Asthma pathophysiology and diagnosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Asthma pathophysiology and diagnosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Asthma pathophysiology and diagnosis US Medical PG Question 1: A 21-year-old man presents with eye redness, itching, and watering; nasal congestion, and rhinorrhea. He reports that these symptoms have been occurring every year in the late spring since he was 18 years old. The patient’s medical history is significant for endoscopic resection of a right maxillary sinus polyp at the age of 16. His father and younger sister have bronchial asthma. He takes oxymetazoline as needed to decrease nasal congestion. The patient’s blood pressure is 120/80 mm Hg, heart rate is 71/min, respiratory rate is 18/min, and temperature is 36.7°C (98.0°F). On physical examination, there is conjunctival injection and clear nasal discharge bilaterally. His lymph nodes are not enlarged and his sinuses do not cause pain upon palpation. Heart and lung sounds are normal. Which of the following is most likely to be a part of his condition’s pathogenesis?
- A. Secretion of granzymes and perforin by cytotoxic T lymphocytes
- B. Excessive release of histamine by the mast cells (Correct Answer)
- C. Production of specific IgM antibodies by B lymphocytes
- D. Release of reactive oxygen species by neutrophils
- E. IL-2 secretion by Th1 lymphocytes
Asthma pathophysiology and diagnosis Explanation: ***Excessive release of histamine by the mast cells***
- This patient presents with symptoms highly suggestive of **allergic rhinitis** and **allergic conjunctivitis**, including seasonal conjunctival injection, itching, watering, nasal congestion, and rhinorrhea, which started in late spring. This is a classic presentation of a **Type I hypersensitivity reaction**, mediated by IgE antibodies primarily acting on **mast cells**.
- Upon re-exposure to the allergen (e.g., pollen in late spring), IgE antibodies cross-link on the surface of **mast cells**, leading to their **degranulation** and the release of preformed mediators, most notably **histamine**. Histamine causes the increased vascular permeability, vasodilation, itching, and mucous secretion characteristic of these allergic conditions.
*Secretion of granzymes and perforin by cytotoxic T lymphocytes*
- The secretion of granzymes and perforin by **cytotoxic T lymphocytes (CTLs)** is characteristic of **Type IV hypersensitivity reactions** (cell-mediated immunity) or direct viral killing, where CTLs target and destroy infected or abnormal cells.
- This mechanism is not directly involved in the acute allergic symptoms described, which are humorally mediated by IgE and mast cells.
*Production of specific IgM antibodies by B lymphocytes*
- While B lymphocytes produce antibodies, the primary antibody class involved in **Type I hypersensitivity** (allergic reactions) is **IgE**, not IgM.
- IgM antibodies are typically involved in the primary immune response and activate the complement system, which is characteristic of **Type II** and **Type III hypersensitivity reactions**, not allergic rhinitis.
*Release of reactive oxygen species by neutrophils*
- The release of **reactive oxygen species (ROS)** by **neutrophils** is a key mechanism of innate immunity, primarily involved in combating bacterial and fungal infections through phagocytosis and oxidative burst.
- This process is associated with inflammation and tissue damage in various conditions but is not the primary pathway for the acute allergic symptoms seen in this patient.
*IL-2 secretion by Th1 lymphocytes*
- **IL-2** secretion by **Th1 lymphocytes** is crucial for the proliferation and differentiation of T cells and is central to cell-mediated immune responses, including **Type IV hypersensitivity reactions**.
- **Allergic reactions (Type I hypersensitivity)** are predominantly driven by **Th2 lymphocytes** which secrete cytokines like IL-4, IL-5, and IL-13, promoting IgE production and eosinophil activation, not Th1-mediated responses.
Asthma pathophysiology and diagnosis US Medical PG Question 2: A 60-year-old woman presents to the emergency department due to progressive shortness of breath and a dry cough for the past week. She notes that her symptoms are exacerbated by physical activity and relieved by rest. The woman was diagnosed with chronic kidney disease 2 years ago and was recently started on regular dialysis treatment. Her pulse rate is 105/min, blood pressure is 110/70 mm Hg, respiratory rate is 30/min, and temperature is 37.8°C (100.0°F). On examination of the respiratory system, there is dullness on percussion, decreased vocal tactile fremitus, and decreased breath sounds over the right lung base. The rest of the physical exam is within normal limits. Which of the following is the most likely cause of this patient’s symptoms?
- A. Primary spontaneous pneumothorax (PSP)
- B. Pleural effusion (Correct Answer)
- C. Acute bronchitis
- D. Pneumonia
- E. Pulmonary tuberculosis (TB)
Asthma pathophysiology and diagnosis Explanation: ***Pleural effusion***
- The patient's symptoms of **progressive shortness of breath**, **dry cough**, and physical exam findings of **dullness to percussion**, **decreased vocal tactile fremitus**, and **decreased breath sounds** over the right lung base are classic signs of a **pleural effusion**.
- Given her history of **chronic kidney disease** and recent initiation of **dialysis**, she is at high risk for fluid overload, which can lead to **transudative pleural effusions** due to **increased hydrostatic pressure**.
*Primary spontaneous pneumothorax (PSP)*
- PSP typically presents with **sudden onset of pleuritic chest pain** and **shortness of breath**, not a progressive onset over a week.
- Physical exam findings for pneumothorax include **hyperresonance to percussion** and **absent or diminished breath sounds**, but **vocal tactile fremitus would be decreased or absent**, which is similar to pleural effusion. However, the patient's presentation of gradual onset and risk factors for fluid overload point away from a PSP.
*Acute bronchitis*
- Acute bronchitis usually presents with a **productive cough**, and symptoms are often preceded by an **upper respiratory tract infection**.
- Physical exam findings typically include **wheezing** or **rhonchi**, with normal percussion and fremitus, differing from the described findings.
*Pneumonia*
- Pneumonia would typically present with a **productive cough**, **fever**, and signs of consolidation on lung exam, such as **bronchial breath sounds** and **increased vocal fremitus**, along with dullness to percussion.
- While dullness and decreased breath sounds can be present, the **decreased vocal tactile fremitus** observed here strongly suggests fluid in the pleural space rather than consolidation.
*Pulmonary tuberculosis (TB)*
- Pulmonary TB often presents with **chronic cough (often productive)**, **night sweats**, **weight loss**, and **low-grade fever**, which are not the primary symptoms described.
- While CXR findings can vary, the acute presentation with clear signs of fluid accumulation in a patient with kidney disease makes TB less likely without other predisposing factors or prolonged symptomatology.
Asthma pathophysiology and diagnosis US Medical PG Question 3: A 28-year-old man makes an appointment with his general practitioner for a regular check-up. He has recently been diagnosed with asthma and was given a short-acting β2-agonist to use during acute exacerbations. He said he usually uses the medication 1–2 times per week. Which of the following is the most appropriate treatment in this case?
- A. He should start using a short-acting β2-agonist every day, not just when he has symptoms.
- B. Long-acting β2-agonists should be added to his treatment regimen.
- C. Inhaled corticosteroids should be added as controller therapy. (Correct Answer)
- D. Systemic corticosteroids should be added to his treatment regimen.
- E. He should continue with current treatment.
Asthma pathophysiology and diagnosis Explanation: ***Inhaled corticosteroids should be added as controller therapy.***
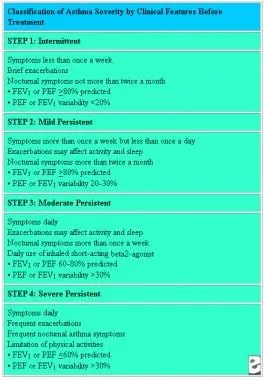
- The patient's use of a **short-acting β2-agonist (SABA)** 1-2 times per week indicates **persistent asthma** that is not well-controlled, suggesting the need for daily controller therapy.
- **Inhaled corticosteroids (ICS)** are the most effective anti-inflammatory controller medication for asthma and are recommended as the first-line add-on therapy when SABA use exceeds twice a week.
*He should start using a short-acting β2-agonist every day, not just when he has symptoms.*
- **SABAs** are **rescue medications** for acute symptom relief and do not address the underlying airway inflammation in asthma.
- Daily SABA use indicates **poor asthma control** and can lead to adverse effects like **tachycardia** and **tremors**, and may even mask worsening disease.
*Long-acting β2-agonists should be added to his treatment regimen.*
- **Long-acting β2-agonists (LABAs)** should typically **not be used as monotherapy** in asthma due to a potential risk of severe exacerbations and asthma-related deaths.
- LABAs are generally added to an **ICS regimen** when asthma remains uncontrolled despite adequate ICS therapy.
*Systemic corticosteroids should be added to his treatment regimen.*
- **Systemic corticosteroids** are reserved for **severe asthma exacerbations** or for patients with very severe persistent asthma unresponsive to other treatments, given their significant side effects with long-term use.
- The patient's current symptoms do not warrant the immediate use of systemic corticosteroids, which carry risks such as **osteoporosis**, **diabetes**, and **hypertension**.
*He should continue with current treatment.*
- Continuing with SABA monotherapy when used 1-2 times per week indicates **persistent asthma**, which is **suboptimally controlled**.
- Current guidelines suggest that SABA use more than twice weekly warrants a step-up in therapy to include daily controller medication like **inhaled corticosteroids**.
Asthma pathophysiology and diagnosis US Medical PG Question 4: A 28-year-old man presents to his primary care provider because of shortness of breath, cough, and wheezing. He reports that in high school, he occasionally had shortness of breath and would wheeze after running. His symptoms have progressively worsened over the past 6 months and are now occurring daily. He also finds himself being woken up from sleep by his wheeze approximately 3 times a week. His medical history is unremarkable. He denies tobacco use or excessive alcohol consumption. His temperature is 37.1°C (98.8°F), blood pressure is 121/82 mm Hg, and heart rate is 82/min. Physical examination is remarkable for expiratory wheezing bilaterally. Spirometry shows an FEV1 of 73% of predicted, which improves by 19% with albuterol. In addition to a short-acting beta-agonist as needed, which of the following is the most appropriate therapy for this patient?
- A. A high-dose inhaled corticosteroid and a long-acting beta-agonist
- B. A long-acting beta-agonist alone
- C. A low-dose inhaled corticosteroid alone
- D. A medium-dose inhaled corticosteroid and a long-acting beta-agonist
- E. A low-dose inhaled corticosteroid and a long-acting beta-agonist (Correct Answer)
Asthma pathophysiology and diagnosis Explanation: ***A low-dose inhaled corticosteroid and a long-acting beta-agonist***
- This patient presents with **persistent asthma symptoms** (daily symptoms, nighttime awakenings 3x/week, and a significant bronchodilator response) that are not controlled by a short-acting beta-agonist alone. This indicates **moderate persistent asthma**.
- According to GINA guidelines, the appropriate step-up therapy for moderate persistent asthma is a **low-dose inhaled corticosteroid (ICS) combined with a long-acting beta-agonist (LABA)**.
*A high-dose inhaled corticosteroid and a long-acting beta-agonist*
- **High-dose ICS/LABA** is reserved for **severe uncontrolled asthma**, typically as Step 4 or 5 therapy, when symptoms persist despite lower-dose combinations or higher-step single agents.
- The patient's current symptoms, while persistent, do not warrant immediate initiation of high-dose therapy as initial step-up from mild persistent.
*A long-acting beta-agonist alone*
- **LABAs should never be used as monotherapy** in asthma due to the risk of severe asthma exacerbations and asthma-related death.
- They must always be combined with an **inhaled corticosteroid** to control underlying airway inflammation.
*A low-dose inhaled corticosteroid alone*
- While a **low-dose ICS alone** is appropriate for **mild persistent asthma** (Step 2), this patient's symptoms (daily symptoms, nighttime awakenings 3x/week) are more severe than mild persistent.
- His severity warrants combination therapy (ICS/LABA) to achieve better symptom control.
*A medium-dose inhaled corticosteroid and a long-acting beta-agonist*
- A **medium-dose ICS/LABA** is typically considered for patients whose asthma remains **uncontrolled on low-dose ICS/LABA**, representing Step 4 therapy.
- Given that this is the initial step-up from SABA-only use, medium-dose is generally too aggressive and should be reserved for subsequent steps if the low-dose combination proves insufficient.
Asthma pathophysiology and diagnosis US Medical PG Question 5: A 24-year-old woman presents with episodic shortness of breath, chest tightness, and wheezing. She has noticed an increased frequency of such episodes in the spring season. She also has a history of urticaria. She has smoked a half pack of cigarettes per day over the last 5 years. Her mother also has similar symptoms. The physical exam is within normal limits. Which of the following findings is characteristic of her condition?
- A. Increased oxygen saturation
- B. Decrease in forced expiratory volume in 1 second (FEV1) after methacholine (Correct Answer)
- C. Decreased forced vital capacity (FVC) on pulmonary tests
- D. Paroxysmal nocturnal dyspnea
- E. Chest X-ray showing hyperinflation
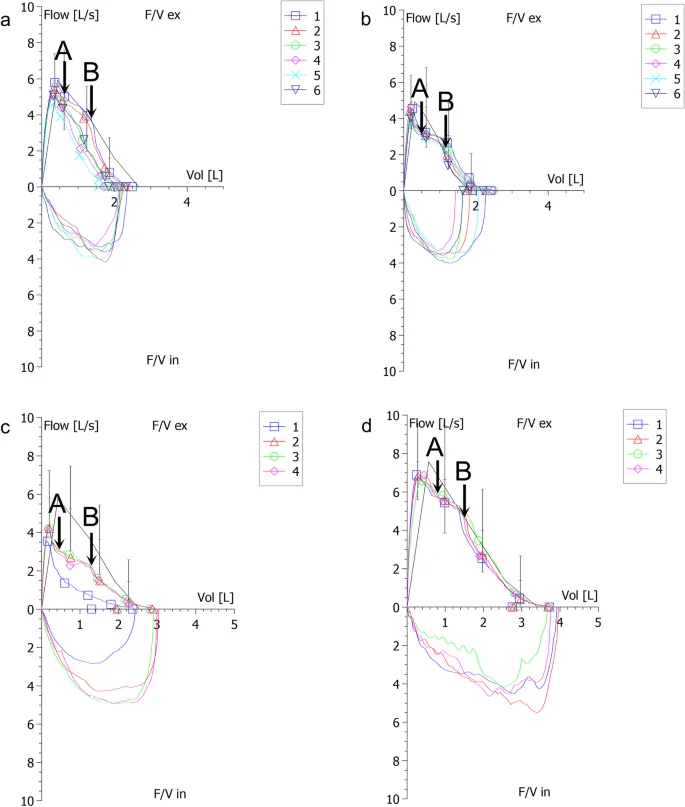
Asthma pathophysiology and diagnosis Explanation: ***Decrease in forced expiratory volume in 1 second (FEV1) after methacholine***
- The patient's symptoms of **episodic shortness of breath, chest tightness, and wheezing**, especially with seasonal variability and a history of **urticaria** and maternal history of similar symptoms, are highly suggestive of **asthma**.
- A significant **decrease in FEV1 after methacholine challenge** is a hallmark of bronchial hyperresponsiveness, which is diagnostic for asthma.
*Increased oxygen saturation*
- While a patient with asthma might have normal oxygen saturation during an asymptomatic period, during an **acute asthma exacerbation**, oxygen saturation would likely be decreased, not increased.
- Increased oxygen saturation is not a characteristic finding and does not help diagnose asthma.
*Decreased forced vital capacity (FVC) on pulmonary tests*
- Although **FVC can be reduced in severe asthma** due to air trapping, it is not the primary or most characteristic pulmonary function test finding.
- The hallmark of asthma is **airflow obstruction**, specifically a reduced FEV1/FVC ratio and reduced FEV1, which is reversible.
*Paroxysmal nocturnal dyspnea*
- **Paroxysmal nocturnal dyspnea (PND)** is typically associated with **heart failure**, where fluid accumulation in the lungs worsens when lying flat, causing shortness of breath that awakens the patient from sleep.
- While some asthmatics may experience nocturnal symptoms, PND is not a defining characteristic of asthma.
*Chest X-ray showing hyperinflation*
- A **chest X-ray is typically normal in asthma** unless there is an exacerbation or complications like pneumonia or pneumothorax.
- **Hyperinflation** can be seen in severe, prolonged asthma or during an acute attack due to air trapping, but it is not a *characteristic diagnostic feature* during asymptomatic periods or generally for diagnosis.
Asthma pathophysiology and diagnosis US Medical PG Question 6: A previously healthy 64-year-old woman comes to the physician because of a dry cough and progressively worsening shortness of breath for the past 2 months. She has not had fever, chills, or night sweats. She has smoked one pack of cigarettes daily for the past 45 years. She appears thin. Examination of the lung shows a prolonged expiratory phase and end-expiratory wheezing. Spirometry shows decreased FEV1:FVC ratio (< 70% predicted), decreased FEV1, and a total lung capacity of 125% of predicted. The diffusion capacity of the lung (DLCO) is decreased. Which of the following is the most likely diagnosis?
- A. Bronchiectasis
- B. Interstitial lung disease
- C. Chronic obstructive pulmonary disease (Correct Answer)
- D. Hypersensitivity pneumonitis
- E. Bronchial asthma
Asthma pathophysiology and diagnosis Explanation: ***Chronic obstructive pulmonary disease***
- The patient's long history of **smoking (45 pack-years)**, **prolonged expiratory phase**, and **end-expiratory wheezing** are classic signs of airway obstruction.
- Spirometry findings of a **decreased FEV1:FVC ratio** (< 70% predicted), **decreased FEV1**, **increased total lung capacity (TLC)**, and **decreased DLCO** are all highly indicative of **emphysema**, a subtype of COPD.
*Bronchiectasis*
- While it shares symptoms like cough and SOB, **bronchiectasis** is characterized by permanent **dilatation of bronchi** and profuse, chronic **sputum production**, which is not mentioned here.
- Spirometry typically shows **obstructive patterns**, but the marked increase in TLC and decreased DLCO are more specific to emphysema.
*Interstitial lung disease*
- This condition primarily causes a **restrictive lung pattern**, meaning a decreased TLC and normal or increased FEV1:FVC ratio.
- The patient's **increased TLC** and **obstructive spirometry** rule out a purely restrictive process.
*Hypersensitivity pneumonitis*
- This is an inflammatory response to inhaled antigens, often presenting with **recurrent episodes** of fever, chills, and cough, and can lead to restrictive physiology.
- The patient lacks a history of specific **antigen exposure** and presents with an obstructive pattern and increased TLC.
*Bronchial asthma*
- While asthma shares obstructive features like wheezing and a decreased FEV1:FVC ratio, it is characterized by **reversibility** of airway obstruction and typically does not cause a significantly **elevated TLC** or **decreased DLCO** in uncomplicated cases.
- The patient's long smoking history points away from asthma as the primary diagnosis.
Asthma pathophysiology and diagnosis US Medical PG Question 7: A 16-year-old boy with a history of severe, persistent asthma presents to the emergency department with severe shortness of breath and cough. He states that he was outside playing basketball with his friends, forgot to take his inhaler, and began to have severe difficulty breathing. On exam, he is in clear respiratory distress with decreased air movement throughout all lung fields. He is immediately treated with beta-agonists which markedly improve his symptoms. Prior to treatment, which of the following was most likely observed in this patient?
- A. Kussmaul's sign
- B. Pulsus paradoxus (Correct Answer)
- C. Friction rub
- D. Inspiratory stridor
- E. Increased breath sounds
Asthma pathophysiology and diagnosis Explanation: ***Pulsus paradoxus***
* **Pulsus paradoxus** is a classic sign of **severe asthma exacerbation**, characterized by an abnormally large decrease in **systolic blood pressure** during inspiration.
* The marked improvement with **beta-agonists** confirms the likely diagnosis of acute severe asthma, making pulsus paradoxus a highly probable finding before treatment.
*Kussmaul's sign*
* **Kussmaul's sign** is a paradoxical rise in **jugular venous pressure (JVP)** during inspiration, typically seen in conditions like **constrictive pericarditis** or **right heart failure**.
* It is not associated with acute asthma exacerbations.
*Friction rub*
* A **friction rub** is a leathery or grating sound heard on auscultation, indicative of inflammation of the **pleura** (pleurisy) or **pericardium** (pericarditis).
* It is not a typical finding in asthma and would suggest an alternative or co-existing pathology.
*Inspiratory stridor*
* **Inspiratory stridor** is a harsh, high-pitched sound primarily heard during inspiration, caused by **upper airway obstruction** (e.g., croup, epiglottitis, foreign body aspiration).
* While severe shortness of breath is present, the symptom relief with beta-agonists points to **lower airway obstruction** characteristic of asthma rather than upper airway issues.
*Increased breath sounds*
* In **severe asthma exacerbations**, there is significant **bronchoconstriction** and **air trapping**, leading to markedly **decreased or absent breath sounds** on auscultation, not increased.
* Increased breath sounds might be heard in consolidation (pneumonia) or early stages of bronchiole inflammation, but not in severe asthma distress.
Asthma pathophysiology and diagnosis US Medical PG Question 8: A 28-year-old man comes to his general practitioner for a regular checkup. He has had trouble breathing lately with coughing, shortness of breath, and wheezing. Problems first started when he went running (outside), but he is also observing the problems when taking a light walk or resting. As a child, he suffered from atopic dermatitis, just like his father and sister. He also has a history of hay fever. What is the most likely cause of his symptoms?
- A. Smoking
- B. Chronic obstructive pulmonary disease
- C. Type I hypersensitivity (Correct Answer)
- D. Type IV hypersensitivity
- E. Exercise
Asthma pathophysiology and diagnosis Explanation: ***Type I hypersensitivity***
- The patient's presentation with **coughing, shortness of breath, and wheezing** suggests **bronchial asthma**, which is a classic manifestation of **Type I hypersensitivity** (allergic reaction).
- The history of **atopic dermatitis** (eczema) and **hay fever** indicates an **atopic diathesis**, which is a strong predisposing factor for allergic asthma. This forms the **atopic triad**.
*Smoking*
- While smoking can cause respiratory symptoms like coughing and shortness of breath, it typically does not cause acute wheezing that improves with rest in a young, otherwise healthy individual.
- The patient's personal history of atopic dermatitis and hay fever, and running in the family does not suggest smoking.
*Chronic obstructive pulmonary disease*
- **COPD** usually develops in older individuals, often with a history of significant smoking or environmental exposure, and is characterized by **progressive, non-reversible airflow limitation**.
- The patient's young age and history of atopic conditions make COPD a less likely diagnosis compared to asthma.
*Type IV hypersensitivity*
- **Type IV hypersensitivity**, or **delayed-type hypersensitivity**, typically manifests as contact dermatitis (e.g., poison ivy) or granulomatous reactions, which are T-cell mediated and develop over 24-72 hours.
- It does not cause acute respiratory symptoms like wheezing, nor is it linked to atopic conditions such as hay fever and asthma.
*Exercise*
- Exercise can trigger **exercise-induced bronchoconstriction (asthma)**, which presents as shortness of breath and wheezing during or after physical activity.
- However, the patient also experiences symptoms during light walks or at rest, and has a strong atopic history, indicating that exercise is a trigger for underlying asthma (Type I hypersensitivity) rather than the sole cause of symptoms.
Asthma pathophysiology and diagnosis US Medical PG Question 9: A 14-year-old boy presents to an urgent care clinic complaining of a runny nose that has lasted for a few weeks. He also reports sneezing attacks that last up to an hour, nasal obstruction, and generalized itching. He has similar episodes each year during the springtime that prevent him from going out with his friends or trying out for sports. His younger brother has a history of asthma. Which of the following diseases has a similar pathophysiology?
- A. Irritant contact dermatitis
- B. Dermatitis herpetiformis
- C. Allergic contact dermatitis
- D. Atopic dermatitis (Correct Answer)
- E. Systemic lupus erythematosus
Asthma pathophysiology and diagnosis Explanation: ***Atopic dermatitis***
- This patient's symptoms are highly suggestive of **allergic rhinitis**, a **type I hypersensitivity reaction** mediated by IgE antibodies, which also underlies atopic dermatitis.
- The family history of asthma (part of the **atopic triad** – allergic rhinitis, asthma, atopic dermatitis) further supports a common underlying allergic predisposition.
*Irritant contact dermatitis*
- This is a **non-allergic inflammatory reaction** caused by direct skin irritation from chemical or physical agents, not an immunological hypersensitivity.
- It does not involve IgE-mediated mechanisms or a systemic allergic predisposition like the patient's condition.
*Dermatitis herpetiformis*
- This is a **chronic blistering skin condition** strongly associated with **celiac disease** and characterized by IgA deposition in the skin.
- It involves an autoimmune response to gluten and is not related to the IgE-mediated allergic response seen in allergic rhinitis.
*Allergic contact dermatitis*
- This is a **type IV delayed-type hypersensitivity reaction** mediated by T cells, often occurring days after exposure to an allergen (e.g., poison ivy, nickel).
- It is distinct from the immediate IgE-mediated (type I) hypersensitivity responsible for allergic rhinitis.
*Systemic lupus erythematosus*
- This is a **chronic autoimmune disease** characterized by systemic inflammation and autoantibody production against various self-antigens, leading to diverse organ involvement.
- It is a complex autoimmune disorder with different immunological mechanisms (e.g., type III hypersensitivity) rather than the IgE-mediated allergy seen in this case.
Asthma pathophysiology and diagnosis US Medical PG Question 10: A high-throughput screen to identify new sympathomimetic compounds was developed such that a transgenic line of cells was created that contained the alpha-1 (red), alpha-2 (yellow), beta-1 (green) and beta-2 (blue) receptors. When each of the receptors was activated a different fluorescent protein was expressed and new compounds with different properties could be identified by the fluorescence that they induced. Compound 7583 selectively induced the expression of the blue fluorescent protein. Which of the following known sympathomimetic medications if administered would similarly result in expression of only the blue fluorescent protein?
- A. Albuterol (Correct Answer)
- B. Fenoldopam
- C. Epinephrine
- D. Isoproterenol
- E. Midodrine
Asthma pathophysiology and diagnosis Explanation: ***Albuterol***
- The blue fluorescent protein is expressed upon activation of the **beta-2 receptor**. Albuterol is a **selective beta-2 adrenergic agonist**.
- Its primary clinical use is as a **bronchodilator** in asthma and COPD, acting by relaxing bronchial smooth muscle via beta-2 receptor activation.
*Fenoldopam*
- Fenoldopam is a **D1 dopamine receptor agonist** used as a rapid-acting vasodilator.
- It has **no significant direct activity** at adrenergic alpha or beta receptors.
*Epinephrine*
- Epinephrine is a **non-selective adrenergic agonist** that activates alpha-1, alpha-2, beta-1, and beta-2 receptors.
- It would induce the expression of **all four fluorescent proteins** (red, yellow, green, and blue).
*Isoproterenol*
- Isoproterenol is a **non-selective beta-adrenergic agonist**, activating both beta-1 and beta-2 receptors.
- It would induce the expression of **green and blue fluorescent proteins**, but not exclusively blue.
*Midodrine*
- Midodrine is a **selective alpha-1 adrenergic agonist** and would induce the expression of the **red fluorescent protein**.
- It is primarily used to treat **orthostatic hypotension** by causing vasoconstriction.
More Asthma pathophysiology and diagnosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.