Systemic complications of acute pancreatitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Systemic complications of acute pancreatitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Systemic complications of acute pancreatitis US Medical PG Question 1: A 78-year-old man dies suddenly from complications of acute kidney failure. An autopsy is performed and microscopic evaluation of the kidneys shows pale, swollen cells in the proximal convoluted tubules. Microscopic evaluation of the liver shows similar findings. Which of the following is the most likely underlying mechanism of these findings?
- A. Double-stranded DNA breakage
- B. Impaired Na+/K+-ATPase pump activity (Correct Answer)
- C. Free radical formation
- D. Cytochrome C release
- E. Cytoplasmic triglyceride accumulation
Systemic complications of acute pancreatitis Explanation: ***Impaired Na+/K+-ATPase pump activity***
- **Acute kidney failure** leads to **hypoxia** and ATP depletion, which impairs the function of the **Na+/K+-ATPase pump** on the cell membrane.
- Failure of this pump results in **intracellular accumulation of sodium** and water, causing **cellular swelling** and pallor as seen in the kidneys and liver.
*Double-stranded DNA breakage*
- This is primarily associated with **apoptosis** or **radiation injury**, which would lead to nuclear fragmentation and cellular death rather than simple cellular swelling.
- While cell death can occur in acute kidney failure, the initial changes described (pale, swollen cells) are characteristic of **reversible cell injury** before extensive DNA damage.
*Free radical formation*
- **Free radical formation** (oxidative stress) can cause cellular injury, but it primarily leads to **lipid peroxidation of membranes** and damage to proteins and DNA, not directly to the widespread intracellular water accumulation described.
- While part of the injury cascade, it's not the most direct mechanism for the initial gross and microscopic findings of swelling.
*Cytochrome C release*
- **Cytochrome C release** from mitochondria is a critical step in the **intrinsic pathway of apoptosis**, leading to programmed cell death.
- The findings described (pale, swollen cells) are more indicative of **reversible cellular injury** or early necrosis, prior to the widespread activation of apoptosis.
*Cytoplasmic triglyceride accumulation*
- **Cytoplasmic triglyceride accumulation** (steatosis or fatty change) is often seen in conditions like **alcoholic liver disease** or **metabolic syndrome**.
- While it can be a sign of cellular injury, it does not directly explain the generalized "pale, swollen cells" observed in both the kidneys and liver following acute kidney failure, which points to water influx.
Systemic complications of acute pancreatitis US Medical PG Question 2: A 48-year-old female suffers a traumatic brain injury while skiing in a remote area. Upon her arrival to the ER, she is severely hypoxemic and not responsive to O2 therapy. She is started on a mechanical ventilator and 2 days later upon auscultation, you note late inspiratory crackles. Which of the following is most likely normal in this patient?
- A. Alveolar-arterial gradient
- B. Left atrial pressure (Correct Answer)
- C. Type II pneumocytes
- D. Type I pneumocytes
- E. Chest X-ray
Systemic complications of acute pancreatitis Explanation: ***Left atrial pressure***
- A normal left atrial pressure would be expected in a patient with **Non-Cardiogenic Pulmonary Edema**, which is implied by her severe hypoxemia refractory to oxygen, crackles, and history of **Traumatic Brain Injury**.
- **Neurogenic Pulmonary Edema**, a form of non-cardiogenic pulmonary edema, is a known complication of severe TBI and does not primarily involve left heart failure, thus maintaining a normal left atrial pressure.
*Alveolar-arterial gradient*
- The patient's severe **hypoxemia** unresponsive to oxygen therapy indicates a significant **ventilation-perfusion mismatch** or shunt, which would lead to an *increased* alveolar-arterial gradient.
- An increased A-a gradient is characteristic of pulmonary edema, where fluid in the alveoli impairs oxygen diffusion into the capillaries.
*Type II pneumocytes*
- In **acute respiratory distress syndrome (ARDS)**, which is strongly suggested by the patient's presentation (non-cardiogenic pulmonary edema), **Type II pneumocytes often proliferate** in the reparative phase.
- While they are normally involved in **surfactant production**, their function can be impaired, and their numbers might increase to replace damaged Type I cells, so they would not be "normal."
*Type I pneumocytes*
- **Type I pneumocytes** are the primary cells responsible for **gas exchange** and are highly susceptible to injury in conditions like ARDS or pulmonary edema.
- In such a critically ill patient with diffuse alveolar damage, these cells would likely be damaged or destroyed, thus *not* normal.
*Chest X-ray*
- Given the patient's severe hypoxemia, late inspiratory crackles, and probable pulmonary edema, her **Chest X-ray** would likely show **bilateral infiltrates** or **diffuse haziness**, characteristic of ARDS or neurogenic pulmonary edema.
- Therefore, a normal chest X-ray is highly unlikely in this clinical scenario.
Systemic complications of acute pancreatitis US Medical PG Question 3: A 27-year-old man is brought to the emergency department 30 minutes after being shot in the abdomen during a violent altercation. His temperature is 36.5°C (97.7°F), pulse is 118/min and regular, and blood pressure is 88/65 mm Hg. Examination shows cool extremities. Abdominal examination shows a 2.5-cm entrance wound in the left upper quadrant at the midclavicular line, below the left costal margin. Focused ultrasound shows free fluid in the left upper quadrant. Which of the following sets of hemodynamic changes is most likely in this patient?
Cardiac output (CO) | Pulmonary capillary wedge pressure (PCWP) | Systemic vascular resistance (SVR) | Central venous pressure (CVP)
- A. ↑ ↓ ↓ ↓
- B. ↓ ↓ ↑ ↑
- C. ↓ ↓ ↓ ↓
- D. ↓ ↓ ↑ ↓ (Correct Answer)
- E. ↓ ↑ ↑ ↑
Systemic complications of acute pancreatitis Explanation: ***↓ ↓ ↑ ↓***
- This patient is in **hypovolemic shock** due to hemorrhage, leading to decreased **cardiac output (CO)** and **pulmonary capillary wedge pressure (PCWP)** due to reduced preload.
- The body compensates for hypovolemia by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, while **central venous pressure (CVP)** decreases due to the depleted blood volume.
*↑ ↓ ↓ ↓*
- An increased **cardiac output** is inconsistent with hypovolemic shock, where the heart's ability to pump blood is compromised by a lack of circulating volume.
- While **PCWP**, **SVR**, and **CVP** decreasing could be seen in some forms of shock, the elevated CO rules out hypovolemic shock.
*↓ ↓ ↑ ↑*
- An elevated **central venous pressure (CVP)** is inconsistent with hypovolemic shock, as CVP reflects right atrial pressure and would be low due to decreased blood volume.
- While other parameters such as **CO** and **PCWP** decreasing and **SVR** increasing can be seen in hypovolemic shock, the increased CVP suggests a different hemodynamic state, like cardiogenic shock.
*↓ ↓ ↓ ↓*
- A decrease in **systemic vascular resistance (SVR)** is characteristic of **distributive shock** (e.g., septic or neurogenic shock), not hypovolemic shock, where compensatory vasoconstriction would lead to increased SVR.
- While **CO**, **PCWP**, and **CVP** would decrease due to overall poor perfusion, the SVR response differentiates it from hypovolemic shock.
*↓ ↑ ↑ ↑*
- An elevated **pulmonary capillary wedge pressure (PCWP)** and **central venous pressure (CVP)** indicate increased fluid volume or cardiac dysfunction, which is contrary to the reduced preload seen in hypovolemic shock.
- While **cardiac output (CO)** may decrease in cardiogenic shock, the other elevated pressures point away from a primary hypovolemic cause.
Systemic complications of acute pancreatitis US Medical PG Question 4: A 56-year-old man comes to the emergency department because of a 3-day history of severe epigastric pain that is radiating to his back and accompanied by nausea and vomiting. He has a history of alcohol use disorder. His blood pressure is 90/60 mm Hg and his pulse is 110/min. Physical examination shows diffuse abdominal tenderness and distention. Laboratory studies show:
Serum
Lipase 180 U/L (N = < 50 U/L)
Amylase 150 U/L
Creatinine 2.5 mg/dL
Urine
Sodium 45 mEq/L
Osmolality 280 mOsmol/kg H2O
Epithelial cell casts numerous
Laboratory studies from a recent office visit were within normal limits. This patient's condition is most likely to affect which of the following kidney structures first?
- A. Collecting duct
- B. Straight segment of proximal tubule (Correct Answer)
- C. Convoluted segment of proximal tubule
- D. Thin descending limb of loop of Henle
- E. Convoluted segment of distal tubule
Systemic complications of acute pancreatitis Explanation: ***Straight segment of proximal tubule***
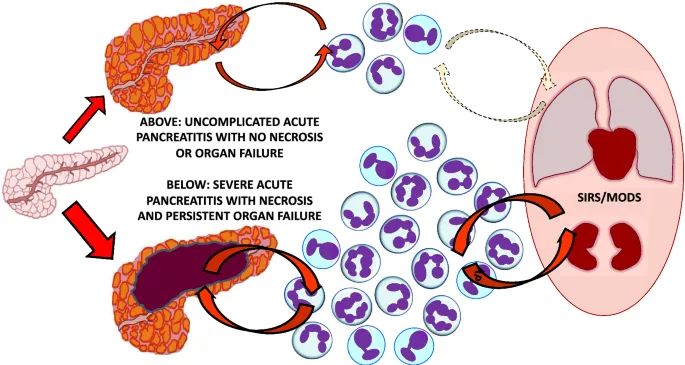
- The patient exhibits signs of **acute pancreatitis** (epigastric pain radiating to the back, nausea, vomiting, elevated lipase) and **hypotension** (90/60 mmHg, pulse 110/min), leading to **prerenal acute kidney injury (AKI)** which progresses to **acute tubular necrosis (ATN)** due to prolonged ischemia.
- The **straight segment of the proximal tubule** (pars recta) is highly susceptible to ischemic injury due to its high metabolic demand, low oxygen tension, and expression of vulnerable transport proteins, making it the first kidney structure affected in ATN.
*Collecting duct*
- While collecting ducts can be affected in severe ATN, they are generally **less vulnerable to ischemic injury** compared to the proximal tubules.
- Their primary role is water and solute reabsorption influenced by ADH, and they are not the initial site of damage in ischemic ATN.
*Convoluted segment of proximal tubule*
- The convoluted segment of the proximal tubule is metabolically active and susceptible to injury, but the **straight segment (pars recta)** is typically considered **more vulnerable to ischemia** due to its location and lower blood flow.
- This part of the tubule is also prone to damage, but the straight segment extending into the outer medulla is often affected earlier and more severely.
*Thin descending limb of loop of Henle*
- The thin descending limb is primarily involved in water reabsorption and has **lower metabolic activity** compared to the proximal tubules.
- It is generally **less susceptible to ischemic injury** than the proximal tubule segments.
*Convoluted segment of distal tubule*
- The distal convoluted tubule is important for fine-tuning electrolyte balance and is also metabolically active, but it is **less sensitive to ischemic injury** than the proximal tubules.
- It usually exhibits better preservation of function compared to the proximal tubule in ATN.
Systemic complications of acute pancreatitis US Medical PG Question 5: A 23-year-old man is admitted to the intensive care unit with acute respiratory distress syndrome (ARDS) due to influenza A. He has no history of serious illness and does not smoke. An x-ray of the chest shows diffuse bilateral infiltrates. Two weeks later, his symptoms have improved. Pulmonary examination on discharge shows inspiratory crackles at both lung bases. This patient is most likely to develop which of the following long-term complications?
- A. Panacinar emphysema
- B. Asthma
- C. Pulmonary embolism
- D. Interstitial lung disease (Correct Answer)
- E. Spontaneous pneumothorax
Systemic complications of acute pancreatitis Explanation: ***Interstitial lung disease***
- Patients who recover from **acute respiratory distress syndrome (ARDS)**, especially severe cases like that induced by influenza A, often develop **pulmonary fibrosis** leading to interstitial lung disease.
- The presence of **inspiratory crackles at both lung bases** after recovery from ARDS strongly suggests residual fibrotic changes.
*Panacinar emphysema*
- This condition is typically associated with **alpha-1 antitrypsin deficiency** or long-term smoking history, neither of which is indicated in this patient.
- Emphysema involves destruction of alveoli, not typically a direct long-term consequence of ARDS.
*Asthma*
- Asthma is a chronic inflammatory airway disease characterized by **reversible airflow obstruction**, usually with a history of recurrent episodes, not necessarily a direct sequela of ARDS.
- This patient's previous lack of serious illness and the nature of ARDS recovery make new-onset asthma unlikely as a long-term complication.
*Pulmonary embolism*
- While ARDS patients are at increased risk of **venous thromboembolism** during the acute phase due to immobility and inflammation, it is an acute complication, not a typical long-term sequela.
- Long-term complications are more related to lung parenchymal damage rather than persistent embolic risk.
*Spontaneous pneumothorax*
- Although ARDS can be complicated by **barotrauma** and pneumothorax during mechanical ventilation, a spontaneous pneumothorax as a long-term complication after recovery is less common.
- It does not explain the persistent bilateral basal crackles.
Systemic complications of acute pancreatitis US Medical PG Question 6: A 29-year-old man is brought to the emergency room 6 hours after the onset of severe epigastric pain and vomiting. His heart rate is 110/min and blood pressure is 98/72 mm Hg. He is diagnosed with acute pancreatitis, and fluid resuscitation with normal saline is initiated. Which of the following is the most likely immediate effect of fluid resuscitation in this patient?
- A. Increase in plasma oncotic pressure
- B. Increase in glomerular filtration fraction
- C. Increase in volume of distribution
- D. Increase in cardiac afterload
- E. Increase in myocardial oxygen demand (Correct Answer)
Systemic complications of acute pancreatitis Explanation: ***Increase in myocardial oxygen demand***
- Fluid resuscitation in a hypotensive patient with tachycardia increases **cardiac preload** and **stroke volume**, leading to higher cardiac output.
- This increased workload on the heart, especially when the patient is already tachycardic, directly translates to an **increased demand for oxygen** by the myocardium.
*Increase in plasma oncotic pressure*
- Fluid resuscitation with **normal saline** (crystalloid solution) primarily increases intravascular volume but does not significantly increase plasma proteins, which are responsible for oncotic pressure.
- In fact, large volumes of crystalloids can sometimes **slightly decrease oncotic pressure** due to hemodilution.
*Increase in glomerular filtration fraction*
- Fluid resuscitation improves **renal perfusion** and **glomerular filtration rate (GFR)** by restoring blood pressure and intravascular volume.
- However, the glomerular filtration fraction, which is the ratio of GFR to renal plasma flow, does not necessarily increase; it might even decrease as renal plasma flow improves.
*Increase in volume of distribution*
- Volume of distribution refers to the apparent volume into which a drug distributes in the body. Fluid resuscitation **increases the intravascular fluid volume**, which is part of the total body water, but this is a change in actual volume, not a change in a pharmacokinetic parameter for drug distribution.
- It would more accurately be described as increasing the **effective circulating volume**, not the **volume of distribution** in a pharmacological sense.
*Increase in cardiac afterload*
- Cardiac afterload refers to the resistance the heart must overcome to eject blood. While fluid resuscitation increases **intravascular volume**, it primarily affects **preload**.
- Although indirectly, by improving cardiac output and maintaining blood pressure, there might be a slight increase in afterload, an **increase in myocardial oxygen demand** is a more direct and immediate consequence of the increased workload.
Systemic complications of acute pancreatitis US Medical PG Question 7: A 59-year-old man presents to the emergency department with diffuse abdominal pain, nausea, and vomiting. Laboratory evaluation on admission is significant for serum glucose of 241 mg/dL, AST of 321 IU/L, and leukocytes of 21,200/μL. Within 3 days of admission with supportive care in the intensive care unit, the patient's clinical condition begins to improve. Based on Ranson's criteria, what is this patient's overall risk of mortality, assuming all other relevant factors are negative?
- A. 15% (Correct Answer)
- B. 40%
- C. 100%
- D. 80%
- E. < 10%
Systemic complications of acute pancreatitis Explanation: ***15%***
- This patient meets four Ranson's criteria on admission: **age > 55 years** (59 years), **WBC > 16,000/μL** (21,200/μL), **glucose > 200 mg/dL** (241 mg/dL), and **AST > 250 U/L** (321 U/L).
- Four Ranson's criteria correspond to a **15% mortality risk**.
- The stem specifies that all other relevant factors (the 48-hour criteria) are negative.
*40%*
- A 40% mortality risk is associated with **5-6 positive Ranson's criteria**.
- This patient fulfilled 4 criteria on admission, indicating a lower risk category.
*100%*
- A 100% mortality risk is associated with **7 or more positive Ranson's criteria**.
- This patient only fulfilled 4 criteria, indicating a significantly lower risk.
*80%*
- An 80% mortality risk is associated with **7 or more positive Ranson's criteria**.
- This patient only fulfilled 4 criteria, which places him in a much lower risk category.
*< 10%*
- A mortality risk of less than 10% typically correlates with **0-2 positive Ranson's criteria**.
- This patient has 4 positive criteria, placing him in a higher risk category.
Systemic complications of acute pancreatitis US Medical PG Question 8: A 27-year-old-man is brought to the emergency department 30 minutes after being involved in a motorcycle accident. He lost control at high speed and was thrown forward onto the handlebars. On arrival, he is alert and responsive. He has abdominal pain and superficial lacerations on his left arm. Vital signs are within normal limits. Examination shows a tender, erythematous area over his epigastrium. The abdomen is soft and non-distended. A CT scan of the abdomen shows no abnormalities. Treatment with analgesics is begun, the lacerations are cleaned and dressed, and the patient is discharged home after 2 hours of observation. Four days later, the patient returns to the emergency department with gradually worsening upper abdominal pain, fever, poor appetite, and vomiting. His pulse is 91/min and blood pressure is 135/82 mm Hg. Which of the following is the most likely diagnosis?
- A. Abdominal compartment syndrome
- B. Aortic dissection
- C. Splenic rupture
- D. Pancreatic ductal injury (Correct Answer)
- E. Diaphragmatic rupture
Systemic complications of acute pancreatitis Explanation: ***Pancreatic ductal injury***
- A forceful impact to the **epigastrium** (e.g., falling onto handlebars) can cause **pancreatic injury**, particularly a **ductal transection**, due to the pancreas being compressed against the vertebral column.
- Initial CT scans can be normal because the injury to the **ductal system** takes time to manifest, leading to delayed symptoms like **worsening abdominal pain, fever, vomiting**, and **poor appetite** several days later due to **pancreatitis** or a **pseudocyst** formation.
*Abdominal compartment syndrome*
- This typically presents with **acute abdominal distension**, increased intra-abdominal pressure, and organ dysfunction (e.g., oliguria, respiratory compromise), which are not described here.
- It's an immediate complication of severe trauma or fluid resuscitation, not a delayed presentation like described.
*Aortic dissection*
- Characterized by **sudden-onset, severe, tearing chest or back pain** and often involves hypertension or Marfan syndrome.
- It would manifest immediately with hemodynamic instability and distinct pain, not a delayed presentation of progressive abdominal symptoms.
*Splenic rupture*
- Often causes **left upper quadrant pain**, **Kehr's sign** (referred shoulder pain), and **hemodynamic instability** due to significant blood loss.
- While possible in trauma, a normal initial CT scan makes this less likely, and its symptoms usually appear earlier or are more severe.
*Diaphragmatic rupture*
- Can present with **dyspnea, shoulder pain**, or signs of **herniated abdominal organs** into the chest.
- It causes more immediate respiratory distress or gastrointestinal obstruction symptoms, and the abdominal symptoms described are not typical for this injury.
Systemic complications of acute pancreatitis US Medical PG Question 9: A 45-year-old man with a history of biliary colic presents with one-day of intractable nausea, vomiting, and abdominal pain radiating to the back. Temperature is 99.7 deg F (37.6 deg C), blood pressure is 102/78 mmHg, pulse is 112/min, and respirations are 22/min. On abdominal exam, he has involuntary guarding and tenderness to palpation in the right upper quadrant and epigastric regions. Laboratory studies show white blood cell count 18,200/uL, alkaline phosphatase 650 U/L, total bilirubin 2.5 mg/dL, amylase 500 U/L, and lipase 1160 U/L. Which of the patient's laboratory findings is associated with increased mortality?
- A. White blood cell count (Correct Answer)
- B. Lipase
- C. Amylase
- D. Total bilirubin
- E. Alkaline phosphatase
Systemic complications of acute pancreatitis Explanation: ***White blood cell count***
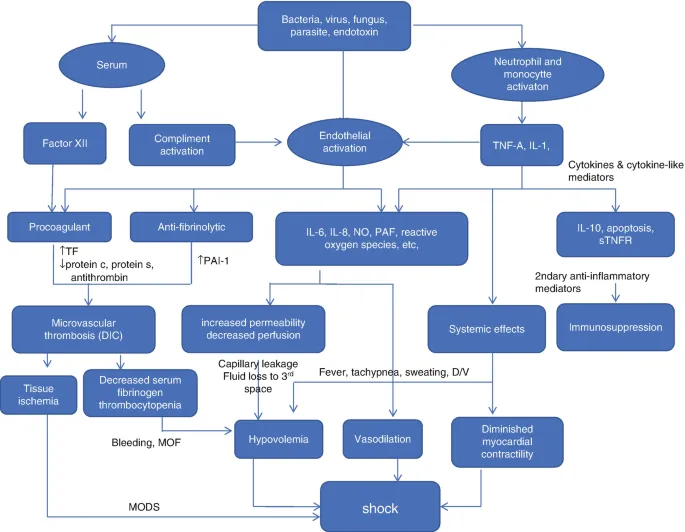
- An **elevated white blood cell count (leukocytosis)** above 16,000/uL is a component of the **Ranson criteria** and can indicate severe inflammation and systemic response, which is associated with increased mortality in acute pancreatitis.
- This finding, in conjunction with other clinical and laboratory signs, points towards a more severe inflammatory process and potential for complications leading to worse outcomes.
*Lipase*
- While significantly elevated **lipase** levels (more than three times the upper limit of normal) are diagnostic for acute pancreatitis, the absolute value itself is not directly correlated with the severity or prognosis of the disease.
- Extremely high lipase levels confirm the diagnosis but do not reliably predict increased mortality.
*Amylase*
- Similar to lipase, markedly elevated **amylase** levels are crucial for diagnosing acute pancreatitis but do not significantly correlate with disease severity or mortality.
- The degree of amylase elevation does not predict the likelihood of complications or death.
*Total bilirubin*
- An elevated **total bilirubin** suggests biliary obstruction, which is often the underlying cause of gallstone pancreatitis in this case.
- While it points to the etiology, isolated bilirubin elevation is not a direct prognostic marker for increased mortality in acute pancreatitis unless it leads to severe complications like cholangitis or liver failure.
*Alkaline phosphatase*
- An elevated **alkaline phosphatase** also indicates cholestasis or biliary obstruction.
- Similar to bilirubin, it helps identify the cause of pancreatitis but is not included in common prognostic scoring systems (like Ranson's or APACHE II) as a direct predictor of increased mortality in acute pancreatitis itself.
Systemic complications of acute pancreatitis US Medical PG Question 10: A 72-year-old woman comes to the emergency department because of upper abdominal pain and nausea for the past hour. The patient rates the pain as an 8 to 9 on a 10-point scale. She has had an episode of nonbloody vomiting since the pain started. She has a history of type 2 diabetes mellitus, hypertension, and osteoporosis. The patient has smoked 2 packs of cigarettes daily for 40 years. She drinks 5–6 alcoholic beverages daily. Current medications include glyburide, lisinopril, and oral vitamin D supplements. Her temperature is 38.5°C (101.3°F), pulse is 110/min, and blood pressure is 138/86 mm Hg. Examination shows severe epigastric tenderness to palpation with guarding but no rebound. Ultrasonography of the abdomen shows diffuse enlargement of the pancreas; no gallstones are visualized. The patient is admitted to the hospital for pain control and intravenous hydration. Which of the following is the most appropriate next step in the management of this patient’s pain?
- A. Oral gabapentin every 24 hours
- B. Transdermal fentanyl every 72 hours
- C. Oral acetaminophen every 6 hours
- D. Patient-controlled intravenous hydromorphone (Correct Answer)
- E. Transdermal bupivacaine on request
Systemic complications of acute pancreatitis Explanation: ***Patient-controlled intravenous hydromorphone***
- This patient presents with **acute pancreatitis**, characterized by severe epigastric pain, nausea, vomiting, fever, and findings indicative of pancreatic inflammation (enlarged pancreas on ultrasound, guarding without rebound). **Opioids**, such as hydromorphone, are the mainstay for **severe pain relief** in acute pancreatitis.
- **Patient-controlled analgesia (PCA)** with intravenous opioids allows the patient to self-administer small, frequent doses, providing optimal pain control while minimizing the risk of over-sedation, making it suitable for managing **acute severe pain**.
*Oral gabapentin every 24 hours*
- **Gabapentin** is primarily used for **neuropathic pain** or as an adjunct for chronic pain, not typically for acute severe visceral pain like that seen in acute pancreatitis.
- Its **oral route** and every 24-hour dosing schedule are too slow and infrequent for rapid pain control in an emergency setting with severe pain.
*Transdermal fentanyl every 72 hours*
- **Transdermal fentanyl** is indicated for **chronic severe pain** that requires continuous opioid administration and is not suitable for the rapid onset and fluctuating intensity of acute pancreatitis pain.
- The **transdermal route** and long dosing interval mean it would not provide immediate or adequate pain relief for a patient experiencing pain rated 8-9/10.
*Oral acetaminophen every 6 hours*
- **Acetaminophen** is a non-opioid analgesic generally used for **mild to moderate pain** and fever control. It is insufficient for the severe pain experienced in acute pancreatitis.
- The **oral route** takes longer to achieve therapeutic levels and may be limited by the patient's nausea and vomiting.
*Transdermal bupivacaine on request*
- **Bupivacaine** is a **local anesthetic** typically used for regional anesthesia or nerve blocks, not for systemic management of acute visceral pain like pancreatitis.
- **Transdermal application** of bupivacaine is not a standard or effective method for managing widespread, severe abdominal pain and would not provide adequate relief.
More Systemic complications of acute pancreatitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.