Pulmonary function testing interpretation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pulmonary function testing interpretation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pulmonary function testing interpretation US Medical PG Question 1: A 60-year-old woman presents to the clinic with a 3-month history of shortness of breath that worsens on exertion. She also complains of chronic cough that has lasted for 10 years. Her symptoms are worsened even with light activities like climbing up a flight of stairs. She denies any weight loss, lightheadedness, or fever. Her medical history is significant for hypertension, for which she takes amlodipine daily. She has a 70-pack-year history of cigarette smoking and drinks 3–4 alcoholic beverages per week. Her blood pressure today is 128/84 mm Hg. A chest X-ray shows flattening of the diaphragm bilaterally. Physical examination is notable for coarse wheezing bilaterally. Which of the following is likely to be seen with pulmonary function testing?
- A. Decreased FEV1: FVC and decreased total lung capacity
- B. Normal FEV1: FVC and decreased total lung capacity
- C. Increased FEV1: FVC and decreased total lung capacity
- D. Decreased FEV1: FVC and increased total lung capacity (Correct Answer)
- E. Increased FEV1: FVC and normal total lung capacity
Pulmonary function testing interpretation Explanation: ***Decreased FEV1:FVC ratio and increased total lung capacity***
- This patient's symptoms (shortness of breath on exertion, chronic cough, 70-pack-year smoking history, coarse wheezing, and diaphragmatic flattening on X-ray) are highly suggestive of **Chronic Obstructive Pulmonary Disease (COPD)**, specifically **emphysema**, an obstructive lung disease.
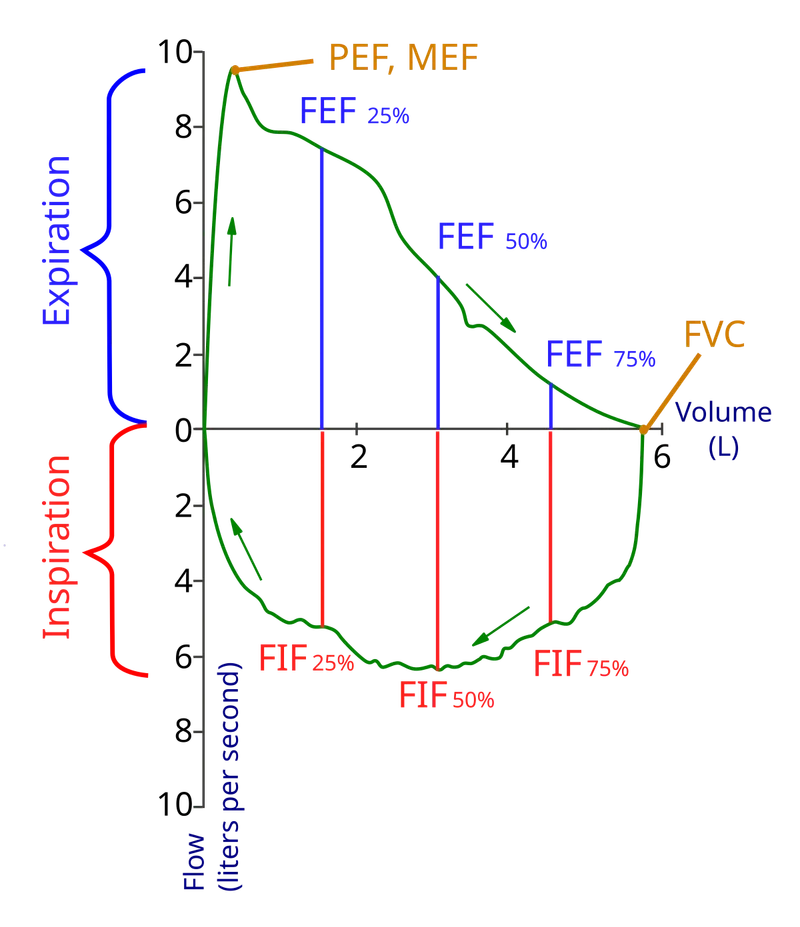
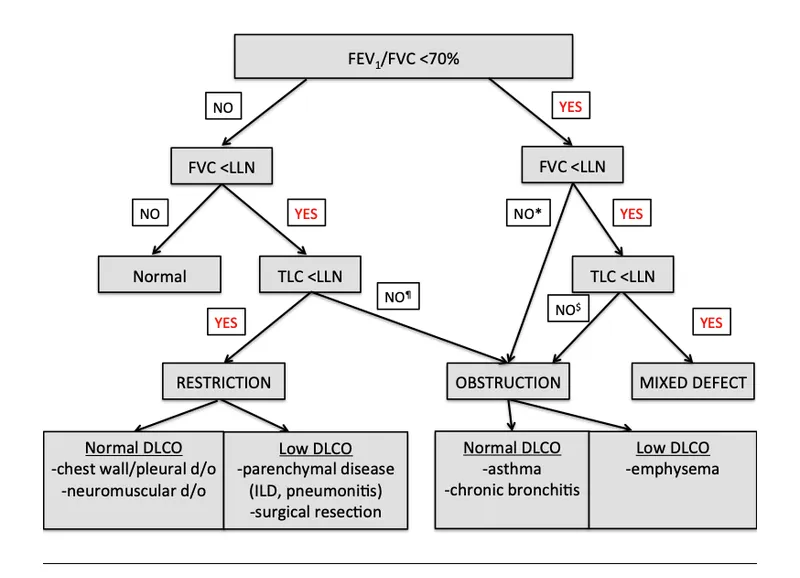
- In COPD, there is airflow limitation, causing a **decreased FEV1:FVC ratio** (typically <0.70). Over time, air trapping occurs due to damaged alveoli and loss of elastic recoil, leading to an **increased total lung capacity (TLC)** and residual volume.
*Decreased FEV1:FVC ratio and decreased total lung capacity*
- A **decreased FEV1:FVC ratio** indicates an **obstructive lung disease**.
- However, a **decreased total lung capacity (TLC)** is characteristic of a **restrictive lung disease**, which does not align with the patient's presentation typical of COPD/emphysema.
*Normal FEV1:FVC ratio and decreased total lung capacity*
- A **normal FEV1:FVC ratio** is inconsistent with the patient's strong history of smoking and symptoms suggestive of airflow obstruction.
- A **decreased total lung capacity (TLC)** indicates a restrictive lung disease, which is not the primary diagnosis here.
*Increased FEV1:FVC ratio and decreased total lung capacity*
- An **increased FEV1:FVC ratio** is not physiologically possible in significant lung disease and is therefore incorrect.
- A **decreased total lung capacity (TLC)** would point towards a restrictive pattern not seen in generalized emphysema.
*Increased FEV1:FVC ratio and normal total lung capacity*
- An **increased FEV1:FVC ratio** is not a characteristic finding in any lung disease and is therefore incorrect.
- A **normal total lung capacity** would not be expected in advanced emphysema where air trapping is prominent.
Pulmonary function testing interpretation US Medical PG Question 2: A 62-year-old man presents to the emergency department for evaluation of a 2-year history of increasing shortness of breath. He also has an occasional nonproductive cough. The symptoms get worse with exertion. The medical history is significant for hypertension and he takes chlorthalidone. He is a smoker with a 40-pack-year smoking history. On physical examination, the patient is afebrile; the vital signs include: blood pressure 125/78 mm Hg, pulse 90/min, and respiratory rate 18/min. The body mass index (BMI) is 31 kg/m2. The oxygen saturation is 94% at rest on room air. A pulmonary examination reveals decreased breath sounds bilaterally, but is otherwise normal with no wheezes or crackles. The remainder of the examination is unremarkable. A chest radiograph shows hyperinflation of both lungs with mildly increased lung markings, but no focal findings. Based on this clinical presentation, which of the following is most likely?
- A. Decreased total lung capacity
- B. Increased DLCO
- C. Metabolic acidosis
- D. FEV1/FVC of 80% with an FEV1 of 82%
- E. FEV1/FVC of 65% (Correct Answer)
Pulmonary function testing interpretation Explanation: ***FEV1/FVC of 65%***
- This patient's symptoms (shortness of breath, nonproductive cough, worsening with exertion), significant smoking history (40-pack-years), and chest X-ray findings (**hyperinflation**, mildly increased lung markings) are highly suggestive of **Chronic Obstructive Pulmonary Disease (COPD)**, particularly **emphysema** given the hyperinflation and decreased breath sounds.
- COPD is characterized by **airflow limitation** that is not fully reversible, which is reflected by a **reduced FEV1/FVC ratio** (typically < 0.7 or < 70%).
*Decreased total lung capacity*
- **Decreased total lung capacity (TLC)** is characteristic of **restrictive lung diseases**, where lung expansion is limited (e.g., pulmonary fibrosis, interstitial lung disease).
- COPD, and especially emphysema, typically presents with **increased TLC** due to air trapping and hyperinflation, not decreased TLC.
*Increased DLCO*
- **Increased DLCO** (diffusing capacity of the lung for carbon monoxide) can be seen in conditions like **pulmonary hemorrhage** or **asthma**.
- In COPD, particularly emphysema, there is destruction of alveolar-capillary membranes, leading to a **decreased DLCO** due to impaired gas exchange.
*Metabolic acidosis*
- **Metabolic acidosis** is not a primary or direct feature of uncomplicated COPD. While severe respiratory failure in later stages might lead to some acid-base disturbances, directly attributing metabolic acidosis as a defining characteristic is incorrect.
- COPD primarily causes **respiratory acidosis** due to CO2 retention in advanced stages.
*FEV1/FVC of 80% with an FEV1 of 82%*
- An **FEV1/FVC ratio of 80%** (or 0.8) and an **FEV1 of 82%** of predicted values are within the normal range and indicate **normal spirometry**.
- This would rule out significant airflow obstruction, which is central to the diagnosis of COPD.
Pulmonary function testing interpretation US Medical PG Question 3: A 50-year-old man presents to the urgent care clinic for 3 hours of worsening cough, shortness of breath, and dyspnea. He works as a long-haul truck driver, and he informs you that he recently returned to the west coast from a trip to Arkansas. His medical history is significant for gout, hypertension, hypercholesterolemia, diabetes mellitus type 2, chronic obstructive pulmonary disease (COPD), and mild intellectual disability. He currently smokes 1 pack of cigarettes/day, drinks a 6-pack of beer/day, and he endorses a past history of injection drug use but currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 23/min. His physical examination shows mild, bilateral, coarse rhonchi, but otherwise clear lungs on auscultation, grade 2/6 holosystolic murmur, and a benign abdominal physical examination. He states that he ran out of his albuterol inhaler 6 days ago and has been meaning to follow-up with his primary care physician (PCP) for a refill. Complete blood count (CBC) and complete metabolic panel are within normal limits. He also has a D-dimer result within normal limits. Which of the following is the most appropriate next step in evaluation?
- A. Chest computed tomography (CT) with contrast
- B. Chest radiographs (Correct Answer)
- C. Pulmonary function tests
- D. Sputum gram stain and culture
- E. Arterial blood gas
Pulmonary function testing interpretation Explanation: ***Chest radiographs***
- A **chest X-ray** is the most appropriate initial imaging study for evaluating acute respiratory symptoms in a patient with a history of COPD and recent exacerbating factors (running out of albuterol). It can help identify common causes like **pneumonia**, **pneumothorax**, or **acute exacerbation of COPD**.
- The patient's presentation with worsening cough, shortness of breath, and dyspnea, particularly in the context of running out of his albuterol inhaler, suggests a primary pulmonary issue that a chest X-ray can quickly assess.
*Chest computed tomography (CT) with contrast*
- A **chest CT with contrast** is more detailed but not the initial diagnostic study in this scenario, especially with a normal D-dimer ruling out pulmonary embolism as a high probability.
- It exposes the patient to **higher radiation** and risks associated with contrast, making it less suitable as a first-line investigation unless the chest X-ray is inconclusive or more specific findings are suspected.
*Pulmonary function tests*
- **Pulmonary function tests (PFTs)** are used to diagnose and monitor chronic lung conditions like COPD, but they are generally not performed in an acute urgent care setting for patients presenting with acute respiratory distress.
- PFTs require patient cooperation and are designed to assess baseline lung function, not to identify the **acute cause** of respiratory decompensation.
*Sputum gram stain and culture*
- A **sputum gram stain and culture** might be considered if there's strong suspicion of a bacterial infection (e.g., fever, purulent sputum), but the patient's current symptoms are more aligned with a COPD exacerbation or other acute pulmonary issue.
- Without clear signs of bacterial infection, this test is **not the most immediate or appropriate first step** in evaluating acute dyspnea, as it requires time for results and may delay more crucial diagnostic steps.
*Arterial blood gas*
- An **arterial blood gas (ABG)** can provide information on oxygenation, ventilation, and acid-base status, which is useful in assessing the severity of respiratory failure.
- However, it's typically ordered after an initial clinical and imaging assessment to quantify the physiological impact of the respiratory distress, rather than being the **very first diagnostic step** to identify the cause.
Pulmonary function testing interpretation US Medical PG Question 4: A 63-year-old man presents to the clinic with fever accompanied by shortness of breath. The symptoms developed a week ago and have been progressively worsening over the last 2 days. He reports his cough is productive of thick, yellow sputum. He was diagnosed with chronic obstructive pulmonary disease 3 years ago and has been on treatment ever since. He quit smoking 10 years ago but occasionally experiences shortness of breath along with chest tightness that improves with the use of an inhaler. However, this time the symptoms seem to be more severe and unrelenting. His temperature is 38.6°C (101.4°F), the respirations are 21/min, the blood pressure is 100/60 mm Hg, and the pulse is 105/min. Auscultation reveals bilateral crackles and expiratory wheezes. His oxygen saturation is 95% on room air. According to this patient’s history, which of the following should be the next step in the management of this patient?
- A. Chest X-ray (Correct Answer)
- B. Arterial blood gases
- C. Bronchoprovocation test
- D. Bronchoscopy
- E. CT scan
Pulmonary function testing interpretation Explanation: ***Chest X-ray***
- A **chest X-ray** is a crucial initial step to evaluate for **pneumonia** or other acute pulmonary processes, given the fever, productive cough, and worsening respiratory symptoms in a patient with COPD [1].
- It can identify infiltrates, effusions, or other anatomical changes that explain the patient's acute decompensation [1].
*Arterial blood gases*
- While important for assessing **respiratory failure** and guiding ventilator management, **ABGs** are usually performed after initial imaging to quantify gas exchange abnormalities once an etiology is suspected [1].
- The patient's **oxygen saturation of 95% on room air** does not immediately suggest severe hypoxemia, although hypercapnia could still be present.
*Bronchoprovocation test*
- A **bronchoprovocation test** is used to diagnose **asthma** or assess **airway hyperresponsiveness** in stable patients.
- It is contraindicated in acute exacerbations due to the risk of worsening bronchoconstriction.
*Bronchoscopy*
- **Bronchoscopy** is an invasive procedure typically reserved for cases of suspicion of **tumor**, **foreign body aspiration**, or non-resolving infiltrates and would not be the immediate next step for fever and productive cough.
- It is not indicated for the initial diagnosis of community-acquired pneumonia or COPD exacerbation.
*CT scan*
- A **CT scan** provides more detailed imaging but is usually reserved for cases where the chest X-ray is inconclusive or to look for specific pathologies like **pulmonary embolism** or **bronchiectasis**.
- It's not the initial imaging choice for suspected **pneumonia** due to cost, radiation exposure, and the adequacy of X-ray for this purpose [1].
Pulmonary function testing interpretation US Medical PG Question 5: A 36-year-old man is seen in the emergency department for back pain that has been getting progressively worse over the last 4 days. Upon further questioning, he also notes that he has been having a tingling and burning sensation rising up from his feet to his knees bilaterally. The patient states he is having difficulty urinating and having bowel movements over the last several days. His temperature is 97.4°F (36.3°C), blood pressure is 122/80 mmHg, pulse is 85/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for weak leg flexion bilaterally along with decreased anal sphincter tone. Which of the following is the best next step in management?
- A. Emergency surgery
- B. CT
- C. Pulmonary function tests
- D. Lumbar puncture
- E. MRI (Correct Answer)
Pulmonary function testing interpretation Explanation: ***MRI***
- The patient's symptoms (back pain, ascending paresthesias, bladder/bowel dysfunction, and decreased anal sphincter tone) are highly suggestive of **cauda equina syndrome**. An **MRI of the spine** is the gold standard for diagnosing this condition, as it can visualize the spinal cord and nerve roots directly.
- Early diagnosis and intervention with MRI are crucial to prevent **permanent neurological deficits** in cauda equina syndrome.
*Emergency surgery*
- While emergency surgery might be the next step *after* diagnosis, it is **not the initial diagnostic step**. The cause of the cauda equina syndrome (e.g., disc herniation, tumor) must first be identified.
- Performing surgery without proper imaging could lead to operating on the wrong level or for the wrong pathology.
*CT*
- A **CT scan** can provide information about bony structures but is generally **inferior to MRI** for visualizing soft tissue structures like the spinal cord, nerve roots, and intervertebral discs, which are critical in cauda equina syndrome.
- It may miss subtle compressions or pathologies of the nerve roots.
*Pulmonary function tests*
- **Pulmonary function tests** are used to assess lung function and are **irrelevant** to the patient's acute neurological symptoms and back pain.
- This test would not provide any diagnostic information for suspected cauda equina syndrome.
*Lumbar puncture*
- A **lumbar puncture** is primarily used to analyze cerebrospinal fluid for conditions like infection or inflammation (e.g., meningitis, Guillain-Barré syndrome).
- While Guillain-Barré can cause ascending paralysis, the prominent back pain, bowel/bladder dysfunction, and decreased anal sphincter tone make **cauda equina syndrome** a more likely diagnosis, for which LP is not the primary diagnostic tool.
Pulmonary function testing interpretation US Medical PG Question 6: A 27-year-old man presents to the emergency department with back pain. The patient states that he has back pain that has been steadily worsening over the past month. He states that his pain is worse in the morning but feels better after he finishes at work for the day. He rates his current pain as a 7/10 and says that he feels short of breath. His temperature is 99.5°F (37.5°C), blood pressure is 130/85 mmHg, pulse is 80/min, respirations are 14/min, and oxygen saturation is 99% on room air. On physical exam, you note a young man who does not appear to be in any distress. Cardiac exam is within normal limits. Pulmonary exam is notable only for a minor decrease in air movement bilaterally at the lung bases. Musculoskeletal exam reveals a decrease in mobility of the back in all four directions. Which of the following is the best initial step in management of this patient?
- A. MRI of the sacroiliac joint (Correct Answer)
- B. CT scan of the chest
- C. Pulmonary function tests
- D. Ultrasound
- E. Radiography of the lumbosacral spine
Pulmonary function testing interpretation Explanation: ***MRI of the sacroiliac joint***
- The patient's symptoms of **worsening back pain**, morning stiffness that improves with activity, and decreased back mobility are highly suggestive of **ankylosing spondylitis**.
- **MRI** is the most sensitive imaging modality for detecting early inflammatory changes in the **sacroiliac joints** and spine, which are characteristic of ankylosing spondylitis, even before radiographic changes are visible.
*CT scan of the chest*
- While the patient reports feeling **short of breath**, his vital signs and oxygen saturation are normal, and he does not appear in acute distress.
- A CT scan of the chest would be a more appropriate step if there were clearer signs of acute pulmonary pathology, such as significant hypoxemia, fever, or adventitious lung sounds, which are not present here.
*Pulmonary function tests*
- **Shortness of breath** could eventually be a complication of severe ankylosing spondylitis due to restricted chest wall expansion.
- However, PFTs are generally not the *initial* diagnostic step given the primary presentation of back pain and the need to confirm the underlying rheumatologic condition first.
*Ultrasound*
- **Ultrasound** is not a primary imaging modality for evaluating the sacroiliac joints or the spine in the context of suspected ankylosing spondylitis.
- It could be useful for assessing peripheral joint inflammation in other arthropathies, but not for axial involvement.
*Radiography of the lumbosacral spine*
- **X-rays of the lumbosacral spine** might show changes in advanced ankylosing spondylitis (e.g., squaring of vertebrae, syndesmophytes), but they are often normal in the early stages of the disease.
- **MRI** is superior for detecting early inflammatory changes and is often used to diagnose the condition before radiographic damage is evident.
Pulmonary function testing interpretation US Medical PG Question 7: A 65-year-old man is brought to the emergency department with central chest pain for the last hour. He rates his pain as 8/10, dull in character, and says it is associated with profuse sweating and shortness of breath. He used to have heartburn and upper abdominal pain associated with food intake but had never experienced chest pain this severe. He has a history of diabetes, hypertension, and hypercholesterolemia. His current medication list includes amlodipine, aspirin, atorvastatin, insulin, valsartan, and esomeprazole. He has smoked 1 pack of cigarettes per day for the past 35 years. Physical examination reveals: blood pressure 94/68 mm Hg, pulse 112/min, oxygen saturation 95% on room air, and BMI 31.8 kg/m2. His lungs are clear to auscultation. An electrocardiogram (ECG) shows ST-segment elevations in the inferior leads. The patient is discharged home after 3 days on aspirin, clopidogrel, and atenolol in addition to his previous medications. He is advised to get an exercise tolerance test (ETT) in one month. A month later at his ETT, his resting blood pressure is 145/86 mm Hg. The pre-exercise ECG shows normal sinus rhythm with Q waves in the inferior leads. After 3 minutes of exercise, the patient develops chest pain that is gradually worsening, and repeat blood pressure is 121/62 mm Hg. No ischemic changes are noted on the ECG. What is the most appropriate next step?
- A. Stop exercise and order a coronary angiography (Correct Answer)
- B. Stop exercise and order a pharmacological stress test
- C. Stop exercise and order an echo stress test
- D. Continue exercise since ECG does not show ischemic changes
- E. Repeat exercise tolerance testing after one month
Pulmonary function testing interpretation Explanation: **Stop exercise and order a coronary angiography**
- The patient's developing chest pain during the exercise tolerance test, despite no ECG changes, is highly suggestive of **myocardial ischemia** due to his extensive cardiac risk factors and prior STEMI. The **drop in blood pressure** during exercise indicates possible cardiac dysfunction or severe ischemia, making immediate investigation with **coronary angiography** critical.
- Given the patient's strong history of coronary artery disease (CAD), including a recent myocardial infarction, an exercise-induced symptom warrants immediate and definitive evaluation for **obstructive CAD** to guide further management.
*Stop exercise and order a pharmacological stress test*
- While pharmacological stress tests are useful for patients unable to exercise, this patient is already undergoing an exercise test and has demonstrated a symptom during exertion.
- A pharmacological stress test would provide functional information but would not directly image the coronary arteries, which is crucial given the high suspicion for severe CAD.
*Stop exercise and order an echo stress test*
- An echo stress test would assess wall motion abnormalities indicative of ischemia, but similar to other stress tests, it provides functional information rather than direct anatomical visualization of coronary blockages.
- While valuable, in the context of this patient's acute symptoms and risk profile, **coronary angiography** offers a more direct and definitive diagnostic approach to identify and potentially intervene on arterial blockages.
*Continue exercise since ECG does not show ischemic changes*
- Continuing exercise when a patient develops chest pain and a drop in blood pressure is **contraindicated** and dangerous.
- **Symptoms (chest pain)** and **hemodynamic changes (blood pressure drop)** are critical indicators of ischemia, even if ECG changes are absent, as ECG sensitivity for detecting ischemia is not 100%.
*Repeat exercise tolerance testing after one month*
- Repeating the test ignores the significant and alarming symptoms the patient experienced during this test.
- It would delay definitive diagnosis and treatment, putting the patient at unnecessarily high risk of another cardiac event.
Pulmonary function testing interpretation US Medical PG Question 8: A 55-year-old man with recurrent pneumonia comes to the physician for a follow-up examination one week after hospitalization for pneumonia. He feels well but still has a productive cough. He has smoked 1 pack of cigarettes daily for 5 years. His temperature is 36.9°C (98.4°F) and respirations are 20/min. Cardiopulmonary examination shows coarse crackles at the right lung base. Microscopic examination of a biopsy specimen of the right lower lung parenchyma shows proliferation of clustered, cuboidal, foamy-appearing cells. These cells are responsible for which of the following functions?
- A. Mucus secretion
- B. Cytokine release
- C. Lecithin production (Correct Answer)
- D. Toxin degradation
- E. Gas diffusion
Pulmonary function testing interpretation Explanation: ***Lecithin production***
- The description of **clustered, cuboidal, foamy-appearing cells** in the lung parenchyma strongly suggests **Type II pneumocytes**.
- **Type II pneumocytes** are primarily responsible for producing and secreting **pulmonary surfactant**, which is rich in **lecithin (phosphatidylcholine)**, to reduce surface tension in the alveoli.
*Mucus secretion*
- **Goblet cells** and **submucosal glands** in the airways are responsible for mucus secretion, not the alveolar cells described.
- Mucus functions to trap particles and pathogens, preventing them from reaching the alveoli.
*Cytokine release*
- While various lung cells, including macrophages and epithelial cells, can release cytokines in response to inflammation or infection, it is not the primary defining function of Type II pneumocytes.
- **Cytokine release** is a broad immune response, not specific to the unique morphology and function described.
*Toxin degradation*
- The liver and kidneys are the primary organs for **toxin degradation** and excretion, though some detoxification can occur in the lungs.
- This function is not characteristic of **Type II pneumocytes**, which are focused on surfactant production and alveolar repair.
*Gas diffusion*
- **Gas diffusion** primarily occurs across the **Type I pneumocytes** (squamous alveolar cells) and the capillary endothelial cells due to their thinness and large surface area.
- **Type II pneumocytes** are thicker and less involved in direct gas exchange.
Pulmonary function testing interpretation US Medical PG Question 9: A father brings his 3-year-old son to the pediatrician because he is concerned about his health. He states that throughout his son's life he has had recurrent infections despite proper treatment and hygiene. Upon reviewing the patient's chart, the pediatrician notices that the child has been infected multiple times with S. aureus, Aspergillus, and E. coli. Which of the following would confirm the most likely cause of this patient's symptoms?
- A. Increased IgM, Decreased IgG, IgA, and IgE
- B. Negative nitroblue-tetrazolium test (Correct Answer)
- C. Positive nitroblue-tetrazolium test
- D. Normal dihydrorhodamine (DHR) flow cytometry test
- E. Increased IgE and IgA, Decreased IgM
Pulmonary function testing interpretation Explanation: ***Negative nitroblue-tetrazolium test***
- A **negative nitroblue-tetrazolium (NBT) test** indicates an inability of phagocytes to produce a respiratory burst, which is characteristic of **Chronic Granulomatous Disease (CGD)**.
- CGD patients suffer from recurrent infections with catalase-positive organisms such as *Staphylococcus aureus*, *Aspergillus*, and *E. coli*, consistent with the patient's history.
*Increased IgM, Decreased IgG, IgA, and IgE*
- This pattern of immunoglobulin levels is characteristic of **X-linked hyper-IgM syndrome**, where there is a defect in CD40L on T cells.
- While it also causes recurrent infections, the typical pathogens differ from those stated in the question, often including *Pneumocystis jirovecii*.
*Positive nitroblue-tetrazolium test*
- A **positive NBT test** indicates that phagocytes are capable of producing a respiratory burst and forming superoxide, thus ruling out CGD.
- This result would be expected in a healthy individual or someone with an immunodeficiency not affecting the phagocytic oxidative burst.
*Normal dihydrorhodamine (DHR) flow cytometry test*
- A **normal DHR flow cytometry test** indicates that neutrophils can produce reactive oxygen species (ROS) effectively, meaning the respiratory burst is intact.
- This result would rule out CGD, as CGD patients have an abnormal (decreased) DHR test.
*Increased IgE and IgA, Decreased IgM*
- This specific pattern of immunoglobulin abnormalities is not typically associated with a single, well-defined primary immunodeficiency that would present with the described infections.
- **Hyper-IgE syndrome (Job's syndrome)**, for example, features very high IgE levels but usually a normal IgM.
Pulmonary function testing interpretation US Medical PG Question 10: A 68-year-old, overweight gentleman with a 20-pack-year history of smoking presents to the primary care physician after noticing multiple blood-stained tissues after coughing attacks in the last month. His vital signs are within normal limits except for an O2 saturation of 93% on room air. He states that over the last 5 years his cough has continued to worsen and has never truly improved. He states that his shortness of breath has also worsened over this time period, as now he can barely make it up the flight of stairs in his home. In this patient, what is the most likely cause of his hemoptysis?
- A. Chronic bronchitis
- B. Bronchogenic carcinoma (Correct Answer)
- C. Lung abscess
- D. Acute pulmonary edema
- E. Goodpasture's disease
Pulmonary function testing interpretation Explanation: ***Bronchogenic carcinoma (Lung cancer)***
- **Hemoptysis in a smoker is lung cancer until proven otherwise** - this is a critical clinical principle in respiratory medicine.
- This patient has major risk factors: **20-pack-year smoking history**, age 68, and chronic progressive symptoms.
- **Hemoptysis** is a common presenting symptom of lung cancer, occurring in 20-50% of patients, caused by tumor invasion of bronchial vessels.
- The **chronic progressive dyspnea** and **worsening cough over 5 years** suggest an evolving mass lesion or bronchial obstruction.
- **Hypoxemia** (O2 sat 93%) indicates significant pulmonary compromise.
- While this patient likely has underlying COPD/chronic bronchitis as a comorbidity, the presence of hemoptysis mandates urgent evaluation for malignancy.
*Chronic bronchitis*
- While this patient likely has chronic bronchitis (a type of COPD) given the smoking history and chronic productive cough, **hemoptysis is NOT a typical feature** of uncomplicated chronic bronchitis.
- Hemoptysis in chronic bronchitis is rare and usually minimal; its presence should prompt investigation for other causes, particularly malignancy.
- Chronic bronchitis explains the dyspnea and chronic cough but does not explain the hemoptysis.
*Lung abscess*
- A lung abscess typically presents with **acute onset of fever**, chills, night sweats, and **foul-smelling purulent sputum**, none of which are mentioned in this case.
- The **chronic, progressive nature over five years** is inconsistent with an acute infectious process.
*Acute pulmonary edema*
- Acute pulmonary edema presents with **sudden onset of severe dyspnea**, orthopnea, and often pink frothy sputum due to acute cardiac decompensation.
- The **gradual progression over five years** rules out an acute cardiac event.
- Vital signs are stable, with no mention of cardiac findings.
*Goodpasture's disease*
- This rare autoimmune disorder causes **pulmonary-renal syndrome** with glomerulonephritis and pulmonary hemorrhage.
- Typically affects younger patients (20s-30s) with acute presentation.
- There are **no renal symptoms** (hematuria, oliguria, elevated creatinine) to suggest this diagnosis.
More Pulmonary function testing interpretation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.