Bronchiectasis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bronchiectasis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bronchiectasis US Medical PG Question 1: In patients with chronic obstructive pulmonary disease, stimulation of muscarinic acetylcholine receptors results in an increase in mucus secretion, smooth muscle contraction and bronchoconstriction. The end result is an increase in airway resistance. Which of the following pharmacologic agents interferes directly with this pathway?
- A. Epinephrine
- B. Albuterol
- C. Theophylline
- D. Ipratropium (Correct Answer)
- E. Metoprolol
Bronchiectasis Explanation: ***Ipratropium***
- **Ipratropium** is an **anticholinergic** agent that blocks muscarinic acetylcholine receptors.
- By blocking these receptors, it **reduces bronchoconstriction**, mucus secretion, and smooth muscle contraction, thus decreasing airway resistance.
*Epinephrine*
- **Epinephrine** is a non-selective **adrenergic agonist** that stimulates both alpha and beta receptors.
- Its effects in the airways are primarily mediated through **beta-2 agonism**, leading to bronchodilation, but it does not directly interfere with muscarinic pathways.
*Albuterol*
- **Albuterol** is a **short-acting beta-2 adrenergic agonist (SABA)**.
- It primarily causes bronchodilation by stimulating beta-2 receptors on airway smooth muscle, independent of the muscarinic pathway.
*Theophylline*
- **Theophylline** is a **methylxanthine** that primarily acts as a non-selective phosphodiesterase inhibitor.
- This leads to increased intracellular **cAMP** and bronchodilation, but it does not directly block muscarinic acetylcholine receptors.
*Metoprolol*
- **Metoprolol** is a **selective beta-1 adrenergic blocker** (beta-blocker).
- Its primary action is on the heart; it has minimal effect on airway beta-2 receptors at therapeutic doses due to its selectivity, and it does not interfere with the muscarinic pathway.
Bronchiectasis US Medical PG Question 2: A 29-year-old man presents for the evaluation of infertility. He has a history of recurrent lower respiratory tract infections, productive cough, abdominal pain, and diarrhea. Physical examination reveals clubbing and bilateral crackles on chest auscultation. Chest X-ray reveals increased pulmonary markings and peripheral bronchi with a ‘tram track’ appearance. Which of the following pathophysiologies is responsible for the patient’s condition?
- A. Fibrosis of the lung parenchyma
- B. Bronchial hypersensitivity
- C. Abnormal ciliary motion
- D. Gluten hypersensitivity
- E. Defective chloride transport (Correct Answer)
Bronchiectasis Explanation: ***Defective chloride transport***
- The patient's presentation with **recurrent respiratory infections**, **bronchiectasis** (tram track appearance on CXR), **clubbing**, and **infertility** is highly suggestive of **cystic fibrosis**.
- **Cystic fibrosis** is caused by mutations in the **CFTR gene**, leading to **defective chloride transport** across epithelial cells, resulting in thick, viscous secretions.
*Fibrosis of the lung parenchyma*
- While chronic lung disease can lead to some **pulmonary fibrosis**, it is not the primary underlying pathophysiology described here.
- Pulmonary fibrosis typically presents with **restrictive lung disease** and interstitial patterns on imaging, rather than the prominent **bronchiectasis** seen in this patient.
*Bronchial hypersensitivity*
- This is characteristic of **asthma**, which involves airway inflammation and bronchoconstriction, but typically does not cause the extensive **recurrent infections**, **bronchiectasis**, or **infertility** seen in this case.
- Asthma is less likely to result in **clubbing** or the progressive lung damage implied by a "tram track" appearance.
*Abnormal ciliary motion*
- This describes **primary ciliary dyskinesia (PCD)**, which can also cause recurrent respiratory infections and male infertility due to **immotile sperm**.
- However, PCD typically presents with **situs inversus** in a significant proportion of cases and does not involve the characteristic **exocrine gland dysfunction** (e.g., severe abdominal symptoms, pancreatic insufficiency leading to diarrhea) often seen in cystic fibrosis implied by the broad clinical picture.
*Gluten hypersensitivity*
- Also known as **celiac disease**, this is primarily a **gastrointestinal condition** characterized by malabsorption due to immune reactions to gluten.
- While celiac disease can cause **abdominal pain** and **diarrhea**, it does not explain the **recurrent respiratory infections**, **bronchiectasis**, **clubbing**, or **male infertility**.
Bronchiectasis US Medical PG Question 3: A 28-year-old man presents to his primary care provider because of shortness of breath, cough, and wheezing. He reports that in high school, he occasionally had shortness of breath and would wheeze after running. His symptoms have progressively worsened over the past 6 months and are now occurring daily. He also finds himself being woken up from sleep by his wheeze approximately 3 times a week. His medical history is unremarkable. He denies tobacco use or excessive alcohol consumption. His temperature is 37.1°C (98.8°F), blood pressure is 121/82 mm Hg, and heart rate is 82/min. Physical examination is remarkable for expiratory wheezing bilaterally. Spirometry shows an FEV1 of 73% of predicted, which improves by 19% with albuterol. In addition to a short-acting beta-agonist as needed, which of the following is the most appropriate therapy for this patient?
- A. A high-dose inhaled corticosteroid and a long-acting beta-agonist
- B. A long-acting beta-agonist alone
- C. A low-dose inhaled corticosteroid alone
- D. A medium-dose inhaled corticosteroid and a long-acting beta-agonist
- E. A low-dose inhaled corticosteroid and a long-acting beta-agonist (Correct Answer)
Bronchiectasis Explanation: ***A low-dose inhaled corticosteroid and a long-acting beta-agonist***
- This patient presents with **persistent asthma symptoms** (daily symptoms, nighttime awakenings 3x/week, and a significant bronchodilator response) that are not controlled by a short-acting beta-agonist alone. This indicates **moderate persistent asthma**.
- According to GINA guidelines, the appropriate step-up therapy for moderate persistent asthma is a **low-dose inhaled corticosteroid (ICS) combined with a long-acting beta-agonist (LABA)**.
*A high-dose inhaled corticosteroid and a long-acting beta-agonist*
- **High-dose ICS/LABA** is reserved for **severe uncontrolled asthma**, typically as Step 4 or 5 therapy, when symptoms persist despite lower-dose combinations or higher-step single agents.
- The patient's current symptoms, while persistent, do not warrant immediate initiation of high-dose therapy as initial step-up from mild persistent.
*A long-acting beta-agonist alone*
- **LABAs should never be used as monotherapy** in asthma due to the risk of severe asthma exacerbations and asthma-related death.
- They must always be combined with an **inhaled corticosteroid** to control underlying airway inflammation.
*A low-dose inhaled corticosteroid alone*
- While a **low-dose ICS alone** is appropriate for **mild persistent asthma** (Step 2), this patient's symptoms (daily symptoms, nighttime awakenings 3x/week) are more severe than mild persistent.
- His severity warrants combination therapy (ICS/LABA) to achieve better symptom control.
*A medium-dose inhaled corticosteroid and a long-acting beta-agonist*
- A **medium-dose ICS/LABA** is typically considered for patients whose asthma remains **uncontrolled on low-dose ICS/LABA**, representing Step 4 therapy.
- Given that this is the initial step-up from SABA-only use, medium-dose is generally too aggressive and should be reserved for subsequent steps if the low-dose combination proves insufficient.
Bronchiectasis US Medical PG Question 4: A 62-year-old woman with hypertension and type 2 diabetes mellitus comes to the physician because of increasing shortness of breath and a dry cough over the past 6 months. She has smoked 1 pack of cigarettes daily for the past 40 years. Chest auscultation shows scattered expiratory wheezes in both lung fields. Spirometry shows an FEV1:FVC ratio of 65% and an FEV1 of 70% of predicted. Her diffusing capacity for carbon monoxide (DLCO) is 42% of predicted. Which of the following is the most likely diagnosis?
- A. Pulmonary fibrosis
- B. Bronchial asthma
- C. Emphysema (Correct Answer)
- D. Bronchiectasis
- E. Chronic bronchitis
Bronchiectasis Explanation: ***Emphysema***
- The patient's history of **40 pack-years of smoking**, combined with **obstructive lung disease (FEV1:FVC ratio of 65%)** and a **markedly reduced DLCO (42% of predicted)**, strongly indicates emphysema.
- **DLCO reduction** is characteristic of emphysema due to the destruction of alveolar-capillary membranes, which impairs gas exchange.
*Pulmonary fibrosis*
- Pulmonary fibrosis presents with shortness of breath and dry cough, but it is a **restrictive lung disease**, meaning both FEV1 and FVC would be reduced proportionally, leading to a **normal or increased FEV1:FVC ratio**.
- While DLCO is reduced in pulmonary fibrosis, the **obstructive pattern on spirometry** rules out this diagnosis.
*Bronchial asthma*
- Asthma is characterized by **reversible airway obstruction** and often presents with wheezing and shortness of breath.
- However, asthma typically has a **normal DLCO**, as the diffusion capacity of the lung is usually preserved.
*Bronchiectasis*
- Bronchiectasis involves **permanent dilation of the bronchi** and can cause chronic cough, sputum production, and obstructive lung physiology.
- While it can cause some airflow obstruction and reduced DLCO in severe cases, the **primary features often include chronic productive cough** and recurrent infections, and the DLCO reduction is typically less severe than seen in emphysema, unless it's very advanced.
*Chronic bronchitis*
- Chronic bronchitis is defined by a **chronic productive cough** for at least 3 months in each of 2 consecutive years, in a patient for whom other causes have been excluded.
- It causes **obstructive lung disease** and can present with wheezing but typically has a **normal or only slightly reduced DLCO**, as the primary issue is inflammation and mucus production in the airways, not destruction of the alveolar-capillary membrane.
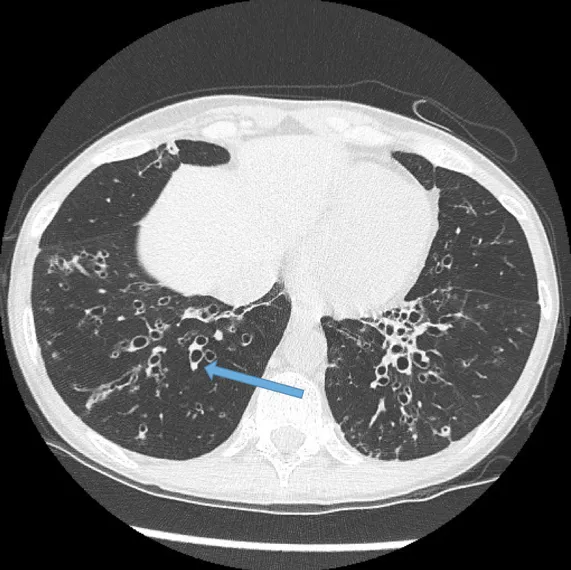
Bronchiectasis US Medical PG Question 5: A 52-year-old man comes to the physician because of a 6-month history of shortness of breath and nonproductive cough. He has smoked 1 pack of cigarettes daily for 15 years. Cardiopulmonary examination shows fine inspiratory crackles bilaterally. There is clubbing present in the fingers bilaterally. Pulmonary function tests (PFTs) show an FVC of 78% of expected and an FEV1/FVC ratio of 92%. A CT scan of the chest is shown. Which of the following is the most likely underlying diagnosis?
- A. Bronchopulmonary aspergillosis
- B. Pulmonary fibrosis (Correct Answer)
- C. Chronic obstructive pulmonary disease
- D. Chronic bronchiectasis
- E. Pulmonary tuberculosis
Bronchiectasis Explanation: ***Pulmonary fibrosis***
- The CT scan shows a pattern of **reticular opacities** and **honeycombing**, classic features of **pulmonary fibrosis**.
- Clinical presentation with **progressive dyspnea**, nonproductive cough, **fine inspiratory crackles**, and **clubbing** are highly suggestive of interstitial lung disease, with PFTs showing a **restrictive pattern** (reduced FVC, preserved FEV1/FVC ratio).
*Bronchopulmonary aspergillosis*
- This condition is typically characterized by **recurrent fleeting infiltrates**, **bronchiectasis**, and **eosinophilia** in asthmatic patients, which are not described.
- The CT findings would usually show **bronchial wall thickening** and **mucus plugging**, rather than widespread fibrosis and honeycombing.
*Chronic obstructive pulmonary disease*
- COPD typically presents with an **obstructive pattern** on PFTs (reduced FEV1/FVC ratio), which is not seen here.
- While smoking is a risk factor, the chest CT findings of extensive **honeycombing** and **fibrosis** are not characteristic of emphysema or chronic bronchitis.
*Chronic bronchiectasis*
- Bronchiectasis is characterized by **permanent dilatation of the bronchi**, often leading to chronic cough with copious sputum production and recurrent infections.
- While the CT scan may show some dilated airways, the predominant pattern of **honeycombing** and **reticular opacities** is more indicative of fibrosis, and the clinical picture does not emphasize chronic productive cough or infections.
*Pulmonary tuberculosis*
- Pulmonary tuberculosis presents with various patterns on CT, often including **cavitary lesions**, **nodules**, or **fibrocalcific changes**, typically in the upper lobes.
- The diffuse interstitial changes and **honeycombing** seen on this CT are not typical for tuberculosis, and symptoms like fever, night sweats, or weight loss are not mentioned.
Bronchiectasis US Medical PG Question 6: A 51-year-old woman is brought to the emergency department because of an aggressive cough with copious amounts of thick, foamy, yellow-green sputum. She says she has had this cough for about 11 years with exacerbations similar to her presentation today. She also reports that her cough is worse in the morning. She was evaluated multiple times in the past because of recurrent bouts of bronchitis that have required treatment with antibiotics. She is a non-smoker. On physical examination, the blood pressure is 125/78 mm Hg, pulse rate is 80/min, respiratory rate is 16/min, and temperature is 36.7°C (98.0°F). Chest auscultation reveals crackles and wheezing over the right middle lobe and the rest of her physical examinations are normal. The chest X-ray shows irregular opacities in the right middle lobe and diffuse airway thickening. Based on this history and physical examination, which of the following is the most likely diagnosis?
- A. Bronchiectasis (Correct Answer)
- B. Tuberculosis
- C. Chronic bronchitis
- D. Chronic obstructive pulmonary disease
- E. Alpha-1-antitrypsin deficiency
Bronchiectasis Explanation: ***Correct: Bronchiectasis***
- The classic presentation of **chronic cough with copious, purulent sputum** (thick, foamy, yellow-green) lasting 11 years is pathognomonic for bronchiectasis
- **Recurrent respiratory infections** requiring multiple antibiotic courses indicate permanent airway damage with impaired mucus clearance
- **Morning cough** reflects postural drainage of secretions that accumulated overnight in dilated bronchi
- **Non-smoker status** with chronic symptoms points to structural lung disease rather than smoking-related conditions
- Chest X-ray findings of **irregular opacities in right middle lobe and diffuse airway thickening** are characteristic of bronchiectasis (permanent dilation and thickening of airways)
- Right middle lobe is a common location for bronchiectasis due to anatomical drainage issues
*Incorrect: Tuberculosis*
- While TB can cause chronic cough and lung lesions, the **copious, foamy, purulent sputum** production is not typical of TB
- TB typically presents with **constitutional symptoms** (fever, night sweats, weight loss), which are absent here
- Chest X-ray in TB classically shows **apical infiltrates, cavitation, or granulomas**, not diffuse airway thickening
- The 11-year history with stable exacerbations would be unusual for untreated TB
*Incorrect: Chronic bronchitis*
- Chronic bronchitis requires **productive cough for ≥3 months per year for ≥2 consecutive years**, but is **strongly associated with smoking**
- This patient is a **non-smoker**, making chronic bronchitis unlikely
- The imaging finding of **diffuse airway thickening** suggests permanent structural changes (bronchiectasis) rather than simple mucosal inflammation
- Chronic bronchitis doesn't typically cause localized findings in one lobe
*Incorrect: Chronic obstructive pulmonary disease*
- COPD is characterized by **irreversible airflow limitation** and is almost exclusively seen in **smokers** or those with significant environmental exposure
- This **non-smoking patient** lacks the primary risk factor for COPD
- The dominant clinical features of **copious purulent sputum and airway thickening** are more consistent with bronchiectasis than the emphysema or chronic bronchitis components of COPD
- Physical exam would typically show **hyperinflation, decreased breath sounds, and prolonged expiration** in COPD, not localized crackles
*Incorrect: Alpha-1-antitrypsin deficiency*
- This genetic condition causes **early-onset emphysema** (typically age 30-40s) in non-smokers and may cause liver disease
- While it can present without smoking history, the predominant feature is **lower lobe-predominant emphysema**, not bronchiectasis
- The clinical picture of **copious purulent sputum, recurrent infections, and airway thickening** is inconsistent with primary alpha-1-antitrypsin deficiency
- This condition would show **hyperinflation and reduced lung markings** on imaging, not airway thickening
Bronchiectasis US Medical PG Question 7: A 10-year-old boy is brought to the clinic by his mother with complaints of cough productive of yellow sputum for the past couple of weeks. This is the 4th episode the boy has had this year. He has had recurrent episodes of cough since childhood, and previous episodes have subsided with antibiotics. There is no family history of respiratory disorders. His vaccinations are up to date. He has a heart rate of 98/min, respiratory rate of 13/min, temperature of 37.6°C (99.7°F), and blood pressure of 102/70 mm Hg. Auscultation of the chest reveals an apex beat on the right side of the chest. A chest X-ray reveals that the cardiac apex is on the right. A high-resolution CT scan is performed which is suggestive of bronchiectasis. Which of the following structures is most likely impaired in this patient?
- A. Neurofilaments
- B. Dynein (Correct Answer)
- C. Kinesin
- D. Microvilli
- E. Microfilaments
Bronchiectasis Explanation: ***Dynein***
- The combination of **recurrent respiratory infections** leading to **bronchiectasis** and **situs inversus** (apex beat on the right, cardiac apex on the right) is characteristic of **primary ciliary dyskinesia (PCD)**, also known as Kartagener syndrome.
- **Dynein arms** are crucial for the beating motion of cilia. An impairment in dynein function leads to ineffective ciliary clearance in the respiratory tract and defective embryonic rotation, causing situs inversus.
*Neurofilaments*
- **Neurofilaments** are intermediate filaments found in neurons, primarily providing structural support to axons.
- Their dysfunction is associated with various neurological disorders, but not with respiratory infections or situs inversus.
*Kinesin*
- **Kinesin** is a motor protein that moves along microtubules, typically transporting cargo away from the cell nucleus (anterograde transport).
- While important for intracellular transport, kinesin dysfunction does not explain the specific constellation of symptoms seen in primary ciliary dyskinesia.
*Microvilli*
- **Microvilli** are actin-filled projections on the surface of some epithelial cells, primarily increasing surface area for absorption.
- They are not involved in ciliary motility or mucociliary clearance, and their impairment would not lead to bronchiectasis or situs inversus.
*Microfilaments*
- **Microfilaments** (actin filaments) are involved in cell shape, motility, and cytokinesis, but are not the primary structural component responsible for ciliary beating.
- While integral to many cellular processes, their direct impairment does not cause the specific symptoms of primary ciliary dyskinesia.
Bronchiectasis US Medical PG Question 8: A 65-year-old man is brought to the emergency department after coughing up copious amounts of blood-tinged sputum at his nursing home. He recently had an upper respiratory tract infection that was treated with antibiotics. He has a long-standing history of productive cough that has worsened since he had a stroke 3 years ago. He smoked a pack of cigarettes daily for 40 years until the stroke, after which he quit. The patient appears distressed and short of breath. His temperature is 38°C (100.4°F), pulse is 92/min, and blood pressure is 145/85 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Physical examination shows digital clubbing and cyanosis of the lips. Coarse crackles are heard in the thorax. An x-ray of the chest shows increased translucency and tram-track opacities in the right lower lung field. Which of the following is the most likely diagnosis?
- A. Aspiration pneumonia
- B. Pulmonary embolism
- C. Lung cancer
- D. Bronchiectasis (Correct Answer)
- E. Emphysema
Bronchiectasis Explanation: ***Bronchiectasis***
- The patient's history of **chronic productive cough**, **hemoptysis** (blood-tinged sputum), **digital clubbing**, and recent respiratory infection suggests bronchiectasis. The chest X-ray finding of **tram-track opacities** is highly characteristic of this condition, indicating bronchial wall thickening and dilation. The history of stroke placing him at risk for aspiration, and prior smoking also contribute to the risk of chronic lung damage.
- **Bronchiectasis** is defined by **permanent dilation of the bronchi** due to chronic inflammation and infection, leading to impaired mucociliary clearance and recurrent infections. The description perfectly fits the clinical and radiological picture.
*Aspiration pneumonia*
- While the patient's history of **stroke** increases his risk for **aspiration**, the chronic nature of his symptoms (long-standing productive cough worsening since stroke) and the presence of **digital clubbing** are less consistent with acute aspiration pneumonia.
- **Aspiration pneumonia** typically presents as an acute illness with fever and cough, and while it could explain some symptoms, it doesn't fully account for the chronic changes (clubbing, tram-track opacities).
*Pulmonary embolism*
- **Pulmonary embolism** usually presents with **acute onset dyspnea** and **pleuritic chest pain**, often without a history of chronic productive cough or digital clubbing. Hemoptysis can occur but is not typically copious and is associated with infarction.
- The chest X-ray findings of **increased translucency** and **tram-track opacities** are not characteristic of pulmonary embolism, which might show an area of opacification (Westermark sign, Hampton hump) or be normal.
*Lung cancer*
- While **lung cancer** can cause cough, hemoptysis, and shortness of breath, and the patient's smoking history is a risk factor, the description of **tram-track opacities** on chest X-ray is not characteristic of lung cancer. **Digital clubbing** can be seen, but the chronic productive cough for years is more indicative of a chronic inflammatory process.
- The typical X-ray findings for lung cancer would be a **mass lesion**, nodule, or atelectasis, not diffuse bronchial wall thickening.
*Emphysema*
- **Emphysema** is characterized by **shortness of breath** and a **chronic cough**, often related to a smoking history, and the X-ray might show **increased translucency** due to hyperinflation. However, copious **blood-tinged sputum** and **digital clubbing** are not typical features of emphysema.
- The classic X-ray finding for emphysema is **hyperinflation** with flattened diaphragms, and while increased translucency is mentioned, **tram-track opacities** are not seen; these indicate bronchial wall thickening, not alveolar destruction.
Bronchiectasis US Medical PG Question 9: A 47-year-old alcoholic man presents to the office for a 72-hour history of intense right hemithorax pain. He also complains of fever, chills, and sweating that started 10 days ago, as well as persistent coughing with abundant malodorous sputum. Chest radiography shows a round consolidation with air-fluid levels in the middle third of the right hemithorax. Sputum samples for a direct exam, culture, and acid-fast bacilli (AFB) are sent. What is the correct diagnosis?
- A. Bronchopulmonary sequestration
- B. Bronchiectasis
- C. Tuberculosis
- D. Lung cancer
- E. Lung abscess (Correct Answer)
Bronchiectasis Explanation: ***Lung abscess***
- The combination of **fever, chills, sweating, persistent coughing with malodorous sputum**, and a **round consolidation with air-fluid levels** on chest radiography in an alcoholic patient is highly indicative of a lung abscess.
- Alcoholism is a significant risk factor due to aspiration, leading to polymicrobial infections and subsequent tissue necrosis and cavitation.
*Bronchopulmonary sequestration*
- This is a rare congenital malformation where a portion of lung tissue is not connected to the tracheobronchial tree and receives its blood supply from the systemic circulation.
- It typically presents as a **mass lesion** on imaging, often without acute signs of infection like fever and malodorous sputum, unless it becomes secondarily infected.
*Bronchiectasis*
- Characterized by **irreversible dilation of the bronchi** resulting from chronic inflammation and infection, leading to chronic cough and sputum production.
- While it can cause chronic cough and sputum, the acute presentation with a distinct **round consolidation with air-fluid levels** points more specifically to an abscess.
*Tuberculosis*
- While tuberculosis can cause **fever, cough, and cavitary lesions** which might appear as air-fluid levels, the **malodorous sputum** is less typical, and the acute onset (72-hour intense pain after 10 days of symptoms) is more consistent with a pyogenic bacterial infection.
- Furthermore, a round consolidation with air-fluid levels without other classic features of TB (e.g., upper lobe predominance, Ghon complex) makes it less likely given the other findings.
*Lung cancer*
- Lung cancer can present as a **mass or consolidation** on imaging, and patients may experience cough, weight loss, and fatigue.
- However, the rapid onset of **fever, chills, malodorous sputum, and air-fluid levels** strongly suggests an infectious process with cavitation rather than an uncomplicated malignancy.
Bronchiectasis US Medical PG Question 10: A new drug is designed to treat asthma by inhibiting bronchoconstriction. Experimental assays show that treated animals had markedly reduced acetylcholine binding to muscarinic receptors relative to untreated controls. The drug is most similar to which of the following:
- A. Theophylline
- B. Cromolyn
- C. Zafirlukast
- D. Prednisone
- E. Ipratropium (Correct Answer)
Bronchiectasis Explanation: ***Ipratropium***
- This drug works as a **muscarinic acetylcholine receptor antagonist**, blocking the bronchoconstrictive effects of acetylcholine release in the airways.
- The experimental assay showing reduced **acetylcholine binding to muscarinic receptors** directly mimics the mechanism of action of ipratropium.
*Theophylline*
- Theophylline is a **phosphodiesterase inhibitor**, leading to increased cyclic AMP and bronchodilation, but it does not directly interfere with acetylcholine binding to muscarinic receptors.
- Its mechanism also involves adenosine receptor antagonism.
*Cromolyn*
- Cromolyn is a **mast cell stabilizer** that prevents the release of inflammatory mediators like histamine, thereby preventing bronchoconstriction.
- It does not act on muscarinic receptors.
*Zafirlukast*
- Zafirlukast is a **leukotriene receptor antagonist**, blocking the actions of leukotrienes which are potent bronchoconstrictors and pro-inflammatory mediators.
- Its mechanism is distinct from muscarinic receptor antagonism.
*Prednisone*
- Prednisone is a **corticosteroid** that reduces inflammation by inhibiting the synthesis of inflammatory mediators and altering gene expression.
- It does not directly affect acetylcholine binding at muscarinic receptors.
More Bronchiectasis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.