COPD pathophysiology and diagnosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for COPD pathophysiology and diagnosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
COPD pathophysiology and diagnosis US Medical PG Question 1: A 63-year-old man with alpha-1-antitrypsin deficiency is brought to the emergency department 1 hour after his daughter found him unresponsive. Despite appropriate care, the patient dies. At autopsy, examination of the lungs shows enlargement of the airspaces in the respiratory bronchioles and alveoli. Enzymatic activity of which of the following cells is the most likely cause of these findings?
- A. Alveolar macrophages (Correct Answer)
- B. Ciliated bronchiolar epithelial cells
- C. Elastic fibers in alveolar septa
- D. Type I pneumocytes
- E. Alveolar septal cells
COPD pathophysiology and diagnosis Explanation: ***Alveolar macrophages***
- In **alpha-1-antitrypsin deficiency**, alveolar macrophages (and neutrophils) release **elastase**, which is normally inhibited by alpha-1-antitrypsin.
- Unchecked elastase activity from alveolar macrophages leads to the **destruction of elastic fibers** in the alveolar walls, causing emphysema with characteristic **panacinar** distribution (worse in lower lobes).
- This results in enlargement of airspaces distal to terminal bronchioles.
*Ciliated bronchiolar epithelial cells*
- These cells are primarily involved in **mucociliary clearance** and do not produce proteolytic enzymes that degrade elastic tissue.
- Their dysfunction would lead to impaired mucus clearance and increased susceptibility to infections, but not emphysema.
*Elastic fibers in alveolar septa*
- Elastic fibers are **extracellular matrix components**, not cells.
- While their destruction is the pathological mechanism of emphysema, they do not have enzymatic activity.
*Type I pneumocytes*
- **Type I pneumocytes** form the structural lining of the alveoli and are primarily involved in gas exchange.
- They do not produce elastase or other proteolytic enzymes responsible for tissue destruction in emphysema.
*Alveolar septal cells*
- This term broadly refers to structural cells including Type I and Type II pneumocytes.
- While these cells may be damaged secondarily in emphysema, they do not produce the elastase responsible for elastic fiber destruction.
COPD pathophysiology and diagnosis US Medical PG Question 2: A 60-year-old woman presents to the clinic with a 3-month history of shortness of breath that worsens on exertion. She also complains of chronic cough that has lasted for 10 years. Her symptoms are worsened even with light activities like climbing up a flight of stairs. She denies any weight loss, lightheadedness, or fever. Her medical history is significant for hypertension, for which she takes amlodipine daily. She has a 70-pack-year history of cigarette smoking and drinks 3–4 alcoholic beverages per week. Her blood pressure today is 128/84 mm Hg. A chest X-ray shows flattening of the diaphragm bilaterally. Physical examination is notable for coarse wheezing bilaterally. Which of the following is likely to be seen with pulmonary function testing?
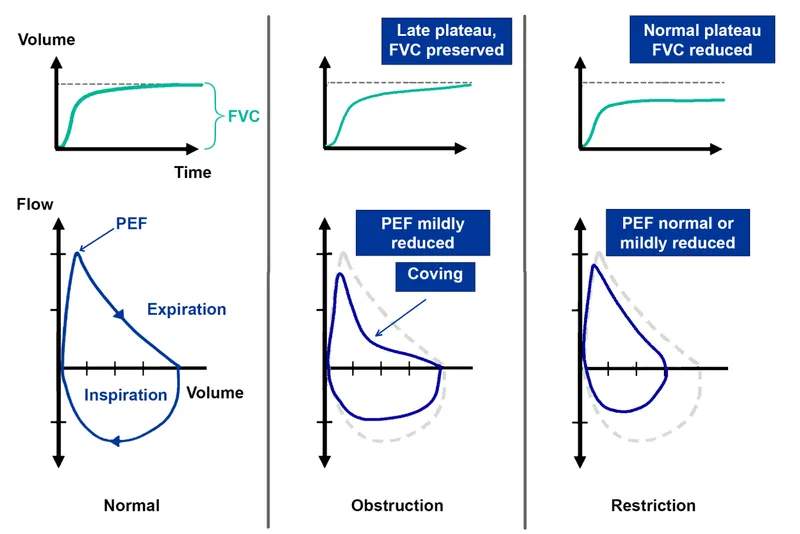
- A. Decreased FEV1: FVC and decreased total lung capacity
- B. Normal FEV1: FVC and decreased total lung capacity
- C. Increased FEV1: FVC and decreased total lung capacity
- D. Decreased FEV1: FVC and increased total lung capacity (Correct Answer)
- E. Increased FEV1: FVC and normal total lung capacity
COPD pathophysiology and diagnosis Explanation: ***Decreased FEV1:FVC ratio and increased total lung capacity***
- This patient's symptoms (shortness of breath on exertion, chronic cough, 70-pack-year smoking history, coarse wheezing, and diaphragmatic flattening on X-ray) are highly suggestive of **Chronic Obstructive Pulmonary Disease (COPD)**, specifically **emphysema**, an obstructive lung disease.
- In COPD, there is airflow limitation, causing a **decreased FEV1:FVC ratio** (typically <0.70). Over time, air trapping occurs due to damaged alveoli and loss of elastic recoil, leading to an **increased total lung capacity (TLC)** and residual volume.
*Decreased FEV1:FVC ratio and decreased total lung capacity*
- A **decreased FEV1:FVC ratio** indicates an **obstructive lung disease**.
- However, a **decreased total lung capacity (TLC)** is characteristic of a **restrictive lung disease**, which does not align with the patient's presentation typical of COPD/emphysema.
*Normal FEV1:FVC ratio and decreased total lung capacity*
- A **normal FEV1:FVC ratio** is inconsistent with the patient's strong history of smoking and symptoms suggestive of airflow obstruction.
- A **decreased total lung capacity (TLC)** indicates a restrictive lung disease, which is not the primary diagnosis here.
*Increased FEV1:FVC ratio and decreased total lung capacity*
- An **increased FEV1:FVC ratio** is not physiologically possible in significant lung disease and is therefore incorrect.
- A **decreased total lung capacity (TLC)** would point towards a restrictive pattern not seen in generalized emphysema.
*Increased FEV1:FVC ratio and normal total lung capacity*
- An **increased FEV1:FVC ratio** is not a characteristic finding in any lung disease and is therefore incorrect.
- A **normal total lung capacity** would not be expected in advanced emphysema where air trapping is prominent.
COPD pathophysiology and diagnosis US Medical PG Question 3: A 48-year-old man comes to the physician because of a 3-month history of worsening shortness of breath and cough productive of frothy, whitish sputum. One year ago, he had a similar episode lasting 6 months. He has smoked a pack of cigarettes daily for 25 years. Physical examination shows bluish discoloration of the tongue and lips. Scattered expiratory wheezing and rhonchi are heard throughout both lung fields. Further evaluation of this patient is most likely to show which of the following findings?
- A. Increased FEV1/FVC ratio
- B. Increased diffusing capacity for carbon monoxide
- C. Increased pulmonary capillary wedge pressure
- D. Increased serum hematocrit (Correct Answer)
- E. Normal FEV1
COPD pathophysiology and diagnosis Explanation: ***Increased serum hematocrit***
- This patient presents with symptoms highly suggestive of **chronic bronchitis**, a form of COPD, characterized by a **chronic productive cough** and **hypoxemia**.
- **Chronic hypoxemia** stimulates the kidneys to release **erythropoietin**, leading to secondary **polycythemia** (increased red blood cell mass) and thus an **increased hematocrit** to improve oxygen-carrying capacity.
*Increased FEV1/FVC ratio*
- This patient's symptoms (shortness of breath, productive cough, wheezing, smoking history) are classic for **chronic obstructive pulmonary disease (COPD)**, which is an **obstructive lung disease**.
- Obstructive lung diseases are characterized by **decreased FEV1/FVC ratio** due to airflow limitation, not an increased ratio.
*Increased diffusing capacity for carbon monoxide*
- In COPD, particularly chronic bronchitis and emphysema, the **diffusing capacity for carbon monoxide (DLCO)** is typically **decreased** due to destruction of alveolar-capillary membranes (emphysema) and ventilation-perfusion mismatch (chronic bronchitis).
- An increased DLCO is more commonly seen in conditions like **pulmonary hemorrhage** or **asthma**.
*Increased pulmonary capillary wedge pressure*
- **Increased pulmonary capillary wedge pressure (PCWP)** is characteristic of **left-sided heart failure**, indicating elevated left atrial and pulmonary venous pressures.
- While patients with severe COPD can develop **pulmonary hypertension** and eventually **right-sided heart failure (cor pulmonale)**, the primary pathology described here points to lung disease, not left ventricular dysfunction.
*Normal FEV1*
- In COPD, there is **airflow obstruction** that manifests as a **reduced forced expiratory volume in 1 second (FEV1)**.
- A normal FEV1 would be inconsistent with the clinical presentation of significant, worsening shortness of breath and airflow limitation.
COPD pathophysiology and diagnosis US Medical PG Question 4: A 55-year-old woman comes to the physician with a 6-month history of cough and dyspnea. She has smoked 1 pack of cigarettes daily for the past 30 years. Analysis of the sputum sample from bronchoalveolar lavage shows abnormal amounts of an isoform of elastase that is normally inhibited by alpha-1 antitrypsin. The cell responsible for secreting this elastase is most likely also responsible for which of the following functions?
- A. Phagocytosis of foreign material (Correct Answer)
- B. Production of lactoferrin
- C. Degradation of toxins
- D. Secretion of mucus
- E. Diffusion of gases
COPD pathophysiology and diagnosis Explanation: ***Phagocytosis of foreign material***
- The abnormal elastase described is **neutrophil elastase**, which is normally inhibited by **alpha-1 antitrypsin**.
- **Neutrophils** are the primary cells responsible for secreting this elastase, and their main function is the **phagocytosis of foreign material** and pathogens.
*Production of lactoferrin*
- **Lactoferrin** is an iron-binding protein with antimicrobial properties, primarily produced by **neutrophils**, but it is not their defining or most unique function in the context of elastase secretion and lung pathology.
- While neutrophils do produce lactoferrin, the question asks for a function that aligns with the described cellular pathology following elastase release.
*Degradation of toxins*
- While certain immune cells and organs (e.g., liver) are involved in **detoxification**, it is not a primary or most characteristic function of **neutrophils** in the lung.
- Neutrophils are more focused on direct microbial killing and inflammation rather than broad toxin degradation.
*Secretion of mucus*
- **Mucus secretion** in the airways is primarily a function of **goblet cells** and submucosal glands, not neutrophils.
- Excessive mucus secretion is a feature of chronic bronchitis, which can coexist with emphysema, but neutrophils themselves do not secrete mucus.
*Diffusion of gases*
- **Gas diffusion** is the primary function of **type I pneumocytes** in the alveolar sacs, which form the thin barrier between air and blood.
- This function is entirely unrelated to the role of neutrophils or the secretion of elastase.
COPD pathophysiology and diagnosis US Medical PG Question 5: A 62-year-old woman with hypertension and type 2 diabetes mellitus comes to the physician because of increasing shortness of breath and a dry cough over the past 6 months. She has smoked 1 pack of cigarettes daily for the past 40 years. Chest auscultation shows scattered expiratory wheezes in both lung fields. Spirometry shows an FEV1:FVC ratio of 65% and an FEV1 of 70% of predicted. Her diffusing capacity for carbon monoxide (DLCO) is 42% of predicted. Which of the following is the most likely diagnosis?
- A. Pulmonary fibrosis
- B. Bronchial asthma
- C. Emphysema (Correct Answer)
- D. Bronchiectasis
- E. Chronic bronchitis
COPD pathophysiology and diagnosis Explanation: ***Emphysema***
- The patient's history of **40 pack-years of smoking**, combined with **obstructive lung disease (FEV1:FVC ratio of 65%)** and a **markedly reduced DLCO (42% of predicted)**, strongly indicates emphysema.
- **DLCO reduction** is characteristic of emphysema due to the destruction of alveolar-capillary membranes, which impairs gas exchange.
*Pulmonary fibrosis*
- Pulmonary fibrosis presents with shortness of breath and dry cough, but it is a **restrictive lung disease**, meaning both FEV1 and FVC would be reduced proportionally, leading to a **normal or increased FEV1:FVC ratio**.
- While DLCO is reduced in pulmonary fibrosis, the **obstructive pattern on spirometry** rules out this diagnosis.
*Bronchial asthma*
- Asthma is characterized by **reversible airway obstruction** and often presents with wheezing and shortness of breath.
- However, asthma typically has a **normal DLCO**, as the diffusion capacity of the lung is usually preserved.
*Bronchiectasis*
- Bronchiectasis involves **permanent dilation of the bronchi** and can cause chronic cough, sputum production, and obstructive lung physiology.
- While it can cause some airflow obstruction and reduced DLCO in severe cases, the **primary features often include chronic productive cough** and recurrent infections, and the DLCO reduction is typically less severe than seen in emphysema, unless it's very advanced.
*Chronic bronchitis*
- Chronic bronchitis is defined by a **chronic productive cough** for at least 3 months in each of 2 consecutive years, in a patient for whom other causes have been excluded.
- It causes **obstructive lung disease** and can present with wheezing but typically has a **normal or only slightly reduced DLCO**, as the primary issue is inflammation and mucus production in the airways, not destruction of the alveolar-capillary membrane.
COPD pathophysiology and diagnosis US Medical PG Question 6: A 53-year-old woman presents to a physician with a cough which she has had for the last 5 years. She mentions that her cough is worse in the morning and is associated with significant expectoration. There is no history of weight loss or constitutional symptoms like fever and malaise. Her past medical records show that she required hospitalization for breathing difficulty on 6 different occasions in the last 3 years. She also mentions that she was never completely free of her respiratory problems during the period between the exacerbations and that she has a cough with sputum most of the months for the last 3 years. She works in a cotton mill and is a non-smoker. Her mother and her maternal grandmother had asthma. Her temperature is 37.1°C (98.8°F), the pulse is 92/min, the blood pressure is 130/86 mm Hg, and her respiratory rate is 22/min. General examination shows obesity and mild cyanosis. Auscultation of her chest reveals bilateral coarse rhonchi. Her lung volumes on pulmonary function test are given below:
Pre-bronchodilator Post-bronchodilator
FEV1 58% 63%
FVC 90% 92%
FEV1/FVC 0.62 0.63
TLC 98% 98%
The results are valid and repeatable as per standard criteria. Which of the following is the most likely diagnosis?
- A. Idiopathic pulmonary fibrosis
- B. Chronic bronchitis (Correct Answer)
- C. Asthma
- D. Extrinsic allergic alveolitis
- E. Emphysema
COPD pathophysiology and diagnosis Explanation: ***Chronic bronchitis***
- The patient presents with a chronic cough and sputum production for at least 3 months a year for 2 consecutive years, consistent with the definition of **chronic bronchitis**.
- **Obstructive pattern** on PFT (FEV1/FVC < 0.70) with minimal reversibility, along with a history of recurrent exacerbations, supports this diagnosis.
*Idiopathic pulmonary fibrosis*
- Characterized by a **restrictive ventilatory defect** (reduced TLC) and often presents with progressive dyspnea and dry cough, which contradicts the patient's PFTs and productive cough.
- Would show **pulmonary fibrosis** on imaging, not suggested by the patient's presentation.
*Asthma*
- Typically presents with **reversible airway obstruction** (significant improvement in FEV1 post-bronchodilator), which is not seen here (only 5% improvement).
- Although the patient's mother and grandmother had asthma, her symptoms and PFTs do not align with active asthma exacerbations.
*Extrinsic allergic alveolitis*
- Usually involves **exposure to inhaled allergens** leading to inflammation of the alveoli, presenting with restrictive lung disease and often acute or subacute symptoms.
- The patient's occupational exposure to cotton mill might suggest **byssinosis**, a type of occupational lung disease, but her PFTs and prolonged chronic cough are more consistent with bronchitis.
*Emphysema*
- Primarily defined by **destruction of alveolar walls** leading to air trapping and severe airflow obstruction, often associated with a history of smoking.
- While it causes an obstructive pattern, the prominent chronic productive cough and minimal reversibility point more towards the airway inflammation of bronchitis rather than the parenchymal destruction of emphysema.
COPD pathophysiology and diagnosis US Medical PG Question 7: A 65-year-old man comes to the physician because of a 10-month history of progressive shortness of breath and a cough productive of a small amount of white phlegm. Bilateral end-expiratory wheezing is heard on auscultation of the chest. Pulmonary function tests show total lung capacity that is 108% of predicted, an FEV1 that is 56% of predicted, and an FEV1:FVC ratio of 62%. Which of the following interventions is most likely to slow the decline in FEV1 in this patient?
- A. Salmeterol therapy
- B. Fluticasone therapy
- C. Smoking cessation (Correct Answer)
- D. Alpha-1 antitrypsin therapy
- E. Breathing exercises
COPD pathophysiology and diagnosis Explanation: ***Smoking cessation***
- This patient's symptoms (progressive shortness of breath, cough, end-expiratory wheezing) and PFT results (reduced FEV1, reduced FEV1:FVC ratio, normal TLC) are highly suggestive of **COPD**, which is primarily caused by smoking.
- **Smoking cessation** is the only intervention clearly shown to slow the rate of FEV1 decline in patients with COPD, thereby improving long-term prognosis.
*Salmeterol therapy*
- **Salmeterol** is a long-acting beta-agonist (LABA) that provides bronchodilation and symptom relief in COPD.
- While it improves symptoms and quality of life, it does **not alter the natural history of the disease** or slow the decline in FEV1.
*Fluticasone therapy*
- **Fluticasone** is an inhaled corticosteroid (ICS) used in COPD, often in combination with LABAs, particularly for patients with frequent exacerbations.
- ICS therapy can reduce exacerbations but does **not slow the FEV1 decline** in COPD and may increase the risk of pneumonia.
*Alpha-1 antitrypsin therapy*
- **Alpha-1 antitrypsin deficiency** is a genetic cause of emphysema, typically presenting at a younger age or with a strong family history. This patient's history does not directly point to this diagnosis.
- While augmentation therapy with alpha-1 antitrypsin can slow lung function decline in genetically deficient individuals, it is **ineffective for typical smoking-induced COPD**.
*Breathing exercises*
- **Breathing exercises**, such as pursed-lip breathing, are components of pulmonary rehabilitation programs.
- They can improve symptoms, exercise tolerance, and quality of life but do **not impact the underlying disease progression** or FEV1 decline in COPD.
COPD pathophysiology and diagnosis US Medical PG Question 8: A 68-year-old, overweight gentleman with a 20-pack-year history of smoking presents to the primary care physician after noticing multiple blood-stained tissues after coughing attacks in the last month. His vital signs are within normal limits except for an O2 saturation of 93% on room air. He states that over the last 5 years his cough has continued to worsen and has never truly improved. He states that his shortness of breath has also worsened over this time period, as now he can barely make it up the flight of stairs in his home. In this patient, what is the most likely cause of his hemoptysis?
- A. Chronic bronchitis
- B. Bronchogenic carcinoma (Correct Answer)
- C. Lung abscess
- D. Acute pulmonary edema
- E. Goodpasture's disease
COPD pathophysiology and diagnosis Explanation: ***Bronchogenic carcinoma (Lung cancer)***
- **Hemoptysis in a smoker is lung cancer until proven otherwise** - this is a critical clinical principle in respiratory medicine.
- This patient has major risk factors: **20-pack-year smoking history**, age 68, and chronic progressive symptoms.
- **Hemoptysis** is a common presenting symptom of lung cancer, occurring in 20-50% of patients, caused by tumor invasion of bronchial vessels.
- The **chronic progressive dyspnea** and **worsening cough over 5 years** suggest an evolving mass lesion or bronchial obstruction.
- **Hypoxemia** (O2 sat 93%) indicates significant pulmonary compromise.
- While this patient likely has underlying COPD/chronic bronchitis as a comorbidity, the presence of hemoptysis mandates urgent evaluation for malignancy.
*Chronic bronchitis*
- While this patient likely has chronic bronchitis (a type of COPD) given the smoking history and chronic productive cough, **hemoptysis is NOT a typical feature** of uncomplicated chronic bronchitis.
- Hemoptysis in chronic bronchitis is rare and usually minimal; its presence should prompt investigation for other causes, particularly malignancy.
- Chronic bronchitis explains the dyspnea and chronic cough but does not explain the hemoptysis.
*Lung abscess*
- A lung abscess typically presents with **acute onset of fever**, chills, night sweats, and **foul-smelling purulent sputum**, none of which are mentioned in this case.
- The **chronic, progressive nature over five years** is inconsistent with an acute infectious process.
*Acute pulmonary edema*
- Acute pulmonary edema presents with **sudden onset of severe dyspnea**, orthopnea, and often pink frothy sputum due to acute cardiac decompensation.
- The **gradual progression over five years** rules out an acute cardiac event.
- Vital signs are stable, with no mention of cardiac findings.
*Goodpasture's disease*
- This rare autoimmune disorder causes **pulmonary-renal syndrome** with glomerulonephritis and pulmonary hemorrhage.
- Typically affects younger patients (20s-30s) with acute presentation.
- There are **no renal symptoms** (hematuria, oliguria, elevated creatinine) to suggest this diagnosis.
COPD pathophysiology and diagnosis US Medical PG Question 9: A 40-year-old man comes to the physician because of a 2-year history of gradually worsening shortness of breath. He smoked half a pack of cigarettes daily for 10 years but stopped 8 years ago. His pulse is 72/min, blood pressure is 135/75 mm Hg, and respirations are 20/min. Examination shows an increased anteroposterior diameter of the chest. Diminished breath sounds are heard on auscultation of the chest. An x-ray of the chest shows widened intercostal spaces, a flattened diaphragm, and bilateral hyperlucency of the lung bases. This patient's condition puts him at greatest risk for which of the following conditions?
- A. Antineutrophil cytoplasmic antibody-positive vasculitis
- B. Bronchiolitis obliterans
- C. IgA nephropathy
- D. Bronchogenic carcinoma (Correct Answer)
- E. Hepatocellular carcinoma
COPD pathophysiology and diagnosis Explanation: ***Bronchogenic carcinoma***
- The patient's presentation with **shortness of breath**, history of **smoking**, and chest X-ray findings (increased AP diameter, flattened diaphragm, hyperlucency) are highly suggestive of **emphysema**, a strong risk factor for bronchogenic carcinoma.
- While he stopped smoking 8 years ago, his past smoking history significantly increases his lifetime risk for lung cancer, and emphysema itself is an independent risk factor for malignancies.
*Antineutrophil cytoplasmic antibody-positive vasculitis*
- This condition involves systemic inflammation of blood vessels, often affecting the **lungs and kidneys**, but there are no clinical or radiological findings suggestive of vasculitis here.
- There is no mention of symptoms like **hematuria**, **rash**, or other systemic inflammatory signs that would point towards ANCA-positive vasculitis.
*Bronchiolitis obliterans*
- This is a rare, severe obstructive lung disease often caused by toxic inhalant exposure (e.g., **sulfur mustard**, **diacetyl**) or as a complication of **lung transplantation** or **rheumatoid arthritis**, none of which are indicated in this patient.
- While it can cause shortness of breath, the characteristic imaging findings in this patient (hyperlucency, flattened diaphragm) are more indicative of **emphysema**, not bronchiolitis obliterans.
*IgA nephropathy*
- This is a **primary glomerulonephritis** characterized by IgA deposits in the glomeruli, leading to **hematuria** and **proteinuria**, and is not related to the patient's respiratory symptoms or imaging findings.
- There is no clinical information provided that would suggest renal involvement.
*Hepatocellular carcinoma*
- This is a **primary liver cancer** typically associated with chronic liver diseases like **hepatitis B** or **C infections**, **cirrhosis**, or **alcohol abuse**, none of which are suggested in the patient's history.
- The patient's symptoms and diagnostic findings are entirely focused on the respiratory system, with no indication of liver disease.
COPD pathophysiology and diagnosis US Medical PG Question 10: A 70-year-old man presents to a physician with a cough and difficulty breathing during the last 7 years. He has smoked since his teenage years and regularly inhales tiotropium, formoterol, and budesonide and takes oral theophylline. The number of exacerbations has been increasing over the last 6 months. His temperature is 37.2°C (99°F), the heart rate is 92/min, the blood pressure is 134/88 mm Hg and the respiratory rate is 26/min. On chest auscultation breath sounds are diffusely decreased and bilateral rhonchi are present. Pulse oximetry shows his resting oxygen saturation to be 88%. Chest radiogram shows a flattened diaphragm, hyperlucency of the lungs, and a long, narrow heart shadow. The physician explains this condition to the patient and emphasizes the importance of smoking cessation. In addition to this, which of the following is most likely to reduce the risk of mortality from the condition?
- A. Roflumilast
- B. Low-dose oral prednisone
- C. Pulmonary rehabilitation
- D. Supplemental oxygen (Correct Answer)
- E. Prophylactic azithromycin
COPD pathophysiology and diagnosis Explanation: ***Supplemental oxygen***
- The patient's **resting oxygen saturation of 88%** indicates significant hypoxemia, which, if chronic, places a high burden on the cardiovascular system and is a strong predictor of premature mortality in **COPD**.
- **Long-term oxygen therapy (LTOT)** for at least 15 hours a day has been shown to improve survival in patients with severe chronic hypoxemia due to COPD.
*Roflumilast*
- **Roflumilast** is a phosphodiesterase-4 inhibitor that reduces inflammation and is used to decrease exacerbations in severe COPD associated with chronic bronchitis and a history of frequent exacerbations.
- While it can improve lung function and reduce exacerbations, it has not been shown to reduce mortality directly.
*Low-dose oral prednisone*
- **Oral corticosteroids** are primarily used for acute exacerbations of COPD, not for long-term maintenance due to significant systemic side effects like osteoporosis, muscle weakness, and increased infection risk.
- While they can temporarily reduce inflammation, chronic low-dose use is not recommended for mortality benefit and may cause harm in the long run.
*Pulmonary rehabilitation*
- **Pulmonary rehabilitation** is a comprehensive program that improves exercise tolerance, dyspnea, and quality of life in patients with COPD.
- It does not directly reduce mortality but significantly improves functional status and potentially reduces hospitalizations.
*Prophylactic azithromycin*
- **Prophylactic azithromycin** can reduce the frequency of exacerbations in select patients with severe COPD, likely due to its anti-inflammatory and immunomodulatory properties, as well as its bactericidal effect.
- Similar to roflumilast, it reduces exacerbations but has not been shown to reduce mortality directly in COPD patients.
More COPD pathophysiology and diagnosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.