Sleep-disordered breathing US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sleep-disordered breathing. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sleep-disordered breathing US Medical PG Question 1: A 63-year-old man presents to his primary care physician complaining of excessive daytime sleepiness. He explains that this problem has worsened slowly over the past few years but is now interfering with his ability to play with his grandchildren. He worked previously as an overnight train conductor, but he has been retired for the past 3 years. He sleeps approximately 8-9 hours per night and believes his sleep quality is good; however, his wife notes that he often snores loudly during sleep. He has never experienced muscle weakness or hallucinations. He has also been experiencing headaches in the morning and endorses a depressed mood. His physical exam is most notable for his large body habitus, with a BMI of 34. What is the best description of the underlying mechanism for this patient's excessive daytime sleepiness?
- A. Poor oropharyngeal tone (Correct Answer)
- B. Circadian rhythm sleep-wake disorder
- C. Deficiency of the neuropeptides, orexin-A and orexin-B
- D. Insufficient sleep duration
- E. Psychiatric disorder
Sleep-disordered breathing Explanation: ***Poor oropharyngeal tone***
- This patient's symptoms, including **excessive daytime sleepiness**, loud **snoring**, **morning headaches**, **obesity (BMI 34)**, and depressed mood, are all highly suggestive of **obstructive sleep apnea (OSA)**.
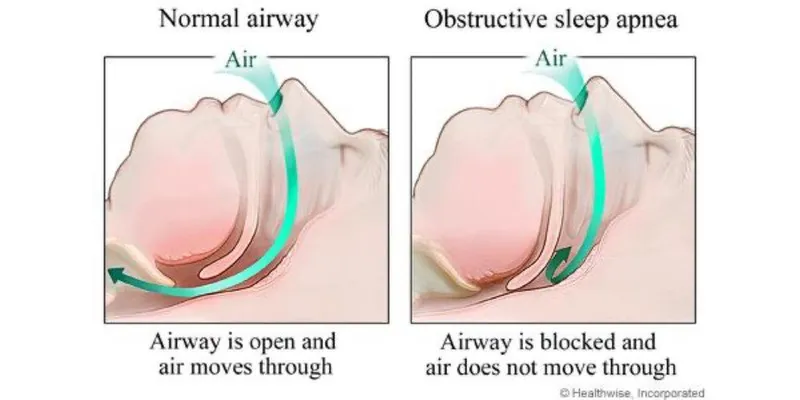
- In OSA, poor oropharyngeal tone, often exacerbated by obesity, leads to the collapse of the upper airway during sleep, causing interrupted breathing and subsequent sleep fragmentation, which manifests as daytime sleepiness.
*Circadian rhythm sleep-wake disorder*
- This disorder typically involves a **misalignment between endogenous sleep-wake rhythms** and external environmental cues, often seen in shift workers or with jet lag.
- While the patient previously worked as an overnight conductor, he has been retired for 3 years, and his symptoms are more aligned with chronic airway obstruction rather than a desynchronized internal clock.
*Deficiency of the neuropeptides, orexin-A and orexin-B*
- A deficiency in **orexin (hypocretin)** is the underlying mechanism for **narcolepsy type 1**, characterized by excessive daytime sleepiness, cataplexy (sudden loss of muscle tone triggered by strong emotions), and sleep paralysis/hypnagogic hallucinations.
- This patient specifically denies muscle weakness or hallucinations, which makes narcolepsy less likely.
*Insufficient sleep duration*
- While insufficient sleep duration can cause excessive daytime sleepiness, the patient reports sleeping approximately **8-9 hours per night**, which is generally considered an adequate duration for adults.
- The loud snoring and other symptoms point towards a **qualitative problem with sleep**, despite seemingly adequate hours.
*Psychiatric disorder*
- While **depressed mood** is present, it is often a **consequence or comorbidity of chronic sleep deprivation** and fragmented sleep rather than the primary cause of the patient's excessive daytime sleepiness and loud snoring.
- Depression alone does not explain the physical signs like snoring and morning headaches without an underlying sleep disorder.
Sleep-disordered breathing US Medical PG Question 2: A 54-year-old man comes to the physician because of excessive daytime sleepiness for 5 months. He wakes up frequently at night, and his wife says his snoring has become louder. He is 180 cm (5 ft 10 in) tall and weighs 104 kg (230 lb); his BMI is 33 kg/m2. His pulse is 80/min and his respiratory rate is 11/min. His jugular venous pressure is 7 cm H2O. He has 2+ pitting edema of the lower legs and ankles. Arterial blood gas analysis on room air shows a pH of 7.42 and a PCO2 of 41 mm Hg. An x-ray of the chest shows normal findings. Which of the following is the most likely underlying cause of this patient's condition?
- A. Daytime alveolar hypoventilation
- B. Decreased levels of hypocretin-1
- C. Increased medullary ventilatory responsiveness
- D. Impaired myocardial relaxation
- E. Intermittent collapse of the oropharynx (Correct Answer)
Sleep-disordered breathing Explanation: ***Intermittent collapse of the oropharynx***
- The patient's symptoms of **excessive daytime sleepiness**, frequent night awakenings, and **loud snoring** are classic signs of **obstructive sleep apnea (OSA)**.
- OSA is characterized by the **intermittent collapse of the oropharynx** during sleep, leading to obstructed airflow. His obesity (BMI 33 kg/m2) is a significant risk factor for OSA.
*Daytime alveolar hypoventilation*
- This would typically present with **elevated PCO2** on arterial blood gas, indicating CO2 retention. The patient's PCO2 of 41 mm Hg is within the normal range, ruling out significant daytime alveolar hypoventilation.
- While chronic severe OSA can eventually lead to obesity hypoventilation syndrome, the current ABG does not support this as the primary underlying cause.
*Decreased levels of hypocretin-1*
- **Decreased hypocretin-1** (also known as orexin) levels in the cerebrospinal fluid are a hallmark of **narcolepsy type 1**.
- While narcolepsy causes excessive daytime sleepiness, it is not associated with loud snoring or night awakenings due to respiratory effort, which are prominent in this patient.
*Increased medullary ventilatory responsiveness*
- **Increased medullary ventilatory responsiveness** would lead to an enhanced drive to breathe, often resulting in **hypocapnia (low PCO2)**, especially in response to metabolic acidosis or hypoxemia.
- This is contrary to the patient's normal PCO2 and clinical picture, which points towards an obstructive rather than a central ventilatory issue.
*Impaired myocardial relaxation*
- **Impaired myocardial relaxation** is a feature of **diastolic heart failure**, which could explain the elevated JVP and peripheral edema.
- However, it does not explain the primary presenting symptoms of excessive daytime sleepiness and loud snoring, which point directly to a sleep-related breathing disorder rather than primarily a cardiac issue.
Sleep-disordered breathing US Medical PG Question 3: A 68-year-old man presents with shortness of breath, particularly when walking up stairs and when lying down to go to sleep at night. He also complains of a chronic cough and states that he now uses 2 extra pillows at night. The patient has a history of type 2 diabetes that is well-managed with metformin. He also takes Prozac for a long-standing history of depression. The patient has a 60-pack-year smoking history. He also has a history significant for alcohol abuse, but he quit cold turkey 15 years ago when his brother was killed in a drunk driving accident. Both he and his brother were adopted, and he does not know other members of his biological family. Despite repeated efforts of patient counseling, the patient is not interested in quitting smoking. The physical exam is significant for an obese male using accessory muscles of respiration. The vital signs include: temperature 36.8°C (98.2°F), heart rate 95/min, respiratory rate 16/min, and blood pressure 130/85 mm Hg. The oxygen saturation is 90% on room air. Additional physical exam findings include cyanotic lips, peripheral edema, hepatomegaly, and ascites. The cardiovascular exam is significant for an S3 heart sound and elevated JVP. The pulmonary exam is significant for expiratory wheezing, diffuse rhonchi, and hyperresonance on percussion. The laboratory test results are as follows:
BUN 15 mg/dL
pCO2 60 mm Hg
Bicarbonate (HCO3) 32 mmol/L
Creatinine 0.8 mg/dL
Glucose 95 mg/dL
Serum chloride 103 mmol/L
Serum potassium 3.9 mEq/L
Serum sodium 140 mEq/L
Total calcium 2.3 mmol/L
Hemoglobin 26 g/dL
Bilirubin total 0.9 mg/dL
Bilirubin indirect 0.4 mg/dL
Iron 100
Ferritin 70
TIBC 300
The posterior-anterior chest X-ray is shown in the image. Which of the following interventions is indicated for decreasing the mortality of this patient?
- A. Flu vaccine
- B. Inhaled anticholinergics
- C. ACE inhibitors
- D. Smoking cessation alone
- E. Both smoking cessation and oxygen administration (Correct Answer)
Sleep-disordered breathing Explanation: **Both smoking cessation and oxygen administration**
- Given the patient's **60-pack-year smoking history**, current respiratory symptoms, and **hypoxemia** (SpO2 90% on room air), **smoking cessation is the single most important intervention to slow the progression of chronic obstructive pulmonary disease (COPD)**.
- **Long-term oxygen therapy (LTOT)** has been shown to **reduce mortality in COPD patients with chronic hypoxemia**. The patient's oxygen saturation of 90% on room air meets the criteria for LTOT.
*Flu vaccine*
- While **influenza vaccination is crucial for preventing exacerbations and reducing morbidity in COPD patients**, it does not directly decrease overall mortality from the underlying disease in the same way as smoking cessation and oxygen therapy.
- It is a recommended prophylactic measure for patients with chronic respiratory conditions, but its impact on all-cause mortality is less direct than the key interventions mentioned.
*Inhaled anticholinergics*
- **Inhaled anticholinergics (e.g., tiotropium)** are bronchodilators that help **improve lung function and reduce symptoms** in COPD, but they do not alter the disease's natural progression or directly reduce mortality.
- They are a cornerstone of **symptomatic management** for COPD but are not considered a mortality-reducing intervention.
*ACE inhibitors*
- **Angiotensin-converting enzyme (ACE) inhibitors** are primarily used in conditions like **hypertension, heart failure, and chronic kidney disease**.
- Although the patient has signs of right-sided heart failure (peripheral edema, hepatomegaly, ascites), which could be secondary to severe COPD (cor pulmonale), ACE inhibitors are **not indicated as a primary treatment for COPD itself** or **to reduce mortality in this context**.
*Smoking cessation alone*
- While **smoking cessation is the most important intervention to slow COPD progression and reduce mortality**, the patient's current **hypoxemia (SpO2 90%) also warrants oxygen administration** for mortality benefit.
- Therefore, **smoking cessation combined with oxygen administration** offers a more comprehensive approach to reducing mortality in this patient.
Sleep-disordered breathing US Medical PG Question 4: A 65-year-old male with multiple comorbidities presents to your office complaining of difficulty falling asleep. Specifically, he says he has been having trouble breathing while lying flat very shortly after going to bed. He notes it only gets better when he adds several pillows, but that sitting up straight is an uncomfortable position for him in which to fall asleep. What is the most likely etiology of this man's sleeping troubles?
- A. Left-sided heart failure (Correct Answer)
- B. Amyotrophic lateral sclerosis (ALS)
- C. Obstructive sleep apnea
- D. Right-sided heart failure
- E. Myasthenia gravis
Sleep-disordered breathing Explanation: ***Left-sided heart failure***
- The patient's inability to breathe while lying flat (orthopnea) and the relief obtained by elevating his head with pillows is a classic symptom of **left-sided heart failure**.
- In this condition, accumulation of fluid in the lungs (pulmonary congestion) due to the heart's inability to pump blood effectively leads to difficulty breathing, especially in the recumbent position.
*Amyotrophic lateral sclerosis (ALS)*
- ALS primarily affects **motor neurons**, leading to progressive muscle weakness, atrophy, and spasticity.
- While it can eventually cause respiratory muscle weakness, it typically presents with more generalized motor symptoms and does not specifically manifest as acute orthopnea relieved by elevating the head of the bed shortly after lying down.
*Obstructive sleep apnea*
- Obstructive sleep apnea is characterized by recurrent upper airway collapse during sleep, leading to **pauses in breathing** and loud snoring.
- While it can cause fragmented sleep and daytime sleepiness, the primary relief is not typically from simply adding pillows but rather from CPAP therapy or surgical interventions to open the airway.
*Right-sided heart failure*
- Right-sided heart failure primarily leads to **systemic venous congestion**, causing symptoms like peripheral edema, ascites, and jugular venous distension.
- It does not typically cause orthopnea as a primary symptom, as pulmonary congestion is not the predominant feature.
*Myasthenia gravis*
- Myasthenia gravis is an **autoimmune disorder** characterized by fluctuating weakness of voluntary muscles, which worsens with activity and improves with rest.
- While it can affect respiratory muscles in severe cases, leading to respiratory compromise, the symptom presentation is more varied than isolated orthopnea, and it does not typically manifest acutely only when lying flat to sleep.
Sleep-disordered breathing US Medical PG Question 5: A 56-year-old man presents to the physician for the evaluation of excess snoring over the past year. He has no history of a serious illness and takes no medications. He does not smoke. His blood pressure is 155/95 mm Hg. BMI is 49 kg/m2. Oropharyngeal examination shows an enlarged uvula. Examination of the nasal cavity shows no septal deviation or polyps. Examination of the lungs and heart shows no abnormalities. Polysomnography shows an apnea-hypopnea index of 2 episodes/h with a PCO2 of 51 mm Hg during REM sleep. Arterial blood gas analysis in room air shows:
pH 7.33
PCO2 50 mm Hg
PO2 92 mm Hg
HCO3− 26 mEq/L
Which of the following best explains these findings?
- A. Obesity hypoventilation syndrome with obstructive sleep apnea
- B. Central hypoventilation syndrome with obstructive sleep apnea
- C. Central hypoventilation syndrome
- D. Obesity hypoventilation syndrome (Correct Answer)
- E. Obstructive sleep apnea-hypopnea syndrome
Sleep-disordered breathing Explanation: ***Obesity hypoventilation syndrome***
- This is the correct diagnosis. The patient presents with **severe obesity (BMI 49 kg/m2)** and **chronic daytime hypercapnia (PCO2 50 mm Hg)** with compensated respiratory acidosis (pH 7.33, HCO3− 26 mEq/L).
- The **apnea-hypopnea index (AHI) of 2 episodes/h is normal** and does not meet criteria for obstructive sleep apnea (OSA requires AHI ≥5).
- Despite the absence of significant obstructive events, the patient has **chronic hypercapnia both awake and during REM sleep**, indicating impaired ventilatory drive due to obesity-related restrictive mechanics rather than upper airway obstruction.
- **Obesity hypoventilation syndrome (OHS)** is diagnosed when BMI ≥30 kg/m2, daytime PCO2 ≥45 mm Hg, and sleep-disordered breathing is present without other causes of hypoventilation.
*Obesity hypoventilation syndrome with obstructive sleep apnea*
- While the patient is severely obese, the **AHI of 2 does not meet diagnostic criteria for OSA** (requires AHI ≥5).
- OHS can coexist with OSA (called "overlap" when present), but in this case, the **absence of significant obstructive events** makes pure OHS without OSA the correct diagnosis.
*Central hypoventilation syndrome with obstructive sleep apnea*
- **Central hypoventilation syndrome** is rare and typically associated with neurological disorders (brainstem lesions, Ondine's curse) or congenital conditions.
- This patient has **no neurological signs or symptoms** to suggest impaired central respiratory control.
- The AHI of 2 does not support a diagnosis of OSA.
*Central hypoventilation syndrome*
- This diagnosis requires **failure of brainstem respiratory control centers** to regulate breathing properly.
- There are **no clinical features** (neurological deficits, history of CNS pathology) to suggest a primary central cause of hypoventilation.
- The patient's hypoventilation is best explained by **obesity-related mechanical restriction** and blunted chemoreceptor response, not central nervous system pathology.
*Obstructive sleep apnea-hypopnea syndrome*
- The **AHI of 2 episodes/h is normal** and does not meet diagnostic criteria for OSA (mild OSA: AHI 5-14, moderate: 15-29, severe: ≥30).
- While obesity and enlarged uvula are risk factors for OSA, the **absence of significant obstructive events on polysomnography** excludes this diagnosis.
- The **chronic daytime hypercapnia** in the setting of normal AHI points to OHS rather than OSA as the primary pathology.
Sleep-disordered breathing US Medical PG Question 6: A 15-year-old boy is brought to the physician with excessive daytime sleepiness over the past year. His parents are concerned with his below-average school performance over the last 3 months. He goes to bed around midnight and wakes up at 7 am on school days, but sleeps in late on weekends. He exercises regularly after school. He usually has a light snack an hour before bed. He does not snore or have awakenings during sleep. He has no history of a serious illness and takes no medications. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. He does not smoke or drink alcohol. There is no history of a similar problem in the family. His vital signs are within normal limits. His BMI is 22 kg/m2. Physical examination shows no abnormal findings. Which of the following is the most appropriate recommendation at this time?
- A. Take melatonin before bedtime
- B. Avoid snacks before bedtime
- C. Decrease exercise intensity
- D. Increase nighttime sleep hours (Correct Answer)
- E. Take a nap in the afternoon
Sleep-disordered breathing Explanation: ***Increase nighttime sleep hours***
- The patient's pattern of going to bed at midnight and waking at 7 AM on school days, along with sleeping in late on weekends, suggests a **chronic sleep deficit** accumulated during the week. Adolescents typically require 8-10 hours of sleep per night.
- The excessive daytime sleepiness and declining school performance are strong indicators of insufficient sleep, and **prioritizing more sleep during school nights** is the most direct intervention.
*Take melatonin before bedtime*
- Melatonin supplements are typically used for **sleep-onset insomnia** or **circadian rhythm disorders**, neither of which is clearly indicated here.
- There is no evidence presented of difficulty falling asleep; rather, the issue appears to be insufficient duration of sleep due to **late bedtime schedules**.
*Avoid snacks before bedtime*
- While heavy meals before bedtime can disrupt sleep, this patient reports having only a **light snack**, which is unlikely to be the primary cause of his significant daytime sleepiness.
- There is no mention of indigestion or gastrointestinal discomfort after the snack that would point to this as a problem.
*Decrease exercise intensity*
- Regular exercise generally **improves sleep quality**, and there's no indication that the patient's exercise routine is negatively impacting his sleep.
- While very intense exercise too close to bedtime can be disruptive for some, exercise itself is generally beneficial for sleep and overall health; therefore, reducing it would not be a primary recommendation.
*Take a nap in the afternoon*
- While naps can temporarily alleviate daytime sleepiness, they can also **disrupt nighttime sleep patterns** by reducing sleep drive.
- Napping would be treating the symptom rather than the root cause, which is a **chronic lack of sufficient nighttime sleep**.
Sleep-disordered breathing US Medical PG Question 7: A 37-year-old man presents to his primary care physician because he has been experiencing episodes where he wakes up at night gasping for breath. His past medical history is significant for morbid obesity as well as hypertension for which he takes lisinopril. He is diagnosed with sleep apnea and prescribed a continuous positive airway pressure apparatus. In addition, the physician discusses making lifestyle and behavioral changes such as dietary modifications and exercise. The patient agrees to attempt these behavioral changes. Which of the following is most likely to result in improving patient adherence to this plan?
- A. Refer the patient to a peer support group addressing lifestyle changes
- B. Ask the patient to bring a family member to next appointment
- C. Provide follow-up appointments to assess progress in attaining goals (Correct Answer)
- D. Provide appropriate publications for the patient's educational level
- E. Inform the patient of the health consequences of not intervening
Sleep-disordered breathing Explanation: ***Provide follow-up appointments to assess progress in attaining goals***
- **Regular follow-up appointments** provide accountability and opportunities to discuss progress, troubleshoot challenges, and reinforce motivation for lifestyle changes
- This approach fosters a **patient-centered relationship** where the physician actively participates in the patient's journey, increasing adherence
- Evidence supports that scheduled follow-up is one of the most effective interventions for improving adherence to chronic disease management plans
*Refer the patient to a peer support group addressing lifestyle changes*
- While peer support can be beneficial for some patients, it is **not universally effective** and might not be suitable for all patients, especially as a primary strategy for adherence
- The effectiveness of such groups varies widely based on the patient's personality and group dynamics, potentially leading to **inconsistent adherence**
*Ask the patient to bring a family member to next appointment*
- Involving family can be supportive, but it may not always be appropriate or desired by the patient and doesn't directly address the patient's individual motivation or challenges
- While family support can enhance adherence, this approach is supplementary rather than primary in effectiveness
*Provide appropriate publications for the patient's educational level*
- Providing educational materials is a good initial step, but information alone is often **insufficient to sustain long-term behavioral changes**
- Without active follow-up and personalized guidance, written materials can be easily forgotten or not fully implemented into daily life
*Inform the patient of the health consequences of not intervening*
- While explaining risks is crucial for informed consent and awareness, relying solely on **fear-based motivation** often has limited long-term effectiveness in promoting sustained behavioral change
- Patients are often aware of potential negative consequences, but this knowledge alone does not provide the practical support or strategies needed for adherence
Sleep-disordered breathing US Medical PG Question 8: A 49-year-old woman comes to the physician because of a 4-month history of a dry cough and shortness of breath on exertion. She also reports recurrent episodes of pain, stiffness, and swelling in her wrist and her left knee over the past 6 months. She had two miscarriages at age 24 and 28. Physical examination shows pallor, ulcerations on the palate, and annular hyperpigmented plaques on the arms and neck. Fine inspiratory crackles are heard over bilateral lower lung fields on auscultation. Which of the following additional findings is most likely in this patient?
- A. Increased airway resistance
- B. Decreased A-a gradient
- C. Decreased right atrial pressure
- D. Decreased diffusing capacity (Correct Answer)
- E. Increased lung compliance
Sleep-disordered breathing Explanation: ***Decreased diffusing capacity***
- This patient presents with symptoms highly suggestive of **systemic lupus erythematosus (SLE)**, including recurrent miscarriages, joint pain, oral ulcers, skin lesions (annular hyperpigmented plaques), and pulmonary involvement (dry cough, dyspnea, crackles).
- **Interstitial lung disease (ILD)**, a common pulmonary manifestation of SLE, leads to **fibrosis** of the alveolar-capillary membrane, thereby **decreasing the diffusing capacity of the lung for carbon monoxide (DLCO)**.
*Increased airway resistance*
- Increased airway resistance is characteristic of **obstructive lung diseases** like asthma or COPD, which primarily involve narrowing of the airways.
- The patient's presentation with **inspiratory crackles** and symptoms of restrictive disease (shortness of breath on exertion, dry cough) is not consistent with increased airway resistance.
*Decreased A-a gradient*
- A **decreased alveolar-arterial (A-a) gradient** indicates efficient gas exchange and is typically seen in healthy individuals or in conditions causing hypoventilation without intrinsic lung disease.
- In conditions like pulmonary fibrosis or ILD, there is impaired gas exchange leading to an **increased A-a gradient**.
*Decreased right atrial pressure*
- **Decreased right atrial pressure** would typically signify reduced venous return or normal cardiac function.
- Given the patient's respiratory symptoms and potential for pulmonary hypertension secondary to ILD, an **increased right atrial pressure** would be more likely due to increased pulmonary vascular resistance.
*Increased lung compliance*
- **Increased lung compliance** is seen in conditions where the lung tissue becomes more distensible, such as **emphysema**, due to destruction of elastic fibers.
- **Interstitial lung disease** and pulmonary fibrosis, as suggested by the patient's symptoms and signs, lead to **decreased lung compliance** due to stiffening of the lung tissue.
Sleep-disordered breathing US Medical PG Question 9: A 35-year-old woman who was recently ill with an upper respiratory infection presents to the emergency department with weakness in her lower limbs and difficulty breathing. Her symptoms began with a burning sensation in her toes along with numbness. She claims that the weakness has been getting worse over the last few days and now involving her arms and face. Currently, she is unable to get up from the chair without some assistance. Her temperature is 37.0°C (98.6°F), the blood pressure is 145/89 mm Hg, the heart rate is 99/min, the respiratory rate is 12/min, and the oxygen saturation is 95% on room air. On physical examination, she has diminished breath sounds on auscultation of bilateral lung fields with noticeably poor inspiratory effort. Palpation of the lower abdomen reveals a palpable bladder. Strength is 3 out of 5 symmetrically in the lower extremities bilaterally. The sensation is intact. What is the most likely diagnosis?
- A. Guillain-Barré syndrome (Correct Answer)
- B. Adrenoleukodystrophy
- C. Myasthenia Gravis
- D. Multiple sclerosis
- E. Acute disseminated encephalomyelitis
Sleep-disordered breathing Explanation: ***Guillain-Barré syndrome***
- The patient presents with **ascending paralysis** (weakness starting in lower limbs and progressing upwards to arms and face) following an **upper respiratory infection**, which is a classic presentation of GBS.
- The presence of **respiratory compromise** (difficulty breathing, diminished breath sounds, poor inspiratory effort), **dysautonomia** (palpable bladder due to urinary retention), and the pattern of **symmetrical weakness with intact sensation** are characteristic features of GBS.
- GBS typically presents with areflexia and shows albumino-cytologic dissociation on CSF analysis (elevated protein with normal cell count).
*Adrenoleukodystrophy*
- This is a rare, **X-linked genetic disorder** that primarily affects white matter in the brain and spinal cord, typically presenting in childhood with neurological deficits, not an acute ascending paralysis after an infection.
- It involves demyelination and adrenal insufficiency, which are not suggested by the acute onset and progressive neurological symptoms described.
*Myasthenia Gravis*
- Myasthenia gravis typically presents with **fluctuating muscle weakness** that worsens with activity and improves with rest, often affecting ocular and bulbar muscles first.
- The progression of weakness in this case is constant and ascending, not fluctuating, and there is no mention of characteristic findings like ptosis or diplopia.
*Multiple sclerosis*
- MS is characterized by **demyelinating lesions** in the central nervous system, leading to neurological symptoms that are often **disseminated in space and time**, meaning they affect different parts of the body at different times.
- While it can cause weakness, the acute onset of rapidly progressive, ascending, symmetrical paralysis following an infection is not typical for MS; MS symptoms are usually more insidious or relapsing-remitting.
*Acute disseminated encephalomyelitis*
- ADEM is an **acute inflammatory demyelinating disease** of the central nervous system that typically follows an infection or vaccination, but it usually presents with **encephalopathy** (altered mental status), multifocal neurological deficits, and often affects the brain and spinal cord diffusely.
- While it can cause weakness, the prominent ascending paralysis, intact sensation, and lack of encephalopathy make GBS a more fitting diagnosis.
Sleep-disordered breathing US Medical PG Question 10: A 47-year-old patient returns to his primary care physician after starting aspirin two weeks ago for primary prevention of coronary artery disease. He complains that he wakes up short of breath in the middle of the night and has had coughing "attacks" three times. After discontinuing aspirin, what medication is most appropriate for prevention of similar symptoms in this patient?
- A. Prednisone
- B. Montelukast (Correct Answer)
- C. Albuterol
- D. Fluticasone
- E. Tiotropium
Sleep-disordered breathing Explanation: ***Montelukast***
- The patient is experiencing symptoms consistent with **aspirin-exacerbated respiratory disease (AERD)**, characterized by asthma symptoms, nasal polyps, and aspirin sensitivity.
- **Montelukast**, a **leukotriene receptor antagonist**, is effective in preventing these symptoms by blocking the inflammatory effects of leukotrienes, which are overproduced in AERD.
*Prednisone*
- While **oral corticosteroids** like prednisone can treat acute exacerbations of AERD, they are not suitable for long-term primary prevention due to significant side effects.
- Long-term use of prednisone is associated with issues like **osteoporosis**, **diabetes**, and **hypertension**.
*Albuterol*
- **Albuterol** is a **short-acting beta-agonist (SABA)** used for rescue relief of acute asthma symptoms and bronchospasm, not for long-term prevention.
- It does not address the underlying inflammatory pathway triggered by aspirin in AERD.
*Fluticasone*
- **Fluticasone** is an **inhaled corticosteroid (ICS)** primarily used for long-term control of asthma by reducing airway inflammation.
- While it can help with some asthma symptoms, it does not specifically prevent the aspirin-induced bronchospasm seen in AERD as effectively as leukotriene modifiers.
*Tiotropium*
- **Tiotropium** is a **long-acting muscarinic antagonist (LAMA)** primarily used in the maintenance treatment of **COPD** and sometimes for severe asthma.
- It works by bronchodilation but does not target the specific leukotriene pathway involved in AERD.
More Sleep-disordered breathing US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.