Idiopathic pulmonary fibrosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Idiopathic pulmonary fibrosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Idiopathic pulmonary fibrosis US Medical PG Question 1: A 57-year-old man comes to the physician because of a 2-month history of worsening shortness of breath with walking. He has not had any cough, fevers, or recent weight loss. He has hypercholesterolemia, for which he takes simvastatin, but otherwise is healthy. For 35 years he has worked for a demolition company. He has smoked 1 pack of cigarettes daily for the past 33 years. Pulmonary examination shows fine bibasilar end-expiratory crackles. An x-ray of the chest shows diffuse bilateral infiltrates predominantly in the lower lobes and bilateral calcified pleural plaques. The patient is most likely to develop which of the following conditions?
- A. Tuberculosis
- B. Thyroid carcinoma
- C. Sarcoidosis
- D. Mesothelioma (Correct Answer)
- E. Bronchogenic carcinoma
Idiopathic pulmonary fibrosis Explanation: ***Mesothelioma***
- The patient has **asbestosis** (interstitial lung disease from asbestos exposure causing bilateral lower lobe infiltrates and bibasilar crackles) due to 35 years working in **demolition** with asbestos exposure.
- **Calcified pleural plaques** are pathognomonic for asbestos exposure and indicate significant cumulative exposure.
- Patients with asbestosis and pleural plaques have markedly increased risk of **malignant mesothelioma**, a highly specific asbestos-related malignancy of the pleura.
- While bronchogenic carcinoma is statistically more common, **mesothelioma is virtually pathognomonic** for asbestos exposure and is the classic malignancy tested in this clinical context.
*Tuberculosis*
- TB typically presents with **cough, fevers, night sweats, and weight loss**, which are absent in this patient.
- Chest x-ray in TB shows **upper lobe cavitations or consolidation**, not bilateral lower lobe interstitial infiltrates with pleural plaques.
- No epidemiologic risk factors for TB are present.
*Thyroid carcinoma*
- Thyroid cancer presents with a **thyroid nodule or mass**, not pulmonary symptoms.
- No association with asbestos exposure or the clinical findings described.
*Sarcoidosis*
- Sarcoidosis typically shows **bilateral hilar lymphadenopathy** and upper/middle lobe involvement on chest x-ray.
- Not associated with asbestos exposure or calcified pleural plaques.
- Occurs more commonly in younger patients (20-40 years old).
*Bronchogenic carcinoma*
- While this patient's **smoking history** increases lung cancer risk, and asbestos exposure synergistically increases this risk further, bronchogenic carcinoma would present with a **focal mass or nodule**, not diffuse bilateral infiltrates.
- The **calcified pleural plaques** and diffuse interstitial pattern point more specifically toward asbestos-related pathology (asbestosis now, mesothelioma risk in future).
- Mesothelioma is more specific to asbestos exposure in this clinical scenario.
Idiopathic pulmonary fibrosis US Medical PG Question 2: A 70-year-old man presents to a physician with a cough and difficulty breathing during the last 7 years. He has smoked since his teenage years and regularly inhales tiotropium, formoterol, and budesonide and takes oral theophylline. The number of exacerbations has been increasing over the last 6 months. His temperature is 37.2°C (99°F), the heart rate is 92/min, the blood pressure is 134/88 mm Hg and the respiratory rate is 26/min. On chest auscultation breath sounds are diffusely decreased and bilateral rhonchi are present. Pulse oximetry shows his resting oxygen saturation to be 88%. Chest radiogram shows a flattened diaphragm, hyperlucency of the lungs, and a long, narrow heart shadow. The physician explains this condition to the patient and emphasizes the importance of smoking cessation. In addition to this, which of the following is most likely to reduce the risk of mortality from the condition?
- A. Roflumilast
- B. Low-dose oral prednisone
- C. Pulmonary rehabilitation
- D. Supplemental oxygen (Correct Answer)
- E. Prophylactic azithromycin
Idiopathic pulmonary fibrosis Explanation: ***Supplemental oxygen***
- The patient's **resting oxygen saturation of 88%** indicates significant hypoxemia, which, if chronic, places a high burden on the cardiovascular system and is a strong predictor of premature mortality in **COPD**.
- **Long-term oxygen therapy (LTOT)** for at least 15 hours a day has been shown to improve survival in patients with severe chronic hypoxemia due to COPD.
*Roflumilast*
- **Roflumilast** is a phosphodiesterase-4 inhibitor that reduces inflammation and is used to decrease exacerbations in severe COPD associated with chronic bronchitis and a history of frequent exacerbations.
- While it can improve lung function and reduce exacerbations, it has not been shown to reduce mortality directly.
*Low-dose oral prednisone*
- **Oral corticosteroids** are primarily used for acute exacerbations of COPD, not for long-term maintenance due to significant systemic side effects like osteoporosis, muscle weakness, and increased infection risk.
- While they can temporarily reduce inflammation, chronic low-dose use is not recommended for mortality benefit and may cause harm in the long run.
*Pulmonary rehabilitation*
- **Pulmonary rehabilitation** is a comprehensive program that improves exercise tolerance, dyspnea, and quality of life in patients with COPD.
- It does not directly reduce mortality but significantly improves functional status and potentially reduces hospitalizations.
*Prophylactic azithromycin*
- **Prophylactic azithromycin** can reduce the frequency of exacerbations in select patients with severe COPD, likely due to its anti-inflammatory and immunomodulatory properties, as well as its bactericidal effect.
- Similar to roflumilast, it reduces exacerbations but has not been shown to reduce mortality directly in COPD patients.
Idiopathic pulmonary fibrosis US Medical PG Question 3: A 62-year-old man with a 5-year history of chronic obstructive pulmonary disease comes to the physician for a follow-up examination. He has had episodic palpitations over the past week. His only medication is a tiotropium-formoterol inhaler. His pulse is 140/min and irregular, respirations are 17/min, and blood pressure is 116/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 95%. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. Serum concentrations of electrolytes, thyroid-stimulating hormone, and cardiac troponins are within the reference range. An electrocardiogram is shown. Which of the following is the most appropriate next step in management?
- A. Procainamide therapy
- B. Radiofrequency ablation
- C. Synchronized cardioversion
- D. Propranolol therapy
- E. Verapamil therapy (Correct Answer)
Idiopathic pulmonary fibrosis Explanation: ***Verapamil therapy***
- The ECG shows **multifocal atrial tachycardia (MAT)**, characterized by at least three different P-wave morphologies, irregular PP/PR/RR intervals, and an atrial rate >100/min. Given the patient's COPD and stable hemodynamics, **verapamil** (a non-dihydropyridine calcium channel blocker) is the preferred treatment to control the ventricular rate.
- Verapamil is effective in slowing AV nodal conduction and can help re-establish a regular rhythm in patients with MAT, especially those with underlying pulmonary disease where beta-blockers may be relatively contraindicated.
*Procainamide therapy*
- **Procainamide**, a Class Ia antiarrhythmic, is typically used for ventricular arrhythmias or re-entrant supraventricular tachycardias, not usually as first-line for MAT.
- It carries risks of proarrhythmia and hypotension, which are less desirable in a patient with stable MAT.
*Radiofrequency ablation*
- **Radiofrequency ablation** is a definitive treatment for refractory arrhythmias but is generally reserved for patients whose MAT is symptomatic and resistant to pharmacological therapy.
- It is an invasive procedure and not the initial management choice for a stable patient with MAT.
*Synchronized cardioversion*
- **Synchronized cardioversion** is indicated for unstable tachyarrhythmias causing hemodynamic compromise (e.g., hypotension, altered mental status, acute heart failure, ischemic chest pain).
- This patient is hemodynamically stable (BP 116/70, clear lungs, normal oxygen saturation), so cardioversion is not immediately necessary.
*Propranolol therapy*
- **Propranolol**, a non-selective beta-blocker, could be effective for rate control in MAT. However, in a patient with **COPD**, non-selective beta-blockers can worsen bronchoconstriction and are generally avoided.
- While cardioselective beta-blockers (e.g., metoprolol) might be considered, **calcium channel blockers** like verapamil are often preferred in MAT with concurrent pulmonary disease due to less risk of bronchospasm.
Idiopathic pulmonary fibrosis US Medical PG Question 4: A 61-year-old man comes to the physician because of a 9-month history of progressive shortness of breath on exertion. Pulmonary examinations shows fine bibasilar end-inspiratory crackles. There is digital clubbing. Pulmonary functions tests show an FEV1:FVC ratio of 97% and a total lung capacity of 70%. An x-ray of the chest shows small bilateral reticular opacities, predominantly in the lower lobes. A photomicrograph of a specimen obtained on lung biopsy is shown. The patient most likely works in which of the following fields?
- A. Coal mining
- B. Cattle farming
- C. Shipbuilding (Correct Answer)
- D. Sandblasting
- E. Aerospace manufacturing
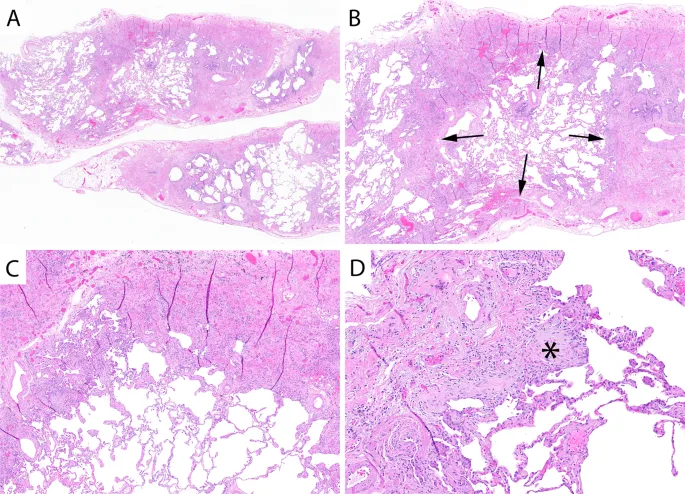
Idiopathic pulmonary fibrosis Explanation: ***Shipbuilding***
- The patient's presentation with progressive shortness of breath, **bibasilar end-inspiratory crackles**, **digital clubbing**, and **restrictive lung disease** (normal FEV1:FVC, reduced TLC) along with **bilateral reticular opacities** on X-ray, points towards **pulmonary fibrosis**.
- **Shipbuilding** is a common occupation associated with **asbestos exposure**, which is a well-known cause of **pulmonary fibrosis** (asbestosis). The photomicrograph would likely show **asbestos bodies** or **fibrotic changes**.
*Coal mining*
- **Coal workers' pneumoconiosis** typically presents with diffuse small nodular opacities on chest X-ray and can also cause restrictive lung disease.
- However, digital clubbing is less common in uncomplicated coal workers' pneumoconiosis, and the primary pathological finding would be **macules and nodules** rather than diffuse fibrosis with asbestos bodies.
*Cattle farming*
- **Hypersensitivity pneumonitis** (farmer's lung) due to exposure to organic dusts from hay or mold is associated with cattle farming.
- While it can cause restrictive lung disease and crackles, it often presents with acute or subacute episodes, and chronic forms might show **centrilobular nodules** or ground-glass opacities, not typically the diffuse lower lobe reticular pattern seen with asbestosis.
*Sandblasting*
- **Silicosis** is associated with sandblasting, causing **nodular opacities** predominantly in the upper lobes, and can lead to progressive massive fibrosis.
- While it causes restrictive lung disease, the radiographic pattern and typical distribution (upper lobe predominance) differ from the presented case.
*Aerospace manufacturing*
- This field can involve exposure to various substances, including **beryllium**, leading to **berylliosis**.
- Berylliosis can cause granulomatous lung disease, with findings such as hilar lymphadenopathy and nodular infiltrates, which do not align with the described lower lobe reticular opacities and digital clubbing, which are hallmarks of asbestos exposure.
Idiopathic pulmonary fibrosis US Medical PG Question 5: A 52-year-old man comes to the physician because of a 6-month history of shortness of breath and nonproductive cough. He has smoked 1 pack of cigarettes daily for 15 years. Cardiopulmonary examination shows fine inspiratory crackles bilaterally. There is clubbing present in the fingers bilaterally. Pulmonary function tests (PFTs) show an FVC of 78% of expected and an FEV1/FVC ratio of 92%. A CT scan of the chest is shown. Which of the following is the most likely underlying diagnosis?
- A. Bronchopulmonary aspergillosis
- B. Pulmonary fibrosis (Correct Answer)
- C. Chronic obstructive pulmonary disease
- D. Chronic bronchiectasis
- E. Pulmonary tuberculosis
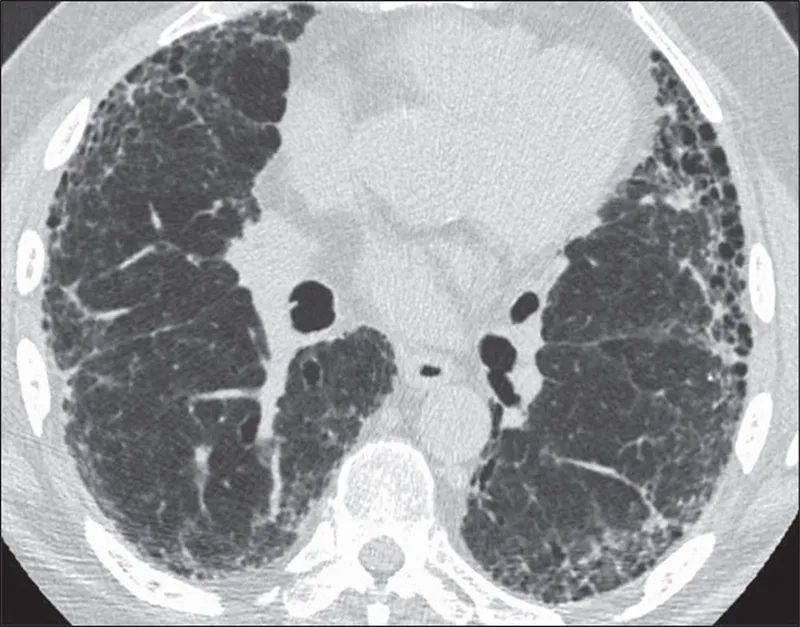
Idiopathic pulmonary fibrosis Explanation: ***Pulmonary fibrosis***
- The CT scan shows a pattern of **reticular opacities** and **honeycombing**, classic features of **pulmonary fibrosis**.
- Clinical presentation with **progressive dyspnea**, nonproductive cough, **fine inspiratory crackles**, and **clubbing** are highly suggestive of interstitial lung disease, with PFTs showing a **restrictive pattern** (reduced FVC, preserved FEV1/FVC ratio).
*Bronchopulmonary aspergillosis*
- This condition is typically characterized by **recurrent fleeting infiltrates**, **bronchiectasis**, and **eosinophilia** in asthmatic patients, which are not described.
- The CT findings would usually show **bronchial wall thickening** and **mucus plugging**, rather than widespread fibrosis and honeycombing.
*Chronic obstructive pulmonary disease*
- COPD typically presents with an **obstructive pattern** on PFTs (reduced FEV1/FVC ratio), which is not seen here.
- While smoking is a risk factor, the chest CT findings of extensive **honeycombing** and **fibrosis** are not characteristic of emphysema or chronic bronchitis.
*Chronic bronchiectasis*
- Bronchiectasis is characterized by **permanent dilatation of the bronchi**, often leading to chronic cough with copious sputum production and recurrent infections.
- While the CT scan may show some dilated airways, the predominant pattern of **honeycombing** and **reticular opacities** is more indicative of fibrosis, and the clinical picture does not emphasize chronic productive cough or infections.
*Pulmonary tuberculosis*
- Pulmonary tuberculosis presents with various patterns on CT, often including **cavitary lesions**, **nodules**, or **fibrocalcific changes**, typically in the upper lobes.
- The diffuse interstitial changes and **honeycombing** seen on this CT are not typical for tuberculosis, and symptoms like fever, night sweats, or weight loss are not mentioned.
Idiopathic pulmonary fibrosis US Medical PG Question 6: A 33-year-old African-American female presents to her physician with complaints of a persistent, dry cough. She states that the cough has gone on for some time now. Three weeks ago, during her last general checkup, she was started on lisinopril and metformin for concerns regarding an elevated blood pressure and fasting blood glucose. Past medical history is notable for eczema, asthma, and seasonal allergies. At this visit the patient has other non-specific complaints such as fatigue and joint pain as well as a burning sensation in her sternum when she eats large meals. Her physical exam is only notable for painful bumps on her lower extremities (figure A) which the patient attributes to "bumping her shins," during exercise, and an obese habitus. Which of the following is most likely true for this patient's chief concern?
- A. Omeprazole is an appropriate next step in management
- B. Loratadine would best treat her chief complaint
- C. Serum levels of bradykinin will be elevated
- D. Non-caseating granulomas are found on biopsy of mediastinal lymph nodes (Correct Answer)
- E. Beta agonists would relieve this patient's symptoms
Idiopathic pulmonary fibrosis Explanation: ***Non-caseating granulomas are found on biopsy of mediastinal lymph nodes***
- The patient's symptoms (persistent dry cough, fatigue, joint pain, painful shin bumps consistent with **erythema nodosum**) in an **African-American female** are highly suggestive of **sarcoidosis**.
- **Sarcoidosis** is characterized by the presence of **non-caseating granulomas** in affected organs, commonly the lungs and mediastinal lymph nodes.
*Omeprazole is an appropriate next step in management*
- While the patient has a "burning sensation in her sternum when she eats large meals," suggesting **gastroesophageal reflux disease (GERD)**, this is not her chief complaint.
- Treating GERD with **omeprazole** would address the burning sensation but not the persistent dry cough or other systemic symptoms.
*Loratadine would best treat her chief complaint*
- **Loratadine** is an antihistamine used to treat allergic reactions, including symptoms of seasonal allergies and eczema.
- Although the patient has a history of allergies and asthma, a persistent dry cough with systemic symptoms and erythema nodosum points away from an **allergic cough** as the primary cause.
*Serum levels of bradykinin will be elevated*
- High serum levels of **bradykinin** can cause an ACE inhibitor-induced dry cough, which should be considered given her recent initiation of **lisinopril**.
- However, the presence of **erythema nodosum**, joint pain, and fatigue, combined with a persistent dry cough, makes **sarcoidosis** a more comprehensive diagnosis that explains all her symptoms beyond just the cough.
*Beta agonists would relieve this patient's symptoms*
- **Beta-agonists** are bronchodilators used to relieve bronchospasm in conditions like asthma.
- While the patient has a history of asthma, her cough is described as persistent and dry, and combined with other systemic symptoms, it is less likely to be solely an asthma exacerbation treatable with **beta-agonists**.
Idiopathic pulmonary fibrosis US Medical PG Question 7: A 65-year-old male engineer presents to the office with shortness of breath on exertion and a dry cough that he has had for about a year. He is a heavy smoker with a 25-pack-years history. His vitals include: heart rate 95/min, respiratory rate 26/min, and blood pressure 110/75 mm Hg. On examination, he presents with nail clubbing and bilateral and persistent crackling rales. The chest radiograph shows basal reticulonodular symmetric images, with decreased lung fields. The pulmonary function tests show the following: diffusing capacity of the lungs for carbon monoxide (DLCO) is 43% and reference SaO2 is 94% and 72%, at rest and with exercise, respectively. What is the most likely diagnosis?
- A. Chronic hypersensitivity pneumonitis
- B. Pulmonary Langerhans cell histiocytosis
- C. Pleuropulmonary fibroelastosis
- D. Asbestosis
- E. Idiopathic pulmonary fibrosis (Correct Answer)
Idiopathic pulmonary fibrosis Explanation: ***Idiopathic pulmonary fibrosis***
- This patient's presentation with **progressive dyspnea**, **dry cough**, **clubbing**, and **basal crackles (rales)**, combined with restrictive lung physiology (low **DLCO**) and **basal reticulonodular infiltrates** on CXR, is highly characteristic of **idiopathic pulmonary fibrosis**. The marked **desaturation with exercise** further supports this diagnosis.
- While smoking is a risk factor, the pattern of lung disease is consistent with IPF, a chronic, progressive, fibrosing interstitial pneumonia of unknown cause.
*Chronic hypersensitivity pneumonitis*
- This condition is caused by **chronic exposure to inhaled antigens** and typically presents with symptoms that link back to the exposure, potentially resolving with avoidance.
- While it can cause interstitial lung disease, the absence of an identifiable antigen exposure and the typical fibrotic pattern with subpleural honeycombing would make IPF more likely.
*Pulmonary Langerhans cells histiocytosis*
- This disease is strongly associated with **smoking** but typically presents with **cysts and nodules** predominantly in the **upper and middle lung fields** on imaging.
- The patient's **basal reticulonodular pattern** with decreased lung fields on CXR, rather than cysts, makes this diagnosis less likely.
*Pleuropulmonary fibroelastosis*
- This is a rare interstitial lung disease characterized by **fibrosis predominantly affecting the upper lobes** and pleura.
- The patient's **basal predominant findings** on chest radiograph and crackles make this diagnosis less consistent.
*Asbestosis*
- Although the patient's occupation as an engineer could suggest **asbestos exposure**, the description lacks specific features like **pleural plaques** or calcifications.
- While asbestosis can cause diffuse interstitial fibrosis and similar symptoms, the clinical and radiological picture, especially the extent of **DLCO reduction** for the given findings, more strongly points to IPF.
Idiopathic pulmonary fibrosis US Medical PG Question 8: A 61-year-old male presents to your office with fever and dyspnea on exertion. He has been suffering from chronic, non-productive cough for 1 year. You note late inspiratory crackles on auscultation. Pulmonary function tests reveal an FEV1/FVC ratio of 90% and an FVC that is 50% of the predicted value. Which of the following would you most likely see on a biopsy of this patient's lung?
- A. Arteriovenous malformations
- B. Hyaline membranes
- C. Charcot-Leyden crystals
- D. Subpleural cystic enlargement (Correct Answer)
- E. Linear immunofluorescence along alveolar basement membranes
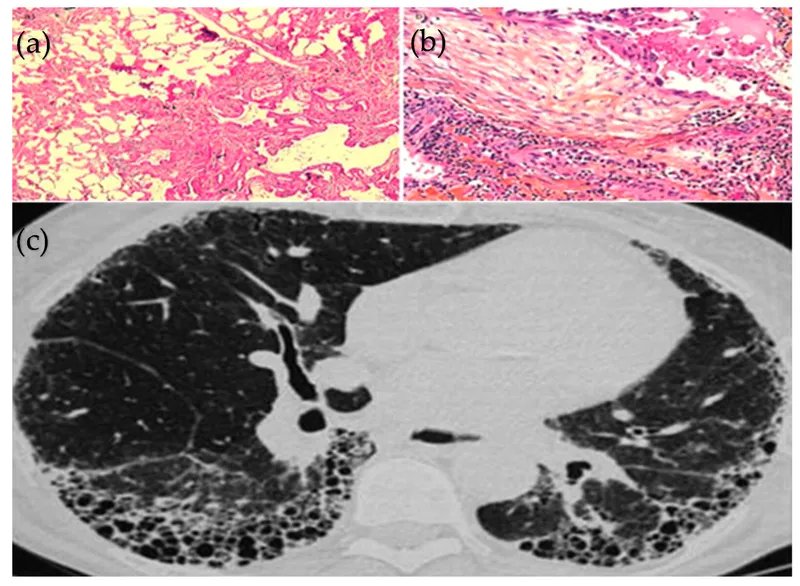
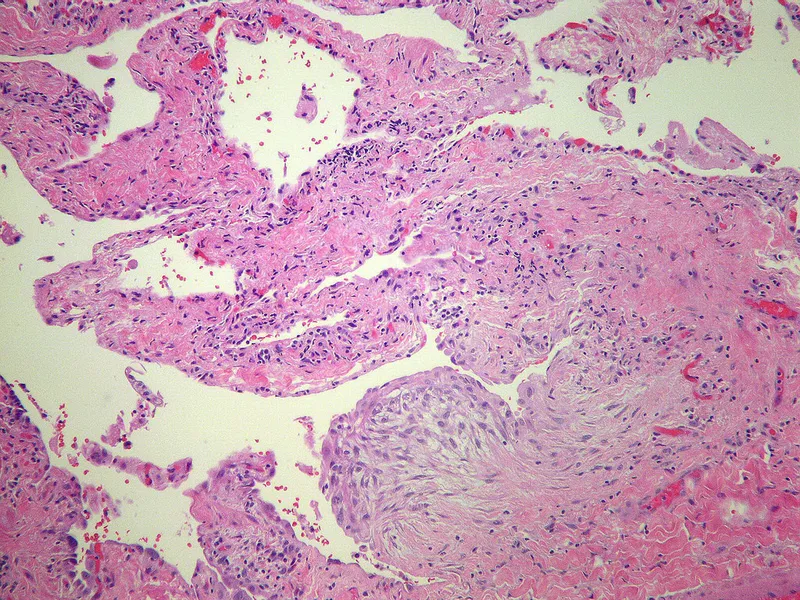
Idiopathic pulmonary fibrosis Explanation: ***Subpleural cystic enlargement***
- The patient's presentation with **dyspnea, non-productive cough, late inspiratory crackles**, and **restrictive lung disease** (normal FEV1/FVC ratio of 90% with reduced FVC of 50%) is highly suggestive of **pulmonary fibrosis**.
- **Subpleural cystic enlargement** (honeycombing) is the characteristic histological finding in advanced pulmonary fibrosis, particularly in the **usual interstitial pneumonia (UIP)** pattern seen in **idiopathic pulmonary fibrosis (IPF)**.
- The chronic, progressive nature (1-year history) and the restrictive PFT pattern make this the most likely biopsy finding.
*Arteriovenous malformations*
- These are abnormal vascular connections between arteries and veins that can cause **hypoxemia** and are typically associated with **hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease)**.
- They do not explain the restrictive PFT pattern or the typical presentation of chronic progressive fibrosis with late inspiratory crackles.
*Linear immunofluorescence along alveolar basement membranes*
- This finding on **direct immunofluorescence** with **IgG deposition** is characteristic of **Goodpasture syndrome** (anti-GBM disease), which causes pulmonary hemorrhage and rapidly progressive glomerulonephritis.
- This condition presents with **hemoptysis** and **acute renal failure**, not chronic non-productive cough, and would show an obstructive or mixed pattern if hemorrhage were present.
*Hyaline membranes*
- **Hyaline membranes** are proteinaceous material lining alveoli seen in **acute respiratory distress syndrome (ARDS)** or **diffuse alveolar damage (DAD)**.
- The patient's **chronic 1-year symptoms** and restrictive PFTs indicate chronic interstitial lung disease, not acute lung injury.
*Charcot-Leyden crystals*
- **Charcot-Leyden crystals** are formed from breakdown of **eosinophils** and are found in conditions with eosinophilic inflammation, such as **asthma** or **eosinophilic pneumonia**.
- While these conditions can cause cough and dyspnea, they would typically show an **obstructive pattern** (reduced FEV1/FVC) in asthma, not the restrictive pattern seen here.
Idiopathic pulmonary fibrosis US Medical PG Question 9: A 52-year-old man is brought to the emergency department by a friend because of a 5-day history of fever and cough productive of purulent sputum. One week ago, he was woken up by an episode of heavy coughing while lying on his back. He drinks large amounts of alcohol daily and has spent most of his time in bed since his wife passed away 2 months ago. His temperature is 38°C (100.4°F), pulse is 96/min, respirations are 24/min, and blood pressure is 110/84 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 87%. Physical examination shows poor dentition and swollen gums. A CT scan of the chest is most likely to show a pulmonary infiltrate in which of the following locations?
- A. Posterior basal segment of the right lower lobe
- B. Posterior basal segment of the left lower lobe
- C. Posterior segment of the right upper lobe
- D. Apicoposterior segment of the left upper lobe
- E. Superior segment of the right lower lobe (Correct Answer)
Idiopathic pulmonary fibrosis Explanation: ***Superior segment of the right lower lobe***
- This patient presents with symptoms and risk factors (alcoholism, poor dentition, recent prolonged bed rest, coughing while lying down) consistent with **aspiration pneumonia**
- Aspiration pneumonia typically affects the superior segment of the lower lobes (especially the right) or the posterior segments of the upper lobes due to **gravitational flow of aspirated material when lying supine**
- The superior segment is the most posterior and dependent portion of the lower lobe in the supine position
*Posterior basal segment of the right lower lobe*
- While the right lower lobe is a common site for aspiration, the posterior basal segment is less common in a supine position where the superior segment is more dependent
- Aspiration into the basal segments (anterior, lateral, posterior) is more typical when a person is upright or in a semi-recumbent position
*Posterior basal segment of the left lower lobe*
- The right lung is generally more susceptible to aspiration than the left due to the **more vertical orientation of the right main bronchus**
- Similar to the right side, the posterior basal segment of the left lower lobe would be less commonly affected in a supine aspirator compared to the superior segment
*Posterior segment of the right upper lobe*
- The posterior segment of the right upper lobe is also a common site for aspiration when lying in a supine position
- However, the superior segment of the right lower lobe is the most frequently cited classic location for aspiration in the supine position
*Apicoposterior segment of the left upper lobe*
- Aspiration into the left upper lobe is less common than into the right lung due to the anatomy of the main bronchi
- The apicoposterior segment could be involved in aspiration, but the right lung and particularly the superior segment of the right lower lobe are statistically more probable
Idiopathic pulmonary fibrosis US Medical PG Question 10: A 27-year-old woman with a history of a "heart murmur since childhood" presents following a series of syncopal episodes over the past several months. She also complains of worsening fatigue over this time period, and notes that her lips have begun to take on a bluish tinge, for which she has been using a brighter shade of lipstick. You do a careful examination, and detect a right ventricular heave, clubbing of the fingers, and 2+ pitting edema bilaterally to the shins. Despite your patient insisting that every doctor she has ever seen has commented on her murmur, you do not hear one. Transthoracic echocardiography would most likely detect which of the following?
- A. Mitral insufficiency
- B. Aortic stenosis
- C. Dynamic left ventricular outflow tract obstruction
- D. Positive bubble study (Correct Answer)
- E. Ventricular aneurysm
Idiopathic pulmonary fibrosis Explanation: ***Positive bubble study***
- The patient's symptoms, including **cyanosis** (**bluish tinge to the lips**), **clubbing**, and **right ventricular heave**, suggest **Eisenmenger syndrome**, a late complication of a **left-to-right shunt** that has reversed due to pulmonary hypertension.
- A positive bubble study on echocardiography would confirm the presence of a **right-to-left shunt**, characteristic of Eisenmenger syndrome, by showing microbubbles crossing from the right to the left side of the heart.
*Mitral insufficiency*
- While mitral insufficiency can cause a murmur and heart failure symptoms, it does not typically lead to the **cyanosis** and **clubbing** described.
- The absence of a murmur, despite a history of one, points away from a significant current insufficiency.
*Aortic stenosis*
- Aortic stenosis is characterized by an **ejection systolic murmur** that would likely be heard on examination, contradicting the scenario where no murmur is audible.
- It usually presents with a different constellation of symptoms, such as angina, syncope, and heart failure, without the prominent cyanosis or clubbing seen here.
*Dynamic left ventricular outflow tract obstruction*
- This is characteristic of **hypertrophic obstructive cardiomyopathy (HOCM)**, which can cause exertional syncope.
- However, HOCM does not typically lead to **cyanosis**, a **right ventricular heave**, or **clubbing**, which are strong indicators of a right-to-left shunt.
*Ventricular aneurysm*
- A ventricular aneurysm is a bulging of the ventricular wall, often a complication of a **myocardial infarction**, which is unlikely in a 27-year-old with a history of a "heart murmur since childhood."
- It typically presents with symptoms related to heart failure, arrhythmias, or embolism, and would not explain the prominent **cyanosis** and **clubbing**.
More Idiopathic pulmonary fibrosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.