Acute pancreatitis diagnosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute pancreatitis diagnosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute pancreatitis diagnosis US Medical PG Question 1: A 42-year-old woman is brought to the emergency department because of a 5-day history of epigastric pain, fever, nausea, and malaise. Five weeks ago she had acute biliary pancreatitis and was treated with endoscopic retrograde cholangiopancreatography and subsequent cholecystectomy. Her maternal grandfather died of pancreatic cancer. She does not smoke. She drinks 1–2 beers daily. Her temperature is 38.7°C (101.7°F), respirations are 18/min, pulse is 120/min, and blood pressure is 100/70 mm Hg. Abdominal examination shows epigastric tenderness and three well-healed laparoscopy scars. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10 g/dL
Leukocyte count 15,800/mm3
Serum
Na+ 140 mEq/L
Cl− 103 mEq/L
K+ 4.5 mEq/L
HCO3- 25 mEq/L
Urea nitrogen 18 mg/dL
Creatinine 1.0 mg/dL
Alkaline phosphatase 70 U/L
Aspartate aminotransferase (AST, GOT) 22 U/L
Alanine aminotransferase (ALT, GPT) 19 U/L
γ-Glutamyltransferase (GGT) 55 U/L (N = 5–50)
Bilirubin 1 mg/dl
Glucose 105 mg/dL
Amylase 220 U/L
Lipase 365 U/L (N = 14–280)
Abdominal ultrasound shows a complex cystic fluid collection with irregular walls and septations in the pancreas. Which of the following is the most likely diagnosis?
- A. Pancreatic cancer
- B. Acute cholangitis
- C. Pancreatic abscess (Correct Answer)
- D. Pancreatic pseudocyst
- E. ERCP-induced pancreatitis
Acute pancreatitis diagnosis Explanation: ***Pancreatic abscess***
- The presence of fever, leukocytosis (WBC 15,800/mm³), and a complex, septated fluid collection seen on ultrasound, following acute pancreatitis, is highly suggestive of a **pancreatic abscess**.
- **Pancreatic abscesses** develop as a complication of acute pancreatitis, typically resulting from infected pancreatic necrosis and often present with persistent symptoms of infection.
*Pancreatic cancer*
- While there is a family history of pancreatic cancer, her acute presentation with **fever, leukocytosis**, and a tender, complex fluid collection is **not typical** for initial pancreatic cancer presentation.
- Pancreatic cancer typically presents with **jaundice, weight loss**, and chronic abdominal pain rather than acute infectious symptoms and a fluid collection after pancreatitis.
*Acute cholangitis*
- Acute cholangitis is characterized by **Charcot's triad** (fever, jaundice, right upper quadrant pain) or **Reynold's pentad** (Charcot's triad plus altered mental status and hypotension).
- The patient's **normal bilirubin level** (1 mg/dL), absence of jaundice, and epigastric pain (not right upper quadrant specific) make acute cholangitis less likely, especially with a history of cholecystectomy.
*Pancreatic pseudocyst*
- A pancreatic pseudocyst is a **sterile** fluid collection without signs of active infection (e.g., fever, leukocytosis) and typically has well-defined, smooth walls rather than irregular walls or septations.
- While she has a fluid collection from pancreatitis, the **fever, leukocytosis, and irregular/septated walls** on ultrasound point away from a simple pseudocyst and towards an infected collection.
*ERCP-induced pancreatitis*
- ERCP-induced pancreatitis would have occurred **immediately after the procedure**, which was five weeks ago. The current symptoms occurring five weeks later suggest a complication of the initial pancreatitis, not a new induction.
- While ERCP can cause pancreatitis, this diagnosis refers to the initial event, not a **secondary infectious complication** manifesting weeks later.
Acute pancreatitis diagnosis US Medical PG Question 2: A 29-year-old female is hospitalized 1 day after an endoscopic retrograde cholangiopancreatography (ERCP) because of vomiting, weakness, and severe abdominal pain. Physical examination findings include abdominal tenderness and diminished bowel sounds. A CT scan demonstrates fluid around the pancreas. Serum levels of which of the following are likely to be low in this patient?
- A. Amylase
- B. Triglycerides
- C. Calcium (Correct Answer)
- D. Glucose
- E. Lipase
Acute pancreatitis diagnosis Explanation: ***Calcium***
- In **acute pancreatitis**, systemic inflammation can lead to **saponification** of perinecrotic fat, binding calcium and causing **hypocalcemia**.
- Additionally, glucagon release and hypomagnesemia can contribute to decreased parathyroid hormone (PTH) secretion and end-organ resistance, further lowering calcium levels.
*Amylase*
- **Amylase** levels are typically **elevated** in acute pancreatitis due to the release of pancreatic enzymes into the bloodstream.
- An elevated amylase, along with lipase, is a key diagnostic marker for pancreatitis.
*Triglycerides*
- **Hypertriglyceridemia** can cause acute pancreatitis, and triglyceride levels would be expected to be **elevated** in such cases.
- Triglycerides themselves are not directly lowered by the pancreatitis process in the way calcium is.
*Glucose*
- **Glucose** levels often become **elevated** in acute pancreatitis due to impaired insulin secretion and increased glucagon release.
- Pancreatic damage can affect the endocrine function of the pancreas, leading to hyperglycemia.
*Lipase*
- **Lipase** levels are also typically **elevated** in acute pancreatitis, often staying elevated longer than amylase.
- It is a more specific marker for pancreatic injury than amylase.
Acute pancreatitis diagnosis US Medical PG Question 3: A 43-year-old man is brought to the emergency department because of severe epigastric pain and vomiting for 6 hours. The pain radiates to his back and he describes it as 9 out of 10 in intensity. He has had 3–4 episodes of vomiting during this period. He admits to consuming over 13 alcoholic beverages the previous night. There is no personal or family history of serious illness and he takes no medications. He is 177 cm (5 ft 10 in) tall and weighs 55 kg (121 lb); BMI is 17.6 kg/m2. He appears uncomfortable. His temperature is 37.5°C (99.5°F), pulse is 97/min, and blood pressure is 128/78 mm Hg. Abdominal examination shows severe epigastric tenderness to palpation. Bowel sounds are hypoactive. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.5 g/dL
Hematocrit 62%
Leukocyte count 13,800/mm3
Serum
Na+ 134 mEq/L
K+ 3.6 mEq/L
Cl- 98 mEq/L
Calcium 8.3 mg/dL
Glucose 180 mg/dL
Creatinine 0.9 mg/dL
Amylase 150 U/L
Lipase 347 U/L (N = 14–280)
Total bilirubin 0.8 mg/dL
Alkaline phosphatase 66 U/L
AST 19 U/L
ALT 18 U/L
LDH 360 U/L
Which of the following laboratory studies is the best prognostic indicator for this patient's condition?
- A. AST/ALT ratio
- B. Alkaline phosphatase
- C. Total bilirubin
- D. Lipase
- E. Hematocrit (Correct Answer)
Acute pancreatitis diagnosis Explanation: ***Hematocrit***
- A rising **hematocrit** (due to **hemoconcentration**) or one that fails to fall after initial fluid resuscitation is an important indicator of volume depletion and a **poor prognostic sign** in **acute pancreatitis**.
- This patient's hematocrit is elevated at **62%**, suggesting significant hemoconcentration and a higher risk for complications like **pancreatic necrosis**.
*AST/ALT ratio*
- While an elevated AST/ALT ratio can suggest **alcoholic liver disease**, it is not a direct **prognostic indicator** for the severity or outcome of **acute pancreatitis**.
- In pancreatitis, liver enzymes are typically elevated secondarily to inflammation or biliary obstruction, but their ratio does not directly predict the course of the pancreatitis itself.
*Alkaline phosphatase*
- **Alkaline phosphatase** is an indicator of **biliary obstruction** or **cholestasis**, which can be a cause of pancreatitis (e.g., gallstone pancreatitis).
- Its value does not directly predict the **severity** or **prognosis** of acute pancreatitis once it has developed, especially in a case of alcoholic pancreatitis.
*Total bilirubin*
- **Total bilirubin** levels primarily reflect **biliary obstruction** or **liver dysfunction**.
- While gallstone pancreatitis can increase bilirubin, it is not a primary prognostic marker for the development of severe complications in **acute pancreatitis**, nor is it significantly elevated in this patient.
*Lipase*
- **Elevated lipase** is highly specific and sensitive for the **diagnosis of acute pancreatitis**, confirming the diagnosis in this case.
- However, the absolute level of lipase does **not correlate** with the **severity** or **prognosis** of acute pancreatitis; even mild pancreatitis can have very high lipase levels.
Acute pancreatitis diagnosis US Medical PG Question 4: A 52-year-old man is brought to the emergency department with severe epigastric discomfort and left-sided chest pain radiating to the back that began after waking up. He has also vomited several times since the pain began. He underwent an esophagogastroduodenoscopy the previous day for evaluation of epigastric pain. He has ischemic heart disease and underwent a coronary angioplasty 3 years ago. His mother died of pancreatic cancer when she was 60 years old. His current medications include aspirin, clopidogrel, metoprolol, ramipril, and rosuvastatin. He is pale, anxious, and diaphoretic. His temperature is 37.9°C (100.2°F), pulse is 140/min, respirations are 20/min, and blood pressure is 100/60 mm Hg in his upper extremities and 108/68 mm Hg in his lower extremities. Pulse oximetry on room air shows oxygen saturation at 98%. An S4 is audible over the precordium, in addition to crepitus over the chest. Abdominal examination shows tenderness to palpation in the epigastric area. Serum studies show an initial Troponin I level of 0.031 ng/mL (N < 0.1 ng/mL) and 0.026 ng/mL 6 hours later. A 12-lead ECG shows sinus tachycardia with nonspecific ST-T changes. Which of the following is the most likely diagnosis?
- A. Esophageal perforation (Correct Answer)
- B. Pneumothorax
- C. Aortic dissection
- D. Acute pancreatitis
- E. Acute myocardial infarction
Acute pancreatitis diagnosis Explanation: ***Esophageal perforation***
- The patient's recent **esophagogastroduodenoscopy (EGD)**, followed by severe epigastric and chest pain radiating to the back, vomiting, and **subcutaneous emphysema (crepitus)**, is highly suggestive of esophageal perforation.
- **Mackler's triad** (vomiting, chest pain, and subcutaneous emphysema) is characteristic, and the overall clinical picture, including stable troponins and ECG, rules out cardiac events.
*Pneumothorax*
- While pneumothorax can cause chest pain and dyspnea, it typically presents with **diminished breath sounds** and **hyperresonance** on percussion, not crepitus over the chest (which indicates subcutaneous emphysema).
- A recent EGD is not a direct risk factor for pneumothorax, and the pain radiation to the back is less typical for a simple pneumothorax.
*Aortic dissection*
- Aortic dissection presents with sudden, **excruciating tearing chest pain** radiating to the back, and can cause a pulse deficit or **blood pressure differential** between limbs.
- While a slight BP differential is noted (100/60 vs 108/68), it's not significant enough for dissection, and the crepitus makes this diagnosis less likely without other definitive signs.
*Acute pancreatitis*
- Acute pancreatitis causes severe epigastric pain radiating to the back and vomiting, similar to this presentation.
- However, the presence of **crepitus** (subcutaneous emphysema) and a recent EGD makes esophageal perforation a more likely diagnosis, as EGD is not a typical trigger for acute pancreatitis.
*Acute myocardial infarction*
- The patient has risk factors for cardiac disease, and initial symptoms like chest pain and diaphoresis could suggest an MI.
- However, the **normal serial troponin levels** and **nonspecific ECG changes** rule out an acute myocardial infarction, especially given the presence of crepitus.
Acute pancreatitis diagnosis US Medical PG Question 5: A 75-year-old man presents to the emergency department for abdominal pain. The patient states the pain started this morning and has been worsening steadily. He decided to come to the emergency department when he began vomiting. The patient has a past medical history of obesity, diabetes, alcohol abuse, and hypertension. His current medications include captopril, insulin, metformin, sodium docusate, and ibuprofen. His temperature is 104.0°F (40°C), blood pressure is 160/97 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Abdominal exam reveals left lower quadrant tenderness. Cardiac exam reveals a crescendo systolic murmur heard best by the right upper sternal border. Lab values are ordered and return as below.
Hemoglobin: 15 g/dL
Hematocrit: 42%
Leukocyte count: 19,500 cells/mm^3 with normal differential
Platelet count: 226,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 144 mg/dL
Creatinine: 1.2 mg/dL
Ca2+: 9.8 mg/dL
Which of the following is the most accurate test for this patient's condition?
- A. Colonoscopy
- B. Sigmoidoscopy
- C. Amylase and lipase levels
- D. Barium enema
- E. CT scan (Correct Answer)
Acute pancreatitis diagnosis Explanation: ***CT scan***
- The patient presents with classic symptoms of **diverticulitis**, including **left lower quadrant pain**, **fever**, and **leukocytosis**. A **CT scan with oral and IV contrast** is the most accurate diagnostic test to identify diverticular inflammation, abscess formation, or perforation.
- A CT scan can also help rule out other causes of abdominal pain and guide further management, such as the need for percutaneous drainage of an abscess.
*Colonoscopy*
- **Colonoscopy is contraindicated during an acute episode of diverticulitis** due to the risk of **perforation** of an inflamed colon.
- It may be considered **6-8 weeks after resolution of acute diverticulitis** to investigate for other pathologies such as malignancy.
*Sigmoidoscopy*
- Similar to colonoscopy, **sigmoidoscopy is generally avoided in acute diverticulitis** because of the risk of **perforation** of the inflamed bowel from instrumentation.
- Its diagnostic yield in acute settings is also limited compared to CT imaging.
*Amylase and lipase levels*
- These tests are primarily used to diagnose **pancreatitis**, which typically presents with **epigastric pain radiating to the back**, often associated with elevated enzyme levels.
- While vomiting is present, the **left lower quadrant tenderness and fever** point away from pancreatitis as the primary diagnosis.
*Barium enema*
- **Barium enema is generally contraindicated in acute diverticulitis** due to the risk of **perforation** and the introduction of barium into the peritoneum, which can cause severe peritonitis.
- It has largely been replaced by **CT scanning** for its superior safety profile and diagnostic accuracy in acute abdominal conditions.
Acute pancreatitis diagnosis US Medical PG Question 6: A 52-year-old woman presents to the urgent care center with several hours of worsening abdominal discomfort that radiates to the back. The patient also complains of malaise, chills, nausea, and vomiting. Social history is notable for alcoholism. On physical exam, she is febrile to 39.5°C (103.1℉), and she is diffusely tender on abdominal palpation. Other vital signs include a blood pressure of 126/74 mm Hg, heart rate of 74/min, and respiratory rate of 14/min. Complete blood count is notable for 13,500 white blood cells (WBCs), and her complete metabolic panel shows bilirubin of 2.1 and amylase of 3210. Given the following options, what is the most likely diagnosis?
- A. Choledocholithiasis
- B. Cholelithiasis
- C. Acute cholecystitis
- D. Ascending cholangitis
- E. Gallstone pancreatitis (Correct Answer)
Acute pancreatitis diagnosis Explanation: ***Gallstone pancreatitis***
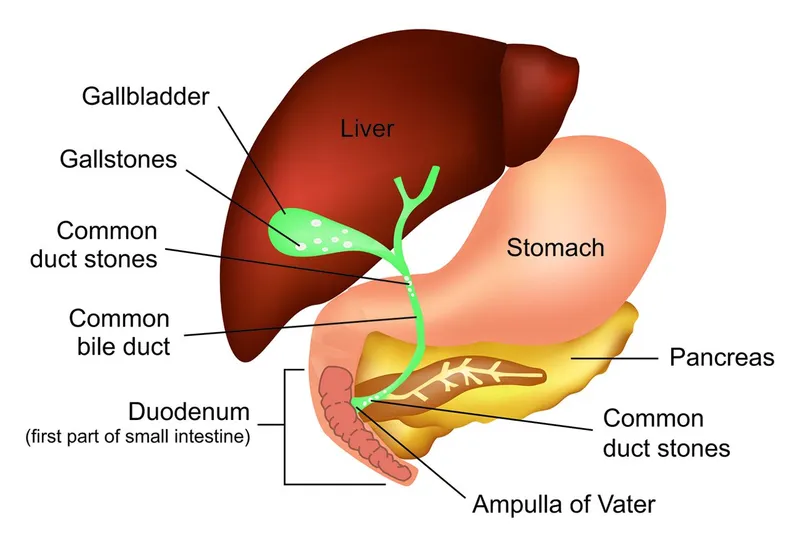
- The elevated **amylase** (3210) strongly indicates **acute pancreatitis**, while the **elevated bilirubin** (2.1) suggests **biliary obstruction**, pointing toward a **gallstone etiology** blocking the common bile duct.
- The radiating abdominal pain to the back, nausea, and vomiting along with systemic inflammatory response (fever, leukocytosis) are classic symptoms of **acute pancreatitis**.
- While the patient has a history of alcoholism, the elevated bilirubin is the key finding that suggests **gallstone-induced** rather than alcoholic pancreatitis.
*Choledocholithiasis*
- While an elevated bilirubin suggests **biliary obstruction**, the significantly high **amylase** points primarily to **pancreatic inflammation** rather than just a stone in the common bile duct.
- **Choledocholithiasis** typically causes **biliary colic**, jaundice, and potentially cholangitis, but not the markedly elevated amylase seen here unless it leads to pancreatitis.
*Cholelithiasis*
- **Cholelithiasis** (gallstones) often presents as **biliary colic**, characterized by episodic right upper quadrant pain, but usually without the systemic symptoms or markedly elevated amylase.
- While it's a precursor to other biliary conditions, it doesn't explain the patient's severe generalized symptoms, fever, or the definitive **pancreatitis labs**.
*Acute cholecystitis*
- **Acute cholecystitis** involves inflammation of the **gallbladder**, typically causing **right upper quadrant pain**, fever, and leukocytosis, often with a positive Murphy's sign.
- Although there's fever and leukocytosis, the **diffuse abdominal tenderness** and significantly high **amylase** are more indicative of pancreatitis than isolated gallbladder inflammation.
*Ascending cholangitis*
- **Ascending cholangitis** presents with **Charcot's triad** (fever, right upper quadrant pain, jaundice) or **Reynolds' pentad** (adding hypotension and altered mental status), but the key differentiating factor here is the extremely high amylase.
- While **elevated bilirubin** suggests biliary involvement, the primary pathology indicated by the **amylase level** is pancreatic, not solely biliary infection.
Acute pancreatitis diagnosis US Medical PG Question 7: A 29-year-old woman presents with a 2-hour history of sudden onset of severe mid-epigastric pain. The pain radiates to the back, and is not relieved by over-the-counter antacids. The patient also complains of profuse vomiting. The patient’s medical history is negative for similar symptoms. She consumes 3–4 alcoholic drinks daily. The blood pressure is 80/40 mm Hg and the heart rate is 105/min. Examination of the lungs reveals bibasilar crackles. Abdominal examination reveals diffuse tenderness involving the entire abdomen, marked guarding, rigidity, and reduced bowel sounds. The chest X-ray is normal. However, the abdominal CT scan reveals peritoneal fluid collection and diffuse pancreatic enlargement. The laboratory findings include:
Aspartate aminotransferase 63 IU/L
Alkaline phosphatase 204 IU/L
Alanine aminotransferase 32 IU/L
Serum amylase 500 IU/L (Normal: 25-125 IU/L)
Serum lipase 1,140 IU/L (Normal: 0-160 IU/L)
Serum calcium 2 mmol/L
Which of the following cellular changes are most likely, based on the clinical and laboratory findings?
- A. Liquefactive necrosis
- B. Dry gangrene
- C. Caseous necrosis
- D. Coagulative necrosis
- E. Fat necrosis (Correct Answer)
Acute pancreatitis diagnosis Explanation: ***Fat necrosis***
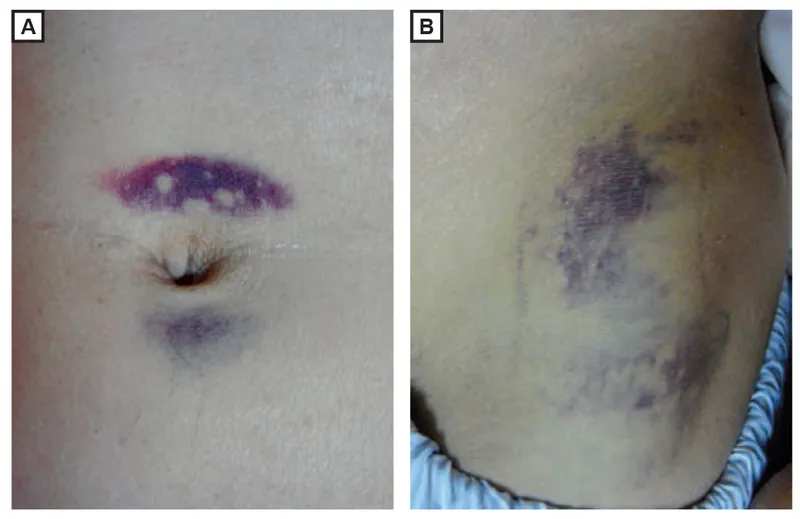
- The patient's presentation with severe epigastric pain radiating to the back, elevated serum amylase and lipase, **alcohol abuse**, and diffuse pancreatic enlargement indicates **acute pancreatitis**.
- **Fat necrosis** is a characteristic pathologic finding in acute pancreatitis, resulting from the release of activated pancreatic enzymes (like lipase) into the surrounding adipose tissue, causing **FFA (free fatty acid)** formation that complexes with calcium (saponification).
*Liquefactive necrosis*
- This type of necrosis is characterized by the complete digestion of dead cells, resulting in a **viscous liquid mass**.
- It is typically seen in **bacterial infections** or **cerebral infarcts**, not primarily in pancreatitis.
*Dry gangrene*
- **Dry gangrene** involves ischemic necrosis, usually affecting the extremities, where the tissue becomes **dry, shrunken, and black**.
- It is caused by **lack of blood supply** and does not fit the clinical picture of acute pancreatitis.
*Caseous necrosis*
- **Caseous necrosis** is a distinct form of coagulative necrosis, characterized by a **cheese-like appearance** of the necrotic tissue.
- It is most commonly associated with **tuberculosis** and certain fungal infections, not acute pancreatitis.
*Coagulative necrosis*
- **Coagulative necrosis** is characterized by the preservation of the cell shape and tissue architecture for several days after cell death, often due to **ischemia** (e.g., myocardial infarction).
- While pancreatic cells can undergo coagulative necrosis in severe ischemia, **fat necrosis** is specifically and prominently associated with the enzymatic destruction in acute pancreatitis.
Acute pancreatitis diagnosis US Medical PG Question 8: A 47-year-old presents to the clinic with a 3-day history of severe mid-epigastric abdominal pain radiating to the back. The patient has hypertension, diabetes mellitus, and hypertriglyceridemia. Prescription medications include enalapril, metformin, sitagliptin, glargine, lispro, and fenofibrate. The patient has not had a cigarette in more than 35 years, and reports only having 1 or 2 drinks during special occasions such as weddings and family reunions. The blood pressure is 146/90 mm Hg, the heart rate is 88/min, the respiratory rate is 10/min, and the temperature is 37.8°C (100.0°F). On physical examination, the patient appears uncomfortable but alert. The visualization of the sclera is negative for jaundice. The neck is supple and non-tender without nodules. There are no heart murmurs. The lungs are clear to auscultation bilaterally. The palpation of the abdomen elicits pain in the epigastric region. The liver is palpable along the costal margin, and the Murphy's sign is negative. The laboratory results are as follows:
Na+ 138 mEq/L
K+ 4.2 mEq/L
Cl- 108 mmol/L
HCO-3 20 mmol/L
BUN 18 mg/dL
Cr 1.0 mg/dL
Glucose 154 mg/dL
LDL 117 mg/dL
HDL 48 mg/dL
TG 942 mg/dL
AST 45 IU/L
ALT 48 IU/L
GGT 27 IU/L
Amylase 110 U/L
Lipase 250 U/L
According to the clinical vignette, which of the following is the most likely diagnosis of the patient?
- A. Duodenal ulcer
- B. Acute pancreatitis (Correct Answer)
- C. Superior mesenteric artery embolism
- D. Abdominal aortic aneurysm
- E. Mallory-Weiss tear
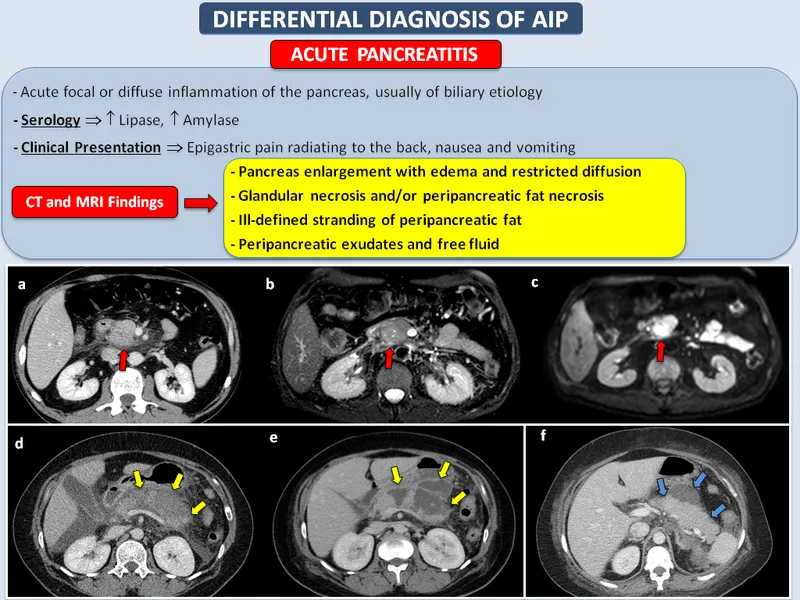
Acute pancreatitis diagnosis Explanation: ***Acute pancreatitis***
- The patient presents with **severe mid-epigastric abdominal pain radiating to the back**, a classic symptom of acute pancreatitis. The **elevated lipase (250 U/L)**, which is more specific than amylase, further supports this diagnosis, especially in the context of **hypertriglyceridemia (942 mg/dL)**, a common cause.
- While amylase is only mildly elevated (110 U/L, upper limit of normal around 100 U/L), lipase is significantly elevated. The patient's history of **hypertriglyceridemia** is a well-known risk factor for acute pancreatitis, and the pain description fits typical presentation.
*Duodenal ulcer*
- A duodenal ulcer would typically present with **epigastric pain that improves with food** and worsens several hours after eating, which is not described.
- While ulcers can cause severe pain, they are not typically associated with pain radiating to the back to this extent, nor would they present with isolated **elevations in lipase in the absence of other GI symptoms** like melena or hematemesis.
*Superior mesenteric artery embolism*
- This condition presents with **sudden onset, severe abdominal pain that is often out of proportion to physical exam findings**. It typically leads to signs of **bowel ischemia**, such as rectal bleeding, metabolic acidosis, and leukocytosis, which are absent here.
- The pain would likely be more diffuse, and while it could be severe, the specific elevated lipase in the setting of hypertriglyceridemia points away from this diagnosis.
*Abdominal aortic aneurysm*
- A ruptured or dissecting abdominal aortic aneurysm would cause **severe, abrupt abdominal or back pain**, often described as a tearing sensation, and would typically be accompanied by signs of **hemodynamic instability** (e.g., hypotension, shock), which are not observed (BP 146/90).
- A pulsating abdominal mass would also likely be present on examination, and this diagnosis does not explain the elevated lipase.
*Mallory-Weiss tear*
- A Mallory-Weiss tear is characterized by **hematemesis** following forceful vomiting or retching, resulting from a tear in the esophageal or gastric mucosa.
- The patient does not report vomiting or hematemesis, and the primary symptom is abdominal pain radiating to the back, not upper GI bleeding.
Acute pancreatitis diagnosis US Medical PG Question 9: A 59-year-old man presents to the emergency department with diffuse abdominal pain, nausea, and vomiting. Laboratory evaluation on admission is significant for serum glucose of 241 mg/dL, AST of 321 IU/L, and leukocytes of 21,200/μL. Within 3 days of admission with supportive care in the intensive care unit, the patient's clinical condition begins to improve. Based on Ranson's criteria, what is this patient's overall risk of mortality, assuming all other relevant factors are negative?
- A. 15% (Correct Answer)
- B. 40%
- C. 100%
- D. 80%
- E. < 10%
Acute pancreatitis diagnosis Explanation: ***15%***
- This patient meets four Ranson's criteria on admission: **age > 55 years** (59 years), **WBC > 16,000/μL** (21,200/μL), **glucose > 200 mg/dL** (241 mg/dL), and **AST > 250 U/L** (321 U/L).
- Four Ranson's criteria correspond to a **15% mortality risk**.
- The stem specifies that all other relevant factors (the 48-hour criteria) are negative.
*40%*
- A 40% mortality risk is associated with **5-6 positive Ranson's criteria**.
- This patient fulfilled 4 criteria on admission, indicating a lower risk category.
*100%*
- A 100% mortality risk is associated with **7 or more positive Ranson's criteria**.
- This patient only fulfilled 4 criteria, indicating a significantly lower risk.
*80%*
- An 80% mortality risk is associated with **7 or more positive Ranson's criteria**.
- This patient only fulfilled 4 criteria, which places him in a much lower risk category.
*< 10%*
- A mortality risk of less than 10% typically correlates with **0-2 positive Ranson's criteria**.
- This patient has 4 positive criteria, placing him in a higher risk category.
Acute pancreatitis diagnosis US Medical PG Question 10: A 46-year-old man is brought to the emergency department because of severe epigastric pain and vomiting for the past 4 hours. The pain is constant, radiates to his back, and is worse on lying down. He has had 3–4 episodes of greenish-colored vomit. He was treated for H. pylori infection around 2 months ago with triple-regimen therapy. He has atrial fibrillation and hypertension. He owns a distillery on the outskirts of a town. The patient drinks 4–5 alcoholic beverages daily. Current medications include dabigatran and metoprolol. He appears uncomfortable. His temperature is 37.8°C (100°F), pulse is 102/min, and blood pressure is 138/86 mm Hg. Examination shows severe epigastric tenderness to palpation with guarding but no rebound. Bowel sounds are hypoactive. Rectal examination shows no abnormalities. Laboratory studies show:
Hematocrit 53%
Leukocyte count 11,300/mm3
Serum
Na+ 133 mEq/L
Cl- 98 mEq/L
K+ 3.1 mEq/L
Calcium 7.8 mg/dL
Urea nitrogen 43 mg/dL
Glucose 271 mg/dL
Creatinine 2.0 mg/dL
Total bilirubin 0.7 mg/dL
Alkaline phosphatase 61 U/L
AST 19 U/L
ALT 17 U/L
γ-glutamyl transferase (GGT) 88 u/L (N=5–50 U/L)
Lipase 900 U/L (N=14–280 U/L)
Which of the following is the most appropriate next step in management?
- A. Crystalloid fluid infusion (Correct Answer)
- B. Fomepizole therapy
- C. Calcium gluconate therapy
- D. Endoscopic retrograde cholangio-pancreatography
- E. Laparotomy
Acute pancreatitis diagnosis Explanation: ***Crystalloid fluid infusion***
- The patient presents with **acute pancreatitis**, indicated by severe epigastric pain radiating to the back, vomiting, epigastric tenderness, and markedly elevated **lipase** (900 U/L).
- He shows clear signs of **hypovolemia**: elevated hematocrit (53%), elevated BUN/Cr ratio (43/2.0 = 21.5), and tachycardia.
- Pancreatitis causes significant **fluid shifts** and third-spacing, requiring aggressive **intravenous fluid resuscitation** with crystalloids (preferably lactated Ringer's) to prevent hypovolemic shock, acute kidney injury, and organ dysfunction.
- Early aggressive fluid resuscitation (250–500 mL/h initially) is the **cornerstone of acute pancreatitis management** and improves outcomes.
*Fomepizole therapy*
- **Fomepizole** is an antidote for **methanol** or **ethylene glycol** poisoning, which cause a high anion gap metabolic acidosis and visual disturbances.
- While the patient owns a distillery, his symptoms and lab findings (elevated lipase, hypocalcemia, mild leukocytosis) are consistent with **alcoholic pancreatitis**, not toxic alcohol ingestion.
- No anion gap is present, and there are no visual symptoms.
*Calcium gluconate therapy*
- Although the patient has **hypocalcemia** (7.8 mg/dL), which is common in severe pancreatitis due to fat saponification and calcium sequestration, routine calcium gluconate administration is generally **not recommended unless symptomatic**.
- Symptomatic hypocalcemia includes tetany, paresthesias, seizures, or prolonged QT interval, none of which are present.
- Aggressive fluid resuscitation and management of the underlying pancreatitis are higher priorities.
*Endoscopic retrograde cholangio-pancreatography*
- **ERCP** is primarily indicated for **gallstone pancreatitis with cholangitis** or persistent biliary obstruction.
- This patient likely has **alcoholic pancreatitis** (heavy alcohol use, elevated GGT), and there's no evidence of biliary obstruction (normal bilirubin, AST, ALT, ALP).
- Routine early ERCP in acute pancreatitis without cholangitis is not beneficial and carries procedural risks.
*Laparotomy*
- **Laparotomy** (surgical exploration) is rarely indicated in the initial management of acute pancreatitis.
- It might be considered for complications such as infected necrosis, pancreatic abscess, or abdominal compartment syndrome, but there is no indication for surgical intervention in this patient at this stage.
- Initial management focuses on medical stabilization with fluid resuscitation and supportive care.
More Acute pancreatitis diagnosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.