Sarcoidosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sarcoidosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
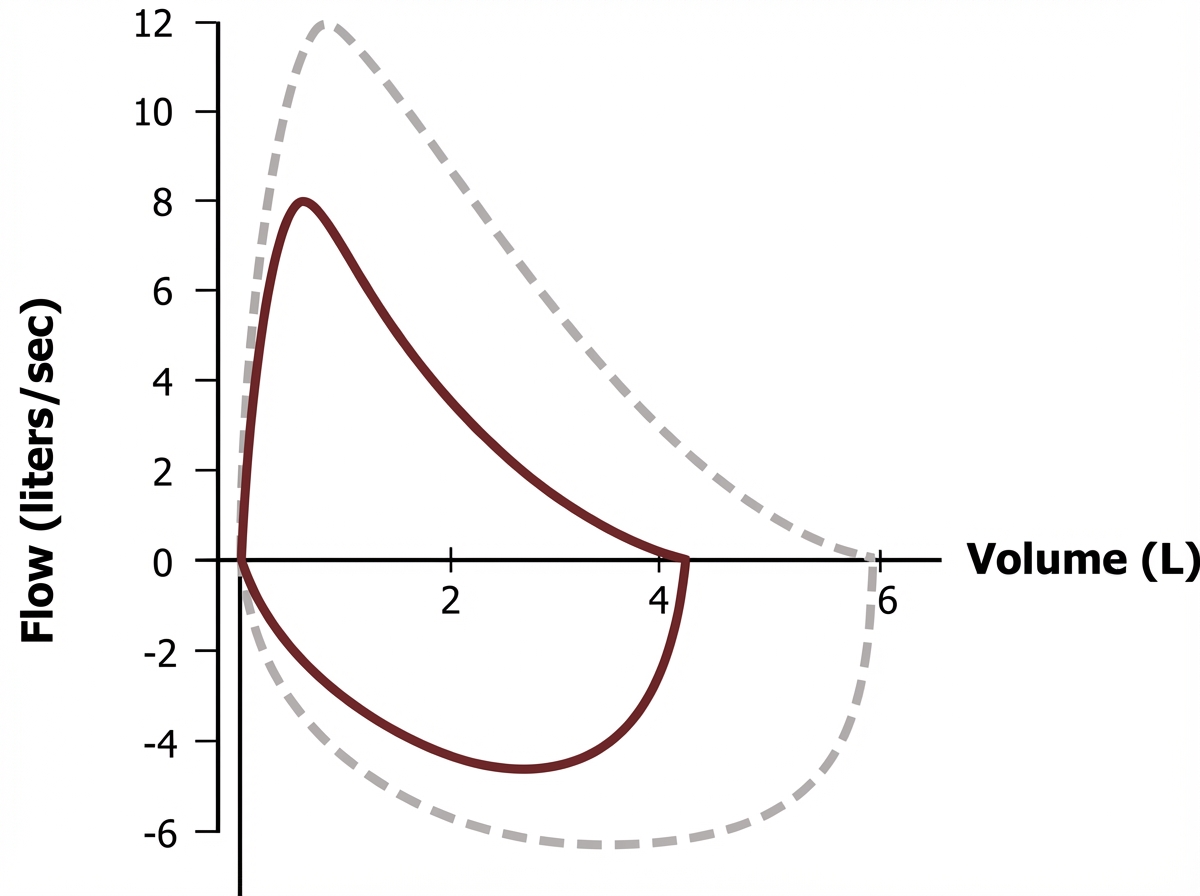
Sarcoidosis US Medical PG Question 1: A 47-year-old woman comes to the physician because of a 3-week history of a dry cough. She does not smoke or use illicit drugs. Physical examination shows mild conjunctival hyperemia. Chest auscultation shows fine crackles in both lung fields. Laboratory studies show a total calcium concentration of 10.8 mg/dL. The results of spirometry are shown (dashed loop shows normal for comparison). Further evaluation of this patient is most likely to show an increase in which of the following?
- A. Mast cell tryptase activity
- B. Monoclonal IgG titers
- C. Angiotensin-converting enzyme activity (Correct Answer)
- D. Cold agglutinin titers
- E. Neutrophil elastase activity
Sarcoidosis Explanation: ***Angiotensin-converting enzyme activity***
- The patient's symptoms (dry cough, crackles, hypercalcemia, conjunctival hyperemia, and restrictive spirometry pattern based on the image description) are classic for **sarcoidosis**.
- **Elevated ACE levels** are a common finding (seen in 60-80% of cases) in sarcoidosis, as the granulomas produce ACE.
*Mast cell tryptase activity*
- This is primarily elevated in **mastocytosis** and severe allergic reactions like **anaphylaxis**.
- The patient's presentation is not consistent with these conditions.
*Monoclonal IgG titers*
- Elevated monoclonal IgG titers are characteristic of **multiple myeloma** or other monoclonal gammopathies.
- While hypercalcemia can occur in multiple myeloma, the pulmonary findings and conjunctival hyperemia point away from this diagnosis.
*Cold agglutinin titers*
- Elevated cold agglutinin titers are associated with infections like **Mycoplasma pneumoniae** or **Epstein-Barr virus**, lymphomas, and some autoimmune diseases.
- The clinical picture (chronic cough, hypercalcemia, conjunctivitis, restrictive lung disease) is not typical for conditions causing cold agglutinins.
*Neutrophil elastase activity*
- Increased neutrophil elastase activity is primarily associated with conditions involving significant **neutrophilic inflammation**, such as **cystic fibrosis** or severe **COPD exacerbations**.
- The patient's presentation does not suggest such a condition; sarcoidosis is characterized by granulomatous inflammation.
Sarcoidosis US Medical PG Question 2: A 35-year-old African-American female presents to the emergency room complaining of chest pain. She also complains of recent onset arthritis and increased photosensitivity. Physical examination reveals bilateral facial rash. Which of the following is most likely to be observed in this patient?
- A. Pain improves with inspiration
- B. High-pitched diastolic murmur
- C. Fixed and split S2
- D. Mid-systolic click
- E. Pain relieved by sitting up and leaning forward (Correct Answer)
Sarcoidosis Explanation: ***Pain relieved by sitting up and leaning forward***
- This patient's symptoms (chest pain, arthritis, photosensitivity, facial rash) are highly suggestive of **systemic lupus erythematosus (SLE)**.
- Among the cardiac manifestations of SLE, **pericarditis** is common. The chest pain of pericarditis is typically relieved by sitting up and leaning forward, as this decreases pressure on the inflamed pericardial sac.
*Pain improves with inspiration*
- This describes **pleuritic chest pain**, which is often associated with conditions like pleurisy or pneumothorax, where inspiration causes stretching of inflamed pleura.
- While pleurisy can occur in SLE, the relief by sitting up and leaning forward is a more classic sign of pericarditis.
*High-pitched diastolic murmur*
- A high-pitched diastolic murmur is characteristic of **aortic regurgitation** or **pulmonic regurgitation**.
- While SLE can cause valvular heart disease (e.g., Libman-Sacks endocarditis, often leading to mitral valve involvement), aortic or pulmonic regurgitation is not the most typical acute cardiac finding associated with these specific chest pain characteristics.
*Fixed and split S2*
- A fixed and split S2 is a classic finding in an **atrial septal defect (ASD)**.
- While rare, SLE can be associated with some congenital heart abnormalities or pulmonary hypertension, but ASD is not a typical direct complication leading to this S2 finding in the context of acute chest pain.
*Mid-systolic click*
- A mid-systolic click is characteristic of **mitral valve prolapse (MVP)**.
- Mitral valve abnormalities, including MVP and mitral regurgitation (due to Libman-Sacks endocarditis), are relatively common in SLE. However, the chest pain associated with pericarditis (relieved by sitting up) is a more direct and common finding given the constellation of symptoms than a mid-systolic click alone.
Sarcoidosis US Medical PG Question 3: A 27-year-old Asian woman presents to her primary care physician with joint pain and a headache. She has had intermittent joint and muscle pain for the past several months in the setting of a chronic headache. She states that the pain seems to migrate from joint to joint, and her muscles typically ache making it hard for her to sleep. The patient's past medical history is non-contributory, and she is currently taking ibuprofen for joint pain. Physical exam is notable for an asymmetrical pulse in the upper extremities. The patient has lost 10 pounds since her previous visit 2 months ago. Laboratory values are notable for an elevated C-reactive protein and erythrocyte sedimentation rate. Which of the following is the best next step in management?
- A. Methotrexate
- B. Recommend exercise and optimize the patient's sleep regimen
- C. Prednisone (Correct Answer)
- D. Temporal artery biopsy
- E. Anti-dsDNA level
Sarcoidosis Explanation: ***Prednisone***
- The patient's presentation with **migratory joint pain**, headache, **asymmetrical pulses**, and elevated inflammatory markers (CRP, ESR) in a young Asian woman suggests **Takayasu arteritis**.
- **Corticosteroids** like prednisone are the cornerstone of initial treatment for active Takayasu arteritis to suppress inflammation and prevent further vascular damage.
*Methotrexate*
- **Methotrexate** is an immunosuppressant often used in conjunction with corticosteroids or as a steroid-sparing agent in rheumatic conditions.
- However, it's not the initial monotherapy of choice for active, severe vasculitis requiring rapid inflammation control.
*Recommend exercise and optimize the patient's sleep regimen*
- While exercise and sleep are important for overall well-being, they do not address the underlying **severe inflammatory vasculitis** and are not an appropriate primary intervention for Takayasu arteritis.
- Delaying proper medical treatment can lead to irreversible vascular damage.
*Temporal artery biopsy*
- A **temporal artery biopsy** is the diagnostic gold standard for **Giant Cell Arteritis (GCA)**, which typically affects older individuals (>50 years).
- The patient's age (27 years) and other clinical features are more consistent with Takayasu arteritis, which affects larger arteries and often presents at a younger age.
*Anti-dsDNA level*
- An **anti-dsDNA level** is a specific marker for **Systemic Lupus Erythematosus (SLE)**.
- While SLE can cause joint pain and headaches, the presence of **asymmetrical pulses** and the demographic (young Asian woman) are more indicative of Takayasu arteritis, not SLE.
Sarcoidosis US Medical PG Question 4: A 32-year-old man comes to the physician for a 1-month history of fever, chest pain with deep breathing, and a 4-kg (9 lb) weight loss. His temperature is 38°C (100.4°F). An x-ray of the chest shows a subpleural nodule in the right lower lobe with right hilar lymphadenopathy. Histological examination of a right hilar lymph node biopsy specimen shows several granulomas with acellular cores. Which of the following is the most likely diagnosis?
- A. Primary tuberculosis (Correct Answer)
- B. Hodgkin lymphoma
- C. Chronic berylliosis
- D. Miliary tuberculosis
- E. Pulmonary sarcoidosis
Sarcoidosis Explanation: ***Primary tuberculosis***
- The combination of **fever**, **chest pain with deep breathing**, **weight loss**, a **subpleural nodule**, **right hilar lymphadenopathy**, and **granulomas with acellular cores** on biopsy strongly points to primary tuberculosis.
- Granulomas in tuberculosis are typically **caseating** (acellular cores often imply caseating necrosis in this context), and the presence of hilar lymphadenopathy with a peripheral nodule (Ghon complex) is classic for primary infection.
*Hodgkin lymphoma*
- While Hodgkin lymphoma can cause fever, weight loss (B symptoms), and lymphadenopathy, the presence of a **subpleural nodule** and **granulomas with acellular cores** is not typical.
- Histology would show **Reed-Sternberg cells** amidst a mixed inflammatory infiltrate, not granulomas with acellular cores.
*Chronic berylliosis*
- This condition is caused by **beryllium exposure** and typically presents with a history of occupational exposure and **non-caseating granulomas**.
- No history of beryllium exposure is provided, and the granulomas described are consistent with **caseating necrosis** (acellular cores).
*Miliary tuberculosis*
- Miliary tuberculosis involves widespread dissemination, often presenting with **diffuse, small nodules** (millet seed-sized) across both lungs on X-ray, rather than a single subpleural nodule and hilar lymphadenopathy.
- While it features granulomas, the **radiological pattern** is distinct.
*Pulmonary sarcoidosis*
- Sarcoidosis is characterized by **non-caseating granulomas** in multiple organs, often presenting with bilateral hilar lymphadenopathy and pulmonary involvement.
- The description of **acellular cores** suggests **caseating granulomas**, which are not typical of sarcoidosis.
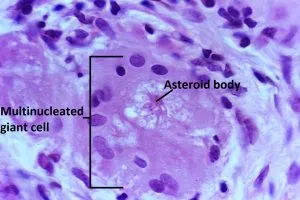
Sarcoidosis US Medical PG Question 5: A 34-year-old woman comes to the physician because of a 6-week history of fever and productive cough with blood-tinged sputum. She has also had a 4-kg (8.8-lb) weight loss during the same time period. Examination shows enlarged cervical lymph nodes. An x-ray of the chest shows a 2.5-cm pulmonary nodule in the right upper lobe. A biopsy specimen of the lung nodule shows caseating granulomas with surrounding multinucleated giant cells. Which of the following is the most likely underlying cause of this patient's pulmonary nodule?
- A. Combined type III/IV hypersensitivity reaction
- B. IgE-mediated mast cell activation
- C. Immune complex deposition
- D. Antibody-mediated cytotoxic reaction
- E. Delayed T cell-mediated reaction (Correct Answer)
Sarcoidosis Explanation: ***Delayed T cell-mediated reaction***
- The presence of **caseating granulomas** with **multinucleated giant cells** is characteristic of tuberculosis, which is mediated by a **Type IV hypersensitivity reaction**.
- This reaction involves **T cells** and **macrophages** forming granulomas to wall off persistent intracellular pathogens.
*Combined type III/IV hypersensitivity reaction*
- While granulomas can sometimes involve aspects of **Type III hypersensitivity** (immune complex deposition), **caseating granulomas** are primarily a feature of **Type IV (delayed T cell-mediated) hypersensitivity**.
- **Type III reactions** are more typically associated with vasculitis or glomerulonephritis, which are not the primary features here.
*IgE-mediated mast cell activation*
- This describes a **Type I hypersensitivity reaction**, responsible for immediate allergic reactions like asthma or anaphylaxis.
- The patient's symptoms (fever, weight loss, productive cough, granulomas) are not consistent with an **IgE-mediated response**.
*Immune complex deposition*
- This is characteristic of a **Type III hypersensitivity reaction**, where antigen-antibody complexes deposit in tissues, leading to inflammation and damage.
- While Type III reactions can cause inflammation, they typically don't manifest as **caseating granulomas** and the chronic, progressive symptoms described.
*Antibody-mediated cytotoxic reaction*
- This describes a **Type II hypersensitivity reaction**, where antibodies directly bind to antigens on cell surfaces, leading to cell lysis (e.g., autoimmune hemolytic anemia).
- The clinical picture of **granulomatous inflammation** is not consistent with a direct **antibody-mediated cytotoxic reaction**.
Sarcoidosis US Medical PG Question 6: An otherwise healthy 27-year-old man presents to his dermatologist because of a rash over his knees. The rash has been present for 5 weeks and is moderately itchy. Physical examination reveals erythematous plaques covered with silvery scales over the extensor surface of the knees as shown in the image. Which of the following is the best initial step in the management of this patient’s condition?
- A. Oral cyclosporine
- B. Oral methotrexate
- C. Skin biopsy
- D. Topical corticosteroids and/or topical vitamin D analog (Correct Answer)
- E. Oral corticosteroids
Sarcoidosis Explanation: ***Topical corticosteroids and/or topical vitamin D analog***
- The patient's presentation with **erythematous plaques** and **silvery scales** on the extensor surfaces of the knees is classic for **plaque psoriasis**.
- For localized, mild-to-moderate plaque psoriasis, **topical corticosteroids** and/or **topical vitamin D analogs** are the first-line treatment due to their effectiveness and favorable side-effect profile.
*Oral cyclosporine*
- **Cyclosporine** is an immunosuppressant typically reserved for **severe, refractory psoriasis** due to its potential for significant side effects, including **nephrotoxicity** and **hypertension**.
- It is not indicated as an initial step for localized psoriasis, especially in an otherwise healthy patient.
*Oral methotrexate*
- **Methotrexate** is a systemic agent used for **moderate to severe psoriasis**, particularly when topical treatments are insufficient or the disease significantly impacts quality of life.
- Its use requires monitoring for potential adverse effects such as **hepatotoxicity** and **myelosuppression**, making it unsuitable as an initial treatment for localized disease.
*Skin biopsy*
- While a **skin biopsy** can confirm the diagnosis of psoriasis, the clinical presentation in this case is highly characteristic, making a biopsy **unnecessary as an initial step** for management initiation.
- A biopsy might be considered if the diagnosis is ambiguous or if the lesions are unresponsive to initial therapy.
*Oral corticosteroids*
- **Oral corticosteroids** are generally **contraindicated** in psoriasis due to the risk of **rebound flares** and potential exacerbation of the condition upon withdrawal.
- They may be used in specific, severe cases but are not suitable as a routine initial treatment for typical plaque psoriasis.
Sarcoidosis US Medical PG Question 7: A 61-year-old construction worker comes to the physician because of a 3-month history of progressively worsening cough and shortness of breath. He has had a 7.5-kg (16.5-lb) weight loss during this period. He smokes occasionally and does not drink alcohol. Physical examination shows clubbing of the fingers. End-inspiratory crackles are heard in both lower lung fields. X-ray of the chest shows bilateral reticulonodular densities with interstitial fibrosis. Histologic examination of a lung biopsy specimen shows noncaseating granulomas in the interstitium. Which of the following is the most likely underlying mechanism of this patient's condition?
- A. Aspergillus-induced eosinophil release
- B. IgE-mediated histamine release
- C. Elastase-mediated parenchymal destruction
- D. IgG-mediated immune complex deposition
- E. Silica-induced macrophage activation (Correct Answer)
Sarcoidosis Explanation: ***Silica-induced macrophage activation***
- The patient's presentation with **progressive cough and shortness of breath**, **weight loss**, **clubbing**, **interstitial crackles**, and **bilateral reticulonodular densities with interstitial fibrosis** in a **construction worker** suggests **silicosis**.
- **Silicosis** is characterized by the inhalation of silica particles, which are then phagocytosed by **macrophages**, leading to their activation, release of inflammatory mediators, and subsequent **granuloma formation** and **fibrosis**.
- Construction workers have occupational exposure to **crystalline silica dust** from cutting, grinding, or drilling concrete, stone, or masonry materials.
*Aspergillus-induced eosinophil release*
- This mechanism is characteristic of **allergic bronchopulmonary aspergillosis (ABPA)**, which typically presents with asthma-like symptoms, recurrent pulmonary infiltrates, and eosinophilia.
- The patient's biopsy showing **noncaseating granulomas without eosinophils** makes ABPA unlikely.
*IgE-mediated histamine release*
- This describes a **Type I hypersensitivity reaction** often seen in **allergic asthma** or anaphylaxis, where IgE antibodies bind to mast cells and basophils, releasing histamine upon allergen exposure.
- This mechanism does not explain the **interstitial fibrosis** and **noncaseating granulomas** observed in the patient's lung biopsy.
*Elastase-mediated parenchymal destruction*
- This mechanism is central to the pathogenesis of **emphysema**, where an imbalance between proteases (like elastase) and antiproteases leads to the destruction of alveolar walls.
- While smoking is a risk factor for emphysema, the imaging findings of **reticulonodular densities** and **interstitial fibrosis**, along with **noncaseating granulomas**, point away from isolated emphysema.
*IgG-mediated immune complex deposition*
- This mechanism (Type III hypersensitivity) is seen in conditions like **hypersensitivity pneumonitis** or some forms of vasculitis.
- **Hypersensitivity pneumonitis** can occur in farmers exposed to organic antigens (e.g., moldy hay causing "Farmer's Lung") and can present with interstitial lung disease and granulomas.
- However, this patient's occupational exposure as a construction worker and the classic histologic finding of **noncaseating granulomas in the interstitium** with the clinical presentation point more strongly to **silicosis** from silica dust exposure rather than hypersensitivity pneumonitis.
Sarcoidosis US Medical PG Question 8: A 49-year-old man comes to the physician because of tender, red nodules that appeared on his chest 3 days ago. Three weeks ago, he had similar symptoms in his right lower limb and another episode in his left foot; both episodes resolved spontaneously. He also has diarrhea and has had a poor appetite for 1 month. He has a history of dry cough and joint pain, for which he takes albuterol and aspirin as needed. He has smoked 2 packs of cigarettes daily for 15 years. He does not drink alcohol. Physical examination shows a linear, erythematous lesion on the right anterior chest wall, through which a cord-like structure can be palpated. The lungs are clear to auscultation. The abdomen is soft, nontender, and non-distended. Examination of the legs is normal. An ultrasound of the legs shows no abnormalities. Which of the following is the most appropriate next step in diagnosis of the underlying condition?
- A. Coagulation studies
- B. Ankle brachial index
- C. Serum angiotensin-converting enzyme level
- D. CT scan of the abdomen
- E. X-ray of the chest (Correct Answer)
Sarcoidosis Explanation: ***X-ray of the chest***
- The patient's migratory thrombophlebitis (Trousseau's syndrome), unexplained diarrhea, weight loss, and chronic cough (despite albuterol) are highly suggestive of an underlying **malignancy**, specifically **pancreatic adenocarcinoma** or **bronchogenic carcinoma**.
- A **chest X-ray** is a crucial initial step to evaluate for a primary lung malignancy, which can often present with paraneoplastic syndromes like migratory thrombophlebitis.
*Coagulation studies*
- While Trousseau's syndrome involves hypercoagulability, obtaining coagulation studies like PT, PTT, or D-dimer would primarily confirm a coagulation abnormality but not identify the **underlying cause** (malignancy).
- The clinical presentation points towards seeking the etiology of the paraneoplastic syndrome, rather than just characterizing the coagulation defect.
*Ankle brachial index*
- An ankle brachial index (ABI) is used to diagnose **peripheral artery disease (PAD)**, which is characterized by claudication and arterial insufficiency.
- The patient's symptoms of migratory thrombophlebitis and palpable cord-like structures are indicative of venous and not arterial pathology, and a normal leg ultrasound rules out deep vein thrombosis.
*Serum angiotensin-converting enzyme level*
- Elevated serum ACE levels are characteristic of **sarcoidosis**, a granulomatous disease that can cause pulmonary symptoms and skin lesions.
- However, sarcoidosis typically does not cause migratory thrombophlebitis, and the diarrhea and weight loss point to a systemic malignant process.
*CT scan of the abdomen*
- While pancreatic adenocarcinoma is a strong consideration given the constellation of symptoms (Trousseau's syndrome, diarrhea, poor appetite/weight loss), a **chest X-ray** is often the first imaging step due to the patient's history of smoking and chronic cough, which raises suspicion for lung cancer.
- If the chest X-ray is negative, then an abdominal CT would be a reasonable next step to investigate for pancreatic or other abdominal malignancies.
Sarcoidosis US Medical PG Question 9: A 33-year-old African-American female presents to her physician with complaints of a persistent, dry cough. She states that the cough has gone on for some time now. Three weeks ago, during her last general checkup, she was started on lisinopril and metformin for concerns regarding an elevated blood pressure and fasting blood glucose. Past medical history is notable for eczema, asthma, and seasonal allergies. At this visit the patient has other non-specific complaints such as fatigue and joint pain as well as a burning sensation in her sternum when she eats large meals. Her physical exam is only notable for painful bumps on her lower extremities (figure A) which the patient attributes to "bumping her shins," during exercise, and an obese habitus. Which of the following is most likely true for this patient's chief concern?
- A. Omeprazole is an appropriate next step in management
- B. Loratadine would best treat her chief complaint
- C. Serum levels of bradykinin will be elevated
- D. Non-caseating granulomas are found on biopsy of mediastinal lymph nodes (Correct Answer)
- E. Beta agonists would relieve this patient's symptoms
Sarcoidosis Explanation: ***Non-caseating granulomas are found on biopsy of mediastinal lymph nodes***
- The patient's symptoms (persistent dry cough, fatigue, joint pain, painful shin bumps consistent with **erythema nodosum**) in an **African-American female** are highly suggestive of **sarcoidosis**.
- **Sarcoidosis** is characterized by the presence of **non-caseating granulomas** in affected organs, commonly the lungs and mediastinal lymph nodes.
*Omeprazole is an appropriate next step in management*
- While the patient has a "burning sensation in her sternum when she eats large meals," suggesting **gastroesophageal reflux disease (GERD)**, this is not her chief complaint.
- Treating GERD with **omeprazole** would address the burning sensation but not the persistent dry cough or other systemic symptoms.
*Loratadine would best treat her chief complaint*
- **Loratadine** is an antihistamine used to treat allergic reactions, including symptoms of seasonal allergies and eczema.
- Although the patient has a history of allergies and asthma, a persistent dry cough with systemic symptoms and erythema nodosum points away from an **allergic cough** as the primary cause.
*Serum levels of bradykinin will be elevated*
- High serum levels of **bradykinin** can cause an ACE inhibitor-induced dry cough, which should be considered given her recent initiation of **lisinopril**.
- However, the presence of **erythema nodosum**, joint pain, and fatigue, combined with a persistent dry cough, makes **sarcoidosis** a more comprehensive diagnosis that explains all her symptoms beyond just the cough.
*Beta agonists would relieve this patient's symptoms*
- **Beta-agonists** are bronchodilators used to relieve bronchospasm in conditions like asthma.
- While the patient has a history of asthma, her cough is described as persistent and dry, and combined with other systemic symptoms, it is less likely to be solely an asthma exacerbation treatable with **beta-agonists**.
Sarcoidosis US Medical PG Question 10: A previously healthy 65-year-old man comes to the physician for chronic left-sided abdominal discomfort. About 3 months ago, he started experiencing early satiety and eating less. He has lost 7 kg (15.4 lb) during this period. He also occasionally has left shoulder pain. He recently retired from his job on a production line at a shoe factory. His pulse is 72/min, blood pressure is 130/70 mm Hg, and temperature is 37.8°C (100.1°F). Physical examination shows nontender, bilateral axillary and right-sided inguinal lymphadenopathy. The spleen is palpated 7 cm below the costal margin. Which of the following is the strongest indicator of a poor prognosis for this patient's condition?
- A. Thrombocytopenia
- B. Lymphocytosis
- C. Bone lesions
- D. BCR-ABL gene
- E. Peripheral lymphadenopathy (Correct Answer)
Sarcoidosis Explanation: ***Peripheral lymphadenopathy***
- The presence of **widespread peripheral lymphadenopathy** (bilateral axillary and inguinal) combined with massive splenomegaly indicates **advanced-stage chronic lymphocytic leukemia (CLL)**.
- In the **Rai staging system**, lymphadenopathy places patients at Stage I-II, and when combined with splenomegaly (Stage II) or organomegaly, indicates **intermediate risk**. Multiple lymph node regions involved suggests more advanced disease.
- In the **Binet staging system**, involvement of ≥3 lymphoid areas (axillary bilateral + inguinal + spleen) places the patient at **Stage B or C**, associated with **poorer prognosis**.
- Extensive lymphadenopathy reflects **higher tumor burden** and is a well-established poor prognostic factor in CLL and low-grade lymphomas.
*Thrombocytopenia*
- While thrombocytopenia in CLL indicates **Rai Stage IV** (highest risk), it is **not mentioned in this patient's presentation**.
- Thrombocytopenia would indeed be a poor prognostic sign if present, but the question asks about findings from the clinical scenario provided.
*Lymphocytosis*
- **Lymphocytosis** is the hallmark laboratory finding in CLL and required for diagnosis.
- However, **isolated lymphocytosis** without lymphadenopathy or organomegaly represents **Rai Stage 0** (low risk) or **Binet Stage A** (best prognosis).
- The **degree of lymphocytosis alone** is not as strong a prognostic indicator as the extent of lymph node and organ involvement.
*Bone lesions*
- **Lytic bone lesions** are characteristic of **multiple myeloma**, not CLL.
- CLL typically causes **bone marrow infiltration** but not destructive bone lesions.
- The clinical presentation (lymphadenopathy, splenomegaly, no bone pain) does not suggest myeloma.
*BCR-ABL gene*
- The **BCR-ABL fusion gene** (Philadelphia chromosome) is the defining feature of **chronic myeloid leukemia (CML)**, not CLL.
- CML typically presents with **marked leukocytosis** (often >100,000/μL), **basophilia**, and massive splenomegaly but **rarely has significant lymphadenopathy**.
- This patient's presentation with **prominent lymphadenopathy** strongly suggests a **lymphoproliferative disorder** (CLL or lymphoma), not CML.
More Sarcoidosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.