Asthma management and exacerbations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Asthma management and exacerbations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Asthma management and exacerbations US Medical PG Question 1: A 21-year-old woman comes to the physician for the evaluation of dry cough and some chest tightness for the past several weeks. The cough is worse at night and while playing volleyball. She frequently has a runny nose and nasal congestion. Her mother has systemic lupus erythematosus. The patient has smoked one pack of cigarettes daily for the last 5 years. She does not drink alcohol. Her only medication is cetirizine. Her vital signs are within normal limits. Pulse oximetry on room air shows an oxygen saturation of 98%. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Spirometry (Correct Answer)
- C. Laboratory studies
- D. Methacholine challenge test
- E. Blood gas analysis
Asthma management and exacerbations Explanation: ***Spirometry***
- The patient's symptoms (dry cough, chest tightness, worse at night and with activity) are highly suggestive of **asthma**.
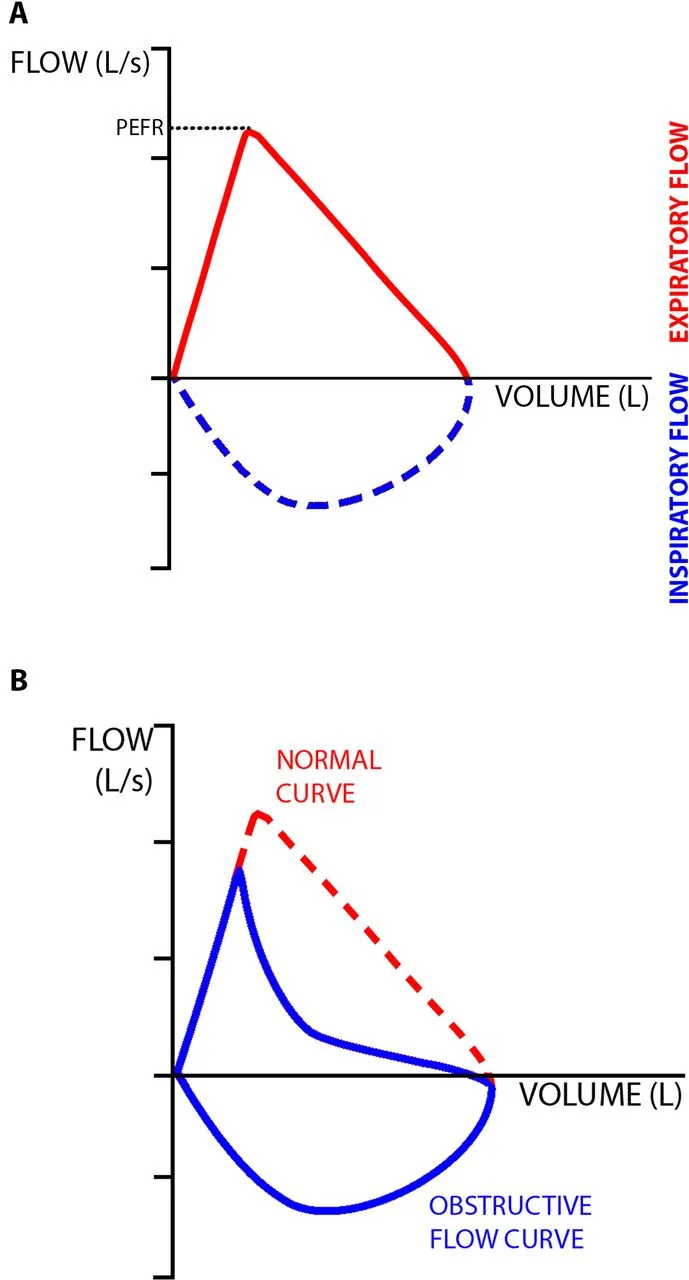
- **Spirometry** is the initial recommended diagnostic test to assess for reversible airway obstruction, which is characteristic of asthma.
*CT scan of the chest*
- A CT scan of the chest is generally reserved for evaluating structural lung diseases, persistent or atypical symptoms, or when other diagnoses (e.g., malignancy, interstitial lung disease) are suspected.
- Given the classic asthma-like symptoms, a **less invasive and more direct physiological test** is indicated first.
*Laboratory studies*
- Routine laboratory studies are typically **not helpful** in the initial diagnosis of asthma.
- While allergy testing or inflammatory markers might be considered later, they do not directly assess airway function to confirm asthma.
*Methacholine challenge test*
- A **methacholine challenge test** is used to diagnose **asthma** when spirometry results are normal but asthma is still strongly suspected.
- It is often considered if initial spirometry with bronchodilator reversal is inconclusive, rather than as a first-line diagnostic step.
*Blood gas analysis*
- Blood gas analysis measures oxygen and carbon dioxide levels in the blood and is used to assess the severity of respiratory failure or acid-base status.
- It is **not a primary diagnostic tool for asthma**, especially in a patient with normal vital signs and pulse oximetry.
Asthma management and exacerbations US Medical PG Question 2: A 13-year-old boy with a history of asthma and seasonal allergies is currently using albuterol to manage his asthma symptoms. Recently, his use of albuterol increased from 1–2 days/week to 4 times/week over the past several weeks, though he does not experience his symptoms daily. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. His physical examination shows clear, bilateral breath sounds and normal heart sounds. What change should be made to his current treatment regimen?
- A. Add tiotropium
- B. Add formoterol + budesonide twice daily
- C. Add montelukast 5 mg daily
- D. Add fluticasone daily (Correct Answer)
- E. Add salmeterol twice daily
Asthma management and exacerbations Explanation: ***Add fluticasone daily***
- This patient currently has **mild persistent asthma** based on his increased albuterol use (4 times/week, but not daily). The guideline-recommended step-up for mild persistent asthma is the daily addition of a **low-dose inhaled corticosteroid (ICS)** like fluticasone.
- Adding fluticasone daily addresses the underlying inflammation of asthma, reducing symptoms and the need for frequent albuterol rescue inhaler use.
*Add tiotropium*
- Tiotropium, a **long-acting muscarinic antagonist (LAMA)**, is primarily used for asthma as an add-on therapy for patients whose symptoms are not well-controlled with ICS and long-acting beta-2 agonists (LABAs).
- It is not a first-line agent for initiating controller therapy in mild persistent asthma.
*Add formoterol + budesonide twice daily*
- This combination, a **LABA/ICS**, is indicated for moderate to severe persistent asthma, not mild persistent asthma, or can be used as a reliever in older children/adults with mild asthma (SMART therapy).
- Prescribing it twice daily would be an over-treatment for this patient's current asthma severity.
*Add montelukast 5 mg daily*
- Montelukast, a **leukotriene receptor antagonist**, is an alternative for mild persistent asthma, but **ICS are generally preferred** due to superior efficacy in controlling inflammation.
- While it could be considered, fluticasone (an ICS) is a more effective first-line option for controller therapy in mild persistent asthma.
*Add salmeterol twice daily*
- Salmeterol is a **long-acting beta-2 agonist (LABA)** that should never be used as monotherapy in asthma due to the risk of severe exacerbations and asthma-related death.
- LABAs should always be used in combination with an **inhaled corticosteroid (ICS)**.
Asthma management and exacerbations US Medical PG Question 3: A 28-year-old man makes an appointment with his general practitioner for a regular check-up. He has recently been diagnosed with asthma and was given a short-acting β2-agonist to use during acute exacerbations. He said he usually uses the medication 1–2 times per week. Which of the following is the most appropriate treatment in this case?
- A. He should start using a short-acting β2-agonist every day, not just when he has symptoms.
- B. Long-acting β2-agonists should be added to his treatment regimen.
- C. Inhaled corticosteroids should be added as controller therapy. (Correct Answer)
- D. Systemic corticosteroids should be added to his treatment regimen.
- E. He should continue with current treatment.
Asthma management and exacerbations Explanation: ***Inhaled corticosteroids should be added as controller therapy.***
- The patient's use of a **short-acting β2-agonist (SABA)** 1-2 times per week indicates **persistent asthma** that is not well-controlled, suggesting the need for daily controller therapy.
- **Inhaled corticosteroids (ICS)** are the most effective anti-inflammatory controller medication for asthma and are recommended as the first-line add-on therapy when SABA use exceeds twice a week.
*He should start using a short-acting β2-agonist every day, not just when he has symptoms.*
- **SABAs** are **rescue medications** for acute symptom relief and do not address the underlying airway inflammation in asthma.
- Daily SABA use indicates **poor asthma control** and can lead to adverse effects like **tachycardia** and **tremors**, and may even mask worsening disease.
*Long-acting β2-agonists should be added to his treatment regimen.*
- **Long-acting β2-agonists (LABAs)** should typically **not be used as monotherapy** in asthma due to a potential risk of severe exacerbations and asthma-related deaths.
- LABAs are generally added to an **ICS regimen** when asthma remains uncontrolled despite adequate ICS therapy.
*Systemic corticosteroids should be added to his treatment regimen.*
- **Systemic corticosteroids** are reserved for **severe asthma exacerbations** or for patients with very severe persistent asthma unresponsive to other treatments, given their significant side effects with long-term use.
- The patient's current symptoms do not warrant the immediate use of systemic corticosteroids, which carry risks such as **osteoporosis**, **diabetes**, and **hypertension**.
*He should continue with current treatment.*
- Continuing with SABA monotherapy when used 1-2 times per week indicates **persistent asthma**, which is **suboptimally controlled**.
- Current guidelines suggest that SABA use more than twice weekly warrants a step-up in therapy to include daily controller medication like **inhaled corticosteroids**.
Asthma management and exacerbations US Medical PG Question 4: A cohort study was conducted to investigate the impact of post-traumatic stress disorder (PTSD) on asthma symptoms in a group of firefighters who worked at Ground Zero during the September 11, 2001 terrorist attacks in New York City and developed asthma in the attack's aftermath. The study compared patients who had PTSD with those who did not have PTSD in order to determine if PTSD is associated with worse asthma control. During a follow-up period of 12 months, the researchers found that patients with PTSD had a greater number of hospitalizations for asthma exacerbations (RR = 2.0, 95% confidence interval = 1.4–2.5) after adjusting for medical comorbidities, psychiatric comorbidities other than PTSD, and sociodemographic variables. Results are shown:
≥ 1 asthma exacerbation No asthma exacerbations
PTSD 80 80
No PTSD 50 150
Based on these results, what proportion of asthma hospitalizations in patients with PTSD could be attributed to PTSD?
- A. 0.25
- B. 4.0
- C. 0.50 (Correct Answer)
- D. 2.0
- E. 3.0
Asthma management and exacerbations Explanation: ***0.50***
- The **Attributable Risk Percent (AR%)** in the exposed group is calculated as (RR - 1) / RR. Given a Relative Risk (RR) of 2.0, AR% = (2.0 - 1) / 2.0 = 1 / 2.0 = 0.50.
- This means that **50% of asthma hospitalizations** in the group with PTSD can be attributed to their PTSD status.
*0.25*
- This value is obtained by dividing 1 by 4, not relevant to the formula for **attributable risk percent** using the given relative risk.
- Incorrectly applying the formula or misinterpreting the RR would lead to this value.
*4.0*
- This value is not derived from the **attributable risk percent formula** (AR% = (RR - 1) / RR) with the given RR of 2.0.
- It might represent a misunderstanding of risk ratios or how to calculate attributable risk.
*2.0*
- This is the **Relative Risk (RR)** itself, not the proportion of asthma hospitalizations attributable to PTSD.
- The RR compares the incidence of an outcome in the exposed group to the unexposed group.
*3.0*
- This value is not obtained through any standard epidemiological calculation for **attributable risk** given the relative risk of 2.0.
- It likely results from an arbitrary calculation or an incorrect application of epidemiological formulas.
Asthma management and exacerbations US Medical PG Question 5: A 23-year-old man presents to his physician's office with increasing breathlessness over the past one month. He was diagnosed with asthma when he was a child and has been able to keep his symptoms under control with a Ventolin inhaler. However, over the past year or so he has found that he gets out of breath on several occasions during the week. He wakes up at least once a week with breathlessness. He finds that he feels out of breath during his weekly football matches, which never used to happen before. He has to sit down and take a couple of puffs of his inhaler to feel better. He has no other pertinent history at this moment, except that he started on a new job painting houses about 5 months ago. His physical examination does not show anything significant. His peak expiratory flow rate during spirometry averages about 85% of the normal value, after conducting the test 3 times. Which of the following would be the next best step in management?
- A. Patch test
- B. Follow up spirometry in 2 months
- C. Arterial blood gas
- D. Chest X-ray
- E. Methacholine bronchoprovocation test (Correct Answer)
Asthma management and exacerbations Explanation: ***Methacholine bronchoprovocation test***
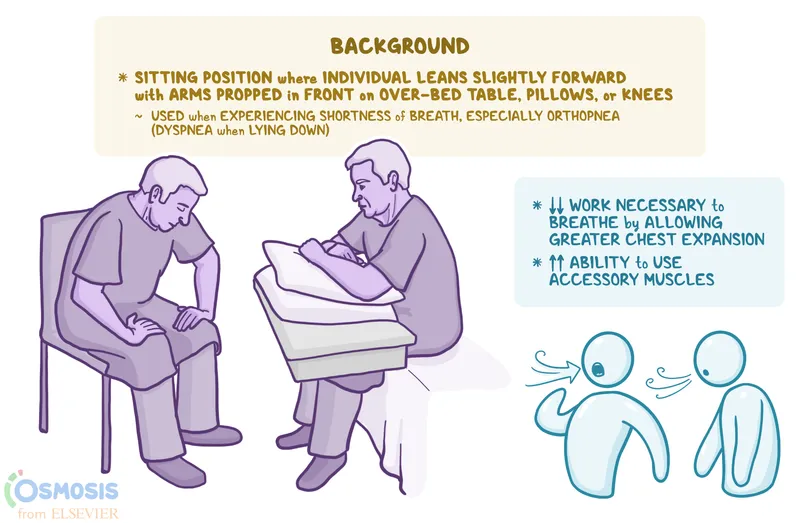
- The patient's history, including **worsening asthma symptoms** despite previous control and a new exposure to paint, suggests a potential diagnosis of **occupational asthma**. A methacholine challenge test is indicated to confirm **airway hyperresponsiveness** if spirometry is inconclusive.
- Given the history of frequent symptoms, night awakenings, and impact on activity, this points to **uncontrolled asthma** or a new trigger. A positive test to methacholine would confirm **bronchial hyperreactivity**, which is essential for diagnosing asthma when baseline spirometry is near normal.
*Patch test*
- A patch test is used to identify **contact allergens** that cause **allergic contact dermatitis**, which presents as a rash rather than respiratory symptoms.
- It is not indicated for the diagnosis of **occupational asthma**, which involves inhalation of triggers.
*Follow up spirometry in 2 months*
- Waiting two months for follow-up spirometry would delay diagnosis and potential treatment for a patient with **worsening and uncontrolled asthma symptoms**.
- The current spirometry reading of **85% of normal** is not significantly obstructive enough to definitively diagnose asthma without further testing, especially given the history.
*Arterial blood gas*
- An ABG measures **blood gas levels** and acid-base balance, which is useful in assessing the severity of an acute asthma exacerbation or chronic respiratory failure.
- In a patient with partially controlled asthma and near-normal spirometry, an ABG is not typically the next best diagnostic step unless there are signs of severe respiratory distress or hypoxemia.
*Chest X-ray*
- A chest X-ray is primarily used to rule out other respiratory conditions like **pneumonia**, **pneumothorax**, or structural lung disease, which are not suggested by this patient's history.
- It's generally not indicated as a primary diagnostic tool for **asthma**, especially when symptoms are chronic and related to bronchoconstriction.
Asthma management and exacerbations US Medical PG Question 6: A 24-year-old woman presents with episodic shortness of breath, chest tightness, and wheezing. She has noticed an increased frequency of such episodes in the spring season. She also has a history of urticaria. She has smoked a half pack of cigarettes per day over the last 5 years. Her mother also has similar symptoms. The physical exam is within normal limits. Which of the following findings is characteristic of her condition?
- A. Increased oxygen saturation
- B. Decrease in forced expiratory volume in 1 second (FEV1) after methacholine (Correct Answer)
- C. Decreased forced vital capacity (FVC) on pulmonary tests
- D. Paroxysmal nocturnal dyspnea
- E. Chest X-ray showing hyperinflation
Asthma management and exacerbations Explanation: ***Decrease in forced expiratory volume in 1 second (FEV1) after methacholine***
- The patient's symptoms of **episodic shortness of breath, chest tightness, and wheezing**, especially with seasonal variability and a history of **urticaria** and maternal history of similar symptoms, are highly suggestive of **asthma**.
- A significant **decrease in FEV1 after methacholine challenge** is a hallmark of bronchial hyperresponsiveness, which is diagnostic for asthma.
*Increased oxygen saturation*
- While a patient with asthma might have normal oxygen saturation during an asymptomatic period, during an **acute asthma exacerbation**, oxygen saturation would likely be decreased, not increased.
- Increased oxygen saturation is not a characteristic finding and does not help diagnose asthma.
*Decreased forced vital capacity (FVC) on pulmonary tests*
- Although **FVC can be reduced in severe asthma** due to air trapping, it is not the primary or most characteristic pulmonary function test finding.
- The hallmark of asthma is **airflow obstruction**, specifically a reduced FEV1/FVC ratio and reduced FEV1, which is reversible.
*Paroxysmal nocturnal dyspnea*
- **Paroxysmal nocturnal dyspnea (PND)** is typically associated with **heart failure**, where fluid accumulation in the lungs worsens when lying flat, causing shortness of breath that awakens the patient from sleep.
- While some asthmatics may experience nocturnal symptoms, PND is not a defining characteristic of asthma.
*Chest X-ray showing hyperinflation*
- A **chest X-ray is typically normal in asthma** unless there is an exacerbation or complications like pneumonia or pneumothorax.
- **Hyperinflation** can be seen in severe, prolonged asthma or during an acute attack due to air trapping, but it is not a *characteristic diagnostic feature* during asymptomatic periods or generally for diagnosis.
Asthma management and exacerbations US Medical PG Question 7: A 20-year-old man comes to the physician because of recurrent episodes of shortness of breath and a nonproductive cough for the past 4 months. He has two episodes per week, which resolve spontaneously with rest. Twice a month, he wakes up at night with shortness of breath. His pulse is 73/min, respirations are 13/min, and blood pressure is 122/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. Physical examination shows no abnormalities. Spirometry shows an FVC of 95%, an FEV1:FVC ratio of 0.85, and an FEV1 of 81% of predicted. Which of the following is the most appropriate initial pharmacotherapy?
- A. Terbutaline inhaler
- B. Mometasone inhaler and oral zafirlukast
- C. Oral montelukast sodium
- D. Fluticasone inhaler (Correct Answer)
- E. Budesonide and formoterol inhaler
Asthma management and exacerbations Explanation: **Fluticasone inhaler**
- The patient presents with symptoms consistent with **persistent asthma** (symptoms >2 times/week and nighttime awakenings >2 times/month).
- **Inhaled corticosteroids** like fluticasone are the preferred initial **controller therapy** for persistent asthma due to their potent **anti-inflammatory effects**.
*Terbutaline inhaler*
- Terbutaline is a **short-acting beta-agonist (SABA)**, primarily used as a **rescue medication** for acute asthma symptoms.
- While it would relieve acute symptoms, it does not address the underlying inflammation in persistent asthma and is not appropriate for **monotherapy** as initial pharmacotherapy in this context.
*Mometasone inhaler and oral zafirlukast*
- This combination includes an **inhaled corticosteroid (mometasone)** and a **leukotriene receptor antagonist (zafirlukast)**.
- While appropriate for more severe or uncontrolled asthma, starting with a **single inhaled corticosteroid** is the recommended initial step for **persistent asthma** before adding a second-line agent.
*Oral montelukast sodium*
- Montelukast is a **leukotriene receptor antagonist** used in asthma management, often as an **add-on therapy** or for patients who cannot tolerate inhaled corticosteroids.
- It is generally **less effective than inhaled corticosteroids** as initial monotherapy for persistent asthma in controlling inflammation and preventing exacerbations.
*Budesonide and formoterol inhaler*
- This is a combination of an **inhaled corticosteroid (budesonide)** and a **long-acting beta-agonist (formoterol)**.
- This combination is typically used for **moderate to severe persistent asthma** or as **maintenance and reliever therapy (MART)**, not as the initial monotherapy for mild persistent asthma.
Asthma management and exacerbations US Medical PG Question 8: A 60-year-old man presents to the emergency department complaining of worsening exertional dyspnea over the last week. He denies chest pain and lightheadedness but reports persistent cough with white sputum. His past medical history includes hypertension and diabetes mellitus. He has a 50 pack-year history of smoking but denies any illicit drug use or alcohol consumption. His temperature is 101°F (38.3°C), blood pressure is 154/104 mmHg, pulse is 110/min, respirations are 26/min, and oxygen saturation is 88% on a non-rebreather mask. Physical exam is notable for an obese man in distress. The anteroposterior diameter of the patient's chest is increased, and he has decreased breath sounds bilaterally with diffuse expiratory wheezing. Which of the following is the best next step in management?
- A. Muscarinic blocker
- B. Glucocorticoid-analog
- C. Alpha-2 blocker
- D. Beta-2 agonist (Correct Answer)
- E. Alpha-1 blocker
Asthma management and exacerbations Explanation: ***Beta-2 agonist***
- The patient presents with **acute exacerbation of COPD**, evidenced by his significant smoking history (50 pack-years), barrel chest (increased AP diameter), decreased breath sounds, and diffuse expiratory wheezing.
- **Short-acting beta-2 agonists (SABAs)** like **albuterol** are **first-line bronchodilators** in acute COPD exacerbations, providing rapid relief of bronchospasm by relaxing airway smooth muscle.
- According to **GOLD guidelines**, SABAs are the primary initial bronchodilator, often combined with short-acting muscarinic antagonists (SAMAs) like ipratropium for optimal effect.
- This patient requires **immediate bronchodilation** to address severe dyspnea and hypoxemia (88% on non-rebreather).
*Muscarinic blocker*
- **Short-acting muscarinic antagonists (SAMAs)** like **ipratropium bromide** are important adjunctive bronchodilators in acute COPD exacerbations.
- While SAMAs are effective and typically used **in combination with SABAs**, they are generally considered **adjunctive rather than first-line monotherapy**.
- In clinical practice, both SABAs and SAMAs are often administered together, but when asked for the "best next step," **beta-2 agonist is the more standard initial choice**.
*Glucocorticoid-analog*
- Systemic **glucocorticoids** like **prednisone** are indeed crucial in managing acute COPD exacerbations to reduce airway inflammation and shorten recovery time.
- However, they do **not provide immediate bronchodilation**, which is the most urgent need for this patient with severe respiratory distress and hypoxemia.
- Glucocorticoids are typically administered **after or concurrent with bronchodilators**, not as the initial intervention.
*Alpha-2 blocker*
- **Alpha-2 blockers have no role** in the management of acute respiratory distress or COPD exacerbations.
- These agents are used for conditions like **hypertension** or psychiatric disorders (note: clonidine is actually an alpha-2 **agonist**, not blocker).
- They do not affect airway caliber and are completely unrelated to bronchodilation.
*Alpha-1 blocker*
- **Alpha-1 blockers** like prazosin or doxazosin are used for **hypertension or benign prostatic hyperplasia (BPH)**.
- They have **no role in acute respiratory management** or COPD exacerbations.
- These agents cause peripheral vasodilation and do not affect airway smooth muscle or bronchospasm.
Asthma management and exacerbations US Medical PG Question 9: A 40-year-old man with persistent moderate asthma presents for a pulmonary function test. His ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) is 0.69, and his FEV1 is 65% of his predicted values. What other findings can be expected in the remainder of his pulmonary function test?
- A. Decreased diffusion capacity of carbon monoxide (DLCO)
- B. Decrease in FEV1 with albuterol
- C. Increase in fractional exhalation of nitric oxide (Correct Answer)
- D. Decrease in total lung capacity
- E. Increase in FEV1 with methacholine
Asthma management and exacerbations Explanation: ***Increase in fractional exhalation of nitric oxide***
- An increase in **fractional exhalation of nitric oxide (FeNO)** is a marker of **airway inflammation**, which is characteristic of asthma.
- This finding would further support the diagnosis of asthma in a patient with **obstructive lung disease** as indicated by the FEV1/FVC ratio and reduced FEV1.
*Decreased diffusion capacity of carbon monoxide (DLCO)*
- A decreased **DLCO** is typically seen in conditions affecting the **alveolar-capillary membrane**, such as emphysema or interstitial lung disease.
- In uncomplicated asthma, the **DLCO** is usually normal or even slightly increased due to increased pulmonary blood volume.
*Decrease in FEV1 with albuterol*
- **Albuterol** is a **short-acting beta-agonist (SABA)**, a bronchodilator that should *increase* FEV1 in a patient with reversible airway obstruction like asthma.
- A **decrease** in FEV1 after albuterol administration would be an unexpected and abnormal response, not consistent with asthma.
*Decrease in total lung capacity*
- A **decrease in total lung capacity (TLC)** is characteristic of **restrictive lung diseases**, where lung expansion is limited.
- Asthma is an **obstructive lung disease**, and patients often exhibit **air trapping** and **hyperinflation**, leading to a *normal or increased* TLC, not a decrease.
*Increase in FEV1 with methacholine*
- **Methacholine** is a **bronchoconstrictor** used in bronchial challenge tests to *induce* bronchospasm and a *decrease* in FEV1 in asthmatic patients.
- An **increase** in FEV1 with methacholine would be contrary to its pharmacological effect and the expected response in asthma.
Asthma management and exacerbations US Medical PG Question 10: A 10-year-old boy is brought in by his parents with increasing breathlessness. He was diagnosed with asthma about 2 years ago and has been on treatment since then. He was initially observed to have breathlessness, cough and chest tightness 2 or 3 times a week. He would wake up once or twice a month in the nighttime with breathlessness. At that time, his pediatrician started him on a Ventolin inhaler to be used during these episodes. His symptoms were well controlled until a few months ago when he started to experience increased nighttime awakenings due to breathlessness. He is unable to play outside with his friends as much because he gets winded easily and has to use his inhaler almost daily to help him breathe easier. He is able to walk and perform other routine activities without difficulty, but playing or participating in sports causes significant struggles. Based on his symptoms, his pediatrician adds an inhaled formoterol and budesonide combination to his current regime. During spirometry, which of the following peak expiratory flow rates will most likely be observed in this patient?
- A. 65% (Correct Answer)
- B. 55%
- C. 90%
- D. 40%
- E. 85%
Asthma management and exacerbations Explanation: ***65%***
- The patient's presentation of symptoms suggests **moderate persistent asthma**. This is characterized by daily symptoms, nighttime awakenings more than once a week but not nightly, and significant limitation in activity where playing causes struggles.
- In moderate persistent asthma, the **peak expiratory flow rate (PEFR)** or forced expiratory volume in 1 second (FEV1) is typically between **60% and 80%** of the predicted value. Therefore, 65% falls within this range.
*55%*
- A PEFR of 55% would indicate **severe persistent asthma**, which is characterized by continual symptoms throughout the day, frequent nighttime awakenings (often nightly), and extreme limitations in physical activity.
- While the patient's asthma is worsening, it does not yet meet the criteria for severe, as he can still perform routine activities without difficulty.
*90%*
- A PEFR of 90% would be consistent with **intermittent asthma** or **mild persistent asthma** that is very well controlled.
- The patient's symptoms, including daily inhaler use, nighttime awakenings, and activity limitations, clearly indicate that his asthma is not well-controlled and is more than mild.
*40%*
- A PEFR of 40% would suggest an **acute severe asthma exacerbation** or **very severe persistent asthma**.
- The patient's symptoms describe increasing frequency and severity, but not an acute, life-threatening exacerbation or such profound chronic lung function impairment.
*85%*
- A PEFR of 85% would typically be seen in **mild persistent asthma** or intermittent asthma, where symptoms are less frequent and less severe.
- The patient's current symptoms, including daily inhaler use and inability to play without significant struggles, are indicative of moderate asthma that is not well controlled.
More Asthma management and exacerbations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.