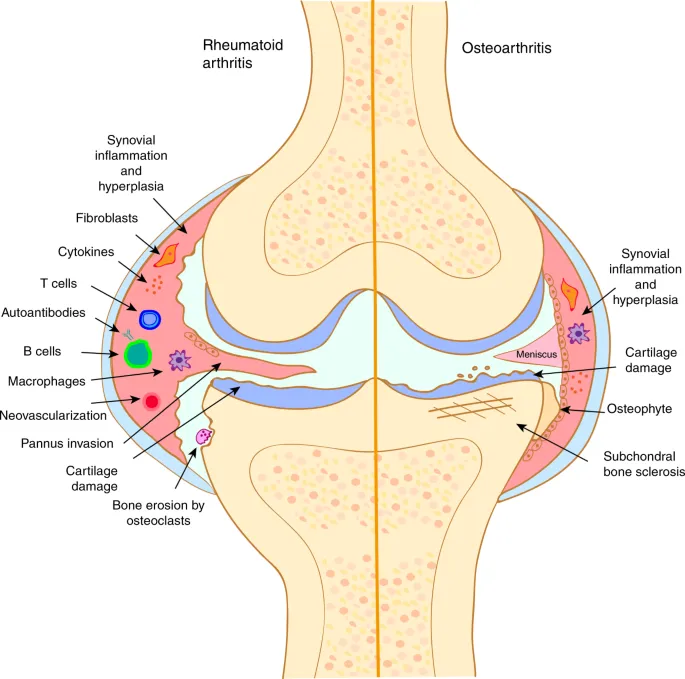
* The patient's age (59 years), obesity (BMI 33 kg/m2), short duration of morning stiffness (10 minutes), evening worsening of knee pain, and the presence of **firm nodules on the distal interphalangeal joints** (Heberden's nodes) are classic signs of **osteoarthritis**.
* This condition is a common **degenerative joint disease** associated with wear and tear, often affecting weight-bearing joints and small joints of the hands.
*Septic arthritis*
* **Septic arthritis** typically presents with an acutely painful, hot, and swollen joint, often with systemic symptoms like fever and chills, which are absent here.
* The chronic, progressive nature of the patient's symptoms and the presence of bony nodules point away from an infectious cause.
*Pseudogout*
* **Pseudogout**, or calcium pyrophosphate deposition disease, involves the deposition of calcium pyrophosphate crystals, leading to episodes of acute, painful arthritis, often in larger joints like the knee.
* While it can affect the knee, the insidious onset, chronic pain, and specific hand nodules seen in this case are not typical features of pseudogout.
*Gout*
* **Gout** is characterized by sudden, severe attacks of pain, redness, and swelling, often affecting a single joint (commonly the great toe) due to **uric acid crystal deposition**.
* The patient's chronic pain pattern, multiple joint involvement (fingers and knees), and the description of firm nodules (not tophi) make gout less likely.
*Rheumatoid arthritis*
* **Rheumatoid arthritis** typically presents with morning stiffness lasting longer than 30 minutes, symmetrical polyarthritis, and often affects the **proximal interphalangeal (PIP)** and **metacarpophalangeal (MCP) joints** of the hands, sparing the DIP joints.
* The patient's short morning stiffness, DIP joint involvement, and the absence of systemic inflammatory signs argue against rheumatoid arthritis.
Rheumatoid arthritis US Medical PG Question 6: A 55-year-old woman presents to the office complaining of leg ulcers for the past 6 months. She has a chronic history of severe rheumatoid arthritis controlled with methotrexate. She does not drink alcohol or smoke cigarettes. Her vitals are normal. Her lungs are clear to auscultation. The abdomen is soft and non-tender with a palpable spleen tip on inspiration. Skin examination shows scattered ulcers on the legs in various stages of healing. Additionally, metacarpophalangeal and proximal interphalangeal joints are tender. Varicose veins are not observed. Laboratory results are as follows:
Hemoglobin 10.5 g/dL
MCV 74 fl
Platelets 226,000/mm3
White blood cells 2500/mm3
Neutrophils 20%
Alanine aminotransferase 36 U/L
Aspartate aminotransferase 39 U/L
Creatinine 1.0 mg/dL
HIV test is negative. Which of the following is the most likely cause of this patient's condition?
- A. Venous stasis and valve insufficiency
- B. Drug toxicity
- C. Caplan syndrome
- D. Vitamin deficiency
- E. Felty syndrome (Correct Answer)
Rheumatoid arthritis Explanation: ***Felty syndrome***
- The patient's presentation with severe, long-standing **rheumatoid arthritis**, **leg ulcers**, **splenomegaly** (palpable spleen tip), and **neutropenia** (WBC 2500, neutrophils 20%) is highly characteristic of **Felty syndrome**.
- **Felty syndrome** is a rare, severe complication of rheumatoid arthritis, defined by the triad of **rheumatoid arthritis, neutropenia, and splenomegaly**. The neutropenia increases susceptibility to infections and can contribute to chronic leg ulcers.
*Venous stasis and valve insufficiency*
- This condition typically presents with **venous stasis ulcers** that are often located in the **gaiter area** (around the ankles) and accompanied by signs of chronic venous insufficiency, such as **edema**, **skin discoloration**, and **varicose veins**, which are noted as absent in this patient.
- It does not explain the patient's systemic symptoms like **splenomegaly** or **neutropenia**.
*Drug toxicity*
- While methotrexate can cause **bone marrow suppression** leading to cytopenias, and liver enzyme elevations, it typically doesn't cause **splenomegaly** or chronic leg ulcers in this specific constellation without other clear signs of severe toxicity.
- The liver enzymes are within normal limits, making significant hepatotoxicity unlikely, and the chronic nature of the leg ulcers along with splenomegaly points away from isolated methotrexate toxicity as the primary cause.
*Caplan syndrome*
- **Caplan syndrome** is characterized by the presence of **pneumoconiosis** (e.g., coal worker's pneumoconiosis) and **rheumatoid arthritis**, resulting in distinctive pulmonary nodules.
- This patient has no history of occupational exposure to dusts and her lungs are clear to auscultation, making **Caplan syndrome** an unlikely diagnosis.
*Vitamin deficiency*
- While certain vitamin deficiencies (e.g., **Vitamin C** causing scurvy) can lead to skin manifestations and impaired wound healing, they do not typically cause the combination of **splenomegaly**, **neutropenia**, and severe leg ulcers in the context of rheumatoid arthritis.
- The specific laboratory findings and the clinical picture are more indicative of a distinct rheumatologic complication.
Rheumatoid arthritis US Medical PG Question 7: A 28-year-old man presents with one week of redness and discharge in his eyes, pain and swelling in his left second and third toes, and rash on the soles of his feet. He is sexually active with multiple partners and uses condoms occasionally. He denies any recent travel or illness and does not take any medications. Review of systems is otherwise unremarkable. On physical exam, he has bilateral conjunctivitis, dactylitis of the left second and third toes, and crusty yellow-brown vesicles on his plantar feet. Complete blood count and chemistries are within normal limits. Erythrocyte sedimentation rate (ESR) is 40 mm/h. Toe radiographs demonstrate soft tissue swelling but no fractures. Which diagnostic test should be performed next?
- A. Rheumatoid factor
- B. Anti-cyclic citrullinated peptide antibody assay
- C. HLA-B27
- D. Nucleic acid amplification testing for Chlamydia trachomatis (Correct Answer)
- E. Antinuclear antibody assay
Rheumatoid arthritis Explanation: ***Nucleic acid amplification testing for Chlamydia trachomatis***
- The patient's symptoms (conjunctivitis, dactylitis, and plantar rash) with a history of unprotected sexual activity are highly suggestive of **reactive arthritis**, often triggered by **Chlamydia trachomatis infection**.
- **NAAT** is the most sensitive and specific test for detecting *Chlamydia trachomatis* in urethral or urine samples, even in asymptomatic infections.
*Rheumatoid factor*
- This test is primarily used for **rheumatoid arthritis**, which typically presents with symmetric polyarthritis, not the asymmetric dactylitis and conjunctivitis seen here.
- The patient’s acute presentation and specific rash are inconsistent with classic rheumatoid arthritis.
*Anti-cyclic citrullinated peptide antibody assay*
- Like rheumatoid factor, this assay is a specific marker for **rheumatoid arthritis** and would not be the most appropriate first step in diagnosing reactive arthritis.
- Its utility in this clinical context is minimal given the patient's symptoms point away from rheumatoid arthritis.
*HLA-B27*
- While **HLA-B27** is associated with reactive arthritis (and other spondyloarthropathies), it is a **genetic predisposition factor**, not a diagnostic test for acute infection.
- A positive result would confirm susceptibility but would not identify the underlying *Chlamydia* infection that needs treatment.
*Antinuclear antibody assay*
- This assay is used to screen for **systemic lupus erythematosus** and other autoimmune connective tissue diseases.
- The patient's acute presentation of conjunctivitis, dactylitis, and plantar rash is not typical for lupus or similar conditions.
Rheumatoid arthritis US Medical PG Question 8: A 34-year-old man with a 2-year history of rheumatoid arthritis is being evaluated on a follow-up visit. He is currently on methotrexate and celecoxib for pain management and has shown a good response until now. However, on this visit, he mentions that the morning stiffness has been getting progressively worse. On physical examination, both his wrists are erythematous and swollen, nodules on his elbows are also noted. Rheumatoid factor is 30 (normal reference values: < 15 IU/mL), ESR is 50 mm/h, anti-citrullinated protein antibodies is 55 (normal reference values: < 20). What is the next best step in the management of this patient?
- A. Sulfasalazine
- B. Adalimumab monotherapy
- C. Methotrexate and Corticosteroids
- D. Methotrexate and Infliximab (Correct Answer)
- E. Infliximab monotherapy
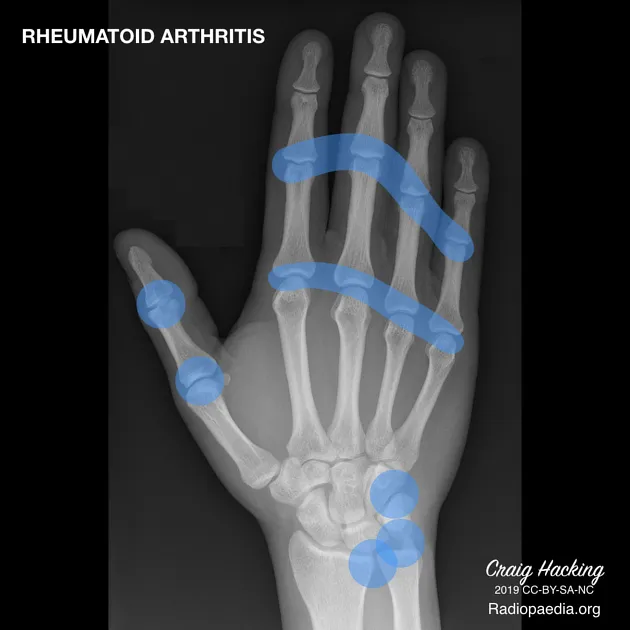
Rheumatoid arthritis Explanation: **Methotrexate and Infliximab**
- The patient is experiencing a **flare-up of rheumatoid arthritis** despite being on methotrexate, indicated by worsening morning stiffness, active synovitis (erythematous and swollen wrists), elevated ESR, and positive rheumatoid factor and anti-CCP. This suggests a need for more aggressive therapy, and adding a **biologic agent like infliximab (an anti-TNF agent)** to methotrexate is a standard approach for moderate to severe RA that is not adequately controlled by methotrexate monotherapy.
- Combination therapy with **methotrexate and a biologic DMARD** (e.g., TNF inhibitors like infliximab) has been shown to be more effective than monotherapy for controlling disease activity and preventing joint damage in refractory RA.
*Sulfasalazine*
- **Sulfasalazine** is a conventional synthetic DMARD that is generally used as a **first-line agent or in combination therapy** for mild to moderate RA.
- Given the patient's ongoing active disease despite methotrexate and the severity of his symptoms, sulfasalazine is unlikely to be sufficient to achieve disease control.
*Adalimumab monotherapy*
- While adalimumab (another anti-TNF biologic) is an effective treatment for RA, **biologic monotherapy is generally less effective** than combination therapy with methotrexate.
- Current guidelines and clinical practice favor combining biologic DMARDs with methotrexate for optimal outcomes in RA management, especially in patients with active disease.
*Methotrexate and Corticosteroids*
- **Corticosteroids** are effective in rapidly reducing inflammation and can be used for **short-term management of RA flares**.
- However, corticosteroids are not recommended for long-term use due to significant side effects and do not address the underlying disease progression as comprehensively as biologic DMARDs in patients refractory to methotrexate.
*Infliximab monotherapy*
- Similar to adalimumab monotherapy, **infliximab is typically more effective when combined with methotrexate**.
- Using infliximab alone would be a less optimal choice for this patient whose disease is clearly not controlled by methotrexate, as it may lead to a suboptimal response and potentially increase the risk of developing anti-drug antibodies.
Rheumatoid arthritis US Medical PG Question 9: A 64-year-old woman presents to the physician with fever and sore throat for 2 days. She was diagnosed with rheumatoid arthritis 15 years ago. She has had several flares necessitating admission to the hospital in recent years. She has developed deformity in her joints despite aggressive therapy. She is a candidate for surgical correction. Her temperature is 38.2°C (100.9°F), and the rest of her vital signs are stable. Physical examination of the hands reveals multiple swan-neck, boutonniere, and Z-line deformities. Ulnar deviation is evident in both hands. She has flat feet. There are 3 firm, nontender nodules palpated around the right elbow and one on the left Achilles tendon. The spleen is palpated 5 cm below the costal margin with a percussion span of 15 cm. Lymphadenopathy is absent on exam. The laboratory test results show:
Hemoglobin 11 g/dL
Mean corpuscular volume 90 μm3
Leukocyte count 3,500/mm3
Segmented neutrophils 20%
Lymphocytes 70%
Platelet count 240,000/mm3
Erythrocyte sedimentation rate 65 mm/hour
Rheumatoid factor 85 IU/mL (Normal: up to 14 IU/mL)
Which of the following is the most likely cause of this patient’s current condition?
- A. Sarcoidosis
- B. Diffuse large B cell lymphoma
- C. Secondary amyloidosis
- D. Felty syndrome (Correct Answer)
- E. T cell large granular lymphocytic leukemia
Rheumatoid arthritis Explanation: ***Felty syndrome***
- This patient presents with a long history of severe, progressive **rheumatoid arthritis (RA)**, characteristic deformities (**swan-neck, boutonniere, Z-line, ulnar deviation**), **splenomegaly**, and **neutropenia** (leukocyte count 3,500/mm3 with 20% neutrophils, meaning an absolute neutrophil count of 700/mm3). This triad defines **Felty syndrome**.
- **Felty syndrome** is a rare, severe complication of chronic RA, often associated with a high **rheumatoid factor (RF)**, and increased risk of infections due to neutropenia.
*Sarcoidosis*
- While sarcoidosis can cause **lymphadenopathy** and occasionally **splenomegaly**, it does not typically present with the specific joint deformities and positive **RF** seen in severe RA.
- The elevated **RF** and characteristic joint changes are not features of sarcoidosis.
*Diffuse large B cell lymphoma*
- This condition can cause **splenomegaly** and systemic symptoms but is not primarily associated with the specific joint deformities and highly positive **RF** characteristic of longstanding, severe **rheumatoid arthritis**.
- While patients with RA have an increased risk of lymphoma, the constellation of neutropenia and splenomegaly in the context of severe RA points more strongly to Felty syndrome.
*Secondary amyloidosis*
- **Secondary amyloidosis** can occur in chronic inflammatory conditions like **rheumatoid arthritis** and can cause **splenomegaly**.
- However, it does not explain the **neutropenia** or the specific pattern of hematologic abnormalities (lymphocytosis with neutropenia) seen in this patient.
*T cell large granular lymphocytic leukemia*
- This leukemia can cause **neutropenia** and **splenomegaly** and is sometimes associated with **rheumatoid arthritis**.
- However, the patient's lymphocyte count is 70% of 3,500, which is 2,450/mm3. While this is absolute lymphocytosis, the diagnosis is confirmed by immunophenotyping to detect abnormal clonal T cells, which is not provided. The classic presentation of severe RA with splenomegaly and neutropenia strongly aligns with Felty syndrome.
Rheumatoid arthritis US Medical PG Question 10: A 33-year-old woman presents to her primary care physician for gradually worsening pain in both wrists that began several months ago. The pain originally did not bother her, but it has recently begun to affect her daily functioning. She states that the early morning stiffness in her hands is severe and has made it difficult to tend to her rose garden. She occasionally takes ibuprofen for the pain, but she says this does not really help. Her medical history is significant for diabetes mellitus and major depressive disorder. She is currently taking insulin, sertraline, and a daily multivitamin. The vital signs include: blood pressure 126/84 mm Hg, heart rate 82/min, and temperature 37.0°C (98.6°F). On physical exam, her wrists and metacarpophalangeal joints are swollen, tender, erythematous, and warm to the touch. There are no nodules or vasculitic lesions. Which of the following antibodies would be most specific to this patient’s condition?
- A. c-ANCA
- B. Anti-Ro
- C. Anti-Scl-70
- D. Anti-cyclic citrullinated peptide (Correct Answer)
- E. Rheumatoid factor
Rheumatoid arthritis Explanation: ***Anti-cyclic citrullinated peptide***
- **Anti-cyclic citrullinated peptide (anti-CCP)** antibodies are highly specific for **rheumatoid arthritis (RA)** and are often present early in the disease course.
- The patient's presentation with **symmetric polyarthritis**, particularly affecting the **wrists and metacarpophalangeal joints**, with severe **morning stiffness**, is classic for RA.
*c-ANCA*
- **c-ANCA (cytoplasmic antineutrophil cytoplasmic antibodies)** are primarily associated with **granulomatosis with polyangiitis (Wegener's)**, a systemic vasculitis.
- This condition typically presents with symptoms such as **upper and lower respiratory tract involvement**, **renal disease**, and constitutional symptoms, which are not described here.
*Anti-Ro*
- **Anti-Ro (SS-A)** antibodies are strongly associated with **Sjögren's syndrome**, a chronic autoimmune disease characterized by dry eyes and mouth, and also with **systemic lupus erythematosus (SLE)**.
- While Sjögren's can present with arthritis, the prominent joint inflammation and morning stiffness described are more characteristic of rheumatoid arthritis.
*Anti-Scl-70*
- **Anti-Scl-70 (anti-topoisomerase I)** antibodies are highly specific for **systemic sclerosis (scleroderma)**, particularly the diffuse cutaneous form.
- Scleroderma presents with **skin thickening**, **Raynaud's phenomenon**, and potential involvement of internal organs like the lungs and esophagus, which are absent in this patient's presentation.
*Rheumatoid factor*
- **Rheumatoid factor (RF)** is often positive in **rheumatoid arthritis**, but it is less specific than anti-CCP antibodies.
- RF can also be elevated in other autoimmune diseases, chronic infections, and even in healthy individuals, making it a less specific diagnostic marker.
More Rheumatoid arthritis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.