Autoimmune pancreatitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Autoimmune pancreatitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Autoimmune pancreatitis US Medical PG Question 1: A 35-year-old Caucasian female presents with anemia, malaise, bloating, and diarrhea. Past genetic testing revealed that this patient carries the HLA-DQ2 allele. The physician suspects that the patient's presentation is dietary in cause. Which of the following findings would definitively confirm this diagnosis?
- A. CT scan showing inflammation of the small bowel wall
- B. Biopsy of the duodenum showing atrophy and blunting of villi (Correct Answer)
- C. Biopsy of the colon showing epithelial cell apoptosis
- D. Esophageal endoscopy showing lower esophageal metaplasia
- E. Liver biopsy showing apoptosis of hepatocytes
Autoimmune pancreatitis Explanation: ***Biopsy of the duodenum showing atrophy and blunting of villi***
- This finding is the **gold standard** for diagnosing **celiac disease**, which aligns with the patient's symptoms (anemia, malaise, bloating, diarrhea), genetic predisposition (HLA-DQ2 allele), and suspected dietary cause.
- The characteristic **villous atrophy** and **crypt hyperplasia** seen in duodenal biopsies are hallmark pathological changes in celiac disease due to gluten exposure.
*CT scan showing inflammation of the small bowel wall*
- While a CT scan can show **inflammation**, it is not specific enough to definitively diagnose celiac disease, as many other conditions can cause small bowel inflammation.
- It does not provide the **histopathological detail** necessary to confirm villous atrophy, which is key for celiac diagnosis.
*Biopsy of the colon showing epithelial cell apoptosis*
- **Epithelial cell apoptosis** in the colon is not a primary diagnostic feature of celiac disease, which primarily affects the **small intestine**.
- This finding might be associated with other inflammatory bowel conditions or infections, not gluten-induced enteropathy.
*Esophageal endoscopy showing lower esophageal metaplasia*
- **Lower esophageal metaplasia**, or **Barrett's esophagus**, is a pre-cancerous condition of the esophagus, often caused by chronic acid reflux.
- This finding is unrelated to celiac disease and does not explain the patient's gastrointestinal symptoms or genetic predisposition.
*Liver biopsy showing apoptosis of hepatocytes*
- **Apoptosis of hepatocytes** (liver cell death) would indicate liver damage or disease, such as hepatitis or drug-induced injury.
- While celiac disease can sometimes have **hepatic manifestations**, liver apoptosis is not a primary or definitive diagnostic criterion for celiac disease itself.
Autoimmune pancreatitis US Medical PG Question 2: A 36-year-old man is brought to the emergency department 3 hours after the onset of progressively worsening upper abdominal pain and 4 episodes of vomiting. His father had a myocardial infarction at the age of 40 years. Physical examination shows tenderness and guarding in the epigastrium. Bowel sounds are decreased. His serum amylase is 400 U/L. Symptomatic treatment and therapy with fenofibrate are initiated. Further evaluation of this patient is most likely to show which of the following findings?
- A. Elevated serum IgG4 levels
- B. Salt and pepper skull
- C. Separate dorsal and ventral pancreatic ducts
- D. Decreased serum ACTH levels
- E. Eruptive xanthomas (Correct Answer)
Autoimmune pancreatitis Explanation: ***Eruptive xanthomas***
- The patient presents with **acute pancreatitis** (abdominal pain, vomiting, elevated amylase) and a strong family history of early **myocardial infarction**, suggesting a genetic predisposition to **hypertriglyceridemia**.
- **Fenofibrate** is prescribed to lower **triglyceride levels**, and **eruptive xanthomas** are a classic cutaneous manifestation of severe **hypertriglyceridemia**, often leading to pancreatitis.
*Elevated serum IgG4 levels*
- Elevated **IgG4 levels** are characteristic of **autoimmune pancreatitis**, which can mimic acute pancreatitis but is typically treated with steroids and not primarily fenofibrate.
- While IgG4-related disease can affect the pancreas, the patient's family history and fenofibrate treatment point away from this diagnosis.
*Salt and pepper skull*
- A **salt and pepper skull** is a classic radiographic finding in **hyperparathyroidism**, indicating bone demineralization and resorption.
- This finding is unrelated to the patient's presentation of acute pancreatitis and hyperlipidemia.
*Separate dorsal and ventral pancreatic ducts*
- **Pancreas divisum** refers to the failure of fusion of the **dorsal and ventral pancreatic ducts**, which can predispose individuals to recurrent pancreatitis due to impaired drainage.
- While a possibility for recurrent pancreatitis, it does not explain the patient's family history of early cardiac events or the specific treatment with fenofibrate, which targets hypertriglyceridemia.
*Decreased serum ACTH levels*
- **Decreased serum ACTH levels** are typically associated with **exogenous corticosteroid use** or **adrenal tumors** producing cortisol, leading to Cushing's syndrome.
- This finding is unrelated to acute pancreatitis or hypertriglyceridemia and does not fit the clinical picture.
Autoimmune pancreatitis US Medical PG Question 3: A 21-year-old female presents to her obstetrician because she has stopped getting her period, after being irregular for the last 3 months. Upon further questioning, the patient reveals that she has had a 17 lb. unintended weight loss, endorses chronic diarrhea, abdominal pain, and constipation that waxes and wanes. Family history is notable only for an older brother with Type 1 Diabetes. She is healthy, and is eager to gain back some weight. Her OBGYN refers her to a gastroenterologist, but first sends serology laboratory studies for IgA anti-tissue transglutaminase antibodies (IgA-tTG). These results come back positive at > 10x the upper limit of normal. Which of the following is the gastroenterologist likely to find on endoscopy and duodenal biopsy?
- A. Friable mucosal pseudopolyps with biopsy notable for crypt abscesses
- B. Cobblestoning with biopsy showing transmural inflammation and noncaseating granulomas
- C. Villous atrophy with crypt lengthening and intraepithelial lymphocytes (Correct Answer)
- D. Foamy macrophages, which stain PAS positive
- E. Normal appearing villi and biopsy
Autoimmune pancreatitis Explanation: ***Villous atrophy with crypt lengthening and intraepithelial lymphocytes***
- The patient's symptoms (amenorrhea, weight loss, diarrhea, abdominal pain, constipation) combined with a **positive IgA anti-tissue transglutaminase antibody (IgA-tTG)** strongly suggest **celiac disease**.
- The characteristic endoscopic and histological findings in celiac disease are **villous atrophy**, **crypt hyperplasia (lengthening)**, and increased **intraepithelial lymphocytes** in the small intestine.
*Friable mucosal pseudopolyps with biopsy notable for crypt abscesses*
- This description is characteristic of **ulcerative colitis**, an inflammatory bowel disease, which typically causes **bloody diarrhea** and is not associated with positive IgA-tTG antibodies.
- **Pseudopolyps** result from cycles of ulceration and regeneration, and **crypt abscesses** are hallmarks of active inflammation in ulcerative colitis.
*Cobblestoning with biopsy showing transmural inflammation and noncaseating granulomas*
- This describes the typical findings in **Crohn's disease**, another inflammatory bowel disease, which can cause **abdominal pain** and **diarrhea** but is not linked to IgA-tTG antibodies.
- **Transmural inflammation** means inflammation extends through all layers of the bowel wall, and **noncaseating granulomas** are a key distinguishing feature.
*Foamy macrophages, which stain PAS positive*
- These findings are characteristic of **Whipple's disease**, a rare bacterial infection caused by *Tropheryma whipplei*.
- While Whipple's disease can present with **malabsorption** and **weight loss**, it is not associated with positive celiac serology.
*Normal appearing villi and biopsy*
- Given the patient's strong clinical suspicion for celiac disease and a **highly positive IgA-tTG** test, normal findings on endoscopy and biopsy would be highly unlikely.
- A definitive diagnosis of celiac disease typically requires characteristic histological changes to confirm the serological findings.
Autoimmune pancreatitis US Medical PG Question 4: A 15-year-old girl is brought to the physician because of an 8-month history of fatigue, intermittent postprandial abdominal bloating and discomfort, foul-smelling, watery diarrhea, and a 7-kg (15-lb) weight loss. She developed a pruritic rash on her knees 3 days ago. Physical examination shows several tense, excoriated vesicles on the knees bilaterally. The abdomen is soft and nontender. Her hemoglobin concentration is 8.2 g/dL and mean corpuscular volume is 76 μm3. Further evaluation of this patient is most likely to show which of the following findings?
- A. IgA tissue transglutaminase antibodies (Correct Answer)
- B. Elevated serum amylase concentration
- C. Intraluminal esophageal membrane
- D. Periodic acid-Schiff-positive macrophages
- E. Positive hydrogen breath test
Autoimmune pancreatitis Explanation: ***IgA tissue transglutaminase antibodies***
- The patient's symptoms of **fatigue, abdominal bloating and discomfort, watery diarrhea, weight loss, iron deficiency anemia**, and a **pruritic rash (dermatitis herpetiformis)** are highly suggestive of **celiac disease**.
- **IgA tissue transglutaminase (tTG) antibodies** are the most sensitive and specific serological test for celiac disease.
*Elevated serum amylase concentration*
- **Elevated serum amylase** is typically indicative of **pancreatitis**, which is not supported by the patient's symptoms (e.g., severe epigastric pain radiating to the back).
- While malabsorption can lead to some pancreatic dysfunction, it would not be the primary diagnostic finding for this presentation.
*Intraluminal esophageal membrane*
- **Intraluminal esophageal membranes** or **webs** are typically associated with conditions like **Plummer-Vinson syndrome** or **eosinophilic esophagitis**, presenting with dysphagia.
- These findings do not explain the patient's prominent gastrointestinal symptoms, weight loss, rash, or anemia.
*Periodic acid-Schiff-positive macrophages*
- **Periodic acid-Schiff (PAS)-positive macrophages** in the lamina propria are characteristic of **Whipple disease**.
- Whipple disease typically presents with polyarthralgia, lymphadenopathy, and neurological symptoms in addition to malabsorption, which are not described here.
*Positive hydrogen breath test*
- A **positive hydrogen breath test** suggests **small intestinal bacterial overgrowth (SIBO)** or **lactose intolerance**.
- While SIBO can cause bloating and diarrhea, it does not explain the pruritic rash (dermatitis herpetiformis) or the severity of the anemia and weight loss as the primary diagnosis.
Autoimmune pancreatitis US Medical PG Question 5: A 42-year-old man comes to the physician because of severe epigastric pain for a week. The pain is constant and he describes it as 6 out of 10 in intensity. The pain radiates to his back and is worse after meals. He has had several episodes of nausea and vomiting during this period. He has taken ibuprofen for multiple similar episodes of pain during the past 6 months. He also has had a 5.4-kg (12-lb) weight loss over the past 4 months. He has a 12-year history of drinking 3 to 4 pints of rum daily. He has been hospitalized three times for severe abdominal pain in the past 3 years. He appears ill. His temperature is 37°C (98.6°F), pulse is 87/min, and blood pressure is 110/70 mm Hg. There is severe epigastric tenderness to palpation. Bowel sounds are normal. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.6 g/dL
Leukocyte count 7,800/mm3
Serum
Glucose 106 mg/dL
Creatinine 1.1 mg/dL
Amylase 150 U/L
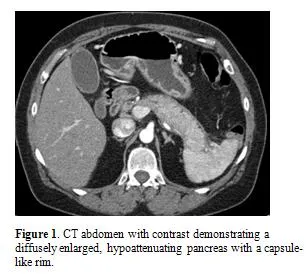
A CT of the abdomen is shown. Which of the following is the most appropriate long-term management for this patient?
- A. Pancreatic enzyme therapy (Correct Answer)
- B. Whipple procedure
- C. Endoscopic stent placement
- D. Celiac ganglion block
- E. Gluten-free diet
Autoimmune pancreatitis Explanation: ***Pancreatic enzyme therapy***
- This patient likely has **chronic pancreatitis** due to long-term alcohol abuse, presenting with severe epigastric pain, weight loss, and recurrent episodes. **Pancreatic enzyme replacement therapy (PERT)** helps in managing malabsorption and pain by reducing pancreatic stimulation.
- While amylase is only slightly elevated (150 U/L), this is typical in chronic pancreatitis where extensive glandular destruction prevents dramatic enzyme elevation seen in acute pancreatitis. The abdominal CT would likely show calcifications or ductal dilation, further supporting the diagnosis and the need for enzyme support due to **exocrine insufficiency.**
*Whipple procedure*
- The **Whipple procedure** (pancreaticoduodenectomy) is a complex surgical intervention primarily performed for **pancreatic head tumors** or severe, intractable chronic pancreatitis not amenable to less invasive treatments.
- This patient's symptoms, while severe, do not immediately indicate a need for such aggressive surgery, and other medical managements should be attempted first.
*Endoscopic stent placement*
- **Endoscopic stent placement** is typically used to relieve **biliary obstruction** or **pancreatic duct strictures** that cause pain or cholangitis in chronic pancreatitis.
- While it might be considered for specific ductal complications, it is not the initial long-term management for the diverse symptoms of chronic pancreatitis, especially **exocrine insufficiency**.
*Celiac ganglion block*
- A **celiac ganglion block** provides temporary pain relief for severe abdominal pain, particularly in conditions like **chronic pancreatitis** or **pancreatic cancer**, by interrupting nerve signals.
- It is a **palliative measure** for pain control and does not address the underlying **exocrine insufficiency** or disease progression, making it not a long-term comprehensive management strategy.
*Gluten-free diet*
- A **gluten-free diet** is the primary treatment for **celiac disease**, an autoimmune disorder affecting the small intestine.
- There is no clinical indication or laboratory finding in this patient's presentation (e.g., diarrhea, positive celiac serology) to suggest celiac disease as the cause of his symptoms or to warrant a gluten-free diet.
Autoimmune pancreatitis US Medical PG Question 6: A 22-year-old woman presents to the emergency department with a 3-day history of fever and abdominal pain. She says that the pain is located in the left lower quadrant of the abdomen and feels crampy in nature. The pain has been associated with bloody diarrhea and joint tenderness. She has no past medical history but says that she returned 2 weeks ago from vacation in Asia where she tried many new foods. Her family history is significant for multiple cancers in close relatives. Physical exam reveals swollen ulcers on her legs, and colonoscopy reveals contiguous ulcerations from the rectum through the descending colon. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Noncaseating granulomas
- B. Severe aortic stenosis
- C. Gram-negative rod
- D. HLA-DQ2 positivity
- E. Perinuclear anti-neutrophil cytoplasmic antibodies (Correct Answer)
Autoimmune pancreatitis Explanation: ***Perinuclear anti-neutrophil cytoplasmic antibodies***
- The patient's presentation with **bloody diarrhea**, low-grade fever, **crampy abdominal pain**, joint tenderness, and contiguous ulcerations in the colon is highly suggestive of **ulcerative colitis**.
- **Perinuclear anti-neutrophil cytoplasmic antibodies (p-ANCA)** are found in 50-70% of patients with ulcerative colitis and are associated with a more extensive disease.
*Noncaseating granulomas*
- **Noncaseating granulomas** are a characteristic histological finding in **Crohn's disease**, not ulcerative colitis.
- Crohn's disease typically presents with **skip lesions**, **transmural inflammation**, and affects any part of the GI tract, often with perianal disease.
*Severe aortic stenosis*
- **Severe aortic stenosis** is a condition of the heart valves that can lead to symptoms like chest pain, syncope, and heart failure, and is not directly associated with the patient's gastrointestinal and systemic symptoms.
- While inflammatory conditions can rarely have cardiac manifestations, there's no direct link between aortic stenosis and inflammatory bowel disease in this context.
*Gram-negative rod*
- While infections, especially from **Gram-negative rods** like *Shigella* or *Salmonella*, can cause acute bloody diarrhea, the 3-day history with joint tenderness and contiguous ulcers on colonoscopy points more towards an inflammatory bowel disease.
- The chronicity and systemic involvement are less typical for an acute bacterial enteritis, although such infections might trigger IBD.
*HLA-DQ2 positivity*
- **HLA-DQ2 positivity** is strongly associated with **celiac disease**, an immune-mediated enteropathy triggered by gluten.
- Celiac disease typically presents with malabsorption symptoms like fatty stools, weight loss, and iron deficiency, rather than bloody diarrhea and contiguous colonic ulcerations.
Autoimmune pancreatitis US Medical PG Question 7: A 46-year-old man is brought to the emergency department because of severe epigastric pain and vomiting for the past 4 hours. The pain is constant, radiates to his back, and is worse on lying down. He has had 3–4 episodes of greenish-colored vomit. He was treated for H. pylori infection around 2 months ago with triple-regimen therapy. He has atrial fibrillation and hypertension. He owns a distillery on the outskirts of a town. The patient drinks 4–5 alcoholic beverages daily. Current medications include dabigatran and metoprolol. He appears uncomfortable. His temperature is 37.8°C (100°F), pulse is 102/min, and blood pressure is 138/86 mm Hg. Examination shows severe epigastric tenderness to palpation with guarding but no rebound. Bowel sounds are hypoactive. Rectal examination shows no abnormalities. Laboratory studies show:
Hematocrit 53%
Leukocyte count 11,300/mm3
Serum
Na+ 133 mEq/L
Cl- 98 mEq/L
K+ 3.1 mEq/L
Calcium 7.8 mg/dL
Urea nitrogen 43 mg/dL
Glucose 271 mg/dL
Creatinine 2.0 mg/dL
Total bilirubin 0.7 mg/dL
Alkaline phosphatase 61 U/L
AST 19 U/L
ALT 17 U/L
γ-glutamyl transferase (GGT) 88 u/L (N=5–50 U/L)
Lipase 900 U/L (N=14–280 U/L)
Which of the following is the most appropriate next step in management?
- A. Crystalloid fluid infusion (Correct Answer)
- B. Fomepizole therapy
- C. Calcium gluconate therapy
- D. Endoscopic retrograde cholangio-pancreatography
- E. Laparotomy
Autoimmune pancreatitis Explanation: ***Crystalloid fluid infusion***
- The patient presents with **acute pancreatitis**, indicated by severe epigastric pain radiating to the back, vomiting, epigastric tenderness, and markedly elevated **lipase** (900 U/L).
- He shows clear signs of **hypovolemia**: elevated hematocrit (53%), elevated BUN/Cr ratio (43/2.0 = 21.5), and tachycardia.
- Pancreatitis causes significant **fluid shifts** and third-spacing, requiring aggressive **intravenous fluid resuscitation** with crystalloids (preferably lactated Ringer's) to prevent hypovolemic shock, acute kidney injury, and organ dysfunction.
- Early aggressive fluid resuscitation (250–500 mL/h initially) is the **cornerstone of acute pancreatitis management** and improves outcomes.
*Fomepizole therapy*
- **Fomepizole** is an antidote for **methanol** or **ethylene glycol** poisoning, which cause a high anion gap metabolic acidosis and visual disturbances.
- While the patient owns a distillery, his symptoms and lab findings (elevated lipase, hypocalcemia, mild leukocytosis) are consistent with **alcoholic pancreatitis**, not toxic alcohol ingestion.
- No anion gap is present, and there are no visual symptoms.
*Calcium gluconate therapy*
- Although the patient has **hypocalcemia** (7.8 mg/dL), which is common in severe pancreatitis due to fat saponification and calcium sequestration, routine calcium gluconate administration is generally **not recommended unless symptomatic**.
- Symptomatic hypocalcemia includes tetany, paresthesias, seizures, or prolonged QT interval, none of which are present.
- Aggressive fluid resuscitation and management of the underlying pancreatitis are higher priorities.
*Endoscopic retrograde cholangio-pancreatography*
- **ERCP** is primarily indicated for **gallstone pancreatitis with cholangitis** or persistent biliary obstruction.
- This patient likely has **alcoholic pancreatitis** (heavy alcohol use, elevated GGT), and there's no evidence of biliary obstruction (normal bilirubin, AST, ALT, ALP).
- Routine early ERCP in acute pancreatitis without cholangitis is not beneficial and carries procedural risks.
*Laparotomy*
- **Laparotomy** (surgical exploration) is rarely indicated in the initial management of acute pancreatitis.
- It might be considered for complications such as infected necrosis, pancreatic abscess, or abdominal compartment syndrome, but there is no indication for surgical intervention in this patient at this stage.
- Initial management focuses on medical stabilization with fluid resuscitation and supportive care.
Autoimmune pancreatitis US Medical PG Question 8: A 36-year-old woman presents for a pre-employment health assessment. She has no complaints. Her last annual physical examination 8 months ago was normal. She has no significant past medical history. She is a nonsmoker and says she quit all alcohol consumption last year. A complete hepatic biochemistry panel is performed, which is significant for a serum alkaline phosphatase (ALP) level 5 times the upper limit of the normal range. Immunologic tests are positive for antimitochondrial antibodies. A liver biopsy is performed and reveals an inflammatory infiltrate surrounding the biliary ducts. Which of the following is the most likely diagnosis in this patient?
- A. Pancreatic cancer
- B. Primary biliary cholangitis (Correct Answer)
- C. Hepatic amyloidosis
- D. Choledocolithiasis
- E. Fascioliasis
Autoimmune pancreatitis Explanation: ***Primary biliary cholangitis***
- The combination of significantly elevated **alkaline phosphatase** (indicating cholestasis), positive **antimitochondrial antibodies (AMA)**, and an inflammatory infiltrate around the bile ducts on biopsy is highly diagnostic of primary biliary cholangitis (PBC).
- PBC is a **chronic autoimmune liver disease** predominantly affecting middle-aged women, characterized by progressive destruction of small intrahepatic bile ducts.
*Pancreatic cancer*
- Pancreatic cancer typically presents with symptoms like **jaundice**, weight loss, and abdominal pain, none of which are present in this asymptomatic patient.
- While it can cause cholestasis and elevated ALP, it would usually be associated with a **dilated common bile duct** on imaging and often obstructive symptoms.
*Hepatic amyloidosis*
- Hepatic amyloidosis can elevate ALP, but it would not typically be associated with **positive antimitochondrial antibodies**.
- Liver biopsy would show **amyloid deposits** rather than an inflammatory infiltrate surrounding biliary ducts.
*Choledocolithiasis*
- Choledocolithiasis (bile duct stones) would cause an **obstructive pattern** of elevated ALP, but it is often acutely symptomatic with **biliary colic** or cholangitis.
- It would not typically involve positive **antimitochondrial antibodies** or an inflammatory infiltrate characteristic of an autoimmune bile duct disease on biopsy.
*Fascioliasis*
- Fascioliasis is a **parasitic infection** that can cause eosinophilia and liver enzyme elevation, but it is associated with exposure to contaminated watercress or aquatic plants.
- It would not typically present with positive **antimitochondrial antibodies** and the specific inflammatory infiltrate seen in PBC.
Autoimmune pancreatitis US Medical PG Question 9: A previously healthy 48-year-old man comes to the physician because of a 3-week history of progressively worsening jaundice, generalized itching, and epigastric discomfort. He also complains of nausea and loss of appetite. His stools have looked like clay for the past week. He has returned from a vacation in Thailand one week ago, where he got a new tattoo. He is sexually active with multiple partners and does not use protection. His vital signs are within normal limits. Examination shows jaundice and scleral icterus. Superficial excoriations are seen on all limbs. Abdominal examination shows no abnormalities. Serum studies show a fasting glucose level of 198 mg/dL, total bilirubin concentration of 10.6 mg/dL, direct bilirubin concentration of 9.8 mg/dl, and alkaline phosphatase activity of 450 U/L. Abdominal ultrasonography shows dilation of the biliary and pancreatic ducts and a 3-cm hypoechoic solid mass with irregular margins in the head of the pancreas. An elevation of which of the following serum findings is most specific for this patient's condition?
- A. Anti-HBc immunoglobulin M
- B. Alpha-fetoprotein
- C. Elevated anti-neutrophil cytoplasmic antibodies
- D. Glucagon
- E. Cancer antigen 19-9 (Correct Answer)
Autoimmune pancreatitis Explanation: ***Cancer antigen 19-9***
- The patient's symptoms (progressively worsening jaundice, epigastric discomfort, clay-colored stools, weight loss, nausea) and imaging findings (dilation of biliary and pancreatic ducts, hypoechoic solid mass in the pancreatic head) are highly suggestive of **pancreatic cancer**.
- **CA 19-9** is a tumor marker that is elevated in most patients with pancreatic cancer and is used for diagnosis, monitoring treatment response, and detecting recurrence.
*Anti-HBc immunoglobulin M*
- **Anti-HBc IgM** indicates **acute hepatitis B infection**, which can cause jaundice but typically presents with elevated transaminases, and abdominal ultrasound would show liver inflammation, not a pancreatic mass or ductal dilation.
- While unprotected sexual activity is a risk factor for hepatitis B, the clinical picture with an obstructed biliary system points away from acute viral hepatitis as the primary cause.
*Alpha-fetoprotein*
- **Alpha-fetoprotein (AFP)** is a tumor marker primarily associated with **hepatocellular carcinoma** and some germ cell tumors.
- Although the patient has jaundice, the ultrasound findings of a pancreatic mass and dilated ducts are not consistent with hepatocellular carcinoma.
*Elevated anti-neutrophil cytoplasmic antibodies*
- **Anti-neutrophil cytoplasmic antibodies (ANCAs)** are associated with **autoimmune vasculitides** (e.g., GPA, MPA) and some inflammatory bowel diseases, not typically with obstructive jaundice due to a pancreatic mass.
- There are no symptoms or signs to suggest a systemic vasculitis in this patient.
*Glucagon*
- **Glucagon** is a hormone involved in glucose regulation. While the patient has elevated fasting glucose, a specific elevation of glucagon itself is associated with a rare **glucagonoma**, which typically presents with a characteristic rash (necrolytic migratory erythema), diabetes, and weight loss, none of which are the primary presenting features here.
- The elevated fasting glucose is more likely a paraneoplastic effect of pancreatic cancer, as the mass is compressing the bile ducts, and the patient has other features specific to pancreatic ductal adenocarcinoma.
Autoimmune pancreatitis US Medical PG Question 10: A 15-year-old African-American male with a BMI of 22 is brought to his physician by his mother to address concerns about a change in his dietary habits. The patient's mother notes that he is constantly hungry and thirsty, despite his eating and drinking water in excess. She also reports an increase in his use of the bathroom. The physician begins explaining that her son's symptoms are likely due to which of the following?
- A. Pancreatic islet hyperplasia and hypertrophy
- B. The patient's weight
- C. Insulitis (Correct Answer)
- D. Amyloid deposition in pancreatic islets
- E. Insensitivity to insulin
Autoimmune pancreatitis Explanation: ***Insulitis***
- This patient's symptoms of **polyphagia**, **polydipsia**, and **polyuria** are classic for **Type 1 Diabetes Mellitus (T1DM)**.
- **Insulitis** is the characteristic autoimmune inflammation of the pancreatic islets that destroys insulin-producing beta cells in T1DM.
*Pancreatic islet hyperplasia and hypertrophy*
- This is typically seen in conditions of **chronic insulin resistance**, such as early **Type 2 Diabetes Mellitus**, as the body attempts to compensate for increased insulin demand.
- It does not explain the acute onset of classic diabetic symptoms in a lean adolescent.
*The patient's weight*
- With a **BMI of 22**, the patient is within a healthy weight range and is not considered overweight or obese.
- While obesity is a major risk factor for **Type 2 Diabetes**, it is not typical for **Type 1 Diabetes**.
*Amyloid deposition in pancreatic islets*
- **Amyloid deposition**, specifically from **islet amyloid polypeptide (IAPP)**, is a pathological hallmark of **Type 2 Diabetes Mellitus**, not Type 1.
- This process contributes to beta-cell dysfunction and death in Type 2 Diabetes, but is secondary to the disease process, not the primary autoimmune destruction seen in Type 1.
*Insensitivity to insulin*
- **Insulin insensitivity** or **insulin resistance** is the defining feature of **Type 2 Diabetes Mellitus**.
- This patient's presentation of sudden symptoms in a lean adolescent strongly points to an absolute **deficiency of insulin**, not resistance.
More Autoimmune pancreatitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.