Cystic fibrosis in adults US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cystic fibrosis in adults. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cystic fibrosis in adults US Medical PG Question 1: A 4-year-old boy is brought by his parents to his pediatrician’s office. His mother mentions that the child has been producing an increased number of foul stools recently. His mother says that over the past year, he has had 1 or 2 foul-smelling stools per month. Lately, however, the stools are looser, more frequent, and have a distinct odor. Over the past several years, he has been admitted 4 times with episodes of pneumonia. Genetic studies reveal a mutation on a specific chromosome that has led to a 3 base-pair deletion for the amino acid phenylalanine. Which of the following chromosomes is the defective gene responsible for this boy’s clinical condition?
- A. Chromosome 4
- B. Chromosome 7 (Correct Answer)
- C. Chromosome 22
- D. Chromosome 17
- E. Chromosome 15
Cystic fibrosis in adults Explanation: ***Chromosome 7***
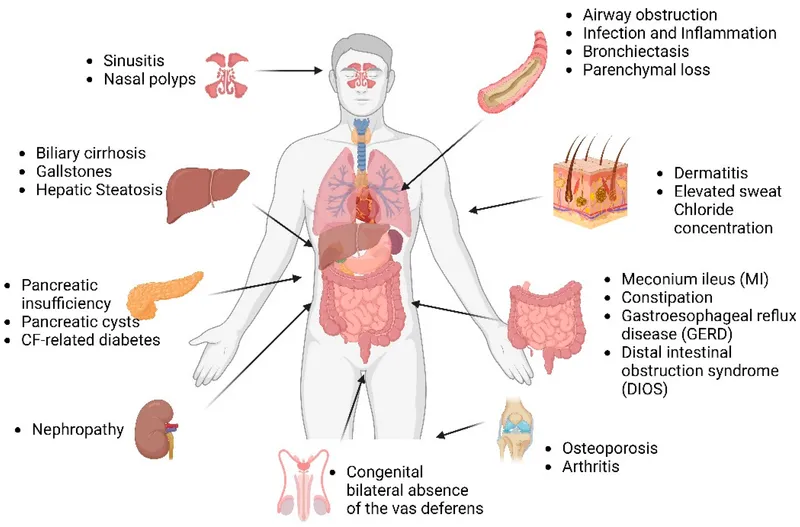
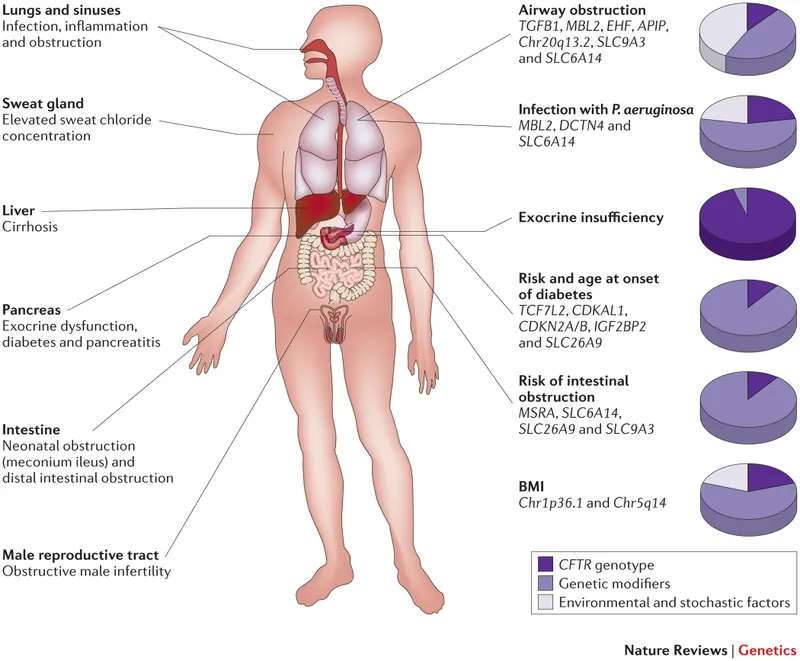
- This patient's symptoms (recurrent pneumonia, foul-smelling stools/steatorrhea) are classic for **cystic fibrosis (CF)**. The most common mutation in CF is a **3-base pair deletion for phenylalanine** (ΔF508), located on the **CFTR gene** on **chromosome 7**.
- The cystic fibrosis transmembrane conductance regulator (CFTR) gene, which is defective in CF, is found on **the long arm (q) of chromosome 7** at position 31.2.
*Chromosome 4*
- **Chromosome 4** is associated with genetic disorders such as **Huntington's disease** and **Wolf-Hirschhorn syndrome**, which do not match the clinical presentation of recurrent pneumonia and steatorrhea.
- Huntington's disease involves trinucleotide repeats and primarily affects neurological function later in life.
*Chromosome 22*
- **Chromosome 22** is implicated in conditions like **DiGeorge syndrome** (22q11.2 deletion syndrome) and certain leukemias, none of which present with the described gastrointestinal and pulmonary symptoms.
- DiGeorge syndrome is characterized by cardiac defects, abnormal facies, thymic hypoplasia, cleft palate, and hypocalcemia.
*Chromosome 17*
- **Chromosome 17** is associated with diseases such as **Neurofibromatosis type 1** and **hereditary breast and ovarian cancer** (BRCA1 gene), which are inconsistent with the patient's symptoms.
- Neurofibromatosis type 1 primarily involves the skin, nervous system, and bones, with manifestations like café-au-lait spots and neurofibromas.
*Chromosome 15*
- **Chromosome 15** is linked to disorders like **Prader-Willi syndrome** and **Angelman syndrome**, which are distinct neurodevelopmental disorders not characterized by recurrent respiratory infections and malabsorption.
- These syndromes result from genomic imprinting defects and present with intellectual disability, developmental delay, and specific physical features.
Cystic fibrosis in adults US Medical PG Question 2: A 29-year-old man presents for the evaluation of infertility. He has a history of recurrent lower respiratory tract infections, productive cough, abdominal pain, and diarrhea. Physical examination reveals clubbing and bilateral crackles on chest auscultation. Chest X-ray reveals increased pulmonary markings and peripheral bronchi with a ‘tram track’ appearance. Which of the following pathophysiologies is responsible for the patient’s condition?
- A. Fibrosis of the lung parenchyma
- B. Bronchial hypersensitivity
- C. Abnormal ciliary motion
- D. Gluten hypersensitivity
- E. Defective chloride transport (Correct Answer)
Cystic fibrosis in adults Explanation: ***Defective chloride transport***
- The patient's presentation with **recurrent respiratory infections**, **bronchiectasis** (tram track appearance on CXR), **clubbing**, and **infertility** is highly suggestive of **cystic fibrosis**.
- **Cystic fibrosis** is caused by mutations in the **CFTR gene**, leading to **defective chloride transport** across epithelial cells, resulting in thick, viscous secretions.
*Fibrosis of the lung parenchyma*
- While chronic lung disease can lead to some **pulmonary fibrosis**, it is not the primary underlying pathophysiology described here.
- Pulmonary fibrosis typically presents with **restrictive lung disease** and interstitial patterns on imaging, rather than the prominent **bronchiectasis** seen in this patient.
*Bronchial hypersensitivity*
- This is characteristic of **asthma**, which involves airway inflammation and bronchoconstriction, but typically does not cause the extensive **recurrent infections**, **bronchiectasis**, or **infertility** seen in this case.
- Asthma is less likely to result in **clubbing** or the progressive lung damage implied by a "tram track" appearance.
*Abnormal ciliary motion*
- This describes **primary ciliary dyskinesia (PCD)**, which can also cause recurrent respiratory infections and male infertility due to **immotile sperm**.
- However, PCD typically presents with **situs inversus** in a significant proportion of cases and does not involve the characteristic **exocrine gland dysfunction** (e.g., severe abdominal symptoms, pancreatic insufficiency leading to diarrhea) often seen in cystic fibrosis implied by the broad clinical picture.
*Gluten hypersensitivity*
- Also known as **celiac disease**, this is primarily a **gastrointestinal condition** characterized by malabsorption due to immune reactions to gluten.
- While celiac disease can cause **abdominal pain** and **diarrhea**, it does not explain the **recurrent respiratory infections**, **bronchiectasis**, **clubbing**, or **male infertility**.
Cystic fibrosis in adults US Medical PG Question 3: A 23-year-old woman is brought to the emergency department 8 hours after the sudden onset of shortness of breath and pleuritic chest pain. She has cystic fibrosis and, during the past year, has had 4 respiratory exacerbations that have required hospitalization. Current medications include an inhaled bronchodilator, an inhaled corticosteroid, inhaled N-acetylcysteine, and azithromycin. The patient appears chronically ill. Her temperature is 37.9°C (100.2°F), pulse is 96/min, respirations are 22/min and labored, and blood pressure is 106/64 mm Hg. Pulse oximetry on 2 L/min of oxygen via nasal cannula shows an oxygen saturation of 96%. Examination shows an increased anteroposterior chest diameter. There is digital clubbing. Chest excursions and tactile fremitus are decreased on the right side. On auscultation of the chest, breath sounds are significantly diminished over the right lung field and diffuse wheezing is heard over the left lung field. Which of the following is the most likely underlying cause of this patient's current symptoms?
- A. Infection with gram-negative coccobacilli
- B. Inflammation of costal cartilage
- C. Bronchial hyperresponsiveness
- D. Increased pulmonary capillary permeability
- E. Apical subpleural cyst (Correct Answer)
Cystic fibrosis in adults Explanation: ***Apical subpleural cyst***
- The sudden onset of **shortness of breath** and **pleuritic chest pain** in a patient with advanced **cystic fibrosis (CF)** and previous frequent pulmonary exacerbations strongly suggests **spontaneous pneumothorax**.
- In CF, chronic inflammation and recurrent infections can lead to the formation of **apical subpleural blebs or cysts**, which can rupture, causing air to leak into the pleural space. This is supported by decreased breath sounds and tactile fremitus on one side, indicating a pneumothorax.
*Infection with gram-negative coccobacilli*
- While **gram-negative bacteria** like *Pseudomonas aeruginosa* are common in CF and can cause respiratory exacerbations, an infection would typically present with increasing productive cough, fever, and leukocytosis, not sudden pleuritic chest pain and diminished breath sounds indicative of pneumothorax.
- The patient's current presentation is more acute and localized to a mechanical issue in the chest rather than a widespread infectious process, especially with normal temperature and relatively stable vitals for an infection.
*Inflammation of costal cartilage*
- **Costochondritis** causes localized chest wall pain that is typically reproducible with palpation and does not cause **shortness of breath** or changes in breath sounds and tactile fremitus like a pneumothorax.
- It is a musculoskeletal issue, not a pulmonary emergency that would explain the acute respiratory distress and physical exam findings.
*Bronchial hyperresponsiveness*
- **Bronchial hyperresponsiveness** is underlying asthma or reactive airway disease, characterized by widespread bronchoconstriction and wheezing. While **wheezing** is present, the unilateral diminished breath sounds and tactile fremitus, coupled with pleuritic chest pain, point away from a primary exacerbation of hyperresponsive airways alone.
- An asthma exacerbation typically presents with more diffuse wheezing and air trapping, rather than a unilateral absence of breath sounds caused by air in the pleural space.
*Increased pulmonary capillary permeability*
- **Increased pulmonary capillary permeability** leads to **pulmonary edema**, which would manifest as diffuse crackles, hypoxemia, and possibly pink frothy sputum, not localized diminished breath sounds and tactile fremitus.
- This condition is more commonly seen in conditions like **ARDS** or **heart failure**, not typically as an acute complication of CF in this manner.
Cystic fibrosis in adults US Medical PG Question 4: A 7-year-old girl is brought by her parents to her pediatrician's office for a persistent cough observed over the past month. She was diagnosed with cystic fibrosis 2 years ago and has been receiving chest physiotherapy regularly and the flu vaccine yearly. Her parents tell the pediatrician that their daughter has been coughing day and night for the past month, and produces thick, purulent, foul-smelling sputum. They are concerned because this is the first time such an episode has occurred. She has not had a fever, chills or any other flu-like symptoms. On examination, her blood pressure is 100/60 mm Hg, the pulse is 82/min, and the respiratory rate is 16/min. Breath sounds are reduced over the lower lung fields along with a presence of expiratory wheezing. Her sputum culture comes back positive for an aerobic, non-lactose fermenting, oxidase-positive, gram-negative bacillus. Which of the following prophylactic regimes should be considered after treating this patient for her current symptoms?
- A. Oral trimethoprim-sulfamethoxazole
- B. Oral amoxicillin/clavulanic acid
- C. Oral ciprofloxacin
- D. Inhaled levofloxacin
- E. Inhaled tobramycin (Correct Answer)
Cystic fibrosis in adults Explanation: ***Inhaled tobramycin***
- The patient's symptoms (persistent cough, purulent sputum, reduced breath sounds, expiratory wheezing) coupled with a positive culture for an **aerobic, non-lactose fermenting, oxidase-positive, gram-negative bacillus** in a patient with cystic fibrosis (CF) strongly suggest a *Pseudomonas aeruginosa* infection.
- **Inhaled tobramycin** is a recommended prophylactic regimen for CF patients with chronic *Pseudomonas aeruginosa* colonization to reduce exacerbations and preserve lung function after initial eradication therapy.
*Oral trimethoprim-sulfamethoxazole*
- This antibiotic is primarily used for infections caused by *Staphylococcus aureus*, *Haemophilus influenzae*, and *Pneumocystis jirovecii*, but not typically for *Pseudomonas aeruginosa* in CF.
- While it has some activity against certain gram-negative bacteria, it is not the preferred prophylactic agent for *Pseudomonas* in CF due to resistance patterns and lack of efficacy compared to antipseudomonal agents.
*Oral amoxicillin/clavulanic acid*
- This combination antibiotic is effective against a broad spectrum of bacteria, including *Haemophilus influenzae* and *Moraxella catarrhalis*, but it does not have reliable activity against *Pseudomonas aeruginosa*.
- It is not indicated for prophylactic use against *Pseudomonas* in CF patients.
*Oral ciprofloxacin*
- While oral ciprofloxacin is active against *Pseudomonas aeruginosa* and is sometimes used for acute exacerbations, chronic daily oral quinolone use is generally avoided for prophylaxis due to concerns about resistance development and significant side effects.
- **Inhaled antibiotics** are preferred for chronic suppression in CF as they deliver high concentrations directly to the lungs, minimizing systemic side effects.
*Inhaled levofloxacin*
- Similar to other quinolones, inhaled levofloxacin can be used for *Pseudomonas* infections in CF. However, given the options, **inhaled tobramycin** has a more established and broader role as a first-line inhaled prophylactic option for *Pseudomonas* in CF.
- Resistance patterns and individual patient response would guide the choice between different inhaled antibiotics, but tobramycin is a classic prophylactic agent in this setting.
Cystic fibrosis in adults US Medical PG Question 5: A 3-year-old girl with cystic fibrosis is brought to the physician for a follow-up examination. Her mother has noticed that the child has had multiple falls over the past 4 months while walking, especially in the evening. Her current medications include pancreatic enzyme supplements, an albuterol inhaler, and acetylcysteine. She is at the 10th percentile for height and the 5th percentile for weight. Examination shows dry skin, and cone shaped elevated papules on the trunk and extremities. There is an irregularly shaped foamy gray patch on the left conjunctiva. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Administer niacin
- B. Administer riboflavin
- C. Administer vitamin A (Correct Answer)
- D. Administer zinc
- E. Administer lutein
Cystic fibrosis in adults Explanation: ***Administer vitamin A***
- The patient's symptoms, including **night blindness** (falls in the evening), **dry skin**, **follicular hyperkeratosis** (cone-shaped elevated papules), and **Bitot spots** (foamy gray patch on conjunctiva), are classic signs of **vitamin A deficiency**.
- **Cystic Fibrosis** patients are prone to **fat-soluble vitamin deficiencies** (A, D, E, K) due to pancreatic insufficiency and malabsorption.
*Administer niacin*
- **Niacin (B3) deficiency** causes **pellagra**, characterized by the "4 Ds": **dermatitis**, **diarrhea**, **dementia**, and **death**. These symptoms are not present in this patient.
- While cystic fibrosis can sometimes lead to general malabsorption, specific signs of pellagra are absent.
*Administer riboflavin*
- **Riboflavin (B2) deficiency** typically presents with **chelosis** (cracked lips), **angular stomatitis**, **glossitis**, and **seborrheic dermatitis**.
- The patient's symptoms do not align with riboflavin deficiency.
*Administer zinc*
- **Zinc deficiency** can cause **growth retardation**, **diarrhea**, **alopecia**, and characteristic **periorificial and acral dermatitis**.
- Although malabsorption in cystic fibrosis can affect zinc levels, the specific constellation of symptoms points more directly to vitamin A deficiency.
*Administer lutein*
- **Lutein** is a carotenoid important for eye health, but its deficiency does not cause the widespread systemic symptoms related to night blindness and dermatological changes seen in this patient.
- It's not a primary vitamin, and its deficiency is not managed as acutely as vitamin A deficiency presenting with these severe symptoms.
Cystic fibrosis in adults US Medical PG Question 6: A 24-year-old woman presents to her physician's office complaining of a worsening cough with large volumes of mucoid sputum every morning and thick, foul-smelling sputum almost every time she coughs. She says that this cough started about one month ago and has been increasing in intensity. Over-the-counter medications are ineffective. Past medical history is significant for cystic fibrosis diagnosed at the age of 6 years, and pneumonia twice in the past 2 years. Other than a cough, she has no fever or any other concerns. A sputum sample grows aerobic, non-lactose fermenting, oxidase-positive, gram-negative bacillus. Which of the following treatment regimens is the most beneficial for her at this time?
- A. Postural drainage of the chest
- B. Surgical therapy
- C. Trimethoprim and sulfamethoxazole
- D. Intravenous ciprofloxacin (Correct Answer)
- E. Amoxicillin and clavulanic acid
Cystic fibrosis in adults Explanation: ***Intravenous ciprofloxacin***
- The patient's history of **cystic fibrosis** with recurrent respiratory infections and the isolation of an **aerobic, non-lactose fermenting, oxidase-positive, gram-negative bacillus** (consistent with *Pseudomonas aeruginosa*) strongly indicates the need for targeted antibiotic therapy.
- **Ciprofloxacin** is a fluoroquinolone antibiotic with good activity against *Pseudomonas aeruginosa*, and intravenous administration is appropriate for pulmonary exacerbations in CF patients.
- The worsening cough with large volumes of mucoid and foul-smelling sputum indicates a significant **pulmonary exacerbation** due to bacterial infection, necessitating effective antibiotic coverage.
- While **combination therapy** (typically an anti-pseudomonal beta-lactam plus an aminoglycoside or fluoroquinolone) is often preferred for Pseudomonas exacerbations in CF, **ciprofloxacin is the best option among those listed** as it provides reliable Pseudomonas coverage.
*Postural drainage of the chest*
- **Postural drainage** is an important component of airway clearance therapy in patients with cystic fibrosis and bronchiectasis, helping to mobilize secretions.
- While beneficial for symptom management and part of comprehensive CF care, it is not a primary treatment for an acute bacterial exacerbation and does not address the underlying **bacterial infection**.
*Surgical therapy*
- **Surgical therapy**, such as lung transplantation, is considered for end-stage lung disease in cystic fibrosis or for localized complications like severe bronchiectasis or massive hemoptysis refractory to medical management.
- It is not the initial or primary treatment for an acute infectious exacerbation, especially in a patient without indications for emergent surgical intervention.
*Trimethoprim and sulfamethoxazole*
- **Trimethoprim-sulfamethoxazole (TMP/SMX)** is a broad-spectrum antibiotic effective against many gram-positive and gram-negative organisms.
- However, it has **poor activity against Pseudomonas aeruginosa**, particularly the strains commonly found in cystic fibrosis patients, which often demonstrate intrinsic or acquired resistance to TMP/SMX.
- This makes it an inappropriate choice for treating Pseudomonas pulmonary exacerbations in CF.
*Amoxicillin and clavulanic acid*
- **Amoxicillin-clavulanic acid** is effective against many gram-positive bacteria and some gram-negative organisms, including *Haemophilus influenzae* and *Moraxella catarrhalis*.
- However, it has **minimal to no activity against Pseudomonas aeruginosa**, which is a common and highly virulent pathogen in cystic fibrosis patients, making it an unsuitable choice for this specific infection.
Cystic fibrosis in adults US Medical PG Question 7: A 2-year-old boy is brought to the physician because of an increasing productive cough with a moderate amount of white phlegm for the past week. He has been treated for pneumonia with antibiotic therapy four times over the past year. A chest x-ray performed 3 months ago showed no anatomical abnormalities. He has had multiple episodes of bulky greasy stools that don't flush easily. He is at 3rd percentile for height and at 5th percentile for weight. His temperature is 38°C (100.4°F), pulse is 132/min, and respirations are 44/min. A few inspiratory crackles are heard in the thorax. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Which of the following is the best initial test to determine the underlying etiology of this patient's illness?
- A. X-ray of the chest
- B. Genetic testing
- C. Serum immunoglobulin level
- D. Sweat chloride test (Correct Answer)
- E. Stool analysis
Cystic fibrosis in adults Explanation: ***Sweat chloride test***
- The patient exhibits classic symptoms of **cystic fibrosis**, including recurrent respiratory infections, failure to thrive (low height and weight percentiles), and greasy, bulky stools suggestive of **pancreatic insufficiency**.
- A **sweat chloride test** measures the concentration of chloride in sweat and is the **most reliable initial screening test** for cystic fibrosis, given the characteristic clinical presentation.
*X-ray of the chest*
- While chest X-rays can show evidence of pulmonary involvement (e.g., **bronchiectasis**, hyperinflation), a previous X-ray showed no abnormalities, and it does not directly determine the **underlying etiology** of the multiple symptoms.
- It would be part of the respiratory assessment but is not the best initial test for diagnosing the systemic genetic disorder.
*Genetic testing*
- **Genetic testing** confirms the diagnosis of cystic fibrosis by identifying specific mutations in the **CFTR gene**.
- However, in a patient with a strong clinical suspicion, the **sweat chloride test** is typically performed first as a more accessible and cost-effective initial diagnostic test in many settings, with genetic testing used for confirmation or when sweat test results are equivocal.
*Serum immunoglobulin level*
- **Serum immunoglobulin levels** would assess for **immunodeficiency**, which can cause recurrent infections.
- While recurrent infections are present, the combination of **malabsorption** (greasy stools, failure to thrive) and respiratory symptoms points more strongly towards **cystic fibrosis** than a primary immunodeficiency.
*Stool analysis*
- **Stool analysis** can identify **malabsorption** (e.g., fecal fat content) or indicate **gastrointestinal infections**.
- While it could confirm pancreatic insufficiency, it does not directly diagnose the underlying cause of both respiratory and gastrointestinal symptoms as effectively as a sweat chloride test for cystic fibrosis.
Cystic fibrosis in adults US Medical PG Question 8: A 5-day-old boy is brought to see his pediatrician after his newborn blood screening showed elevated levels of immunoreactive trypsinogen, a marker for cystic fibrosis. The boy was born at 39 weeks gestation after regular prenatal care. He has 2 siblings that tested negative on screening. On physical exam, his vitals are normal and he appears healthy. Which of the following tests should be performed next to evaluate the newborn for cystic fibrosis?
- A. Nasal potential difference
- B. Intestinal current measurement
- C. Measurement of fecal elastase levels
- D. Mutation analysis
- E. Sweat test (Correct Answer)
Cystic fibrosis in adults Explanation: ***Sweat test***
- A **sweat test** is the gold standard for diagnosing cystic fibrosis, measuring **chloride concentration** in sweat which is elevated in CF.
- Given the elevated **immunoreactive trypsinogen (IRT)** on newborn screening, a confirmatory diagnostic test like the sweat test is the appropriate next step.
*Nasal potential difference*
- **Nasal potential difference (NPD)** measures the electrical potential across the nasal epithelium, reflecting **CFTR channel function**.
- While used for CF diagnosis, it is typically employed in cases with **borderline sweat test results** or atypical presentations, not as a primary confirmatory test after positive newborn screening.
*Intestinal current measurement*
- **Intestinal current measurement (ICM)** assesses **chloride secretion** across the intestinal epithelium in response to secretagogues.
- This is a highly specialized research tool, generally not used in routine clinical diagnosis for confirming cystic fibrosis.
*Measurement of fecal elastase levels*
- **Fecal elastase levels** are used to assess **pancreatic exocrine function**, which is often impaired in cystic fibrosis.
- While relevant to CF, it primarily evaluates pancreatic involvement and is not the primary diagnostic test for CF itself following a positive newborn screen, but rather for assessing disease severity.
*Mutation analysis*
- **Mutation analysis** (genetic testing for **CFTR gene mutations**) can identify CF, especially if a sweat test is inconclusive or for screening purposes.
- Although useful, it's often done *after* a positive sweat test or when the sweat test is equivocal, as the **sweat test** remains the initial confirmatory diagnostic test after elevated IRT.
Cystic fibrosis in adults US Medical PG Question 9: A 14-year-old boy is brought to the physician because of increasing swelling of his legs and generalized fatigue for 1 month. During this period he has also had a productive cough and shortness of breath. He has been unable to carry out his daily activities. He has a history of recurrent respiratory tract infections and chronic nasal congestion since childhood. He has a 3-month history of foul-smelling and greasy stools. He is at 4th percentile for height and weight. His temperature is 37°C (98.6°F), pulse is 112/min, respirations are 23/min, and blood pressure is 104/64 mm Hg. Examination shows clubbing of his fingers and scoliosis. There is 2+ pitting edema of the lower extremities. Jugular venous distention is present. Inspiratory crackles are heard in the thorax. Cardiac examination shows a loud S2. The abdomen is mildly distended and the liver is palpated 2 cm below the right costal margin. Hepato-jugular reflux is present. Which of the following is the most likely diagnosis?
- A. Goodpasture syndrome
- B. Hypertrophic cardiomyopathy
- C. Cystic fibrosis (Correct Answer)
- D. Minimal change disease
- E. Protein malnutrition
Cystic fibrosis in adults Explanation: ***Cystic fibrosis***
- Chronic respiratory symptoms (productive cough, recurrent infections, crackles, shortness of breath), malabsorption (foul-smelling, greasy stools, poor growth), and signs of right-sided heart failure (edema, JVD, hepatomegaly, loud S2 indicating **pulmonary hypertension**) are all classic manifestations of **cystic fibrosis**.
- The combination of **respiratory, gastrointestinal, and cardiac involvement** in a child with a history of chronic respiratory issues and poor growth strongly points to this diagnosis.
*Goodpasture syndrome*
- Characterized by rapidly progressive **glomerulonephritis** and **pulmonary hemorrhage**, presenting with hemoptysis and renal dysfunction.
- While it affects lungs, it does not typically cause chronic respiratory infections, malabsorption, or right-sided heart failure in this manner.
*Hypertrophic cardiomyopathy*
- Primarily a genetic disorder causing thickening of the heart muscle, leading to **diastolic dysfunction** and outflow obstruction.
- It would not explain the chronic respiratory infections, malabsorption, or the systemic edema and JVD suggestive of right heart failure secondary to chronic lung disease.
*Minimal change disease*
- A cause of **nephrotic syndrome** in children, characterized by proteinuria, hypoalbuminemia, and edema.
- While it causes significant edema, it does not explain the chronic respiratory symptoms, malabsorption, or the clear signs of cardiac and pulmonary involvement.
*Protein malnutrition*
- Can cause **edema** due to low oncotic pressure (kwashiorkor), and may lead to poor growth and increased susceptibility to infections.
- However, it would not directly cause the specific chronic respiratory symptoms, productive cough, or the obstructive lung disease often indicated by signs of pulmonary hypertension.
Cystic fibrosis in adults US Medical PG Question 10: A 24-year-old male with cystic fibrosis is brought to the emergency room by his mother after he had difficulty breathing. He previously received a lung transplant 6 months ago and was able to recover quickly from the operation. He is compliant with all of his medications and had been doing well with no major complaints until 2 weeks ago when he began to experience shortness of breath. Exam reveals a decreased FEV1/FVC ratio and biopsy reveals lymphocytic infiltration. Which of the following components is present in the airway zone characteristically affected by the most likely cause of this patient's symptoms?
- A. Pseudostratified columnar cells
- B. Goblet cells
- C. Simple cuboidal cells (Correct Answer)
- D. Stratified cuboidal cells
- E. Cartilage
Cystic fibrosis in adults Explanation: ***Simple cuboidal cells***
- The patient's symptoms, history of a lung transplant, and biopsy findings of **lymphocytic infiltration** suggest **bronchiolitis obliterans**, a form of chronic lung allograft dysfunction.
- Bronchiolitis obliterans primarily affects the **small airways** (bronchioles), which are characterized by an epithelial lining of **simple cuboidal cells** and lack cartilage.
*Pseudostratified columnar cells*
- These cells line the **trachea** and **main bronchi** (larger airways), which are typically not the primary site of damage in bronchiolitis obliterans.
- They are part of the **mucociliary escalator** and are also associated with cartilage.
*Goblet cells*
- While present in the **larger airways** along with pseudostratified columnar cells, goblet cells are less prominent or absent in the small bronchioles primarily affected by bronchiolitis obliterans.
- Their characteristic function is mucus production, not the specific epithelial type of the affected bronchioles.
*Stratified cuboidal cells*
- This cell type is **rare** in the respiratory tract and is not characteristic of the small airways affected by bronchiolitis obliterans.
- Stratified epithelia are typically seen in ducts of glands or specialized transitional zones, not the functional bronchioles.
*Cartilage*
- Cartilage provides structural support to the **trachea and main bronchi**, but it is **absent** in the small airways (bronchioles) that are the primary target of bronchiolitis obliterans.
- The presence of cartilage would indicate a larger airway, contradicting the pathophysiology of this condition.
More Cystic fibrosis in adults US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.