Osteoarthritis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Osteoarthritis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Osteoarthritis US Medical PG Question 1: A previously healthy 61-year-old man comes to the physician because of bilateral knee pain for the past year. The pain is worse with movement and is relieved with rest. Physical examination shows crepitus, pain, and decreased range of motion with complete flexion and extension of both knees. There is no warmth, redness, or swelling. X-rays of both knees show irregular joint space narrowing, osteophytes, and subchondral cysts. Which of the following is the most appropriate pharmacotherapy?
- A. Allopurinol
- B. Naproxen (Correct Answer)
- C. Celecoxib
- D. Infliximab
- E. Prednisone
Osteoarthritis Explanation: ***Naproxen***
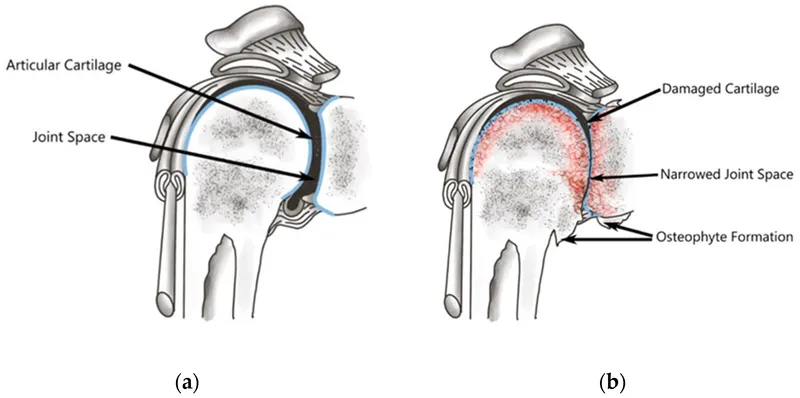
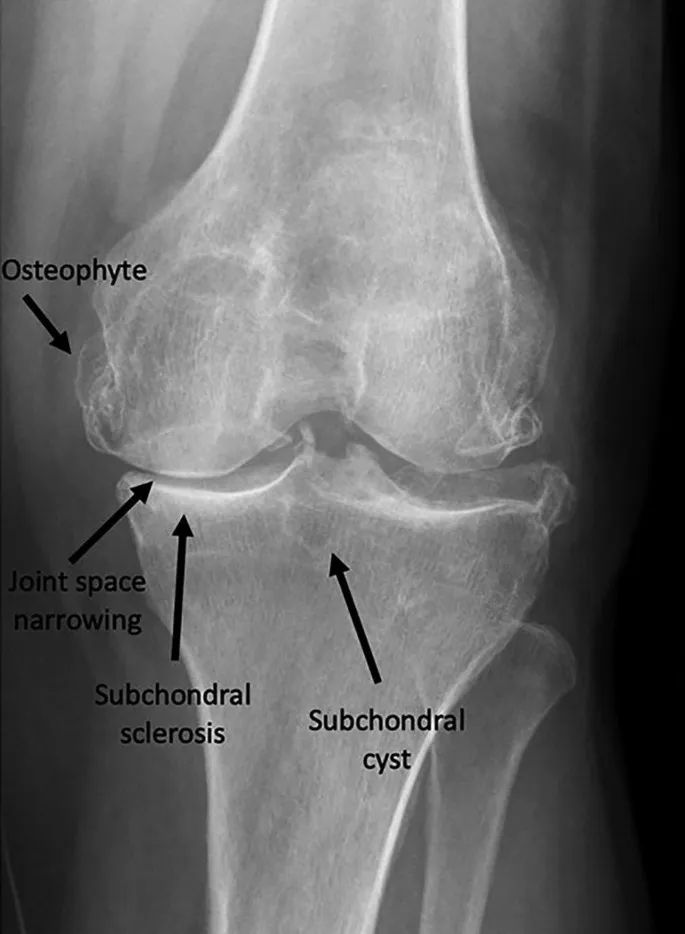
- The patient's presentation with **bilateral knee pain worse with movement**, relief with rest, crepitus, and characteristic X-ray findings (joint space narrowing, osteophytes, subchondral cysts) is classic for **osteoarthritis (OA)** [3].
- **NSAIDs** like naproxen are **first-line pharmacotherapy** for managing pain and inflammation in osteoarthritis that is not adequately controlled by acetaminophen or topical agents [1].
- As a **non-selective NSAID**, naproxen is an appropriate initial choice for a patient without specified risk factors for GI complications or cardiovascular disease [2].
*Allopurinol*
- **Allopurinol** is a xanthine oxidase inhibitor used to reduce **urate production in hyperuricemia** and prevent gout attacks.
- The patient's symptoms are not consistent with gout, as there is **no acute inflammatory arthritis, redness, warmth, or swelling**.
*Celecoxib*
- **Celecoxib** is a **COX-2 selective NSAID** that can be used for osteoarthritis pain.
- It is generally preferred in patients with **documented GI risk factors** (history of peptic ulcer, concurrent anticoagulation, or advanced age with other risk factors).
- While this 61-year-old patient has age as a consideration, in the absence of other specified GI risk factors, either non-selective or COX-2 selective NSAIDs are reasonable; **naproxen is acceptable as initial therapy** and is more cost-effective.
*Infliximab*
- **Infliximab** is a **biologic disease-modifying antirheumatic drug (DMARD)**, specifically a TNF-alpha inhibitor, used to treat inflammatory arthritides like rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
- It is **not indicated for osteoarthritis**, which is a degenerative joint disease rather than an autoimmune inflammatory process.
*Prednisone*
- **Prednisone** is a corticosteroid used to **reduce inflammation** in various conditions, including inflammatory arthritides and acute pain flares.
- While it can provide symptomatic relief, it is **not a first-line or long-term pharmacotherapy for osteoarthritis** due to significant **side effects** with chronic use (weight gain, hyperglycemia, osteoporosis, immunosuppression) [1].
Osteoarthritis US Medical PG Question 2: A 58-year-old woman comes to the physician because of a 2-year history of progressively worsening pain in her knees and fingers. The knee pain is worse when she walks for longer than 30 minutes. When she wakes up in the morning, her fingers and knees are stiff for about 15 minutes. She cannot recall any trauma to the joints. She was treated with amoxicillin following a tick bite 2 years ago. She is otherwise healthy and only takes a multivitamin and occasionally acetaminophen for the pain. She drinks 1–2 glasses of wine daily. She is 160 cm (5 ft 3 in) tall and weighs 79 kg (174 lb); BMI is 31 kg/m2. Her temperature is 36.9°C (98.4°F), pulse is 70/min, and blood pressure is 133/78 mm Hg. Examination of the lower extremities reveals mild genu varum. Range of motion of both knees is limited; there is palpable crepitus. Complete flexion and extension elicit pain. Tender nodules are present on the proximal and distal interphalangeal joints of the index, ring, and little fingers bilaterally. Which of the following is the most likely diagnosis?
- A. Septic arthritis
- B. Lyme arthritis
- C. Gout
- D. Pseudogout
- E. Osteoarthritis (Correct Answer)
Osteoarthritis Explanation: ***Osteoarthritis***
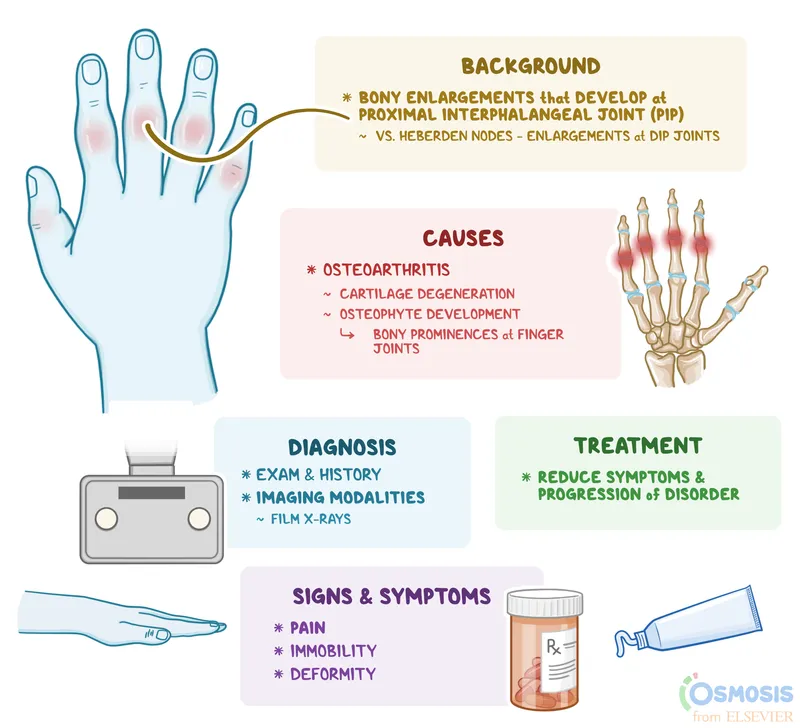
- The patient's presentation with **joint pain worse with activity**, **morning stiffness lasting less than 30 minutes**, **crepitus**, **limited range of motion**, **obesity**, and involvement of **DIP and PIP joints** (Heberden's and Bouchard's nodes) is classic for **osteoarthritis**.
- **Genu varum** (bow-leggedness) is also a common feature of long-standing knee osteoarthritis.
*Septic arthritis*
- Septic arthritis typically presents acutely with **severe, acute pain**, swelling, warmth, and systemic symptoms like **fever and chills**, which are absent here.
- It usually affects a **single joint** and is unlikely to present with chronic, bilateral, and polyarticular involvement over two years.
*Lyme arthritis*
- While the patient had a tick bite and received amoxicillin, **Lyme arthritis** often presents with **monoarticular** or **oligoarticular** large joint involvement, typically the knee, and usually has more significant effusions.
- The chronic, progressive, and polyarticular nature involving DIPs and PIPs, along with short morning stiffness, is not typical for Lyme arthritis.
*Gout*
- Gout typically presents with **acute, excruciating pain** in a single joint (often the **first MTP joint**), intense inflammation, and rapid resolution of attacks.
- The patient's chronic, symmetrical, and progressive pain, and morning stiffness are inconsistent with the typical presentation of gout.
*Pseudogout*
- Pseudogout (calcium pyrophosphate deposition disease) typically presents as **acute attacks** of pain and swelling, often in larger joints like the knee, wrist or shoulder, similar to gout.
- While it can involve multiple joints, the chronic, progressive nature with specific involvement of DIPs and PIPs with osteoarthritic features (crepitus, activity-related pain, short morning stiffness) is more consistent with osteoarthritis.
Osteoarthritis US Medical PG Question 3: A 57-year-old woman presents to her primary care physician with a concern for joint pain. She states that she often feels minor joint pain and morning stiffness in both of her hands every day, particularly in the joints of her fingers. Her symptoms tend to improve as the day goes on and she states they are not impacting the quality of her life. She lives alone as her partner recently died. She smokes 1 pack of cigarettes per day and drinks 2-3 alcoholic drinks per day. Her last menses was at age 45 and she works at a library. The patient has a history of diabetes and chronic kidney disease with her last GFR at 45 mL/min. Her temperature is 97.5°F (36.4°C), blood pressure is 117/58 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical examination is within normal limits. Which of the following interventions is appropriate management of future complications in this patient?
- A. Methotrexate
- B. Ibuprofen
- C. Prednisone
- D. Alendronate (Correct Answer)
- E. Infliximab
Osteoarthritis Explanation: ***Alendronate***
- This patient, a 57-year-old postmenopausal woman with **early menopause (age 45)**, **smoking**, **alcohol use**, and **chronic kidney disease**, is at **significantly increased risk for osteoporosis**. Alendronate, a **bisphosphonate**, is an appropriate intervention to prevent future osteoporotic fractures.
- While her joint pain is likely **osteoarthritis** and currently mild, the question targets **future complication management**, highlighting her significant risk factors for bone density loss.
- Her **GFR of 45 mL/min** (Stage 3a CKD) is at the lower acceptable range for bisphosphonate use; alendronate is generally avoided when GFR < 30-35 mL/min, but can be used with monitoring at GFR 45 mL/min given her high fracture risk.
*Methotrexate*
- Methotrexate is a **disease-modifying antirheumatic drug (DMARD)** typically used for inflammatory arthropathies like **rheumatoid arthritis** or **psoriatic arthritis**.
- The patient's symptoms (mild, improving with activity, no significant exam findings) are not consistent with an inflammatory arthritis requiring methotrexate, and her **chronic kidney disease** makes its use more complex due to renal elimination and toxicity risk.
*Ibuprofen*
- Ibuprofen, a **nonsteroidal anti-inflammatory drug (NSAID)**, could be used for symptomatic relief of her mild osteoarthritis.
- However, the question asks about **"future complications"** and her history of **chronic kidney disease** makes long-term NSAID use potentially harmful due to the risk of worsening renal function and increased cardiovascular risk.
*Prednisone*
- Prednisone is a powerful **corticosteroid** used for acute flares of inflammatory conditions or severe autoimmune diseases.
- Her current joint pain is mild and not indicative of an inflammatory process requiring prednisone; furthermore, long-term corticosteroid use is a significant **risk factor for osteoporosis**, which would worsen her already elevated fracture risk.
*Infliximab*
- Infliximab is a **biologic agent** (TNF-alpha inhibitor) used for severe, refractory inflammatory conditions such as **rheumatoid arthritis**, **ankylosing spondylitis**, or **inflammatory bowel disease**.
- Her symptoms are mild and do not suggest a severe inflammatory arthropathy that would warrant the use of a high-risk biologic medication, which also carries risks like increased infection susceptibility and significant cost.
Osteoarthritis US Medical PG Question 4: A 56-year-old woman with rheumatoid arthritis comes to the physician for a follow-up examination. She has no other history of serious illness. Menopause occurred 1 year ago. Current medications include antirheumatic drugs and hormone replacement therapy. She exercises regularly. A DEXA scan shows a T-score of -1.80, indicating decreased bone density. Which of the following drugs is most likely involved in the pathogenesis of this finding?
- A. Naproxen
- B. Medroxyprogesterone acetate
- C. Adalimumab
- D. Prednisone (Correct Answer)
- E. Sulfasalazine
Osteoarthritis Explanation: ***Prednisone***
- **Glucocorticoids** like prednisone are a major cause of secondary osteoporosis due to their direct inhibitory effects on osteoblast function and promotion of osteoclast activity.
- Long-term use of prednisone, common in managing rheumatoid arthritis, significantly increases the risk of decreased bone density, even with a history of regular exercise and hormone replacement therapy.
*Naproxen*
- **Naproxen** is a **nonsteroidal anti-inflammatory drug (NSAID)** used for pain and inflammation; it does not directly cause bone loss or osteoporosis.
- While it may be used in rheumatoid arthritis, its mechanism of action does not involve bone metabolism.
*Medroxyprogesterone acetate*
- **Medroxyprogesterone acetate (MPA)** is a progestin that can cause **bone mineral density loss** with long-term use, particularly as a contraceptive injection (Depo-Provera).
- However, the patient is on **hormone replacement therapy** (likely estrogen, which is bone-protective) and MPA's effect on bone is generally less significant than that of glucocorticoids in this context, and it's not a typical long-term RA medication.
*Adalimumab*
- **Adalimumab** is a **TNF-alpha inhibitor** used to treat rheumatoid arthritis; it has no known adverse effect on bone density.
- By controlling the inflammatory process in RA, it may indirectly help preserve bone health by reducing inflammation-induced bone erosion.
*Sulfasalazine*
- **Sulfasalazine** is a **disease-modifying antirheumatic drug (DMARD)** used for rheumatoid arthritis and inflammatory bowel disease.
- It does not have any direct adverse effects on bone density or metabolism.
Osteoarthritis US Medical PG Question 5: A 55-year-old man with a BMI of 34 kg/m² presents to his primary care physician for knee pain. The patient has had left knee pain, which has been steadily worsening for the past year. He states that ice and rest has led to minor improvement in his symptoms. He recently bumped his knee; however, he says that it has not altered his baseline pain when ambulating. The patient is a butcher and lives with his wife. His current medications include insulin, metformin, hydrochlorothiazide, and lisinopril. He is attending Alcoholics Anonymous with little success. Physical exam reveals a left knee that is mildly erythematous with some bruising. There is no pain upon palpation of the joint or with passive range of motion. The patient exhibits a mildly antalgic gait. Which of the following is the best initial step in management?
- A. Rest for 1-2 weeks
- B. Colchicine
- C. Aspirin
- D. MRI
- E. Weight loss (Correct Answer)
Osteoarthritis Explanation: ***Weight loss***
- The patient has **obesity (BMI 34 kg/m²)** and several risk factors for **osteoarthritis**, including age (55), chronic knee pain, occupational stress (butcher), and an antalgic gait.
- **Weight reduction** is the most important initial conservative management for osteoarthritis in obese patients, as it significantly reduces mechanical stress on weight-bearing joints like the knee, improves pain, and slows disease progression.
- Every pound of weight lost reduces knee joint load by approximately 4 pounds, making weight loss one of the most effective interventions for symptomatic relief and disease modification.
- Given the patient's diabetes and cardiovascular risk factors, weight loss also addresses multiple comorbidities simultaneously.
*Rest for 1-2 weeks*
- While rest can temporarily alleviate symptoms in acute exacerbations, prolonged rest for 1-2 weeks is generally **not the best long-term initial management** for chronic knee pain caused by osteoarthritis, and it may lead to deconditioning and muscle atrophy.
- The patient's pain has been steadily worsening for a year, suggesting a chronic issue where activity modification and weight loss are more beneficial than complete immobility.
*Colchicine*
- **Colchicine** is primarily used for diagnosing and treating **gout**, which is not strongly indicated here despite the patient's alcohol use and diabetes (risk factors for gout).
- Although the patient has mild erythema and bruising, the bruising is explained by recent trauma, and there are no classic signs of an acute gout attack, such as severe pain, rapid onset, or specific joint involvement like the first metatarsophalangeal joint.
- The absence of pain on palpation makes gout unlikely.
*Aspirin*
- **Aspirin** is an NSAID and can provide symptomatic pain relief, but it does not address the underlying mechanical cause of osteoarthritis in an obese patient.
- Given the patient's existing medications (lisinopril, HCTZ) and diabetes, adding NSAIDs like aspirin could increase the risk of adverse effects such as **renal dysfunction**, gastrointestinal bleeding, and fluid retention.
- NSAIDs are better used as adjunctive therapy after addressing fundamental issues like excess weight.
*MRI*
- While an MRI can provide detailed images of knee structures, it is generally **not the initial step** for chronic knee pain suggestive of osteoarthritis.
- Clinical diagnosis and plain radiographs are usually sufficient for initial evaluation of osteoarthritis, and an MRI would typically be reserved for cases where other pathologies (meniscal tears, ligamentous injuries) are suspected or when surgery is being considered.
- Imaging does not change the initial management recommendation of weight loss in this obese patient with clinical osteoarthritis.
Osteoarthritis US Medical PG Question 6: A 72-year-old man presents to his primary care physician for his annual exam. He has a very stoic personality and says that he is generally very healthy and has "the normal aches and pains of old age." On further probing, you learn that he does have pretty significant back and hip pain that worsens throughout the day. On physical exam you note bony enlargement of the distal interphalangeal joints bilaterally. Which of the following is the likely cause of his symptoms?
- A. Rheumatoid arthritis
- B. Osteoarthritis (Correct Answer)
- C. Gout
- D. Pseudogout
- E. Osteopenia
Osteoarthritis Explanation: ***Osteoarthritis***
- The patient's age (72 years), back and hip pain that **worsens throughout the day** (classic for *wear-and-tear*), and **bony enlargement of the distal interphalangeal (DIP) joints** (Heberden's nodes) are highly characteristic of osteoarthritis.
- This condition involves the progressive **degeneration of articular cartilage**, leading to bone-on-bone friction and osteophyte formation.
*Osteopenia*
- **Osteopenia** is a precursor to osteoporosis, characterized by **reduced bone mineral density**, making bones weaker.
- It typically presents with **no symptoms** until it progresses to osteoporosis and causes fractures; it does not cause pain that worsens throughout the day or bony enlargements of joints.
*Rheumatoid arthritis*
- **Rheumatoid arthritis** typically affects the **small joints of the hands and feet symmetrically**, but it predominantly involves the **proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints**, sparing the distal interphalangeal (DIP) joints.
- Pain and stiffness associated with rheumatoid arthritis are usually **worse in the morning** and *improve with activity*, in contrast to the patient's symptoms.
*Gout*
- **Gout** is an inflammatory arthritis caused by the deposition of **urate crystals**, typically presenting as *acute, severe attacks* of pain, swelling, and redness in a single joint, most commonly the **big toe**.
- While it can affect other joints over time, it does not typically cause gradual onset, activity-related pain, or bony enlargement of DIP joints as described.
*Pseudogout*
- **Pseudogout**, or **calcium pyrophosphate deposition disease (CPPD)**, is caused by the deposition of **calcium pyrophosphate crystals** in joints.
- Similar to gout, it causes *acute inflammatory arthritis*, often affecting larger joints like the knee or wrist, and is not characterized by the chronic, activity-related pain and DIP joint bony changes seen in this patient.
Osteoarthritis US Medical PG Question 7: A 55-year-old male presents with left hip pain and stiffness. Radiographs are shown in Figures A and B. Serum alkaline phosphatase levels are elevated. A biopsy of the left femur is performed and shown in Figure C. Which of the following cells are initially responsible for this condition?
- A. T-Cells
- B. Fibroblasts
- C. Osteoblasts
- D. Osteoclasts (Correct Answer)
- E. Neutrophils
Osteoarthritis Explanation: ***Osteoclasts***
- The presented images and elevated **alkaline phosphatase** strongly suggest **Paget's disease of bone**, which is characterized by abnormal bone remodeling initially driven by excessive osteoclastic activity.
- In Paget's disease, the initial phase involves a chaotic increase in **osteoclast** number and activity, leading to focal areas of excessive bone resorption.
*T-Cells*
- **T-cells** are primarily involved in immune responses and cell-mediated immunity rather than direct bone remodeling in Paget's disease.
- While immune factors may play a role in the pathogenesis of Paget's disease, **T-cells** are not the primary cells responsible for the initial destructive phase.
*Fibroblasts*
- **Fibroblasts** are connective tissue cells involved in producing collagen and extracellular matrix, important for tissue repair and scarring.
- They are not the main cells responsible for the initial abnormal bone resorption observed in Paget's disease.
*Osteoblasts*
- **Osteoblasts** are bone-forming cells responsible for synthesizing and depositing new bone matrix.
- In Paget's disease, osteoblastic activity is increased in a compensatory and disorganized manner following the initial osteoclastic hyperactivity, but they are not the cells _initially_ responsible for the condition.
*Neutrophils*
- **Neutrophils** are a type of white blood cell primarily involved in acute inflammatory responses to infections.
- They have no direct role in the primary pathogenesis of Paget's disease of bone.
Osteoarthritis US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Osteoarthritis Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Osteoarthritis US Medical PG Question 9: A 69-year-old woman presents with pain in her hip and groin. She states that the pain is present in the morning, and by the end of the day it is nearly unbearable. Her past medical history is notable for a treated episode of acute renal failure, diabetes mellitus, obesity, and hypertension. Her current medications include losartan, metformin, insulin, and ibuprofen. The patient recently started taking high doses of vitamin D as she believes that it could help her symptoms. She also states that she recently fell off the treadmill while exercising at the gym. On physical exam you note an obese woman. There is pain, decreased range of motion, and crepitus on physical exam of her right hip. The patient points to the areas that cause her pain stating that it is mostly over the groin. The patient's skin turgor reveals tenting. Radiography is ordered.
Which of the following is most likely to be found on radiography?
- A. Loss of joint space and osteophytes (Correct Answer)
- B. Posterior displacement of the femoral head
- C. Hyperdense foci in the ureters
- D. Femoral neck fracture
- E. Normal radiography
Osteoarthritis Explanation: ***Loss of joint space and osteophytes***
- The patient's presentation with **hip and groin pain worsened by activity**, improved with rest, and associated with **crepitus** and **decreased range of motion**, is highly suggestive of **osteoarthritis**.
- **Osteoarthritis** is characterized radiographically by **loss of joint space**, **osteophytes** (bone spurs), subchondral sclerosis, and subchondral cysts.
*Posterior displacement of the femoral head*
- This finding is characteristic of a **posterior hip dislocation**, which usually presents with severe pain and an inability to bear weight after a significant traumatic event.
- While the patient fell, her symptoms are chronic and progressive, and she has signs of arthritis rather than acute dislocation.
*Hyperdense foci in the ureters*
- These would indicate **kidney stones**, which typically present with acute, severe flank pain radiating to the groin, and hematuria.
- The patient's symptoms are chronic and localized to the hip joint, making kidney stones an unlikely cause of her primary complaint.
*Femoral neck fracture*
- A **femoral neck fracture** would cause acute, severe hip pain, inability to bear weight, and often external rotation and shortening of the leg, usually following a fall.
- Although she fell, her chronic, activity-related pain and crepitus are more indicative of a degenerative process.
*Normal radiography*
- Given the patient's age, chronic and worsening hip pain, physical exam findings of crepitus and decreased range of motion, and risk factors like obesity, it is highly improbable that her hip X-rays would be normal.
- These symptoms are classic for **osteoarthritis**, which shows distinct radiographic changes.
Osteoarthritis US Medical PG Question 10: A 70-year-old woman presents to her primary care doctor complaining of left knee pain. She states that she has noticed this more during the past several months after a fall at home. Previously, she was without pain and has no history of trauma to her knees. The patient states that the majority of her pain starts in the afternoon after she has been active for some time, and that the pain resolves with rest and over-the-counter analgesics. Aside from the left knee, she has no other symptoms and no other joint findings. On exam, her temperature is 98.8°F (37.1°C), blood pressure is 124/76 mmHg, pulse is 70/min, and respirations are 12/min. The patient has no limitations in her range of motion and no changes in strength on motor testing. However, there is tenderness along the medial joint line. What finding is most likely seen in this patient?
- A. Association with HLA-DR4
- B. Heberden nodes
- C. Increased synovial fluid
- D. Marginal sclerosis (Correct Answer)
- E. Joint pannus
Osteoarthritis Explanation: ***Marginal sclerosis***
- The patient's symptoms (age, knee pain worsening with activity and relieved by rest, tenderness on the medial joint line) are highly suggestive of **osteoarthritis**.
- **Marginal sclerosis** (increased bone density at the joint margins) is a characteristic radiological finding in osteoarthritis, resulting from increased stress on the subchondral bone.
*Association with HLA-DR4*
- **HLA-DR4** is strongly associated with **rheumatoid arthritis**, an autoimmune inflammatory condition.
- The patient's symptoms (pain worsening with activity, relief with rest, absence of systemic inflammation) do not align with rheumatoid arthritis.
*Heberden nodes*
- **Heberden nodes** are bony enlargements of the **distal interphalangeal (DIP)** joints of the fingers, characteristic of osteoarthritis.
- While frequently seen in osteoarthritis, the question describes knee pain and does not mention findings in the hands, so this is not the most direct finding for the described locale of pain.
*Increased synovial fluid*
- While some mild effusion can occur in osteoarthritis, significant **increased synovial fluid** (effusion or swelling) is more typical of **inflammatory arthropathies** or acute injuries.
- The patient's exam notes no limitations in range of motion and only tenderness, not overt swelling.
*Joint pannus*
- A **pannus** is an abnormal layer of fibrovascular tissue that invades and erodes cartilage and bone, a hallmark of **rheumatoid arthritis**.
- This finding is specific to inflammatory arthritides and not characteristic of osteoarthritis.
More Osteoarthritis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.