Diagnosis of chronic pancreatitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diagnosis of chronic pancreatitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diagnosis of chronic pancreatitis US Medical PG Question 1: A 43-year-old man is brought to the emergency department because of severe epigastric pain and vomiting for 6 hours. The pain radiates to his back and he describes it as 9 out of 10 in intensity. He has had 3–4 episodes of vomiting during this period. He admits to consuming over 13 alcoholic beverages the previous night. There is no personal or family history of serious illness and he takes no medications. He is 177 cm (5 ft 10 in) tall and weighs 55 kg (121 lb); BMI is 17.6 kg/m2. He appears uncomfortable. His temperature is 37.5°C (99.5°F), pulse is 97/min, and blood pressure is 128/78 mm Hg. Abdominal examination shows severe epigastric tenderness to palpation. Bowel sounds are hypoactive. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.5 g/dL
Hematocrit 62%
Leukocyte count 13,800/mm3
Serum
Na+ 134 mEq/L
K+ 3.6 mEq/L
Cl- 98 mEq/L
Calcium 8.3 mg/dL
Glucose 180 mg/dL
Creatinine 0.9 mg/dL
Amylase 150 U/L
Lipase 347 U/L (N = 14–280)
Total bilirubin 0.8 mg/dL
Alkaline phosphatase 66 U/L
AST 19 U/L
ALT 18 U/L
LDH 360 U/L
Which of the following laboratory studies is the best prognostic indicator for this patient's condition?
- A. AST/ALT ratio
- B. Alkaline phosphatase
- C. Total bilirubin
- D. Lipase
- E. Hematocrit (Correct Answer)
Diagnosis of chronic pancreatitis Explanation: ***Hematocrit***
- A rising **hematocrit** (due to **hemoconcentration**) or one that fails to fall after initial fluid resuscitation is an important indicator of volume depletion and a **poor prognostic sign** in **acute pancreatitis**.
- This patient's hematocrit is elevated at **62%**, suggesting significant hemoconcentration and a higher risk for complications like **pancreatic necrosis**.
*AST/ALT ratio*
- While an elevated AST/ALT ratio can suggest **alcoholic liver disease**, it is not a direct **prognostic indicator** for the severity or outcome of **acute pancreatitis**.
- In pancreatitis, liver enzymes are typically elevated secondarily to inflammation or biliary obstruction, but their ratio does not directly predict the course of the pancreatitis itself.
*Alkaline phosphatase*
- **Alkaline phosphatase** is an indicator of **biliary obstruction** or **cholestasis**, which can be a cause of pancreatitis (e.g., gallstone pancreatitis).
- Its value does not directly predict the **severity** or **prognosis** of acute pancreatitis once it has developed, especially in a case of alcoholic pancreatitis.
*Total bilirubin*
- **Total bilirubin** levels primarily reflect **biliary obstruction** or **liver dysfunction**.
- While gallstone pancreatitis can increase bilirubin, it is not a primary prognostic marker for the development of severe complications in **acute pancreatitis**, nor is it significantly elevated in this patient.
*Lipase*
- **Elevated lipase** is highly specific and sensitive for the **diagnosis of acute pancreatitis**, confirming the diagnosis in this case.
- However, the absolute level of lipase does **not correlate** with the **severity** or **prognosis** of acute pancreatitis; even mild pancreatitis can have very high lipase levels.
Diagnosis of chronic pancreatitis US Medical PG Question 2: A 52-year-old woman presents to the urgent care center with several hours of worsening abdominal discomfort with radiation to the back. The patient also complains of malaise, chills, nausea, and vomiting. Social history is notable for alcoholism. On physical exam, she is febrile to 39.5°C (103.1°F), and she is diffusely tender to abdominal palpation. Complete blood count is notable for 13,500 white blood cells, bilirubin 2.1, lipase 842, and amylase 3,210. Given the following options, what is the most likely diagnosis?
- A. Choledocholithiasis
- B. Ascending cholangitis
- C. Gallstone pancreatitis (Correct Answer)
- D. Cholelithiasis
- E. Acute cholecystitis
Diagnosis of chronic pancreatitis Explanation: ***Gallstone pancreatitis***
- The patient presents with classic symptoms of **acute pancreatitis**: severe abdominal pain radiating to the back, nausea, vomiting, and markedly elevated **lipase (842)** and **amylase (3,210)**.
- The **key differentiating feature** is the elevated **bilirubin (2.1 mg/dL)**, which indicates biliary obstruction from a gallstone passing through or obstructing the ampulla of Vater.
- **Gallstone pancreatitis** is the most common cause of acute pancreatitis in women, and the combination of pancreatitis with hyperbilirubinemia strongly suggests a biliary etiology rather than alcoholic pancreatitis (which typically does not cause elevated bilirubin).
- While the patient has a history of alcoholism, the elevated bilirubin makes **gallstone pancreatitis** the most likely diagnosis.
*Choledocholithiasis*
- This refers to a stone in the **common bile duct**, which can cause biliary obstruction and elevated bilirubin.
- However, choledocholithiasis alone does not explain the **markedly elevated lipase and amylase**, which indicate pancreatic inflammation.
- Choledocholithiasis may be present as part of the pathophysiology, but the clinical picture is acute pancreatitis caused by the stone (gallstone pancreatitis).
*Ascending cholangitis*
- This serious bile duct infection presents with **Charcot's triad** (fever, jaundice, right upper quadrant pain) or **Reynolds' pentad** (adds altered mental status and hypotension).
- While the patient is febrile, she lacks **jaundice**, hypotension, or altered mental status.
- The **extremely elevated lipase and amylase** point to pancreatitis rather than cholangitis as the primary process.
*Cholelithiasis*
- This simply means **gallstones in the gallbladder**, which are often asymptomatic.
- The patient's acute presentation with fever, systemic symptoms, and markedly elevated pancreatic enzymes indicates a complication of gallstones (pancreatitis), not just their presence.
*Acute cholecystitis*
- This is **gallbladder inflammation**, typically presenting with right upper quadrant pain, fever, positive Murphy's sign, and leukocytosis.
- The **diffuse abdominal tenderness** (not localized to RUQ), pain radiating to the back, and **extremely elevated lipase and amylase** are characteristic of pancreatitis, not cholecystitis.
- Acute cholecystitis does not cause such dramatic elevations in pancreatic enzymes.
Diagnosis of chronic pancreatitis US Medical PG Question 3: A 42-year-old man comes to the physician because of severe epigastric pain for a week. The pain is constant and he describes it as 6 out of 10 in intensity. The pain radiates to his back and is worse after meals. He has had several episodes of nausea and vomiting during this period. He has taken ibuprofen for multiple similar episodes of pain during the past 6 months. He also has had a 5.4-kg (12-lb) weight loss over the past 4 months. He has a 12-year history of drinking 3 to 4 pints of rum daily. He has been hospitalized three times for severe abdominal pain in the past 3 years. He appears ill. His temperature is 37°C (98.6°F), pulse is 87/min, and blood pressure is 110/70 mm Hg. There is severe epigastric tenderness to palpation. Bowel sounds are normal. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.6 g/dL
Leukocyte count 7,800/mm3
Serum
Glucose 106 mg/dL
Creatinine 1.1 mg/dL
Amylase 150 U/L
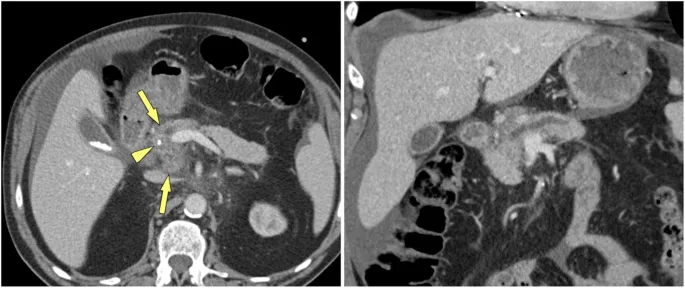
A CT of the abdomen is shown. Which of the following is the most appropriate long-term management for this patient?
- A. Pancreatic enzyme therapy (Correct Answer)
- B. Whipple procedure
- C. Endoscopic stent placement
- D. Celiac ganglion block
- E. Gluten-free diet
Diagnosis of chronic pancreatitis Explanation: ***Pancreatic enzyme therapy***
- This patient likely has **chronic pancreatitis** due to long-term alcohol abuse, presenting with severe epigastric pain, weight loss, and recurrent episodes. **Pancreatic enzyme replacement therapy (PERT)** helps in managing malabsorption and pain by reducing pancreatic stimulation.
- While amylase is only slightly elevated (150 U/L), this is typical in chronic pancreatitis where extensive glandular destruction prevents dramatic enzyme elevation seen in acute pancreatitis. The abdominal CT would likely show calcifications or ductal dilation, further supporting the diagnosis and the need for enzyme support due to **exocrine insufficiency.**
*Whipple procedure*
- The **Whipple procedure** (pancreaticoduodenectomy) is a complex surgical intervention primarily performed for **pancreatic head tumors** or severe, intractable chronic pancreatitis not amenable to less invasive treatments.
- This patient's symptoms, while severe, do not immediately indicate a need for such aggressive surgery, and other medical managements should be attempted first.
*Endoscopic stent placement*
- **Endoscopic stent placement** is typically used to relieve **biliary obstruction** or **pancreatic duct strictures** that cause pain or cholangitis in chronic pancreatitis.
- While it might be considered for specific ductal complications, it is not the initial long-term management for the diverse symptoms of chronic pancreatitis, especially **exocrine insufficiency**.
*Celiac ganglion block*
- A **celiac ganglion block** provides temporary pain relief for severe abdominal pain, particularly in conditions like **chronic pancreatitis** or **pancreatic cancer**, by interrupting nerve signals.
- It is a **palliative measure** for pain control and does not address the underlying **exocrine insufficiency** or disease progression, making it not a long-term comprehensive management strategy.
*Gluten-free diet*
- A **gluten-free diet** is the primary treatment for **celiac disease**, an autoimmune disorder affecting the small intestine.
- There is no clinical indication or laboratory finding in this patient's presentation (e.g., diarrhea, positive celiac serology) to suggest celiac disease as the cause of his symptoms or to warrant a gluten-free diet.
Diagnosis of chronic pancreatitis US Medical PG Question 4: A 75-year-old man presents to the emergency department for abdominal pain. The patient states the pain started this morning and has been worsening steadily. He decided to come to the emergency department when he began vomiting. The patient has a past medical history of obesity, diabetes, alcohol abuse, and hypertension. His current medications include captopril, insulin, metformin, sodium docusate, and ibuprofen. His temperature is 104.0°F (40°C), blood pressure is 160/97 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Abdominal exam reveals left lower quadrant tenderness. Cardiac exam reveals a crescendo systolic murmur heard best by the right upper sternal border. Lab values are ordered and return as below.
Hemoglobin: 15 g/dL
Hematocrit: 42%
Leukocyte count: 19,500 cells/mm^3 with normal differential
Platelet count: 226,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 144 mg/dL
Creatinine: 1.2 mg/dL
Ca2+: 9.8 mg/dL
Which of the following is the most accurate test for this patient's condition?
- A. Colonoscopy
- B. Sigmoidoscopy
- C. Amylase and lipase levels
- D. Barium enema
- E. CT scan (Correct Answer)
Diagnosis of chronic pancreatitis Explanation: ***CT scan***
- The patient presents with classic symptoms of **diverticulitis**, including **left lower quadrant pain**, **fever**, and **leukocytosis**. A **CT scan with oral and IV contrast** is the most accurate diagnostic test to identify diverticular inflammation, abscess formation, or perforation.
- A CT scan can also help rule out other causes of abdominal pain and guide further management, such as the need for percutaneous drainage of an abscess.
*Colonoscopy*
- **Colonoscopy is contraindicated during an acute episode of diverticulitis** due to the risk of **perforation** of an inflamed colon.
- It may be considered **6-8 weeks after resolution of acute diverticulitis** to investigate for other pathologies such as malignancy.
*Sigmoidoscopy*
- Similar to colonoscopy, **sigmoidoscopy is generally avoided in acute diverticulitis** because of the risk of **perforation** of the inflamed bowel from instrumentation.
- Its diagnostic yield in acute settings is also limited compared to CT imaging.
*Amylase and lipase levels*
- These tests are primarily used to diagnose **pancreatitis**, which typically presents with **epigastric pain radiating to the back**, often associated with elevated enzyme levels.
- While vomiting is present, the **left lower quadrant tenderness and fever** point away from pancreatitis as the primary diagnosis.
*Barium enema*
- **Barium enema is generally contraindicated in acute diverticulitis** due to the risk of **perforation** and the introduction of barium into the peritoneum, which can cause severe peritonitis.
- It has largely been replaced by **CT scanning** for its superior safety profile and diagnostic accuracy in acute abdominal conditions.
Diagnosis of chronic pancreatitis US Medical PG Question 5: A 29-year-old woman presents with a 2-hour history of sudden onset of severe mid-epigastric pain. The pain radiates to the back, and is not relieved by over-the-counter antacids. The patient also complains of profuse vomiting. The patient’s medical history is negative for similar symptoms. She consumes 3–4 alcoholic drinks daily. The blood pressure is 80/40 mm Hg and the heart rate is 105/min. Examination of the lungs reveals bibasilar crackles. Abdominal examination reveals diffuse tenderness involving the entire abdomen, marked guarding, rigidity, and reduced bowel sounds. The chest X-ray is normal. However, the abdominal CT scan reveals peritoneal fluid collection and diffuse pancreatic enlargement. The laboratory findings include:
Aspartate aminotransferase 63 IU/L
Alkaline phosphatase 204 IU/L
Alanine aminotransferase 32 IU/L
Serum amylase 500 IU/L (Normal: 25-125 IU/L)
Serum lipase 1,140 IU/L (Normal: 0-160 IU/L)
Serum calcium 2 mmol/L
Which of the following cellular changes are most likely, based on the clinical and laboratory findings?
- A. Liquefactive necrosis
- B. Dry gangrene
- C. Caseous necrosis
- D. Coagulative necrosis
- E. Fat necrosis (Correct Answer)
Diagnosis of chronic pancreatitis Explanation: ***Fat necrosis***
- The patient's presentation with severe epigastric pain radiating to the back, elevated serum amylase and lipase, **alcohol abuse**, and diffuse pancreatic enlargement indicates **acute pancreatitis**.
- **Fat necrosis** is a characteristic pathologic finding in acute pancreatitis, resulting from the release of activated pancreatic enzymes (like lipase) into the surrounding adipose tissue, causing **FFA (free fatty acid)** formation that complexes with calcium (saponification).
*Liquefactive necrosis*
- This type of necrosis is characterized by the complete digestion of dead cells, resulting in a **viscous liquid mass**.
- It is typically seen in **bacterial infections** or **cerebral infarcts**, not primarily in pancreatitis.
*Dry gangrene*
- **Dry gangrene** involves ischemic necrosis, usually affecting the extremities, where the tissue becomes **dry, shrunken, and black**.
- It is caused by **lack of blood supply** and does not fit the clinical picture of acute pancreatitis.
*Caseous necrosis*
- **Caseous necrosis** is a distinct form of coagulative necrosis, characterized by a **cheese-like appearance** of the necrotic tissue.
- It is most commonly associated with **tuberculosis** and certain fungal infections, not acute pancreatitis.
*Coagulative necrosis*
- **Coagulative necrosis** is characterized by the preservation of the cell shape and tissue architecture for several days after cell death, often due to **ischemia** (e.g., myocardial infarction).
- While pancreatic cells can undergo coagulative necrosis in severe ischemia, **fat necrosis** is specifically and prominently associated with the enzymatic destruction in acute pancreatitis.
Diagnosis of chronic pancreatitis US Medical PG Question 6: A 55-year-old woman presents with acute onset abdominal pain radiating to her back, nausea, and vomiting. CT scan suggests a diagnosis of acute pancreatitis. The pathogenesis of acute pancreatitis relates to inappropriate activation of trypsinogen to trypsin. Which of the following activates trypsin in normal digestion?
- A. Secretin
- B. Lipase
- C. Cholecystokinin
- D. Enterokinase (Correct Answer)
- E. Amylase
Diagnosis of chronic pancreatitis Explanation: ***Enterokinase***
- **Enterokinase** (also known as enteropeptidase) is a brush border enzyme of the duodenum that specifically cleaves and activates pancreatic **trypsinogen** into its active form, **trypsin**.
- Once activated, **trypsin** then activates other pancreatic proteases (e.g., chymotrypsinogen, procarboxypeptidases, proelastase) within the intestinal lumen.
*Secretin*
- **Secretin** is a hormone released by S cells in the duodenum in response to acidic chyme and acts on the pancreas to stimulate the secretion of **bicarbonate-rich fluid**, which neutralizes gastric acid.
- It does not directly activate digestive enzymes like trypsinogen.
*Lipase*
- **Lipase** is a pancreatic enzyme secreted in its active form that breaks down **dietary fats** (triglycerides) into fatty acids and monoglycerides.
- It plays no role in the activation of trypsinogen.
*Cholecystokinin*
- **Cholecystokinin (CCK)** is a hormone released by I cells in the duodenum in response to fats and proteins, stimulating the contraction of the **gallbladder** and the secretion of **pancreatic enzymes**.
- While it promotes the release of pancreatic enzymes, it does not directly activate trypsinogen.
*Amylase*
- **Amylase** is a pancreatic enzyme secreted in its active form that breaks down **complex carbohydrates** (starches) into simpler sugars (disaccharides and oligosaccharides).
- It is not involved in the activation cascade of pancreatic proteases.
Diagnosis of chronic pancreatitis US Medical PG Question 7: A 54-year-old man presents to his primary care physician with a 2-month-history of diarrhea. He says that he feels the urge to defecate 3-4 times per day and that his stools have changed in character since the diarrhea began. Specifically, they now float, stick to the side of the toilet bowl, and smell extremely foul. His past medical history is significant for several episodes of acute pancreatitis secondary to excessive alcohol consumption. His symptoms are found to be due to a deficiency in an enzyme. Which of the following enzymes is most likely deficient in this patient?
- A. Enterokinase
- B. Amylase
- C. Colipase
- D. Lipase (Correct Answer)
- E. Chymotrypsin
Diagnosis of chronic pancreatitis Explanation: ***Lipase***
- The patient's history of **recurrent pancreatitis** likely led to **exocrine pancreatic insufficiency**, reducing the production of digestive enzymes, particularly **lipase**.
- **Steatorrhea** (foul-smelling, floating, sticky stools) is a classic symptom of **fat malabsorption**, which occurs due to insufficient lipase for triglyceride digestion.
*Enterokinase*
- **Enterokinase** is an enzyme produced in the **duodenum** that activates trypsinogen to trypsin, which then activates other pancreatic proteases.
- A deficiency would primarily cause **protein malabsorption**, not the pronounced fat malabsorption (steatorrhea) seen in this patient.
*Amylase*
- **Amylase** is responsible for **carbohydrate digestion**.
- While chronic pancreatitis can lead to amylase deficiency, the primary symptom of this patient's diarrhea, steatorrhea, points more directly to **fat malabsorption** rather than carbohydrate malabsorption.
*Colipase*
- **Colipase** is a co-enzyme that helps **lipase** bind to the fat-water interface to digest triglycerides.
- While essential for fat digestion, lipase itself is the primary enzyme responsible, and a direct deficiency in colipase alone is less commonly implicated as the sole cause of severe steatorrhea than a general pancreatic enzyme insufficiency affecting lipase production.
*Chymotrypsin*
- **Chymotrypsin** is a **protease** primarily involved in **protein digestion**.
- A deficiency would lead to **protein malabsorption**, which typically presents with symptoms like muscle wasting and edema, rather than the prominent steatorrhea described.
Diagnosis of chronic pancreatitis US Medical PG Question 8: A patient presents to the emergency room in an obtunded state. The patient is a known nurse within the hospital system and has no history of any medical problems. A finger stick blood glucose is drawn showing a blood glucose of 25 mg/dL.
The patient's daughter immediately arrives at the hospital stating that her mother has been depressed recently and that she found empty syringes in the bathroom at the mother's home. Which of the following is the test that will likely reveal the diagnosis?
- A. Fasting blood glucose
- B. Urine metanephrines
- C. Genetic testing
- D. 24 hr cortisol
- E. C-peptide level (Correct Answer)
Diagnosis of chronic pancreatitis Explanation: ***C-peptide level***
- A **low C-peptide level** in the presence of **hypoglycemia** and high insulin levels confirms the diagnosis of **exogenous insulin administration** (factitious hypoglycemia).
- **C-peptide** is cleaved from **proinsulin** in equimolar amounts with endogenous insulin, making it an excellent marker to differentiate endogenous insulin production from exogenous insulin injection.
- In this case: **Low C-peptide + High insulin + Hypoglycemia** = exogenous insulin administration.
*Fasting blood glucose*
- The patient already has documented **hypoglycemia (25 mg/dL)**, so an additional fasting blood glucose test would not provide further diagnostic information about the **cause** of hypoglycemia.
- A single fasting blood glucose level indicates current glucose status but **does not differentiate** between endogenous insulin overproduction (insulinoma) and exogenous insulin administration.
*Urine metanephrines*
- **Urine metanephrines** are used to diagnose **pheochromocytoma**, a catecholamine-secreting tumor of the adrenal medulla.
- Pheochromocytoma presents with **hypertension**, palpitations, headaches, and diaphoresis—**not hypoglycemia**.
- This test is not relevant to the differential diagnosis of hypoglycemia.
*Genetic testing*
- **Genetic testing** might be considered for rare hereditary causes of hypoglycemia, such as congenital hyperinsulinism or genetic insulinoma syndromes (e.g., MEN1).
- Given the clinical context (depressed nurse with access to insulin and empty syringes found at home), **exogenous insulin administration** is far more likely than a genetic condition.
- Genetic testing is not the appropriate initial diagnostic step in this scenario.
*24 hr cortisol*
- A **24-hour urinary cortisol** test is used to diagnose **Cushing's syndrome** (cortisol excess), not hypoglycemia.
- While **adrenal insufficiency** (cortisol deficiency) can cause hypoglycemia, it typically presents with **hypotension**, **hyponatremia**, **hyperkalemia**, and **hyperpigmentation**—features not described in this case.
- The clinical presentation strongly suggests insulin-related hypoglycemia rather than adrenal insufficiency.
Diagnosis of chronic pancreatitis US Medical PG Question 9: A 54-year-old woman comes to the physician because of an ulcer on her left ankle for 6 years. She has had multiple ulcers over her left lower extremity during this period that have subsided with wound care and dressing. She has type 2 diabetes mellitus and gastroesophageal reflux disease. Current medications include metformin, sitagliptin, and omeprazole. She appears anxious. She is 162 cm (5 ft 4 in) tall and weighs 89 kg (196 lb); BMI is 34 kg/m2. Vital signs are within normal limits. Examination shows a 7.5-cm (3-in) ulcer with elevated, indurated margins and a necrotic floor above the left medial malleolus. There are multiple dilated, tortuous veins along the left lower extremity. There is 2+ pretibial edema of the lower extremities bilaterally. The skin around the left ankle appears darker than the right and there are multiple excoriation marks. Cardiopulmonary examination shows no abnormalities. Which of the following is the most appropriate next step in management of this patient's current condition?
- A. Trendelenburg test
- B. Punch biopsy (Correct Answer)
- C. Digital subtraction angiography
- D. Perthes test
- E. CT scan of the left leg
Diagnosis of chronic pancreatitis Explanation: ***Punch biopsy***
- A 6-year history of a non-healing **ulcer with elevated, indurated margins and a necrotic floor** is highly suspicious for **Marjolin's ulcer**, a type of squamous cell carcinoma arising in chronic wounds.
- A **punch biopsy** is the most appropriate next step to obtain a tissue diagnosis and confirm or rule out malignancy.
*Trendelenburg test*
- The Trendelenburg test assesses **venous valve competence** in superficial veins.
- While this patient has signs of **venous insufficiency** (dilated veins, edema, skin changes), the primary concern is the non-healing, suspicious ulcer, for which biopsy is more urgent.
*Digital subtraction angiography*
- Digital subtraction angiography is used to visualize **arterial blood flow** and diagnose peripheral artery disease.
- Although the patient has diabetes, there are no classic signs of significant arterial insufficiency (e.g., claudication, cold limb, diminished pulses), and the ulcer characteristics are more suggestive of malignancy or venous etiology.
*Perthes test*
- The Perthes test evaluates the **patency of deep veins** and the function of communicating veins by assessing changes in superficial venous distension after exercise with a tourniquet.
- Similar to the Trendelenburg test, it focuses on venous hemodynamics, which is secondary to the suspicion of malignancy in a chronic, non-healing ulcer.
*CT scan of the left leg*
- A CT scan can assess the **extent of soft tissue destruction or bone involvement** if malignancy is suspected or confirmed.
- However, it is not the initial diagnostic step for determining the nature of the ulcer itself; a **tissue biopsy** is required for definitive diagnosis.
Diagnosis of chronic pancreatitis US Medical PG Question 10: A pathologist receives a skin biopsy specimen from a patient who is suspected to have developed graft-versus-host disease (GVHD) following allogeneic stem-cell transplantation. The treating physician informs the pathologist that he is specifically concerned about the diagnosis as the patient developed skin lesions on the 90th-day post-transplantation and therefore, by definition, it should be considered a case of acute GVHD. However, the lesions clinically appear like those of chronic GVHD. The pathologist examines the slide under the microscope and confirms the diagnosis of chronic GVHD. Which of the following findings on skin biopsy is most likely to have helped the pathologist to confirm the diagnosis?
- A. Complete separation of the dermis and epidermis
- B. Focal vacuolization in the basal cell layer
- C. Lymphocytic infiltration of the superficial dermis
- D. Hypergranulosis (Correct Answer)
- E. Diffuse vacuolization in the basal cell layer
Diagnosis of chronic pancreatitis Explanation: ***Hypergranulosis***
- The presence of **hypergranulosis** (thickening of the granular layer) is a characteristic histological feature often seen in **chronic graft-versus-host disease (GVHD)**, especially in the sclerodermoid variant.
- This finding, along with other changes like epidermal atrophy and dermal fibrosis, helps differentiate chronic GVHD from acute forms.
*Complete separation of the dermis and epidermis*
- **Dermal-epidermal separation** (e.g., **subepidermal bullae**) is characteristic of severe acute GVHD (grade III-IV), indicating extensive tissue damage.
- It is not a typical feature of chronic GVHD, and its presence would suggest a more acute process.
*Focal vacuolization in the basal cell layer*
- **Focal vacuolization** and **dyskeratosis** (apoptotic keratinocytes) in the basal layer are classic microscopic signs of **acute graft-versus-host disease (GVHD)**.
- While some basal layer changes can occur in chronic GVHD, focal involvement specifically points towards an acute process rather than chronic features.
*Lymphocytic infiltration of the superficial dermis*
- **Lymphocytic infiltrate** in the superficial dermis is present in both acute and chronic GVHD, making it a **non-specific finding** for differentiating between the two.
- More specific features are needed to confirm a diagnosis of chronic GVHD.
*Diffuse vacuolization in the basal cell layer*
- Diffuse **vacuolar degeneration** of the basal cell layer is also a hallmark of **acute graft-versus-host disease (GVHD)**, indicating early epidermal damage.
- This feature points towards an acute process rather than the typical changes observed in chronic GVHD.
More Diagnosis of chronic pancreatitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.