Large vessel vasculitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Large vessel vasculitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Large vessel vasculitis US Medical PG Question 1: A 74-year-old woman with no significant past medical history presents with 1 week of fever, unremitting headache and hip and shoulder stiffness. She denies any vision changes. Physical examination is remarkable for right scalp tenderness and range of motion is limited due to pain and stiffness. Neurological testing is normal. Laboratory studies are significant for an erythrocyte sedimentation rate (ESR) at 75 mm/h (normal range 0-22 mm/h for women). Which of the following is the most appropriate next step in management?
- A. Start IV methylprednisolone
- B. Obtain CT head without contrast
- C. Start oral prednisone (Correct Answer)
- D. Perform a temporal artery biopsy
- E. Perform a lumbar puncture
Large vessel vasculitis Explanation: **Start oral prednisone**
- The patient's symptoms (fever, headache, hip and shoulder stiffness, scalp tenderness, elevated ESR) are highly suggestive of **giant cell arteritis (GCA)**, which is closely associated with **polymyalgia rheumatica (PMR)**.
- Starting oral prednisone promptly is appropriate to manage the symptoms and prevent potential complications like **vision loss**, especially when classic GCA symptoms are present but there is no acute vision loss.
*Start IV methylprednisolone*
- **IV methylprednisolone** is typically reserved for patients with **acute vision loss** or other severe ischemic complications of GCA, which are not described in this patient.
- While GCA is a serious condition, oral prednisone is usually sufficient for initial management unless impending or active catastrophic events like blindness are present.
*Obtain CT head without contrast*
- A **CT head without contrast** would primarily be useful for evaluating acute neurological deficits or ruling out intracranial pathology like a hemorrhage or mass, which are not indicated by this patient's presentation (normal neurological exam).
- It would not confirm GCA or PMR and would delay appropriate steroid initiation.
*Perform a temporal artery biopsy*
- A **temporal artery biopsy** is the gold standard for confirming GCA, but it is not the most appropriate *next step in management* for a suspected case.
- **Steroid therapy should be initiated immediately** based on clinical suspicion to prevent irreversible vision loss, even before the biopsy results are available. The biopsy can be performed within 1-2 weeks of starting steroids without significantly affecting diagnostic yield.
*Perform a lumbar puncture*
- A **lumbar puncture** is used to diagnose conditions affecting the central nervous system, such as meningitis or subarachnoid hemorrhage.
- The patient's presentation, including normal neurological testing and specific musculoskeletal symptoms, does not point towards an infectious or inflammatory process requiring a lumbar puncture.
Large vessel vasculitis US Medical PG Question 2: A 72-year-old man presents to his primary care provider complaining of fatigue, mild headache, and discomfort with chewing for roughly 1 week. Before this, he felt well overall, but now he is quite bothered by these symptoms. His medical history is notable for hypertension and hyperlipidemia, both controlled. On examination, he is uncomfortable but nontoxic-appearing. There is mild tenderness to palpation over his right temporal artery, but otherwise the exam is not revealing. Prompt recognition and treatment can prevent which of the following feared complications:
- A. Renal failure
- B. Cognitive impairment
- C. Blindness (Correct Answer)
- D. Pulmonary fibrosis
- E. Pericarditis
Large vessel vasculitis Explanation: ***Blindness***
- **Giant cell arteritis (GCA)**, suggested by the patient's symptoms (fatigue, headache, jaw claudication, tender temporal artery), can lead to irreversible **vision loss** if not treated promptly with high-dose steroids.
- The most feared complication is **ischemic optic neuropathy** due to inflammation of the ophthalmic artery or its branches, supplying the optic nerve.
*Renal failure*
- While some vasculitides can affect the kidneys, **renal failure** is not a characteristic or feared complication directly associated with untreated giant cell arteritis.
- Other systemic vasculitides like **ANCA-associated vasculitis** are more commonly linked to kidney involvement.
*Cognitive impairment*
- Although GCA can cause headache and general malaise, it does not typically lead to **progressive cognitive impairment** as a direct or feared complication.
- **Stroke** can occur but is less common than visual loss, and a stroke would be a cause of acute cognitive deficits.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is not a known complication of giant cell arteritis.
- It is more commonly associated with conditions like **systemic sclerosis**, certain autoimmune diseases, or environmental exposures.
*Pericarditis*
- **Pericarditis** (inflammation of the sac surrounding the heart) is not a typical or feared complication of giant cell arteritis.
- While GCA can affect large vessels, it does not commonly target the pericardium.
Large vessel vasculitis US Medical PG Question 3: A 58-year-old woman presents to the physician with a throbbing headache. She says she had it for the last year and it’s usually located in the right temporal area. There is localized tenderness over the scalp. During the last 2 weeks, she experienced 3 episodes of transient loss of vision on the right side, without ocular pain. On physical examination, her vital signs are normal. Palpation reveals that the pulsations of the superficial temporal artery on the right side are reduced in amplitude. Laboratory studies show:
Blood hemoglobin 10.7 g/dL (6.64 mmol/L)
Leukocyte count 8,000/mm3 (8.0 x 109/L)
Platelet count 470,000/mm3 (470 x 109/L)
Erythrocyte sedimentation rate 60 mm/h (60 mm/h)
Which of the following conditions is most likely to co-exist with the presenting complaint in this woman?
- A. Amyloidosis
- B. Sjogren’s syndrome
- C. Fibromyalgia
- D. Polymyalgia rheumatica (Correct Answer)
- E. Dermatomyositis
Large vessel vasculitis Explanation: ***Polymyalgia rheumatica***
- This patient's symptoms are highly suggestive of **giant cell arteritis** (temporal arteritis) due to the throbbing headache, temporal tenderness, reduced temporal artery pulsation, **amaurosis fugax**, and elevated ESR.
- **Polymyalgia rheumatica** is closely associated with giant cell arteritis, often co-existing in up to 50% of patients. Both conditions are characterized by systemic inflammation.
*Amyloidosis*
- **Amyloidosis** is a disorder caused by the deposition of abnormal proteins in various tissues, leading to organ dysfunction.
- It does not typically present with the acute inflammatory symptoms or vascular complications seen in this patient, and there is no direct link to giant cell arteritis.
*Sjogren’s syndrome*
- **Sjogren's syndrome** is an autoimmune disease primarily affecting the **exocrine glands**, leading to dry eyes and dry mouth.
- While it can cause systemic symptoms, it does not typically manifest with temporal arteritis or its specific visual and cranial symptoms.
*Fibromyalgia*
- **Fibromyalgia** is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances, often without clear inflammation markers.
- It is not associated with giant cell arteritis or the inflammatory markers (high ESR) and vascular occlusion symptoms (amaurosis fugax) seen in this patient.
*Dermatomyositis*
- **Dermatomyositis** is an inflammatory myopathy characterized by muscle weakness and distinctive skin rashes.
- While it is an inflammatory condition, it does not typically present with the specific headache, temporal artery abnormalities, or visual symptoms that are hallmarks of giant cell arteritis.
Large vessel vasculitis US Medical PG Question 4: A 5-year-old boy presents to his pediatrician for a well-child visit. His mother reports him to be doing well and has no concerns. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. On physical exam, he is noted to have a right upper extremity blood pressure of 150/80 mm Hg. 2+ radial pulses and trace femoral pulses are felt. Cardiac auscultation reveals a regular rate and rhythm with a normal S1 and S2. A 2/6 long systolic murmur with systolic ejection click is heard over left sternal border and back. The point of maximal impulse is normal. Which of the following is the most likely diagnosis?
- A. Takayasu arteritis
- B. Essential hypertension
- C. Interrupted aortic arch
- D. Pheochromocytoma
- E. Coarctation of the aorta (Correct Answer)
Large vessel vasculitis Explanation: ***Coarctation of the aorta***
- The classic presentation includes **hypertension in the upper extremities** and **diminished or delayed femoral pulses** due to narrowing of the aorta.
- A **systolic murmur heard over the left sternal border and back** is characteristic, often accompanied by an ejection click.
*Takayasu arteritis*
- This is a **large vessel vasculitis** that can cause pulse discrepancies and hypertension, but it typically affects **adolescent girls and young women** and presents with systemic inflammatory symptoms, which are absent here.
- While it can affect the aorta, the specific murmur and discrete pulse findings are more indicative of a fixed, congenital obstruction.
*Essential hypertension*
- Although the patient has hypertension, **essential hypertension** in a 5-year-old is rare and less likely to cause differential pulses (strong radial, weak femoral) and a specific cardiac murmur.
- A secondary cause, like coarctation, should be ruled out first in pediatric hypertension.
*Interrupted aortic arch*
- This is a more severe congenital heart defect where the **aortic arch is completely discontinuous**, leading to profound shock and heart failure usually in the neonatal period, making survival to age 5 without prior diagnosis highly unlikely.
- It would present with much more severe symptoms than described.
*Pheochromocytoma*
- This is a **catecholamine-secreting tumor** that causes episodic or sustained hypertension, sweating, and palpitations.
- It does not typically cause **differential pulses** or a **systolic murmur** pathognomonic for an obstructive lesion.
Large vessel vasculitis US Medical PG Question 5: A 32-year-old woman presents with new left-arm pain. She was previously well but for 2 months has had episodes of low-grade fever, night sweats, and dizziness. She works as a stock assistant and has noticed left arm pain when she stocks shelves. She is taking a multivitamin but no other medications. On physical examination, her blood pressure is 126/72 in her right arm, but it cannot be measured in her left arm. The left radial pulse is not detectable. There is a bruit over the left subclavian area. Femoral and pedal pulses are normal and no abdominal bruits are heard. The left hand is cool but has no other evidence of ischemia. Which of the following is the most likely etiology of this patient’s condition?
- A. Raynaud’s phenomenon
- B. Fibromuscular dysplasia
- C. Subclavian steal syndrome
- D. Aortic coarctation
- E. Takayasu arteritis (Correct Answer)
Large vessel vasculitis Explanation: ***Takayasu arteritis***
- This **large-vessel vasculitis** predominantly affects **young women** (typically <40 years old) and involves the aorta and its major branches, including the subclavian arteries.
- The patient's **constitutional symptoms** (low-grade fever, night sweats) reflect the systemic inflammatory nature of the disease.
- The **absent left radial pulse**, **unmeasurable left arm blood pressure**, and **subclavian bruit** indicate significant stenosis or occlusion of the left subclavian artery, a hallmark of Takayasu arteritis.
- This arterial stenosis can lead to **subclavian steal syndrome** (a manifestation, not the etiology) and **arm claudication** with exertion (pain when stocking shelves).
- The **normal femoral and pedal pulses** help localize the pathology to the upper extremity vessels.
*Subclavian steal syndrome*
- This is a **hemodynamic phenomenon** (manifestation), not an underlying etiology.
- It occurs when subclavian artery stenosis causes retrograde flow from the vertebral artery to supply the affected arm, which can cause dizziness due to vertebrobasilar insufficiency.
- The underlying **cause** in this young woman with systemic symptoms is most likely Takayasu arteritis.
*Raynaud's phenomenon*
- Characterized by **episodic vasospasm** of digital arteries in response to cold or stress, causing color changes (white-blue-red).
- Does not cause **absent pulses**, **unequal blood pressures between arms**, **bruits**, or **constitutional symptoms**.
*Aortic coarctation*
- A **congenital narrowing of the aorta**, typically just distal to the left subclavian artery origin.
- Would cause **hypertension in both upper extremities** with **diminished lower extremity pulses and blood pressures** (upper-lower discrepancy, not left-right arm discrepancy).
- Does not explain the constitutional symptoms or isolated left arm findings.
*Fibromuscular dysplasia*
- A **noninflammatory arteriopathy** causing abnormal cellular proliferation in arterial walls, most commonly affecting **renal and carotid arteries**.
- Typically occurs in **middle-aged women** without systemic symptoms.
- While it can rarely affect subclavian arteries, the **constitutional symptoms** and pattern of large-vessel involvement strongly favor an inflammatory vasculitis like Takayasu arteritis.
Large vessel vasculitis US Medical PG Question 6: A 40-year-old woman comes to the emergency department because of difficulty walking for the past 4 hours. She first noticed her symptoms after getting up this morning and her foot dragging while walking. She feels tired. She has a history of chronic sinusitis. Six months ago, she was diagnosed with asthma. Current medications include an albuterol inhaler and inhaled corticosteroids. Her temperature is 38.9°C (102°F), pulse is 80/min, and her blood pressure is 140/90 mm Hg. Auscultation of her lungs shows diffuse wheezing over bilateral lung fields. Physical examination shows tender subcutaneous nodules on the extensor surfaces of the elbows. There are palpable, non-blanching erythematous lesions on both shins. Dorsiflexion of the right foot is impaired. Sensation to pinprick, light touch, and vibration is decreased over the ulnar aspect of the left forearm. Laboratory studies show:
Hemoglobin 11.3 g/dL
Leukocyte count 24,500
Segmented neutrophils 48%
Eosinophils 29%
Lymphocytes 19%
Monocytes 4%
Platelet count 290,000/mm3
Serum
Urea nitrogen 32 mg/dL
Creatinine 1.85 mg/dL
Urine
Blood 2+
Protein 3+
Which of the following is the most likely diagnosis in this patient?
- A. Granulomatosis with polyangiitis
- B. Excessive glucocorticoid use
- C. Goodpasture syndrome
- D. Henoch-Schönlein purpura
- E. Eosinophilic granulomatosis with polyangiitis (Correct Answer)
Large vessel vasculitis Explanation: ***Eosinophilic granulomatosis with polyangiitis (EGPA)***
- This patient presents with a classic triad: **asthma**, **eosinophilia** (29%), and **multisystem vasculitis** as evidenced by mononeuropathy, skin lesions (nodules and palpable purpura), and kidney involvement.
- The history of chronic sinusitis, new-onset foot drop (mononeuropathy), **palpable purpura**, and elevated creatinine with proteinuria strongly point towards EGPA.
*Granulomatosis with polyangiitis (GPA)*
- While GPA can cause sinusitis, kidney disease, and neuropathy, it typically presents with **neutrophilic inflammation** and **c-ANCA** positivity, not prominent eosinophilia or severe asthma.
- Granulomatosis with polyangiitis typically involves the **upper and lower respiratory tracts** and kidneys but lacks the pronounced eosinophilia and severe asthma seen here.
*Excessive glucocorticoid use*
- This condition is associated with Cushingoid features, **osteoporosis**, and immunosuppression, none of which fully explain the patient's acute neurological deficits, eosinophilia, or vasculitic manifestations.
- Although the patient has asthma, her symptoms are not consistent with the side effects of inhaled corticosteroids or chronic systemic glucocorticoid use.
*Goodpasture syndrome*
- Goodpasture syndrome is characterized by **recurrent pulmonary hemorrhage** and rapidly progressive **glomerulonephritis** due to anti-GBM antibodies.
- It does not explain the prominent eosinophilia, asthma, or the presence of subcutaneous nodules and palpable purpura.
*Henoch-Schönlein purpura (HSP)*
- HSP typically presents in children with **palpable purpura** on the buttocks and lower extremities, **arthralgias**, abdominal pain, and **IgA nephropathy**.
- It does not involve significant eosinophilia, severe asthma, or mononeuropathy as seen in this adult patient.
Large vessel vasculitis US Medical PG Question 7: A 62-year-old man presents to the emergency department with hematuria and hemoptysis that started in the morning. He notes that he has had frequent lung infections throughout his adult life, the most recent being 2 weeks ago. He also mentions that he has had hematuria twice before but never as severe as he is having currently. His medical history is otherwise non-significant, and his only medication is acetaminophen as needed. His blood pressure is 136/92 mm Hg, heart rate is 86/min, respiratory rate is 16/min, and temperature is 37.0°C (98.6°F). Chest radiography shows a resolving right middle lobe airspace opacity. His initial laboratory tests are notable for elevated erythrocyte sedimentation rate and C-reactive protein level. While in the examination room, the patient develops a spontaneous nosebleed. What is the most likely diagnosis?
- A. Goodpasture syndrome
- B. IgA nephropathy
- C. Minimal change disease
- D. Post-streptococcal glomerulonephritis
- E. Granulomatosis with polyangiitis (Correct Answer)
Large vessel vasculitis Explanation: ***Granulomatosis with polyangiitis***
- This patient presents with a **triad of upper airway (nosebleed), lower airway (hemoptysis, recurrent lung infections), and renal involvement (hematuria)**, which is classic for granulomatosis with polyangiitis (GPA), a form of ANCA-associated vasculitis.
- The elevated **ESR and CRP** indicate systemic inflammation, which is common in vasculitic conditions.
*Goodpasture syndrome*
- Characterized by **glomerulonephritis and pulmonary hemorrhage (hemoptysis)**, but typically does not involve the upper airways (e.g., nosebleeds).
- Diagnosis is confirmed by the presence of **anti-glomerular basement membrane antibodies**, which often presents more acutely.
*IgA nephropathy*
- Often presents with **recurrent episodes of gross hematuria**, frequently following an upper respiratory tract infection.
- While it involves the kidneys, it **does not typically cause pulmonary or upper airway symptoms** such as hemoptysis or recurrent lung opacities.
*Minimal change disease*
- Characterized by **nephrotic syndrome (proteinuria, hypoalbuminemia, edema)** and rarely presents with hematuria.
- **Does not cause pulmonary or upper airway manifestations** like hemoptysis or nosebleeds.
*Post-streptococcal glomerulonephritis*
- Typically occurs **1-3 weeks after a streptococcal infection** and presents with acute nephritic syndrome (hematuria, proteinuria, edema, hypertension).
- **Does not involve recurrent lung infections or hemoptysis** and is less likely in an adult with recurrent hematuria episodes.
Large vessel vasculitis US Medical PG Question 8: A 27-year-old man presents to his primary care physician with worsening cough and asthma. The patient reports that he was in his usual state of health until 1 month ago, when he developed a cold. Since then his cold has improved, but he continues to have a cough and worsening asthma symptoms. He says that he has been using his rescue inhaler 3 times a day with little improvement. He is studying for an accounting exam and states that his asthma is keeping him up at night and making it hard for him to focus during the day. The patient admits to smoking tobacco. His smoking has increased from a half pack per day since he was 17 years old to 1 pack per day during the past month to cope with the stress of his exam. The patient's temperature is 99°F (37.2°C), blood pressure is 110/74 mmHg, pulse is 75/min, and respirations are 15/min with an oxygen saturation of 97% on room air. Physical examination is notable for mild expiratory wheezes bilaterally. Labs are obtained, as shown below:
Serum:
Na+: 144 mEq/L
Cl-: 95 mEq/L
K+: 4.3 mEq/L
HCO3-: 23 mEq/L
Urea nitrogen: 24 mg/dL
Glucose: 100 mg/dL
Creatinine: 1.6 mg/dL
Leukocyte count and differential:
Leukocyte count: 13,000/mm^3
Segmented neutrophils: 63%
Eosinophils: 15%
Basophils: < 1%
Lymphocytes: 20%
Monocytes: 1.3%
Hemoglobin: 13.5 g/dL
Hematocrit: 50%
Platelets: 200,000/mm^3
Urinalysis reveals proteinuria and microscopic hematuria. Which of the following is associated with the patient's most likely diagnosis?
- A. IgA deposits
- B. Smoking
- C. c-ANCA levels
- D. Hepatitis B surface antigen
- E. p-ANCA levels (Correct Answer)
Large vessel vasculitis Explanation: ***p-ANCA levels***
- The patient presents with asthma, sinusitis-like symptoms (prior cold followed by worsening cough/asthma), eosinophilia (15%), and renal involvement (proteinuria, hematuria, elevated creatinine). This constellation of symptoms is highly suggestive of **Eosinophilic Granulomatosis with Polyangiitis (EGPA)**, formerly known as Churg-Strauss Syndrome.
- Approximately 30-40% of EGPA patients are positive for **p-ANCA (anti-myeloperoxidase antibodies)**, which are associated with the vasculitic phase and renal involvement.
*IgA deposits*
- **IgA deposits** are characteristic of **IgA nephropathy (Berger's disease)** or **Henoch-Schönlein purpura** (now IgA vasculitis), which typically present with hematuria and proteinuria, sometimes after an upper respiratory infection.
- However, these conditions do not typically cause severe asthma, significant eosinophilia, or a systemic vasculitis picture with pulmonary involvement as seen in this patient.
*Smoking*
- While the patient is a smoker and smoking can exacerbate asthma and contribute to chronic lung disease, it is not an *associated factor* with the underlying diagnosis of EGPA itself.
- Smoking is a risk factor for many respiratory illnesses but doesn't specifically point to EGPA in the context of the given clinical and laboratory findings.
*c-ANCA levels*
- **c-ANCA (anti-proteinase 3 antibodies)** are primarily associated with **Granulomatosis with Polyangiitis (GPA)**, formerly Wegener's granulomatosis.
- While GPA can present with kidney involvement and pulmonary symptoms, it typically involves the upper airways (sinusitis, otitis), lungs, and kidneys, but is usually *not* associated with severe asthma or prominent eosinophilia, which are key features in this patient.
*Hepatitis B surface antigen*
- **Hepatitis B surface antigen** positivity is associated with **polyarteritis nodosa (PAN)** due to immune complex deposition.
- PAN is a necrotizing vasculitis that can affect multiple organs but typically spare the lungs and is not associated with asthma or eosinophilia.
Large vessel vasculitis US Medical PG Question 9: A 45-year-old man comes to the physician because of fatigue and joint pain for 8 months. He has pain in both knees, both elbows, and diffuse muscle pain. He does not have dyspnea. He also had several episodes of a nonpruritic rash on his lower extremities. Eight years ago, the patient was diagnosed with hepatitis C. His temperature is 37.9°C (100.2°F), pulse is 90/min, and blood pressure is 140/90 mm Hg. Examination of the lower extremities shows raised purple papules that do not blanch when pressure is applied. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.9 g/dL
Leukocyte count 8,500/mm3
Platelets 160,000/mm3
Serum
Creatinine 1.1 mg/dL
ALT 123 U/L
AST 113 U/L
Further evaluation of this patient is most likely to show which of the following findings?
- A. Elevated IgA in serum
- B. Granulomatous inflammation of vessels
- C. Hypocomplementemia (Correct Answer)
- D. Elevated perinuclear anti-neutrophil cytoplasmic antibodies
- E. Positive pathergy test
Large vessel vasculitis Explanation: ***Hypocomplementemia***
- The patient's history of **hepatitis C** infection, along with **fatigue, polyarthralgia, elevated liver enzymes, and palpable purpura**, is classic for **HCV-associated mixed cryoglobulinemia syndrome**.
- **Mixed cryoglobulinemia** (types II and III) involves immune complex deposition, which activates and consumes complement, leading to **low C3 and C4 levels** (hypocomplementemia).
- **Hypocomplementemia** is a hallmark laboratory finding and helps distinguish cryoglobulinemic vasculitis from other small vessel vasculitides.
*Elevated IgA in serum*
- Elevated IgA levels are characteristic of **IgA vasculitis (Henoch-Schönlein purpura)**, which typically affects children and presents with palpable purpura, abdominal pain, and glomerulonephritis.
- While IgA vasculitis can occur in adults, the strong association with **hepatitis C infection** and the typical adult presentation point toward cryoglobulinemia rather than IgA vasculitis.
*Granulomatous inflammation of vessels*
- **Granulomatous inflammation of vessels** is a hallmark of **Granulomatosis with Polyangiitis (GPA)** or **Eosinophilic Granulomatosis with Polyangiitis (EGPA)**.
- These conditions typically present with upper/lower respiratory tract involvement, renal disease, and **ANCA positivity**, not the pattern seen here.
*Elevated perinuclear anti-neutrophil cytoplasmic antibodies*
- **p-ANCA** (perinuclear anti-neutrophil cytoplasmic antibodies) are primarily associated with **microscopic polyangiitis** and **eosinophilic granulomatosis with polyangiitis (EGPA)**.
- The clinical picture of **HCV-associated mixed cryoglobulinemia** does not typically involve ANCA positivity; instead, **rheumatoid factor** and **cryoglobulins** would be the relevant serologic markers.
*Positive pathergy test*
- A **positive pathergy test** is characteristic of **Behçet's disease**, an inflammatory disorder causing recurrent oral and genital ulcers, skin lesions, and uveitis.
- This condition does not align with the patient's presentation of palpable purpura, polyarthralgia, and HCV-associated systemic symptoms.
Large vessel vasculitis US Medical PG Question 10: A 32-year-old woman who recently emigrated to the USA from Japan comes to the physician because of a 3-month history of night sweats, malaise, and joint pain. During this time, she has also had a 6-kg (13-lb) weight loss. Physical examination shows weak brachial and radial pulses. There are tender subcutaneous nodules on both legs. Carotid bruits are heard on auscultation bilaterally. Laboratory studies show an erythrocyte sedimentation rate of 96 mm/h. A CT scan of the chest shows thickening and narrowing of the aortic arch. Microscopic examination of the aortic arch is most likely to show which of the following findings?
- A. Fibrinoid necrosis of the intima and media
- B. Calcification of the media
- C. Granulomatous inflammation of the media (Correct Answer)
- D. Subendothelial hyaline deposition
- E. Subendothelial immune complex deposition
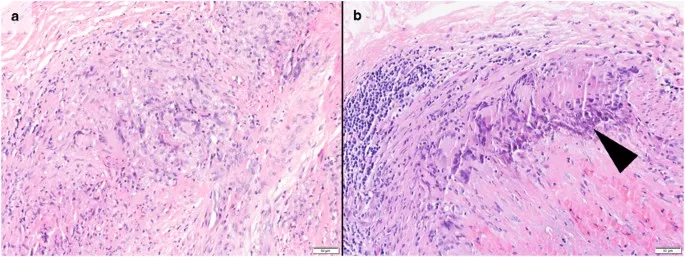
Large vessel vasculitis Explanation: ***Granulomatous inflammation of the media***
- The clinical presentation, including **night sweats, malaise, weight loss, weak brachial and radial pulses** (pulseless disease), and **thickening and narrowing of the aortic arch**, is highly suggestive of **Takayasu arteritis**.
- **Takayasu arteritis** is a **large-vessel vasculitis** characterized pathologically by **granulomatous inflammation** primarily affecting the **tunica media** of the aorta and its major branches.
*Fibrinoid necrosis of the intima and media*
- **Fibrinoid necrosis** is typically seen in **small-to-medium vessel vasculitides** (e.g., polyarteritis nodosa) or in severe **hypertensive vasculopathy**.
- It involves the deposition of **fibrin-like material** in the vessel wall, which is not the primary histological feature of Takayasu arteritis.
*Calcification of the media*
- **Medial calcification** (Mönckeberg arteriosclerosis) primarily affects **muscular arteries** and is typically seen in older individuals, often incidentally.
- It does not cause significant luminal narrowing, inflammation, or the systemic symptoms described in this patient.
*Subendothelial hyaline deposition*
- **Hyaline deposition** in the subendothelium is characteristic of **hyaline arteriolosclerosis**, commonly seen in **benign hypertension** or **diabetes mellitus**, affecting small arteries and arterioles.
- This finding is not consistent with the specific large-vessel inflammatory process seen in Takayasu arteritis.
*Subendothelial immune complex deposition*
- **Immune complex deposition** in the subendothelium is typical of **Type III hypersensitivity reactions**, such as those seen in **lupus nephritis** or **Type II cryoglobulinemia**, often affecting glomeruli or small vessels.
- While Takayasu arteritis is immune-mediated, its hallmark is **granulomatous inflammation**, not primary immune complex deposition in the vessel wall.
More Large vessel vasculitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.