Interstitial lung disease classification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Interstitial lung disease classification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Interstitial lung disease classification US Medical PG Question 1: A 61-year-old male presents to your office with fever and dyspnea on exertion. He has been suffering from chronic, non-productive cough for 1 year. You note late inspiratory crackles on auscultation. Pulmonary function tests reveal an FEV1/FVC ratio of 90% and an FVC that is 50% of the predicted value. Which of the following would you most likely see on a biopsy of this patient's lung?
- A. Arteriovenous malformations
- B. Hyaline membranes
- C. Charcot-Leyden crystals
- D. Subpleural cystic enlargement (Correct Answer)
- E. Linear immunofluorescence along alveolar basement membranes
Interstitial lung disease classification Explanation: ***Subpleural cystic enlargement***
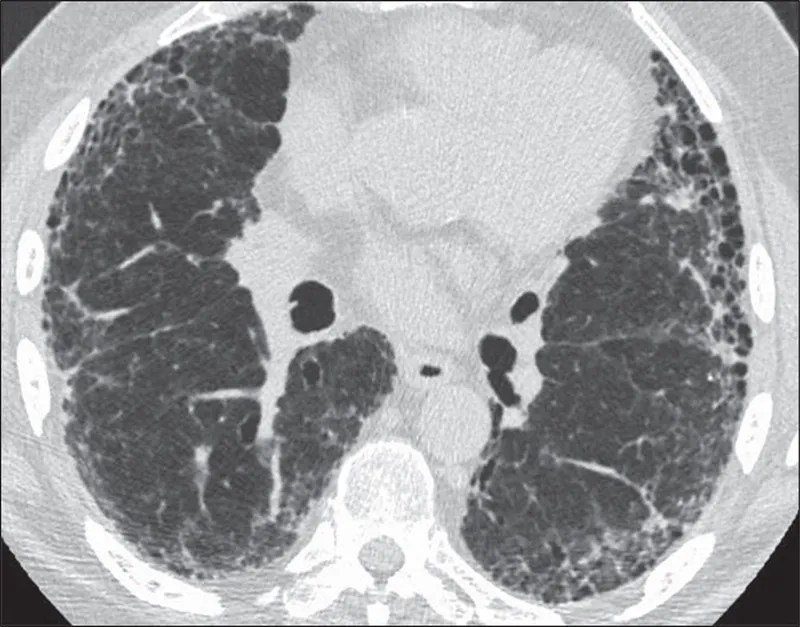
- The patient's presentation with **dyspnea, non-productive cough, late inspiratory crackles**, and **restrictive lung disease** (normal FEV1/FVC ratio of 90% with reduced FVC of 50%) is highly suggestive of **pulmonary fibrosis**.
- **Subpleural cystic enlargement** (honeycombing) is the characteristic histological finding in advanced pulmonary fibrosis, particularly in the **usual interstitial pneumonia (UIP)** pattern seen in **idiopathic pulmonary fibrosis (IPF)**.
- The chronic, progressive nature (1-year history) and the restrictive PFT pattern make this the most likely biopsy finding.
*Arteriovenous malformations*
- These are abnormal vascular connections between arteries and veins that can cause **hypoxemia** and are typically associated with **hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease)**.
- They do not explain the restrictive PFT pattern or the typical presentation of chronic progressive fibrosis with late inspiratory crackles.
*Linear immunofluorescence along alveolar basement membranes*
- This finding on **direct immunofluorescence** with **IgG deposition** is characteristic of **Goodpasture syndrome** (anti-GBM disease), which causes pulmonary hemorrhage and rapidly progressive glomerulonephritis.
- This condition presents with **hemoptysis** and **acute renal failure**, not chronic non-productive cough, and would show an obstructive or mixed pattern if hemorrhage were present.
*Hyaline membranes*
- **Hyaline membranes** are proteinaceous material lining alveoli seen in **acute respiratory distress syndrome (ARDS)** or **diffuse alveolar damage (DAD)**.
- The patient's **chronic 1-year symptoms** and restrictive PFTs indicate chronic interstitial lung disease, not acute lung injury.
*Charcot-Leyden crystals*
- **Charcot-Leyden crystals** are formed from breakdown of **eosinophils** and are found in conditions with eosinophilic inflammation, such as **asthma** or **eosinophilic pneumonia**.
- While these conditions can cause cough and dyspnea, they would typically show an **obstructive pattern** (reduced FEV1/FVC) in asthma, not the restrictive pattern seen here.
Interstitial lung disease classification US Medical PG Question 2: A 46-year-old woman comes to the physician with a 4-month history of lethargy. She has had joint pain for the past 15 years and does not have a primary care physician. Her temperature is 37.4°C (99.3°F), pulse is 97/min, and blood pressure is 132/86 mm Hg. Physical examination shows pallor of the oral mucosa and nontender subcutaneous nodules on both elbows. The distal interphalangeal joints of both hands are flexed and the proximal interphalangeal joints appear hyperextended. Range of motion in the fingers is restricted. The liver span is 6 cm and the spleen tip is palpated 4 cm below the left costal margin. Laboratory studies show:
Hematocrit 33%
Leukocyte count 1,800/mm3
Segmented neutrophils 35%
Lymphocytes 60%
Platelet count 130,000/mm3
Increased serum titers of which of the following is most specific for this patient's condition?
- A. Anti-U1-RNP antibody
- B. Rheumatoid factor
- C. Antinuclear antibody
- D. Anti-CCP antibody (Correct Answer)
- E. Anti-Sm antibody
Interstitial lung disease classification Explanation: ***Anti-CCP antibody***
- The patient's presentation with **long-standing joint pain**, **nodules**, specific finger deformities (**swan neck deformity** - PIP hyperextension with DIP flexion), **splenomegaly**, and **pancytopenia** (WBC 1,800/mm³, platelets 130,000/mm³, hematocrit 33%) is highly suggestive of **Felty's syndrome**, a severe complication of **rheumatoid arthritis (RA)**.
- **Anti-CCP antibodies** are highly specific for RA (over 95% specificity) and can be present years before symptoms develop, making them the most specific marker for this condition.
*Anti-U1-RNP antibody*
- This antibody is characteristic of **mixed connective tissue disease (MCTD)**, which presents with overlapping features of SLE, systemic sclerosis, and polymyositis.
- While joint pain can occur in MCTD, the classic deformities, nodule presence, and specific hematologic findings (leukopenia, thrombocytopenia, anemia) better align with Felty's syndrome due to rheumatoid arthritis.
*Rheumatoid factor*
- **Rheumatoid factor (RF)** is positive in about 80% of RA patients, but it is less specific than anti-CCP antibodies as it can be elevated in other autoimmune diseases, chronic infections, and even in healthy individuals.
- While likely positive in this patient, its lower specificity means it's not the *most* specific marker compared to anti-CCP antibodies.
*Antinuclear antibody*
- **Antinuclear antibody (ANA)** is a screening test for various autoimmune diseases, particularly **systemic lupus erythematosus (SLE)**, and is positive in many systemic autoimmune conditions.
- Its high sensitivity but low specificity (positive in other conditions and even in 5-10% of the healthy population) means it is not the most specific marker for this patient's condition.
*Anti-Sm antibody*
- **Anti-Smith (Sm) antibody** is highly specific for **systemic lupus erythematosus (SLE)**.
- The patient's clinical picture, particularly the long history of joint pain with specific deformities and subcutaneous nodules, is not typical for SLE, making anti-Sm antibody an unlikely specific finding.
Interstitial lung disease classification US Medical PG Question 3: A 36-year-old man presents with increasing shortness of breath for a month, which is aggravated while walking and climbing up the stairs. He also complains of pain and stiffness in both wrists, and the distal interphalangeal and metacarpophalangeal joints of both hands. He was diagnosed with rheumatoid arthritis 6 months ago and was started on methotrexate with some improvement. He is a lifetime non-smoker and has no history of drug abuse. The family history is insignificant for any chronic disease. The blood pressure is 135/85 mm Hg, pulse rate is 90/min, temperature is 36.9°C (98.5°F), and the respiratory rate is 22/min. Physical examination reveals short rapid breathing with fine end-inspiratory rales. An echocardiogram is normal with an ejection fraction of 55%. A chest X-ray shows diffuse bilateral reticular markings with multiple pulmonary nodules. Which of the following is the most likely cause of this patient’s lung condition?
- A. Idiopathic pulmonary fibrosis
- B. Cardiogenic pulmonary edema
- C. Granulomatous lung disease
- D. Drug-induced pulmonary disease (Correct Answer)
- E. Radiation-induced pulmonary disease
Interstitial lung disease classification Explanation: ***Drug-induced pulmonary disease***
- The patient's recent diagnosis of **rheumatoid arthritis** and initiation of **methotrexate** are key clues, as methotrexate is a common cause of drug-induced pneumonitis.
- Symptoms like **shortness of breath**, **fine inspiratory rales**, and chest X-ray findings of **bilateral reticular markings** and **pulmonary nodules** are consistent with drug-induced lung injury.
*Idiopathic pulmonary fibrosis*
- This condition typically affects **older adults** (over 50) and progresses slowly, which is less consistent with the patient's age and the relatively rapid onset of symptoms.
- While it causes **reticular markings**, the presence of multiple **pulmonary nodules** makes it less likely.
*Cardiogenic pulmonary edema*
- The **normal echocardiogram** with an ejection fraction of 55% rules out significant cardiac dysfunction as the cause of pulmonary edema.
- This condition would also primarily show **interstitial and alveolar edema**, not nodules or prominent reticular markings without signs of heart failure.
*Granulomatous lung disease*
- This category includes conditions like **sarcoidosis** or **tuberculosis**, which can cause nodules and reticular changes.
- However, there are no other clinical features (e.g., hilar lymphadenopathy, erythema nodosum, or signs of infection) to specifically suggest a granulomatous process in this context, and the history of recent drug initiation is a stronger lead.
*Radiation-induced pulmonary disease*
- The patient has no history of **radiation exposure** to the chest, which is a prerequisite for this diagnosis.
- This condition typically occurs within 6 months of radiation therapy and presents with symptoms localized to the irradiated field.
Interstitial lung disease classification US Medical PG Question 4: A 65-year-old male engineer presents to the office with shortness of breath on exertion and a dry cough that he has had for about a year. He is a heavy smoker with a 25-pack-years history. His vitals include: heart rate 95/min, respiratory rate 26/min, and blood pressure 110/75 mm Hg. On examination, he presents with nail clubbing and bilateral and persistent crackling rales. The chest radiograph shows basal reticulonodular symmetric images, with decreased lung fields. The pulmonary function tests show the following: diffusing capacity of the lungs for carbon monoxide (DLCO) is 43% and reference SaO2 is 94% and 72%, at rest and with exercise, respectively. What is the most likely diagnosis?
- A. Chronic hypersensitivity pneumonitis
- B. Pulmonary Langerhans cell histiocytosis
- C. Pleuropulmonary fibroelastosis
- D. Asbestosis
- E. Idiopathic pulmonary fibrosis (Correct Answer)
Interstitial lung disease classification Explanation: ***Idiopathic pulmonary fibrosis***
- This patient's presentation with **progressive dyspnea**, **dry cough**, **clubbing**, and **basal crackles (rales)**, combined with restrictive lung physiology (low **DLCO**) and **basal reticulonodular infiltrates** on CXR, is highly characteristic of **idiopathic pulmonary fibrosis**. The marked **desaturation with exercise** further supports this diagnosis.
- While smoking is a risk factor, the pattern of lung disease is consistent with IPF, a chronic, progressive, fibrosing interstitial pneumonia of unknown cause.
*Chronic hypersensitivity pneumonitis*
- This condition is caused by **chronic exposure to inhaled antigens** and typically presents with symptoms that link back to the exposure, potentially resolving with avoidance.
- While it can cause interstitial lung disease, the absence of an identifiable antigen exposure and the typical fibrotic pattern with subpleural honeycombing would make IPF more likely.
*Pulmonary Langerhans cells histiocytosis*
- This disease is strongly associated with **smoking** but typically presents with **cysts and nodules** predominantly in the **upper and middle lung fields** on imaging.
- The patient's **basal reticulonodular pattern** with decreased lung fields on CXR, rather than cysts, makes this diagnosis less likely.
*Pleuropulmonary fibroelastosis*
- This is a rare interstitial lung disease characterized by **fibrosis predominantly affecting the upper lobes** and pleura.
- The patient's **basal predominant findings** on chest radiograph and crackles make this diagnosis less consistent.
*Asbestosis*
- Although the patient's occupation as an engineer could suggest **asbestos exposure**, the description lacks specific features like **pleural plaques** or calcifications.
- While asbestosis can cause diffuse interstitial fibrosis and similar symptoms, the clinical and radiological picture, especially the extent of **DLCO reduction** for the given findings, more strongly points to IPF.
Interstitial lung disease classification US Medical PG Question 5: A 41-year-old woman presents to urgent care with complaints of a new rash. On review of systems, she endorses ankle pain bilaterally. Otherwise, she has no additional localized complaints. Physical examination reveals numerous red subcutaneous nodules overlying her shins, bilaterally. Complete blood count shows leukocytes 7,300, Hct 42.0%, Hgb 14.0 g/dL, mean corpuscular volume (MCV) 88 fL, and platelets 209. Chest radiography demonstrates bilateral hilar adenopathy with clear lungs. Which of the following is the most likely diagnosis?
- A. Yersiniosis
- B. Coccidioidomycosis
- C. Histoplasmosis
- D. Chlamydophila pneumoniae
- E. Sarcoidosis (Correct Answer)
Interstitial lung disease classification Explanation: ***Sarcoidosis***
- The combination of **erythema nodosum** (red subcutaneous nodules on shins), **bilateral hilar adenopathy**, and **ankle arthralgia** (ankle pain) in a young woman is highly characteristic of **Lofgren's syndrome**, a common acute presentation of sarcoidosis.
- While other conditions can cause hilar adenopathy or erythema nodosum, the triad presented makes sarcoidosis the most likely diagnosis.
*Yersiniosis*
- Can cause **erythema nodosum** and arthralgia, but **bilateral hilar adenopathy** is not a typical feature of *Yersinia* infection.
- Often associated with **gastrointestinal symptoms** (e.g., diarrhea) which are not mentioned here.
*Coccidioidomycosis*
- Can cause **erythema nodosum** and affect the lungs, but typically presents with **pulmonary infiltrates** or **nodules**, not just isolated bilateral hilar adenopathy.
- Endemic to specific geographic regions (e.g., southwestern US), which is not specified but relevant for exposure.
*Histoplasmosis*
- Can cause **hilar adenopathy** and **erythema nodosum**, especially in acute disseminated forms.
- However, it's more common in individuals exposed to **bird or bat droppings** (Ohio and Mississippi River valleys), and a fungal infection would likely present with more systemic symptoms or specific lung findings beyond just hilar adenopathy.
*Chlamydophila pneumoniae*
- This atypical bacterial infection can cause respiratory symptoms and, rarely, reactive arthritis or erythema nodosum.
- However, **bilateral hilar adenopathy** is not a typical prominent feature of *Chlamydophila pneumoniae* infection.
Interstitial lung disease classification US Medical PG Question 6: A 40-year-old woman comes to the physician for a 2-month history of chest pain and heartburn after meals. The patient reports that the pain is worse at night and especially when lying down. She has a history of Raynaud's disease treated with nifedipine. There is no family history of serious illness. She emigrated to the US from Nigeria 5 years ago. She does not smoke or drink alcohol. Vital signs are within normal limits. Cardiopulmonary examination shows no abnormalities. Thickening and hardening of the skin is seen on the hands and face. There are several firm, white nodules on the elbows and fingertips. Further evaluation of this patient is most likely to show which of the following findings?
- A. Anti-RNA polymerase III antibodies
- B. Anti-U1 RNP antibodies
- C. Anti-Scl-70 antibodies
- D. Anticentromere antibodies (Correct Answer)
- E. Anti-dsDNA antibodies
Interstitial lung disease classification Explanation: ***Anticentromere antibodies***
- The patient presents with symptoms consistent with **limited cutaneous systemic sclerosis (lcSSc)**, including Raynaud's phenomenon, heartburn, skin thickening confined to the face and hands, and calcinosis (firm, white nodules). **Anticentromere antibodies** are highly specific for lcSSc.
- **Calcinosis**, **Raynaud's phenomenon**, **esophageal dysmotility**, **sclerodactyly**, and **telangiectasias** (CREST syndrome) are hallmarks of lcSSc, and anticentromere antibodies are found in 50-90% of these patients.
*Anti-RNA polymerase III antibodies*
- These antibodies are strongly associated with **diffuse cutaneous systemic sclerosis (dcSSc)**, which typically involves widespread skin thickening on the trunk and proximal extremities.
- They are also linked to a higher risk of **scleroderma renal crisis** and **malignancy**, neither of which are suggested by the patient's current presentation.
*Anti-U1 RNP antibodies*
- These antibodies are characteristic of **mixed connective tissue disease (MCTD)**, an overlap syndrome with features of systemic lupus erythematosus, scleroderma, and polymyositis.
- While MCTD can include Raynaud's and esophageal dysfunction, the prominence of skin thickening and calcinosis more strongly points towards scleroderma.
*Anti-Scl-70 antibodies*
- Also known as **anti-topoisomerase I antibodies**, these are primarily associated with **diffuse cutaneous systemic sclerosis (dcSSc)**.
- Patients with anti-Scl-70 antibodies tend to have more severe internal organ involvement, particularly **interstitial lung disease**, which is not the prominent feature in this case.
*Anti-dsDNA antibodies*
- These antibodies are highly specific for **systemic lupus erythematosus (SLE)** and are often associated with lupus nephritis.
- The patient's symptoms of prominent skin thickening, Raynaud's, and calcinosis are not typical for SLE as the primary diagnosis.
Interstitial lung disease classification US Medical PG Question 7: A 70-year-old man comes to the physician because of intermittent shortness of breath while going up stairs and walking his dog. It began about 1 month ago and seems to be getting worse. He has also developed a dry cough. He has not had any wheezing, fevers, chills, recent weight loss, or shortness of breath at rest. He has a history of Hodgkin lymphoma, for which he was treated with chemotherapy and radiation to the chest 7 years ago. He also has hypertension, for which he takes lisinopril. Ten years ago, he retired from work in the shipbuilding industry. He has smoked half a pack of cigarettes daily since the age of 21. Vital signs are within normal limits. On lung auscultation, there are mild bibasilar crackles. A plain x-ray of the chest shows bilateral ground-glass opacities at the lung bases and bilateral calcified pleural plaques. Which of the following is the greatest risk factor for this patient's current condition?
- A. Family history
- B. Smoking
- C. Radiation therapy
- D. Occupational exposure (Correct Answer)
- E. Advanced age
Interstitial lung disease classification Explanation: ***Occupational exposure***
- The patient's history of working in the **shipbuilding industry** and the presence of **calcified pleural plaques** strongly suggest **asbestosis**, a chronic lung disease caused by inhaling asbestos fibers.
- **Asbestosis** typically presents with **progressive shortness of breath** and a **dry cough**, along with bibasilar crackles and ground-glass opacities, consistent with the patient's symptoms and chest X-ray findings.
*Family history*
- While genetics can play a role in some interstitial lung diseases (e.g., familial pulmonary fibrosis), there is no specific family history mentioned that would strongly link it to the patient's present illness.
- The patient's presentation with **pleural plaques** points away from a primary genetic cause and towards environmental exposure.
*Smoking*
- Smoking is a risk factor for various lung conditions, including **emphysema** and **lung cancer**, and can exacerbate other lung diseases. However, the presence of **pleural plaques** is not caused by smoking.
- While smoking can worsen the prognosis of asbestos-related diseases, it is not the primary cause of the pleural plaques or the most likely underlying condition in this specific clinical picture.
*Radiation therapy*
- **Radiation pneumonitis** and **fibrosis** can occur following chest radiation, and the patient received radiation for Hodgkin lymphoma 7 years ago. However, the **calcified pleural plaques** are highly characteristic of asbestos exposure, not radiation.
- Radiation-induced lung changes are typically more localized to the irradiated field and would not specifically cause pleural plaques.
*Advanced age*
- While the incidence of many chronic diseases increases with age, age itself is not a specific risk factor for the characteristic findings of **calcified pleural plaques** and the described clinical picture.
- The presence of specific radiological findings (pleural plaques) strongly points to an environmental exposure rather than simply advanced age.
Interstitial lung disease classification US Medical PG Question 8: A 49-year-old woman comes to the physician because of a 4-month history of a dry cough and shortness of breath on exertion. She also reports recurrent episodes of pain, stiffness, and swelling in her wrist and her left knee over the past 6 months. She had two miscarriages at age 24 and 28. Physical examination shows pallor, ulcerations on the palate, and annular hyperpigmented plaques on the arms and neck. Fine inspiratory crackles are heard over bilateral lower lung fields on auscultation. Which of the following additional findings is most likely in this patient?
- A. Increased airway resistance
- B. Decreased A-a gradient
- C. Decreased right atrial pressure
- D. Decreased diffusing capacity (Correct Answer)
- E. Increased lung compliance
Interstitial lung disease classification Explanation: ***Decreased diffusing capacity***
- This patient presents with symptoms highly suggestive of **systemic lupus erythematosus (SLE)**, including recurrent miscarriages, joint pain, oral ulcers, skin lesions (annular hyperpigmented plaques), and pulmonary involvement (dry cough, dyspnea, crackles).
- **Interstitial lung disease (ILD)**, a common pulmonary manifestation of SLE, leads to **fibrosis** of the alveolar-capillary membrane, thereby **decreasing the diffusing capacity of the lung for carbon monoxide (DLCO)**.
*Increased airway resistance*
- Increased airway resistance is characteristic of **obstructive lung diseases** like asthma or COPD, which primarily involve narrowing of the airways.
- The patient's presentation with **inspiratory crackles** and symptoms of restrictive disease (shortness of breath on exertion, dry cough) is not consistent with increased airway resistance.
*Decreased A-a gradient*
- A **decreased alveolar-arterial (A-a) gradient** indicates efficient gas exchange and is typically seen in healthy individuals or in conditions causing hypoventilation without intrinsic lung disease.
- In conditions like pulmonary fibrosis or ILD, there is impaired gas exchange leading to an **increased A-a gradient**.
*Decreased right atrial pressure*
- **Decreased right atrial pressure** would typically signify reduced venous return or normal cardiac function.
- Given the patient's respiratory symptoms and potential for pulmonary hypertension secondary to ILD, an **increased right atrial pressure** would be more likely due to increased pulmonary vascular resistance.
*Increased lung compliance*
- **Increased lung compliance** is seen in conditions where the lung tissue becomes more distensible, such as **emphysema**, due to destruction of elastic fibers.
- **Interstitial lung disease** and pulmonary fibrosis, as suggested by the patient's symptoms and signs, lead to **decreased lung compliance** due to stiffening of the lung tissue.
Interstitial lung disease classification US Medical PG Question 9: A 35-year-old female comes to the physician because of a 2-year history of progressive fatigue and joint pain. She has a 1-year history of skin problems and a 4-month history of episodic pallor of her fingers. She reports that the skin of her face, neck, and hands is always dry and itchy; there are also numerous “red spots” on her face. She has become more “clumsy” and often drops objects. She has gastroesophageal reflux disease treated with lansoprazole. She does not smoke. She occasionally drinks a beer or a glass of wine. Her temperature is 36.5°C (97.7°F), blood pressure is 154/98 mm Hg, and pulse is 75/min. Examination shows hardening and thickening of the skin of face, neck, and hands. There are small dilated blood vessels around her mouth and on her oral mucosa. Mouth opening is reduced. Active and passive range of motion of the proximal and distal interphalangeal joints is limited. Cardiopulmonary examination shows no abnormalities. Her creatinine is 1.4 mg/dL. The patient is at increased risk for which of the following complications?
- A. Digital ulcers (Correct Answer)
- B. Scleroderma renal crisis
- C. Pulmonary arterial hypertension
- D. Gastrointestinal dysmotility
- E. Interstitial lung disease
Interstitial lung disease classification Explanation: ***Digital ulcers***
- The patient exhibits several features of **systemic sclerosis (scleroderma)**, including **active Raynaud phenomenon** (**episodic pallor of fingers**), skin thickening, and telangiectasias (**red spots**). **Digital ulcers are the most immediate complication** given the active vascular symptoms.
- Raynaud phenomenon causes repeated ischemia-reperfusion injury to the digits, and **up to 50% of patients with systemic sclerosis and Raynaud develop digital ulcers**, making this the highest near-term risk among the options.
- The patient's **reduced mouth opening** and **limited range of motion in interphalangeal joints** are consistent with skin changes and joint involvement in scleroderma, further supporting the diagnosis and vascular complications.
*Scleroderma renal crisis*
- While **hypertension** is present (154/98 mm Hg) and **creatinine is elevated** (1.4 mg/dL), these findings are relatively mild and do not meet criteria for **scleroderma renal crisis**, which typically presents with **acute malignant hypertension** (>180/100 mmHg), rapidly progressive renal failure, microangiopathic hemolytic anemia, and thrombocytopenia.
- Renal crisis tends to occur earlier in the disease course (within first 4-5 years) and is more common with diffuse cutaneous scleroderma and recent corticosteroid use. This patient's presentation suggests limited cutaneous involvement (face, neck, hands - consistent with CREST/limited variant).
*Pulmonary arterial hypertension*
- **Pulmonary arterial hypertension (PAH)** is a serious late complication of systemic sclerosis, particularly in limited cutaneous disease, but there are **no current signs or symptoms** on cardiopulmonary examination.
- While this remains a long-term risk requiring screening, it is not the most immediate complication. PAH typically develops years after disease onset and would present with dyspnea, fatigue, and signs of right heart dysfunction.
*Gastrointestinal dysmotility*
- The patient **already has** **gastroesophageal reflux disease (GERD)**, which is a manifestation of gastrointestinal dysmotility in systemic sclerosis due to esophageal smooth muscle involvement.
- Since the patient already has this complication (not "at risk for" a future complication), this is not the best answer. Further GI complications could occur, but digital ulcers represent a more immediate risk.
*Interstitial lung disease*
- **Interstitial lung disease (ILD)** is a common and severe complication of systemic sclerosis, particularly in the diffuse cutaneous form, and is a leading cause of mortality.
- However, the patient's **cardiopulmonary examination is noted as normal**, which does not suggest active or clinically apparent ILD at this time. While this remains a long-term risk requiring monitoring (with pulmonary function tests and HRCT), it is not the most immediate complication given the active Raynaud phenomenon.
Interstitial lung disease classification US Medical PG Question 10: A 37-year-old woman comes to the physician because of a 10-month history of excessive daytime sleepiness and fatigue. She says she has difficulty concentrating and has fallen asleep at work on numerous occasions. She also reports having frequent headaches during the day. She has no difficulty falling asleep at night, but wakes up gasping for breath at least once. She has always snored loudly and began using an oral device to decrease her snoring a year ago. She has occasional lower back pain, for which she takes tramadol tablets 1–2 times per week. She also began taking one rabeprazole tablet daily 3 weeks ago. She does not smoke. She is 175 cm (5 ft 7 in) tall and weighs 119 kg (262 lb); BMI is 38.8 kg/m2. Her vital signs are within normal limits. Physical and neurologic examinations show no other abnormalities. Arterial blood gas analysis on room air shows:
pH 7.35
PCO2 51 mm Hg
PO2 64 mm Hg
HCO3- 29 mEq/L
O2 saturation 92%
An x-ray of the chest and ECG show no abnormalities. Which of the following is the most likely cause of this patient's condition?
- A. Chronic inflammatory airflow limitation
- B. Thickening of alveolar membranes
- C. Drug-induced respiratory depression
- D. Diurnal alveolar hypoventilation
- E. Apneic episodes with obstructed upper airways (Correct Answer)
Interstitial lung disease classification Explanation: **Apneic episodes with obstructed upper airways**
- This patient has classic **obstructive sleep apnea (OSA)**, characterized by **loud snoring**, **waking up gasping for breath** (witnessed apneas), and **excessive daytime sleepiness**.
- Her **obesity (BMI 38.8)** is a major risk factor for OSA, as excess soft tissue in the upper airway predisposes to collapse during sleep.
- The ABG shows **compensated respiratory acidosis (pH 7.35, PCO2 51, HCO3- 29)** and **hypoxemia (PO2 64, O2 sat 92%)**, indicating chronic hypoventilation from recurrent apneic episodes.
- OSA is the **underlying cause** of her condition; the oral device she uses is typically employed to treat OSA by repositioning the jaw to maintain airway patency.
- The question asks for the **cause** of her condition, which is the **obstructed upper airways** leading to apneic episodes during sleep.
*Diurnal alveolar hypoventilation*
- While this patient does have daytime (diurnal) hypoventilation as evidenced by the elevated PCO2, this is a **consequence** of severe OSA, not the primary cause.
- This describes **Obesity Hypoventilation Syndrome (OHS)**, which overlaps with OSA but refers specifically to the chronic hypoventilation state.
- The **obstructed airways causing apneic episodes** are the underlying pathophysiology that leads to the chronic hypoventilation.
*Chronic inflammatory airflow limitation*
- This refers to **COPD**, which typically presents with **dyspnea, chronic cough, and wheezing**.
- The patient is a **non-smoker**, has a **normal chest x-ray**, and lacks respiratory symptoms typical of COPD.
- The clinical picture is classic for OSA, not obstructive lung disease.
*Thickening of alveolar membranes*
- This describes **interstitial lung diseases (ILD)**, which present with **progressive dyspnea, restrictive physiology**, and often **interstitial infiltrates on imaging**.
- The patient's **normal chest x-ray** and lack of exertional dyspnea make ILD unlikely.
- Her symptoms are related to sleep-disordered breathing, not parenchymal lung disease.
*Drug-induced respiratory depression*
- **Tramadol** (an opioid) can cause respiratory depression, but she takes it only **1-2 times per week** for back pain.
- The ABG shows **compensated** respiratory acidosis with elevated bicarbonate, indicating a **chronic process** lasting weeks to months, not acute drug effect.
- Her symptoms (snoring, gasping, daytime sleepiness) and obesity clearly point to OSA as the cause.
More Interstitial lung disease classification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.