Chronic pancreatitis pathophysiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Chronic pancreatitis pathophysiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Chronic pancreatitis pathophysiology US Medical PG Question 1: A 29-year-old female is hospitalized 1 day after an endoscopic retrograde cholangiopancreatography (ERCP) because of vomiting, weakness, and severe abdominal pain. Physical examination findings include abdominal tenderness and diminished bowel sounds. A CT scan demonstrates fluid around the pancreas. Serum levels of which of the following are likely to be low in this patient?
- A. Amylase
- B. Triglycerides
- C. Calcium (Correct Answer)
- D. Glucose
- E. Lipase
Chronic pancreatitis pathophysiology Explanation: ***Calcium***
- In **acute pancreatitis**, systemic inflammation can lead to **saponification** of perinecrotic fat, binding calcium and causing **hypocalcemia**.
- Additionally, glucagon release and hypomagnesemia can contribute to decreased parathyroid hormone (PTH) secretion and end-organ resistance, further lowering calcium levels.
*Amylase*
- **Amylase** levels are typically **elevated** in acute pancreatitis due to the release of pancreatic enzymes into the bloodstream.
- An elevated amylase, along with lipase, is a key diagnostic marker for pancreatitis.
*Triglycerides*
- **Hypertriglyceridemia** can cause acute pancreatitis, and triglyceride levels would be expected to be **elevated** in such cases.
- Triglycerides themselves are not directly lowered by the pancreatitis process in the way calcium is.
*Glucose*
- **Glucose** levels often become **elevated** in acute pancreatitis due to impaired insulin secretion and increased glucagon release.
- Pancreatic damage can affect the endocrine function of the pancreas, leading to hyperglycemia.
*Lipase*
- **Lipase** levels are also typically **elevated** in acute pancreatitis, often staying elevated longer than amylase.
- It is a more specific marker for pancreatic injury than amylase.
Chronic pancreatitis pathophysiology US Medical PG Question 2: A 42-year-old man comes to the physician because of severe epigastric pain for a week. The pain is constant and he describes it as 6 out of 10 in intensity. The pain radiates to his back and is worse after meals. He has had several episodes of nausea and vomiting during this period. He has taken ibuprofen for multiple similar episodes of pain during the past 6 months. He also has had a 5.4-kg (12-lb) weight loss over the past 4 months. He has a 12-year history of drinking 3 to 4 pints of rum daily. He has been hospitalized three times for severe abdominal pain in the past 3 years. He appears ill. His temperature is 37°C (98.6°F), pulse is 87/min, and blood pressure is 110/70 mm Hg. There is severe epigastric tenderness to palpation. Bowel sounds are normal. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.6 g/dL
Leukocyte count 7,800/mm3
Serum
Glucose 106 mg/dL
Creatinine 1.1 mg/dL
Amylase 150 U/L
A CT of the abdomen is shown. Which of the following is the most appropriate long-term management for this patient?
- A. Pancreatic enzyme therapy (Correct Answer)
- B. Whipple procedure
- C. Endoscopic stent placement
- D. Celiac ganglion block
- E. Gluten-free diet
Chronic pancreatitis pathophysiology Explanation: ***Pancreatic enzyme therapy***
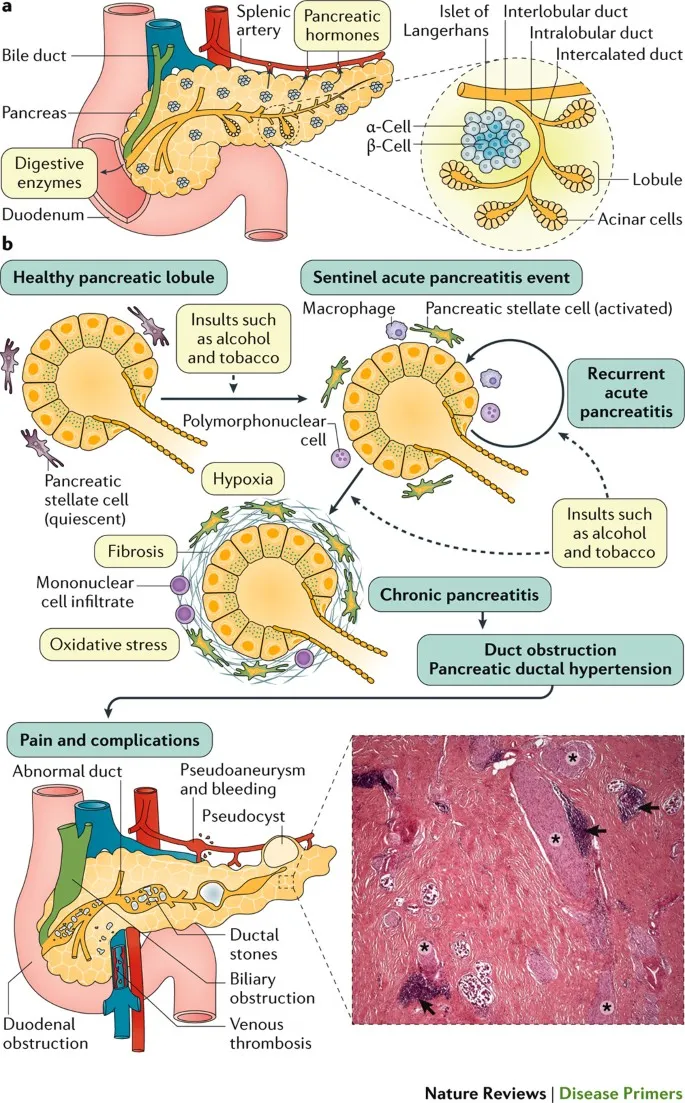
- This patient likely has **chronic pancreatitis** due to long-term alcohol abuse, presenting with severe epigastric pain, weight loss, and recurrent episodes. **Pancreatic enzyme replacement therapy (PERT)** helps in managing malabsorption and pain by reducing pancreatic stimulation.
- While amylase is only slightly elevated (150 U/L), this is typical in chronic pancreatitis where extensive glandular destruction prevents dramatic enzyme elevation seen in acute pancreatitis. The abdominal CT would likely show calcifications or ductal dilation, further supporting the diagnosis and the need for enzyme support due to **exocrine insufficiency.**
*Whipple procedure*
- The **Whipple procedure** (pancreaticoduodenectomy) is a complex surgical intervention primarily performed for **pancreatic head tumors** or severe, intractable chronic pancreatitis not amenable to less invasive treatments.
- This patient's symptoms, while severe, do not immediately indicate a need for such aggressive surgery, and other medical managements should be attempted first.
*Endoscopic stent placement*
- **Endoscopic stent placement** is typically used to relieve **biliary obstruction** or **pancreatic duct strictures** that cause pain or cholangitis in chronic pancreatitis.
- While it might be considered for specific ductal complications, it is not the initial long-term management for the diverse symptoms of chronic pancreatitis, especially **exocrine insufficiency**.
*Celiac ganglion block*
- A **celiac ganglion block** provides temporary pain relief for severe abdominal pain, particularly in conditions like **chronic pancreatitis** or **pancreatic cancer**, by interrupting nerve signals.
- It is a **palliative measure** for pain control and does not address the underlying **exocrine insufficiency** or disease progression, making it not a long-term comprehensive management strategy.
*Gluten-free diet*
- A **gluten-free diet** is the primary treatment for **celiac disease**, an autoimmune disorder affecting the small intestine.
- There is no clinical indication or laboratory finding in this patient's presentation (e.g., diarrhea, positive celiac serology) to suggest celiac disease as the cause of his symptoms or to warrant a gluten-free diet.
Chronic pancreatitis pathophysiology US Medical PG Question 3: A 29-year-old woman presents with a 2-hour history of sudden onset of severe mid-epigastric pain. The pain radiates to the back, and is not relieved by over-the-counter antacids. The patient also complains of profuse vomiting. The patient’s medical history is negative for similar symptoms. She consumes 3–4 alcoholic drinks daily. The blood pressure is 80/40 mm Hg and the heart rate is 105/min. Examination of the lungs reveals bibasilar crackles. Abdominal examination reveals diffuse tenderness involving the entire abdomen, marked guarding, rigidity, and reduced bowel sounds. The chest X-ray is normal. However, the abdominal CT scan reveals peritoneal fluid collection and diffuse pancreatic enlargement. The laboratory findings include:
Aspartate aminotransferase 63 IU/L
Alkaline phosphatase 204 IU/L
Alanine aminotransferase 32 IU/L
Serum amylase 500 IU/L (Normal: 25-125 IU/L)
Serum lipase 1,140 IU/L (Normal: 0-160 IU/L)
Serum calcium 2 mmol/L
Which of the following cellular changes are most likely, based on the clinical and laboratory findings?
- A. Liquefactive necrosis
- B. Dry gangrene
- C. Caseous necrosis
- D. Coagulative necrosis
- E. Fat necrosis (Correct Answer)
Chronic pancreatitis pathophysiology Explanation: ***Fat necrosis***
- The patient's presentation with severe epigastric pain radiating to the back, elevated serum amylase and lipase, **alcohol abuse**, and diffuse pancreatic enlargement indicates **acute pancreatitis**.
- **Fat necrosis** is a characteristic pathologic finding in acute pancreatitis, resulting from the release of activated pancreatic enzymes (like lipase) into the surrounding adipose tissue, causing **FFA (free fatty acid)** formation that complexes with calcium (saponification).
*Liquefactive necrosis*
- This type of necrosis is characterized by the complete digestion of dead cells, resulting in a **viscous liquid mass**.
- It is typically seen in **bacterial infections** or **cerebral infarcts**, not primarily in pancreatitis.
*Dry gangrene*
- **Dry gangrene** involves ischemic necrosis, usually affecting the extremities, where the tissue becomes **dry, shrunken, and black**.
- It is caused by **lack of blood supply** and does not fit the clinical picture of acute pancreatitis.
*Caseous necrosis*
- **Caseous necrosis** is a distinct form of coagulative necrosis, characterized by a **cheese-like appearance** of the necrotic tissue.
- It is most commonly associated with **tuberculosis** and certain fungal infections, not acute pancreatitis.
*Coagulative necrosis*
- **Coagulative necrosis** is characterized by the preservation of the cell shape and tissue architecture for several days after cell death, often due to **ischemia** (e.g., myocardial infarction).
- While pancreatic cells can undergo coagulative necrosis in severe ischemia, **fat necrosis** is specifically and prominently associated with the enzymatic destruction in acute pancreatitis.
Chronic pancreatitis pathophysiology US Medical PG Question 4: A 28-year-old man presents to the emergency department with diffuse abdominal pain and nausea for the past 5 hours. The pain started with a dull ache but is now quite severe. He notes that he “just doesn’t feel like eating” and has not eaten anything for almost a day. Although the nausea is getting worse, the patient has not vomited. He notes no medical issues in the past and is not currently taking any medications. He admits to drinking alcohol (at least 2–3 bottles of beer per day after work and frequent binge-drinking weekends with friends). He says that he does not smoke or use illicit drugs. Vital signs include: pulse rate 120/min, respiratory rate 26/min, and blood pressure 100/70 mm Hg. On examination, the patient’s abdomen is diffusely tender. His breath smells like alcohol, with a fruity tinge to it. Bowel sounds are present. No other findings are noted. Fingerstick glucose is 76mg/dL. After the examination, the patient suddenly and spontaneously vomits. Which of the following is the underlying mechanism of the most likely diagnosis in this patient?
- A. Increased acetyl CoA levels (Correct Answer)
- B. Inadequate insulin production
- C. Increased osmolal gap
- D. Starvation
- E. Thiamine deficiency
Chronic pancreatitis pathophysiology Explanation: ***Increased acetyl CoA levels***
- This patient presents with **alcoholic ketoacidosis (AKA)**, and the underlying biochemical mechanism is the accumulation of **acetyl CoA** that is shunted into ketone body synthesis.
- In AKA, starvation depletes glycogen stores and **oxaloacetate** (needed for the TCA cycle). Simultaneously, alcohol metabolism increases the **NADH/NAD+ ratio**, which further impairs gluconeogenesis and reduces oxaloacetate availability.
- Enhanced lipolysis (due to low insulin and high counter-regulatory hormones) produces large amounts of fatty acids, which undergo β-oxidation to generate **acetyl CoA**.
- With insufficient oxaloacetate to enter the TCA cycle, acetyl CoA accumulates and is diverted to **ketogenesis** (producing acetoacetate, β-hydroxybutyrate, and acetone).
- The **fruity breath** is from acetone, and the metabolic acidosis causes the patient's symptoms (abdominal pain, nausea, tachycardia, tachypnea).
*Starvation*
- While **starvation** is a critical **precipitating factor** in AKA (it depletes glycogen and triggers lipolysis), it is not the underlying biochemical mechanism itself.
- Starvation creates the metabolic conditions (low insulin, depleted oxaloacetate) that lead to the accumulation of acetyl CoA and subsequent ketogenesis, but the question asks for the mechanism, not the trigger.
*Inadequate insulin production*
- **Inadequate insulin production** is the primary defect in **diabetic ketoacidosis (DKA)**, which is ruled out by this patient's normal blood glucose (76 mg/dL).
- In AKA, insulin levels are typically low (due to starvation), but this is secondary to metabolic stress rather than a primary pancreatic failure. The key mechanism is still the acetyl CoA accumulation and shunting to ketogenesis.
*Increased osmolal gap*
- An **increased osmolal gap** suggests unmeasured osmolytes, typically seen with toxic alcohol ingestions (methanol, ethylene glycol) or severe lactic acidosis.
- While ethanol itself can transiently increase the osmolal gap, this is not the mechanism explaining the ketoacidosis, fruity breath, and clinical presentation in this case.
*Thiamine deficiency*
- **Thiamine deficiency** is common in chronic alcoholics and causes Wernicke-Korsakoff syndrome and other neurological complications.
- Thiamine is a cofactor for pyruvate dehydrogenase and α-ketoglutarate dehydrogenase, but its deficiency does not directly cause the ketoacidosis seen here, which results from altered lipid metabolism and acetyl CoA accumulation.
Chronic pancreatitis pathophysiology US Medical PG Question 5: A group of scientists is studying the mechanism of action of various pancreatic hormones in rats. The scientists studied hormone A, which is secreted by the β-cells of the pancreas, and found that hormone A binds to a complex dimeric receptor on the cell membrane and exerts its effects via phosphorylation and subsequent downstream signaling that includes dephosphorylation of different intracellular proteins. Now they are studying hormone B, which is secreted by the α-cells and antagonizes the actions of hormone A. Which 2nd messenger system would hormone B utilize to exert its cellular effects?
- A. Direct cytoplasmic receptor binding
- B. Phospholipase C
- C. Tyrosine kinase
- D. Direct nuclear receptor binding
- E. Adenylyl cyclase-cyclic AMP (Correct Answer)
Chronic pancreatitis pathophysiology Explanation: ***Adenylyl cyclase-cyclic AMP***
- Hormone B is **glucagon**, secreted by pancreatic α-cells, which antagonizes the effects of insulin (hormone A). Glucagon primarily acts through a **G protein-coupled receptor** that activates **adenylyl cyclase**, leading to an increase in intracellular **cyclic AMP (cAMP)**.
- Increased cAMP then activates **protein kinase A (PKA)**, which phosphorylates various intracellular proteins to promote **glycogenolysis** and **gluconeogenesis**, thereby raising blood glucose levels.
*Direct cytoplasmic receptor binding*
- This mechanism is characteristic of **steroid hormones**, which are lipid-soluble and can diffuse across the cell membrane to bind to receptors in the cytoplasm.
- Pancreatic hormones like glucagon are **peptide hormones**, which are water-soluble and typically bind to cell surface receptors.
*Phospholipase C*
- Activation of **phospholipase C (PLC)** leads to the production of **inositol triphosphate (IP3)** and **diacylglycerol (DAG)**, which mobilize intracellular calcium and activate protein kinase C, respectively.
- While some G protein-coupled receptors activate PLC, **glucagon's primary signaling pathway** involves adenylyl cyclase.
*Tyrosine kinase*
- **Tyrosine kinase receptors** are often associated with growth factors and insulin (hormone A) signaling, leading to phosphorylation of tyrosine residues on target proteins.
- Glucagon's receptor is a **G protein-coupled receptor**, not a receptor tyrosine kinase, and its actions are mediated through serine/threonine phosphorylation via PKA.
*Direct nuclear receptor binding*
- This mechanism is typical for **steroid hormones** and **thyroid hormones**, which are lipid-soluble and bind to receptors in the nucleus to directly influence gene transcription.
- As a peptide hormone, glucagon binds to cell surface receptors and does not directly interact with nuclear receptors.
Chronic pancreatitis pathophysiology US Medical PG Question 6: A 47-year-old woman with chronic epigastric pain comes to the physician because of a 1-month history of intermittent, loose, foul-smelling stools. She has also had a 6-kg (13-lb) weight loss. She has consumed 9–10 alcoholic beverages daily for the past 25 years. Seven years ago, she traveled to Mexico on vacation; she has not been outside the large metropolitan area in which she resides since then. She appears malnourished. The stool is pale and loose; fecal fat content is elevated. An immunoglobulin A serum anti-tissue transglutaminase antibody assay is negative. Further evaluation is most likely to show which of the following?
- A. Inflammation of subcutaneous fat
- B. Pancreatic calcifications (Correct Answer)
- C. Trophozoites on stool microscopy
- D. Positive lactulose breath test
- E. Villous atrophy of duodenal mucosa
Chronic pancreatitis pathophysiology Explanation: ***Pancreatic calcifications*** (Correct Answer)
- The patient's history of **chronic epigastric pain**, heavy **alcohol consumption** for 25 years, **steatorrhea** (foul-smelling, loose, pale stools with elevated fecal fat), and **weight loss** are classic signs of **chronic pancreatitis**.
- **Pancreatic calcifications** are a hallmark finding in chronic pancreatitis on imaging (CT scan or abdominal X-ray), often indicating irreversible damage and impaired exocrine function, leading to **malabsorption** and steatorrhea.
- This is the most likely finding on further evaluation given the clinical presentation.
*Inflammation of subcutaneous fat*
- This symptom, known as **panniculitis** (pancreatic panniculitis), is associated with pancreatic disease but is a rare complication and less specific diagnostic finding than pancreatic calcifications in chronic pancreatitis.
- While it can occur in severe pancreatitis due to **lipolytic enzymes** (lipase, amylase), the core presentation strongly points to underlying pancreatic dysfunction impacting digestion, not primarily skin involvement.
*Trophozoites on stool microscopy*
- **Trophozoites** in stool suggest parasitic infections like **Giardiasis**, which can cause steatorrhea and malabsorption.
- However, the patient's long history of **alcohol abuse** and chronic epigastric pain makes chronic pancreatitis a much more likely explanation for her symptoms than a parasitic infection, especially given her travel history was seven years prior.
*Positive lactulose breath test*
- A **positive lactulose breath test** indicates **small intestinal bacterial overgrowth (SIBO)**, which can cause malabsorption and steatorrhea.
- While SIBO can occur as a complication of chronic pancreatitis, it is a less direct explanation for the entire constellation of symptoms (chronic pain, severe alcohol history, and weight loss) compared to the structural pancreatic changes seen in chronic pancreatitis.
*Villous atrophy of duodenal mucosa*
- **Villous atrophy of the duodenal mucosa** is characteristic of **celiac disease**, which also causes malabsorption and steatorrhea.
- However, the patient's **negative anti-tissue transglutaminase antibody assay** effectively rules out celiac disease as the cause of her symptoms.
Chronic pancreatitis pathophysiology US Medical PG Question 7: A 46-year-old man is brought to the emergency department because of severe epigastric pain and vomiting for the past 4 hours. The pain is constant, radiates to his back, and is worse on lying down. He has had 3–4 episodes of greenish-colored vomit. He was treated for H. pylori infection around 2 months ago with triple-regimen therapy. He has atrial fibrillation and hypertension. He owns a distillery on the outskirts of a town. The patient drinks 4–5 alcoholic beverages daily. Current medications include dabigatran and metoprolol. He appears uncomfortable. His temperature is 37.8°C (100°F), pulse is 102/min, and blood pressure is 138/86 mm Hg. Examination shows severe epigastric tenderness to palpation with guarding but no rebound. Bowel sounds are hypoactive. Rectal examination shows no abnormalities. Laboratory studies show:
Hematocrit 53%
Leukocyte count 11,300/mm3
Serum
Na+ 133 mEq/L
Cl- 98 mEq/L
K+ 3.1 mEq/L
Calcium 7.8 mg/dL
Urea nitrogen 43 mg/dL
Glucose 271 mg/dL
Creatinine 2.0 mg/dL
Total bilirubin 0.7 mg/dL
Alkaline phosphatase 61 U/L
AST 19 U/L
ALT 17 U/L
γ-glutamyl transferase (GGT) 88 u/L (N=5–50 U/L)
Lipase 900 U/L (N=14–280 U/L)
Which of the following is the most appropriate next step in management?
- A. Crystalloid fluid infusion (Correct Answer)
- B. Fomepizole therapy
- C. Calcium gluconate therapy
- D. Endoscopic retrograde cholangio-pancreatography
- E. Laparotomy
Chronic pancreatitis pathophysiology Explanation: ***Crystalloid fluid infusion***
- The patient presents with **acute pancreatitis**, indicated by severe epigastric pain radiating to the back, vomiting, epigastric tenderness, and markedly elevated **lipase** (900 U/L).
- He shows clear signs of **hypovolemia**: elevated hematocrit (53%), elevated BUN/Cr ratio (43/2.0 = 21.5), and tachycardia.
- Pancreatitis causes significant **fluid shifts** and third-spacing, requiring aggressive **intravenous fluid resuscitation** with crystalloids (preferably lactated Ringer's) to prevent hypovolemic shock, acute kidney injury, and organ dysfunction.
- Early aggressive fluid resuscitation (250–500 mL/h initially) is the **cornerstone of acute pancreatitis management** and improves outcomes.
*Fomepizole therapy*
- **Fomepizole** is an antidote for **methanol** or **ethylene glycol** poisoning, which cause a high anion gap metabolic acidosis and visual disturbances.
- While the patient owns a distillery, his symptoms and lab findings (elevated lipase, hypocalcemia, mild leukocytosis) are consistent with **alcoholic pancreatitis**, not toxic alcohol ingestion.
- No anion gap is present, and there are no visual symptoms.
*Calcium gluconate therapy*
- Although the patient has **hypocalcemia** (7.8 mg/dL), which is common in severe pancreatitis due to fat saponification and calcium sequestration, routine calcium gluconate administration is generally **not recommended unless symptomatic**.
- Symptomatic hypocalcemia includes tetany, paresthesias, seizures, or prolonged QT interval, none of which are present.
- Aggressive fluid resuscitation and management of the underlying pancreatitis are higher priorities.
*Endoscopic retrograde cholangio-pancreatography*
- **ERCP** is primarily indicated for **gallstone pancreatitis with cholangitis** or persistent biliary obstruction.
- This patient likely has **alcoholic pancreatitis** (heavy alcohol use, elevated GGT), and there's no evidence of biliary obstruction (normal bilirubin, AST, ALT, ALP).
- Routine early ERCP in acute pancreatitis without cholangitis is not beneficial and carries procedural risks.
*Laparotomy*
- **Laparotomy** (surgical exploration) is rarely indicated in the initial management of acute pancreatitis.
- It might be considered for complications such as infected necrosis, pancreatic abscess, or abdominal compartment syndrome, but there is no indication for surgical intervention in this patient at this stage.
- Initial management focuses on medical stabilization with fluid resuscitation and supportive care.
Chronic pancreatitis pathophysiology US Medical PG Question 8: A 62-year-old Caucasian man visits his primary care provider with recurrent episodes of moderate to severe abdominal pain, nausea, and anorexia for the past 2 years. Additional complaints include constipation, steatorrhea, weight loss, polyphagia, and polyuria. His personal history is relevant for a 2-year period of homelessness when the patient was 55 years old, cigarette smoking since the age of 20, alcohol abuse, and cocaine abuse for which is currently under the supervision of a psychiatry team. He has a pulse of 70/min, a respiratory rate of 16/min, a blood pressure of 130/70 mm Hg, and a body temperature of 36.4°C (97.5°F). His height is 178 cm (5 ft 10 in) and weight is 90 kg (198 lb). On physical examination, he is found to have telangiectasias over the anterior chest, mild epigastric tenderness, and a small nodular liver. Laboratory test results from his previous visit a month ago are shown below:
Fasting plasma glucose 160 mg/dL
HbA1c 8%
Serum triglycerides 145 mg/dL
Total cholesterol 250 mg/dL
Total bilirubin 0.8 mg/dL
Direct bilirubin 0.2 mg/dL
Amylase 180 IU/L
Lipase 50 IU/L
Stool negative for blood; low elastase
This patient’s condition is most likely secondary to which of the following conditions?
- A. Hypertriglyceridemia
- B. Alcohol abuse (Correct Answer)
- C. Cocaine abuse
- D. Hypercholesterolemia
- E. Obesity
Chronic pancreatitis pathophysiology Explanation: ***Alcohol abuse***
- Chronic alcohol abuse is a major risk factor for **chronic pancreatitis**, which manifests with recurrent abdominal pain, steatorrhea, weight loss, and can lead to **diabetes mellitus** (polyphagia, polyuria, elevated fasting glucose and HbA1c).
- The elevated amylase, although not diagnostic for chronic pancreatitis on its own, along with low stool elastase (indicating **pancreatic exocrine insufficiency**), telangiectasias (suggesting liver disease often associated with alcohol), and a nodular liver (pointing to **cirrhosis**), strongly support chronic pancreatitis secondary to alcohol.
*Hypertriglyceridemia*
- While severe hypertriglyceridemia (typically >1000 mg/dL) can cause acute pancreatitis, the patient's triglyceride level (145 mg/dL) is not high enough to be the cause of his chronic pancreatic issues.
- Furthermore, chronic pancreatitis symptoms like steatorrhea and diabetes are better explained by long-term alcohol exposure.
*Cocaine abuse*
- Cocaine can cause **vasoconstriction** and ischemia, potentially leading to acute pancreatitis, but it is not a common cause of chronic pancreatitis with the constellation of symptoms observed here.
- The clinical picture strongly aligns with the chronic effects of alcohol on the pancreas and liver.
*Hypercholesterolemia*
- While hypercholesterolemia (total cholesterol 250 mg/dL) is a risk factor for cardiovascular disease, it is not directly implicated in causing pancreatitis or liver disease in the way described.
- It does not explain the recurrent abdominal pain, steatorrhea, or the development of diabetes and liver changes seen in this patient.
*Obesity*
- Obesity is a risk factor for various metabolic disorders, including type 2 diabetes and non-alcoholic fatty liver disease (NAFLD), but it is not a primary cause of chronic pancreatitis.
- The specific signs of liver damage (telangiectasias, nodular liver) and the pancreatic exocrine insufficiency point away from obesity as the primary etiology for this patient's condition.
Chronic pancreatitis pathophysiology US Medical PG Question 9: A 55-year-old man with a history of repeated hospitalization for chronic pancreatitis comes to the physician because of difficulty walking and standing steadily. Neurological examination shows an unsteady, broad-based gait, distal muscle weakness, decreased deep tendon reflexes, and an abnormal Romberg test. His hemoglobin concentration is 11.9 g/dL, mean corpuscular volume is 89/μm3, and serum lactate dehydrogenase is 105 U/L. His serum haptoglobin is slightly decreased. A deficiency of which of the following substances is the most likely cause of this patient's findings?
- A. Niacin
- B. Folate
- C. Phytomenadione
- D. Tocopherol (Correct Answer)
- E. Pyridoxine
Chronic pancreatitis pathophysiology Explanation: ***Tocopherol***
- **Tocopherol (Vitamin E)** deficiency can cause neurological symptoms such as **ataxia**, **distal muscle weakness**, decreased deep tendon reflexes, and an **abnormal Romberg test** due to its role in nerve function and antioxidant properties.
- **Chronic pancreatitis** often leads to **fat malabsorption** as pancreatic enzymes are crucial for fat digestion, which impairs the absorption of fat-soluble vitamins like Vitamin E.
*Niacin*
- **Niacin (Vitamin B3)** deficiency causes **pellagra**, characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia**, none of which are the primary presenting symptoms here.
- While neurological symptoms can occur in severe cases, the specific presentation of ataxia and peripheral neuropathy points away from pellagra.
*Folate*
- **Folate (Vitamin B9)** deficiency primarily causes **megaloblastic anemia** with an elevated **mean corpuscular volume (MCV)**, which is normal in this patient (MCV 89/μm3).
- While neurological symptoms can be present, they are less specific to folate deficiency compared to the classic presentation seen here.
*Phytomenadione*
- **Phytomenadione (Vitamin K)** deficiency leads to **coagulopathy** due to impaired synthesis of clotting factors, resulting in bleeding tendencies.
- It does not typically cause neurological symptoms like ataxia or peripheral neuropathy.
*Pyridoxine*
- **Pyridoxine (Vitamin B6)** deficiency can cause **peripheral neuropathy** and **ataxia**, but it's often associated with **sideroblastic anemia** or seizures.
- While some symptoms overlap, the strong history of chronic pancreatitis and fat malabsorption makes a fat-soluble vitamin deficiency more likely.
Chronic pancreatitis pathophysiology US Medical PG Question 10: A 32-year-old man with a history of chronic alcoholism presents to the emergency department with vomiting and diarrhea for 1 week. He states he feels weak and has had poor oral intake during this time. The patient is a current smoker and has presented many times to the emergency department for alcohol intoxication. His temperature is 97.5°F (36.4°C), blood pressure is 102/62 mmHg, pulse is 135/min, respirations are 25/min, and oxygen saturation is 99% on room air. On physical exam, he is found to have orthostatic hypotension and dry mucus membranes. Laboratory studies are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 3.9 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 9.8 mg/dL
The patient is given normal saline, oral potassium, dextrose, thiamine, and folic acid. The following day, the patient seems confused and complains of diffuse weakness and muscle/bone pain. An ECG and head CT are performed and are unremarkable. Which of the following is the most likely explanation for this patient's new symptoms?
- A. Hypomagnesemia
- B. Hyponatremia
- C. Hypoglycemia
- D. Hypophosphatemia (Correct Answer)
- E. Hypocalcemia
Chronic pancreatitis pathophysiology Explanation: **Hypophosphatemia**
- **Hypophosphatemia** is common in **alcoholics**, often exacerbated by refeeding (administration of glucose and fluids). The patient's initial symptoms of weakness and muscle/bone pain after treatment suggest this condition.
- Symptoms such as **confusion**, **diffuse weakness**, and **muscle/bone pain** are classic manifestations of severe hypophosphatemia as phosphorus is vital for muscle and nerve function, and bone health.
*Hypomagnesemia*
- While common in alcoholics and capable of causing weakness, **hypomagnesemia** typically presents with symptoms like **tremors**, **seizures**, and **cardiac arrhythmias**.
- The patient's primary symptoms of confusion and diffuse muscle/bone pain are less characteristic of magnesium deficiency compared to phosphorus deficiency.
*Hyponatremia*
- The patient's initial sodium level was 139 mEq/L, which is within the normal range, making **hyponatremia** unlikely to be the cause of new symptoms.
- While severe hyponatremia can cause confusion, it typically presents with other neurological symptoms like **headache** and **seizures**, which are not reported here.
*Hypoglycemia*
- The initial glucose level of 99 mg/dL was normal, and the patient received dextrose, making **hypoglycemia** an unlikely cause of the new symptoms.
- Symptoms of hypoglycemia usually include **sweating**, **tremors**, and **palpitations**, in addition to confusion.
*Hypocalcemia*
- The patient's initial calcium level was 9.8 mg/dL, which is within the normal range, making **hypocalcemia** an unlikely cause of the new symptoms.
- Symptoms of hypocalcemia typically include **tetany**, **paresthesias**, and a **prolonged QT interval** on EKG, none of which are described.
More Chronic pancreatitis pathophysiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.